Impact of Pain Neuroscience Education Program in Community Physiotherapy Context on Pain Perception and Psychosocial Variables Associated with It in Elderly Persons: A Ranzomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
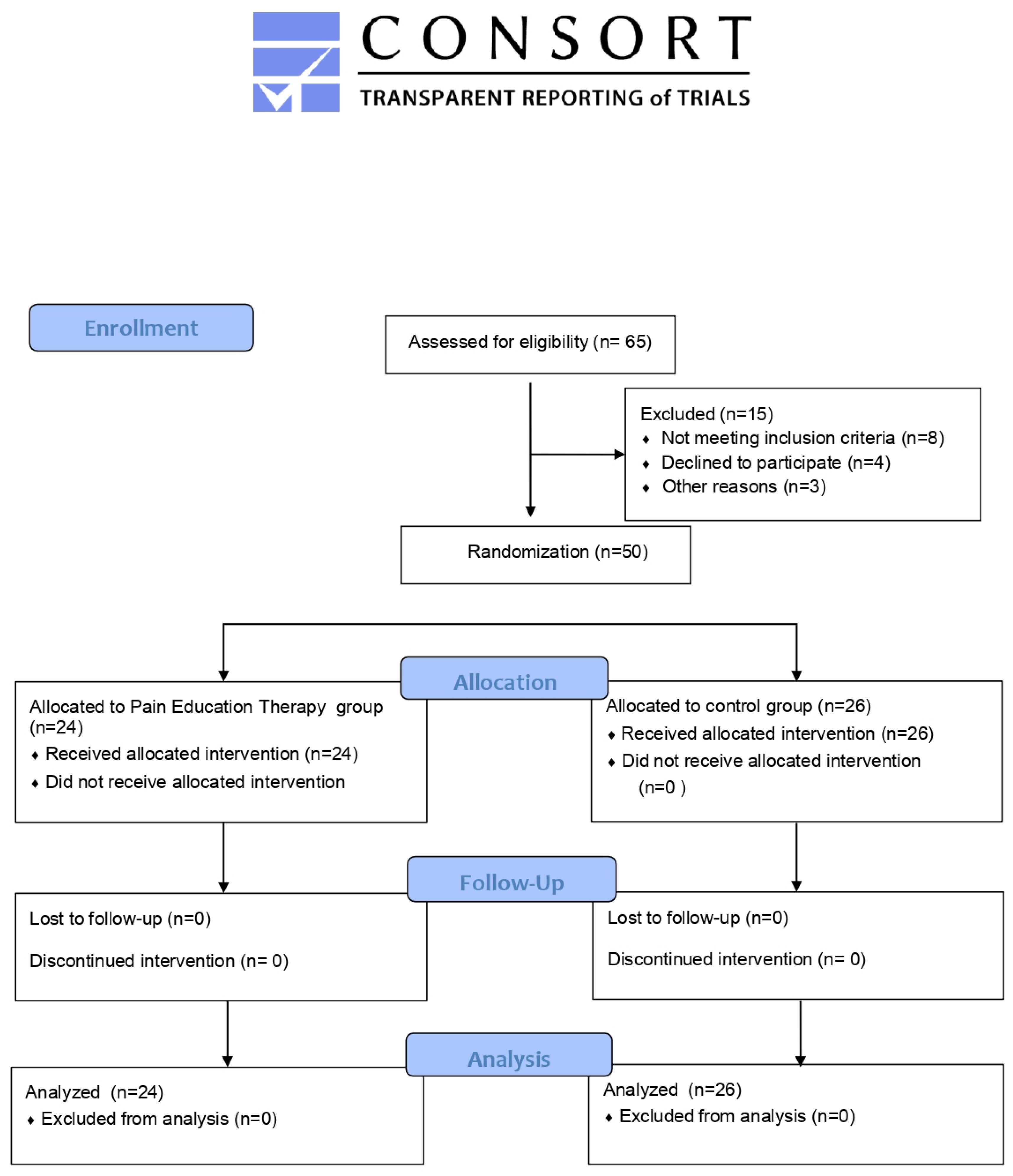
2.1. Study Design
2.2. Participants
2.3. Procedures
2.3.1. Experimental Sessions
2.3.2. Control Group
2.4. Outcomes
2.4.1. Pain Perception
2.4.2. Quality of Life
2.4.3. Catastrophism
2.4.4. Kinesiophobia
2.5. Statistical Analysis
3. Results
3.1. Participant Flow and Baseline Characteristics
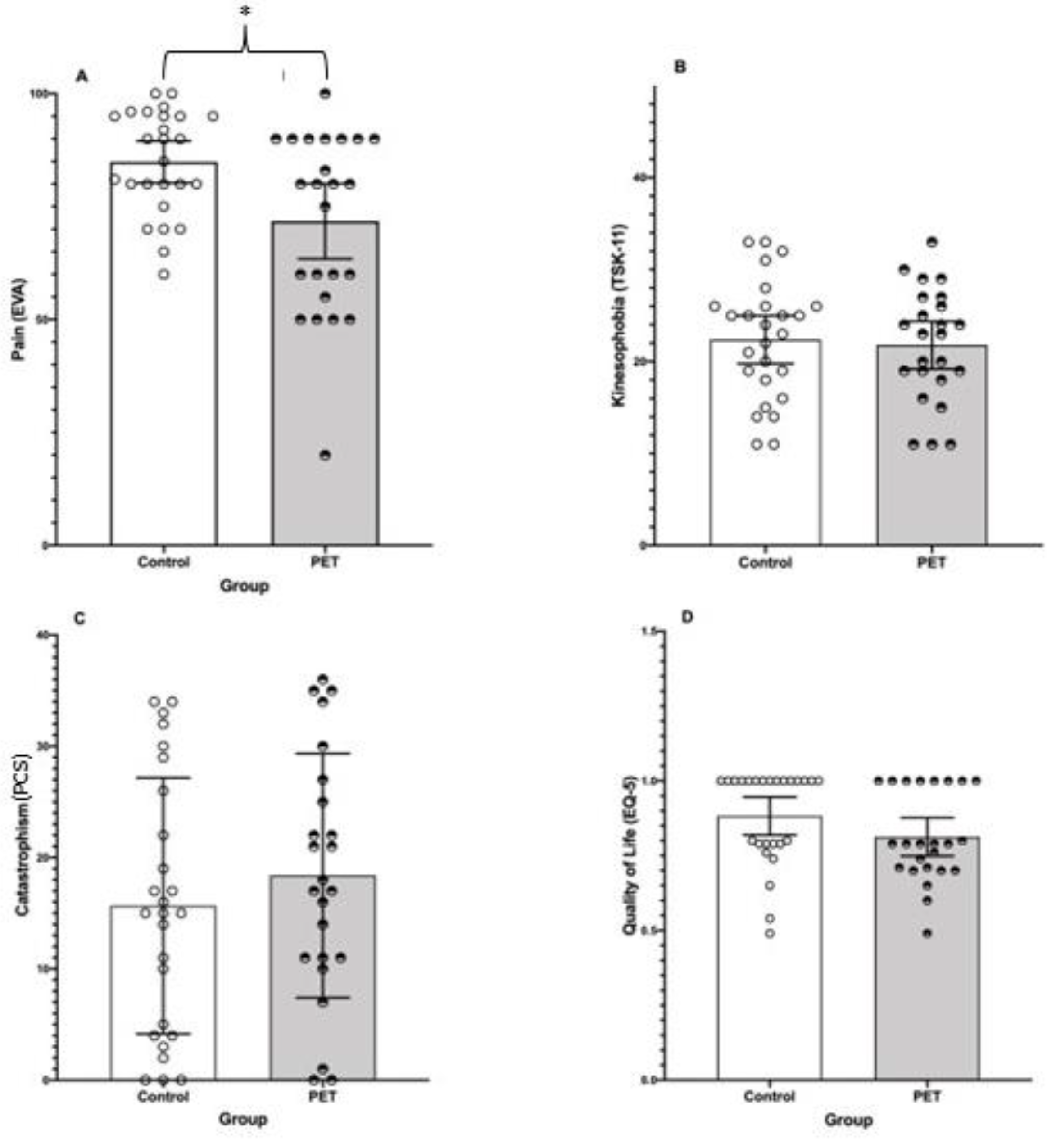
3.2. Effects of Intervention
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cesari, M.; Prince, M.; Thiyagarajan, J.A.; De Carvalho, I.A.; Bernabei, R.; Chan, P.; Gutierrez-Robledo, L.M.; Michel, J.-P.; Morley, J.E.; Ong, P. Frailty: An emerging public health priority. J. Am. Med. Dir. Assoc. 2016, 17, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Olimid, A.P.; Olimid, D.A. Societal Challenges, Population Trends and Human Security: Evidence from the Public Governance within the United Nations Publications (2015–2019). Rev. Stiinte Polit. 2019, 64, 53–64. [Google Scholar]
- Manini, T.M.; Clark, B.C. Dynapenia and aging: An update. J. Gerontol. Ser. Biomed. Sci. Med. Sci. 2012, 67, 28–40. [Google Scholar] [CrossRef]
- Larsson, C.; Hansson, E.E.; Sundquist, K.; Jakobsson, U. Chronic pain in older adults: Prevalence, incidence, and risk factors. Scand. J. Rheumatol. 2017, 46, 317–325. [Google Scholar] [CrossRef]
- Schwan, J.; Sclafani, J.; Tawfik, V.L. Chronic pain management in the elderly. Anesthesiol. Clin. 2019, 37, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Zhao, Y.; Xia, X.; Ge, N.; Yue, J. Association between frailty and chronic pain among older adults: A systematic review and meta-analysis. Eur. Geriatr. Med. 2020, 11, 945–959. [Google Scholar] [CrossRef]
- Sodhi, J.K.; Karmarkar, A.; Raji, M.; Markides, K.S.; Ottenbacher, K.J.; Al Snih, S. Pain as a predictor of frailty over time among older Mexican Americans. Pain 2020, 161, 109–113. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet Lond. Engl. 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Zis, P.; Daskalaki, A.; Bountouni, I.; Sykioti, P.; Varrassi, G.; Paladini, A. Depression and chronic pain in the elderly: Links and management challenges. Clin. Interv. Aging 2017, 12, 709. [Google Scholar] [CrossRef]
- Tegner, H.; Frederiksen, P.; Esbensen, B.A.; Juhl, C. Neurophysiological Pain Education for Patients with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Clin. J. Pain 2018, 34, 778–786. [Google Scholar] [CrossRef]
- Hylands-White, N.; Duarte, R.V.; Raphael, J.H. An overview of treatment approaches for chronic pain management. Rheumatol. Int. 2017, 37, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Marris, D.; Theophanous, K.; Cabezon, P.; Dunlap, Z.; Donaldson, M. The impact of combining pain education strategies with physical therapy interventions for patients with chronic pain: A systematic review and meta-analysis of randomized controlled trials. Physiother. Theory Pract. 2021, 37, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Zimney, K.; O’Hotto, C.; Hilton, S. The clinical application of teaching people about pain. Physiother. Theory Pract. 2016, 32, 385–395. [Google Scholar] [CrossRef]
- Moseley, L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust. J. Physiother. 2002, 48, 297–302. [Google Scholar] [CrossRef]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef]
- Zahari, Z.; Ishak, A.; Justine, M. The effectiveness of patient education in improving pain, disability and quality of life among older people with low back pain: A systematic review. J. Back Musculoskelet. Rehabil. 2020, 33, 245–254. [Google Scholar] [CrossRef]
- Kaye, A.D.; Baluch, A.; Scott, J.T. Pain management in the elderly population: A review. Ochsner J. 2010, 10, 179–187. [Google Scholar]
- Organización Mundial de la Salud. OMS Banco Mundial; Informe mundial sobre la discapacidad (Report on Disability in the World); Organización Mundial de la Salud: Valletta, Malta, 2011. [Google Scholar]
- Cramm, J.M.; Twisk, J.; Nieboer, A.P. Self-management abilities and frailty are important for healthy aging among community-dwelling older people; a cross-sectional study. BMC Geriatr. 2014, 14, 28. [Google Scholar] [CrossRef]
- Grant, S.; Mayo-Wilson, E.; Montgomery, P.; Macdonald, G.; Michie, S.; Hopewell, S.; Moher, D.; on behalf of the CONSORT-SPI Group. CONSORT-SPI 2018 Explanation and Elaboration: Guidance for reporting social and psychological intervention trials. Trials 2018, 19, 406. [Google Scholar] [CrossRef]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. The IASP classification of chronic pain for ICD-11: Chronic primary pain. Pain 2019, 160, 28–37. [Google Scholar] [CrossRef]
- Butler, D.; Moseley, L.; Torres Cueco, R.; Sunyata. Explaining Pain; Neuro Orthopaedic Institute, Noigroup Publications: Adelaide, Australia, 2010; ISBN 978-0-9750910-8-1. [Google Scholar]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test–retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 2018, 11, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Bijur, P.E.; Silver, W.; Gallagher, E.J. Reliability of the visual analog scale for measurement of acute pain. Acad. Emerg. Med. 2001, 8, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Gusi, N.; Badía, X.; Herdman, M.; Olivares, P.R. Traducción y adaptación cultural de la versión española del cuestionario EQ-5D-Y en niños y adolescentes (Spanish translation and cultural adaptation of the EQ-5D-Y ques-tionnaire for children and adolescents). Aten. Primaria 2009, 41, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Marten, O.; Brand, L.; Greiner, W. Feasibility of the EQ-5D in the elderly population: A systematic review of the literature. Qual. Life Res. 2022, 31, 1621–1637. [Google Scholar] [CrossRef]
- Badia, X.; Schiaffino, A.; Alonso, J.; Herdman, M. Using the EuroQoI 5-D in the Catalan general population: Feasibility and construct validity. Qual. Life Res. 1998, 7, 311–322. [Google Scholar] [CrossRef]
- Hernandez, G.; Garin, O.; Pardo, Y.; Vilagut, G.; Pont, A.; Suarez, M.; Neira, M.; Rajmil, L.; Gorostiza, I.; Ramallo-Farina, Y.; et al. Validity of the EQ-5D-5L and reference norms for the Spanish population. Qual. Life Res. 2018, 27, 2337–2348. [Google Scholar] [CrossRef]
- Rodero, B.; Alda, M.; Sobradiel, N.; Montero, J.; Moreno, S. Validation of the Spanish version of the Pain Catastrophizing Scale in fibromyalgia. Med. Clínica 2008, 131, 487–492. [Google Scholar]
- Morris, L.D.; Grimmer-Somers, K.A.; Spottiswoode, B.; Louw, Q.A. Virtual reality exposure therapy as treatment for pain catastrophizing in fibromyalgia patients: Proof-of-concept study (Study Protocol). BMC Musculoskelet. Disord. 2011, 12, 85. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Preuper, H.R.S.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef]
- Gómez-Pérez, L.; López-Martínez, A.E.; Ruiz-Párraga, G.T. Psychometric Properties of the Spanish Version of the Tampa Scale for Kinesiophobia (TSK). J. Pain 2011, 12, 425–435. [Google Scholar] [CrossRef]
- Tkachuk, G.A.; Harris, C.A. Psychometric Properties of the Tampa Scale for Kinesiophobia-11 (TSK-11). J. Pain 2012, 13, 970–977. [Google Scholar] [CrossRef] [PubMed]
- Larsson, C.; Hansson, E.E.; Sundquist, K.; Jakobsson, U. Psychometric properties of the Tampa Scale of Kinesiophobia (TSK-11) among older people with chronic pain. Physiother. Theory Pract. 2014, 30, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G. A Scale of Magnitudes for Effect Statistics: A New View of Statistics. 2002. Available online: http://www.sportsci.org/resource/stats/effectmag.html (accessed on 3 February 2022).
- Sillevis, R.; Trincado, G.; Shamus, E. The immediate effect of a single session of pain neuroscience education on pain and the autonomic nervous system in subjects with persistent pain, a pilot study. PeerJ 2021, 9, e11543. [Google Scholar] [CrossRef]
- Rufa, A.; Beissner, K.; Dolphin, M. The use of pain neuroscience education in older adults with chronic back and/or lower extremity pain. Physiother. Theory Pract. 2019, 35, 603–613. [Google Scholar] [CrossRef]
- Gatchel, R.J.; Haggard, R.; Thomas, C.; Howard, K.J. Biopsychosocial approaches to understanding chronic pain and disability. In Handbook of Pain and Palliative Care; Springer: Berlin/Heidelberg, Germany, 2018; pp. 3–22. [Google Scholar]
- Amer-Cuenca, J.J.; Pecos-Martín, D.; Martínez-Merinero, P.; Lluch Girbés, E.; Nijs, J.; Meeus, M.; Ferrer Peña, R.; Fernández-Carnero, J. How Much Is Needed? Comparison of the Effectiveness of Different Pain Education Dosages in Patients with Fibromyalgia. Pain Med. Malden Mass 2020, 21, 782–793. [Google Scholar] [CrossRef]
- Yildirim, Y.K.; Cicek, F.; Uyar, M. Effects of pain education program on pain intensity, pain treatment satisfaction, and barriers in Turkish cancer patients. Pain Manag. Nurs. 2009, 10, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L.; Butler, D.S. Fifteen Years of Explaining Pain: The Past, Present, and Future. J. Pain 2015, 16, 807–813. [Google Scholar] [CrossRef]
- Tavafian, S.S.; Jamshidi, A.; Mohammad, K.; Montazeri, A. Low back pain education and short term quality of life: A randomized trial. BMC Musculoskelet. Disord. 2007, 8, 21. [Google Scholar] [CrossRef]
- Brandauer, A.; Berger, S.; Freywald, N.; Gnass, I.; Osterbrink, J.; Seidenspinner, D.; Kutschar, P. Quality of life in nursing home residents with pain: Pain interference, depression and multiple pain-related diseases as important determinants. Qual. Life Res. 2020, 29, 91–97. [Google Scholar] [CrossRef]
- Putri Mellaratna, W.; Jusuf, N.K.; Yosi, A. The impact of pain intensity on quality of life of postherpetic neuralgia patients. Med. Glas. 2020, 17, 439–444. [Google Scholar] [CrossRef]
- Fatoye, F.; Palmer, S.; Macmillan, F.; Rowe, P.; van der Linden, M. Pain intensity and quality of life perception in children with hypermobility syndrome. Rheumatol. Int. 2012, 32, 1277–1284. [Google Scholar] [CrossRef] [PubMed]
- Lautenbacher, S. Experimental approaches in the study of pain in the elderly. Pain Med. Malden Mass 2012, 13 (Suppl. S2), S44–S50. [Google Scholar] [CrossRef] [PubMed]
- Gunendi, Z.; Eker, D.; Tecer, D.; Karaoglan, B.; Ozyemisci-Taskiran, O. Is the word “osteoporosis” a reason for kinesiophobia? Eur. J. Phys. Rehabil. Med. 2018, 54, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, P.; Zeppieri, G.; Bialosky, J.; Bocchino, C.; van den Boogaard, J.; Tillman, S.; Chmielewski, T.L. Kinesiophobia and Its Association With Health-Related Quality of Life Across Injury Locations. Arch. Phys. Med. Rehabil. 2018, 99, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Beltran-Alacreu, H.; López-de-Uralde-Villanueva, I.; Fernández-Carnero, J.; La Touche, R. Manual Therapy, Therapeutic Patient Education, and Therapeutic Exercise, an Effective Multimodal Treatment of Nonspecific Chronic Neck Pain: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2015, 94 (Suppl. S1), 887–897. [Google Scholar] [CrossRef]
- Leung, L. Pain Catastrophizing: An Updated Review. Indian J. Psychol. Med. 2012, 34, 204–217. [Google Scholar] [CrossRef]
- Gallagher, L.; McAuley, J.; Moseley, G.L. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin. J. Pain 2013, 29, 20–25. [Google Scholar] [CrossRef]
- Bodes Pardo, G.; Lluch Girbés, E.; Roussel, N.A.; Gallego Izquierdo, T.; Jiménez Penick, V.; Pecos Martín, D. Pain Neurophysiology Education and Therapeutic Exercise for Patients With Chronic Low Back Pain: A Single-Blind Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2018, 99, 338–347. [Google Scholar] [CrossRef]
- Main, C.J.; Foster, N.; Buchbinder, R. How important are back pain beliefs and expectations for satisfactory recovery from back pain? Best Pract. Res. Clin. Rheumatol. 2010, 24, 205–217. [Google Scholar] [CrossRef]
- Calzone, K.A.; Prindiville, S.A.; Jourkiv, O.; Jenkins, J.; DeCarvalho, M.; Wallerstedt, D.B.; Liewehr, D.J.; Steinberg, S.M.; Soballe, P.W.; Lipkowitz, S.; et al. Randomized comparison of group versus individual genetic education and counseling for familial breast and/or ovarian cancer. J. Clin. Oncol. 2005, 23, 3455–3464. [Google Scholar] [CrossRef]
- de Carvalho Torres, H.; Franco, L.J.; Stradioto, M.A.; Hortale, V.A.; Schall, V.T. Evaluation of group and individual strategies in a diabetes education program. Rev. Saude Publica 2009, 43, 291–298. [Google Scholar] [CrossRef]
- Dalmau Llorca, M.R.; García Bernal, G.; Aguilar Martín, C.; Palau Galindo, A. Group versus individual education for type-2 diabetes patients. Aten. Primaria 2003, 32, 36–41. [Google Scholar] [CrossRef]
- Gokhale, A.; Yap, T.; Heaphy, N.; McCullough, M.J. Group pain education is as effective as individual education in patients with chronic temporomandibular disorders. J. Oral Pathol. Med. 2020, 49, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen-Barr, E.; Nilsson-Wikmar, L.; Arvidsson, I. Stabilizing training compared with manual treatment in sub-acute and chronic low-back pain. Man. Ther. 2003, 8, 233–241. [Google Scholar] [CrossRef]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Birney, D.P.; Beckmann, J.F.; Beckmann, N.; Double, K.S. Beyond the intellect: Complexity and learning trajectories in Raven’s Progressive Matrices depend on self-regulatory processes and conative dispositions. Intelligence 2017, 61, 63–77. [Google Scholar] [CrossRef]
| Topic | Type of Topic | Week |
|---|---|---|
| Topic 1 | Acute vs. chronic Pain | Week 1 |
| Topic 2 | Acute Pain Physiology: nociception process | Week 2 |
| Topic 3 | Pain Chronification Processes I: peripheral sensitization | Week 3 |
| Topic 4 | Pain Chronification Processes II: central sensitization | Week 4 |
| Topic 5 | Chronic Pain Neurophysiology: neuromatrix theory | Week 5 |
| Topic 6 | Pain Dimensions: emotional, psychological, and social factors | Week 6 |
| PET (n = 24) | CG (n = 26) | |
|---|---|---|
| Age (years) | 75.79 ± 5.92 | 74.07 ± 6.27 |
| Body Mass (kg) | 66.37 ± 14.56 | 68.12 ± 8.76 |
| Height (cm) | 161 ± 6.12 | 159.23 ± 5.48 |
| Participants without co-morbidities or minor disorders otherwise from pain | 4 | 5 |
| Participants with co-morbidities | 20 | 21 |
| Co-morbidities, % (n): | ||
| Diabetes | 6 (23%) | 4 (15%) |
| Hypertension | 9 (34%) | 8 (30%) |
| Hypercholesterolemia | 15 (57%) | 10 (38%) |
| Arthrosis | 2 (7%) | 1 (3%) |
| Others (prostatitis, rheumatoid arthritis, hypothyroidism, lymphoproliferative syndrome, heart disease, breast carcinoma) | 1 (3%) | 7 (26%) |
| Pain medication use: | ||
| Any pain medication use | 23 (96%) | 22 (84%) |
| Paracetamol | 1 | 2 |
| Ibuprofen | 0 | 1 |
| Other Analgesics | 0 | 1 |
| n (F/M) | Pain (VAS) # | Quality of Life (EQ-5D) | Kinesiophobia (TSK-11) | Catastrophism (PSC) | |
|---|---|---|---|---|---|
| PET | 24 (14/12) | 71.79 (19.72) * | 0.81 (0.15) | 21.79 (6.15) | 18.38 (10.97) |
| CG | 26 (13/13) | 84.89 (11.49) | 0.88 (0.16) | 22.39 (6.44) | 15.65 (11.51) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vicente-Mampel, J.; Gargallo, P.; Bautista, I.J.; Blanco-Gímenez, P.; de Bernardo Tejedor, N.; Alonso-Martín, M.; Martínez-Soler, M.; Baraja-Vegas, L. Impact of Pain Neuroscience Education Program in Community Physiotherapy Context on Pain Perception and Psychosocial Variables Associated with It in Elderly Persons: A Ranzomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 11855. https://doi.org/10.3390/ijerph191911855
Vicente-Mampel J, Gargallo P, Bautista IJ, Blanco-Gímenez P, de Bernardo Tejedor N, Alonso-Martín M, Martínez-Soler M, Baraja-Vegas L. Impact of Pain Neuroscience Education Program in Community Physiotherapy Context on Pain Perception and Psychosocial Variables Associated with It in Elderly Persons: A Ranzomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(19):11855. https://doi.org/10.3390/ijerph191911855
Chicago/Turabian StyleVicente-Mampel, Juan, Pedro Gargallo, Iker Javier Bautista, Paula Blanco-Gímenez, Nieves de Bernardo Tejedor, Mónica Alonso-Martín, Marta Martínez-Soler, and Luis Baraja-Vegas. 2022. "Impact of Pain Neuroscience Education Program in Community Physiotherapy Context on Pain Perception and Psychosocial Variables Associated with It in Elderly Persons: A Ranzomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 19: 11855. https://doi.org/10.3390/ijerph191911855
APA StyleVicente-Mampel, J., Gargallo, P., Bautista, I. J., Blanco-Gímenez, P., de Bernardo Tejedor, N., Alonso-Martín, M., Martínez-Soler, M., & Baraja-Vegas, L. (2022). Impact of Pain Neuroscience Education Program in Community Physiotherapy Context on Pain Perception and Psychosocial Variables Associated with It in Elderly Persons: A Ranzomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(19), 11855. https://doi.org/10.3390/ijerph191911855






