Factors That Foster Therapeutic Alliance in Pediatric Sports and Orthopedics: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Searches
2.2. Participants
2.3. Operational Definitions
2.4. Study Selection
2.5. Data Extraction
2.6. Quality Assessment
3. Results
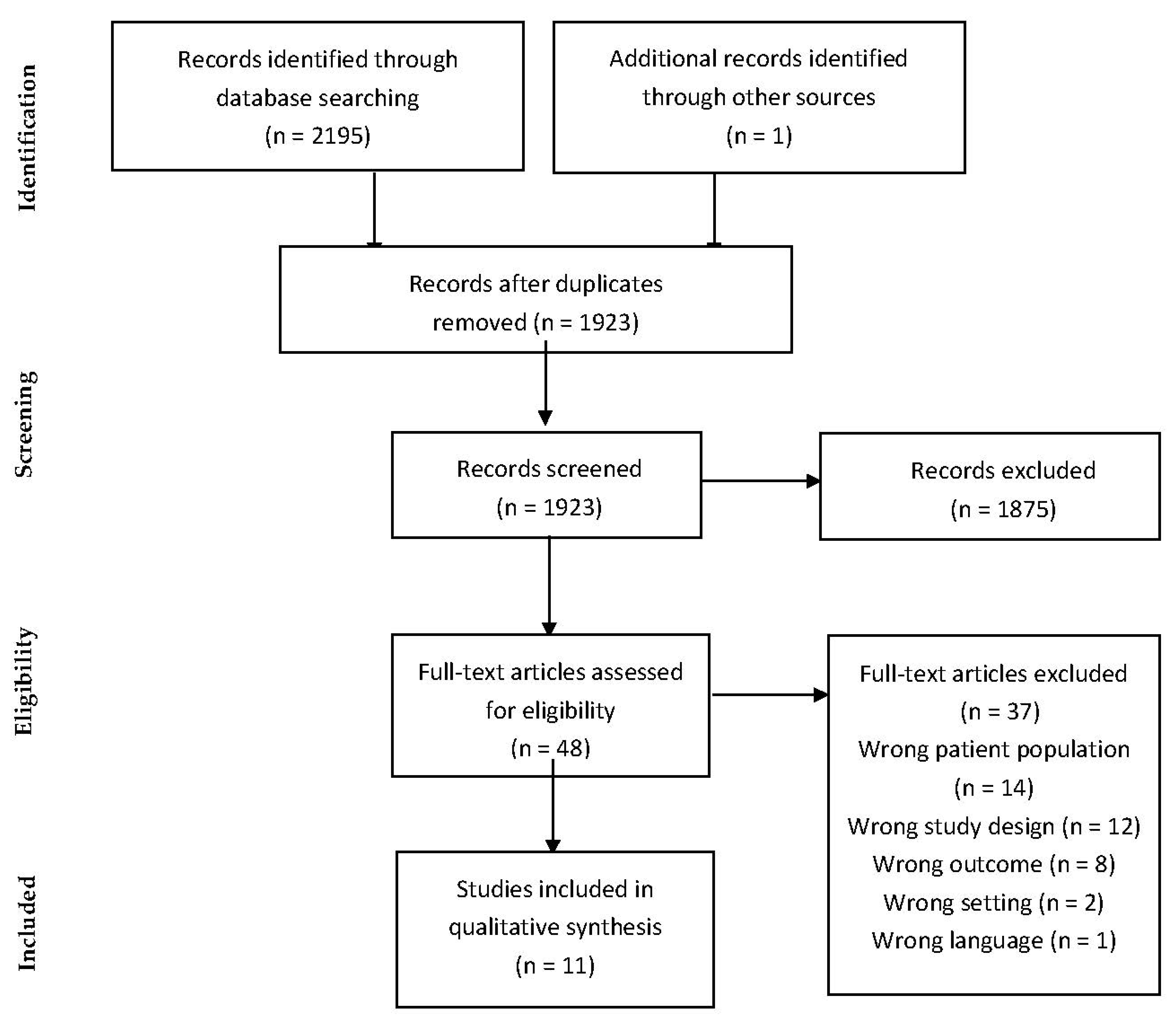
3.1. Study Selection
3.2. Study Characteristics
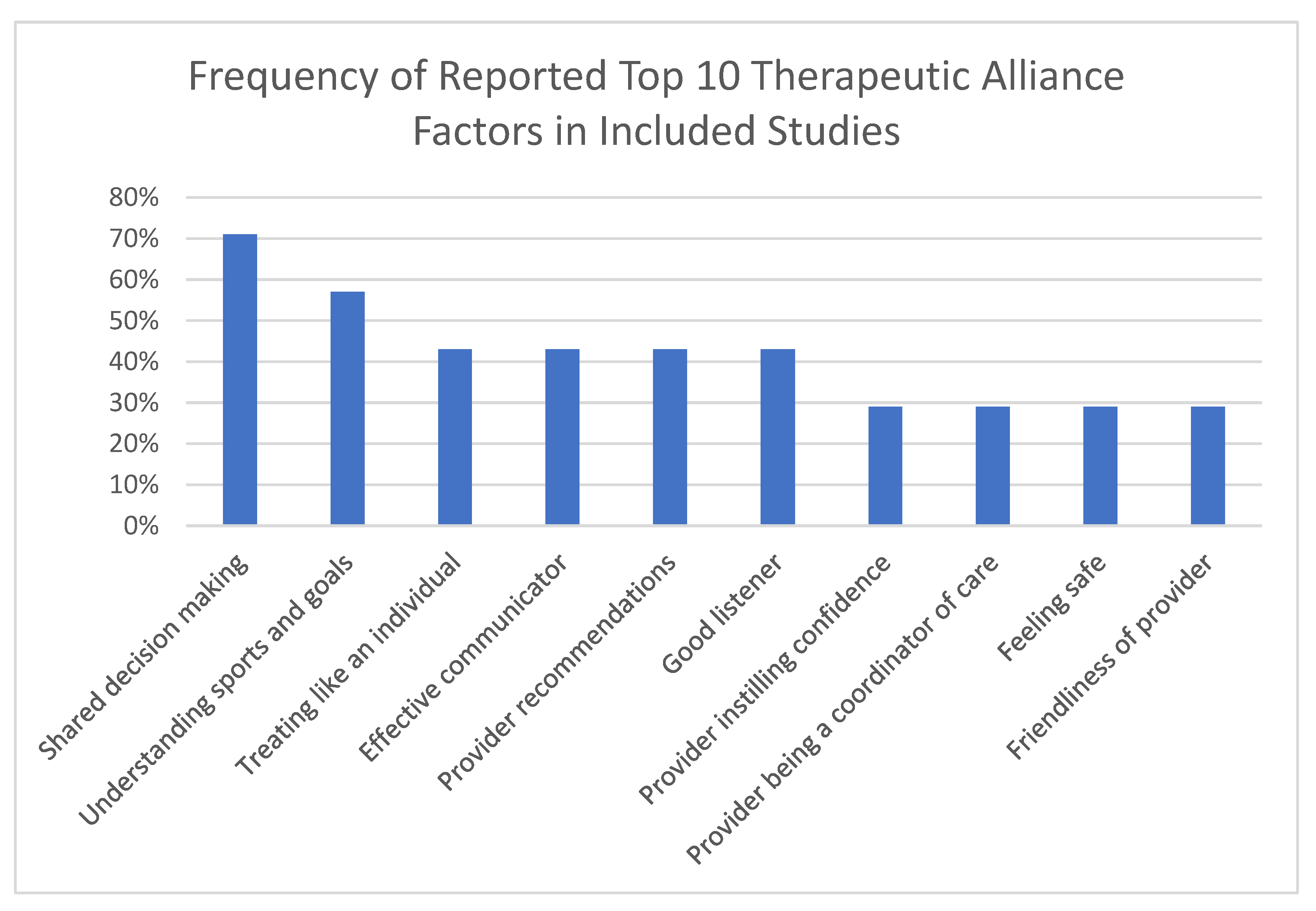
3.3. Factors Associated with Therapeutic Alliance
3.3.1. Patient Perspective
| Study | Study Design, ROB Score | Outcome Measure | Provider | Patient Perspective | Parent Perspective | Telehealth | Factors |
|---|---|---|---|---|---|---|---|
| Beck et al., 2019 [20] | Cross-sectional, 12 | Survey | Surgeon | x | x | Shared decision making Understanding sports and goals Treating like an individual Provider recommendations Good listener Provider sex Demonstrates assertiveness Demonstrates compassion | |
| Paterno et al., 2019 [26] | Qualitative, 7 | Interview | PT | x | x | Provider instilling confidence Provider being a coordinator of care Provider being a guide Provider being a motivator | |
| Allison et al., 2022 [21] | Cross-sectional, 12 | TSUQ, WAI | Physician | x | x | x | Having a pre-established relationship with provider |
| Elbin et al., 2021 [28] | Randomized prospective, 16 | TASCP, TASC-R | Physician | x | x | x | In-person visits for parents |
| Beck et al., 2021 [29] | Prospective cohort, 12 | Survey | Physician | x | x | Shared decision making Understanding goals Treating like an individual Provider recommendations Good listener Physician schooling | |
| Peng et al., 2018 [22] | Cross-sectional, 8 | Survey | Orthopedic team | x | Shared decision making Effective communicator Provider recommendations | ||
| Singleton et al., 2021 [23] | Cross-sectional, 13 | CARE measure | Physician | x | Empathy | ||
| Singleton et al., 2022 [19] | Cross-sectional, 12 | CARE measure | Physician | x | Good listener Respect for caregiver’s thoughts | ||
| Adado et al., 2021 [24] | Cross-sectional, 10 | PCC model | Orthopedic team | x | Shared decision making Understanding patient’s needs and goals Being an effective communicator and educator Being a coordinator of care Making the child feel safe and comfortable Provide emotional support to the child Involving the child’s support system in the plan of care Setting up a continuing care plan after each visit | ||
| Hanna et al., 2021 [25] | Cross-sectional, 13 | PSQ, TUQ | Surgeon | x | x | Treatment time > 30 min English-speaking provider for English-speaking patients | |
| VanEtten et al., 2021 [27] | Case report, NA | Stages technique | PT | x | Shared decision making Congruence in goals Treating like an individual Effective communicator Connectedness/friendliness Giving clear expectations of recovery Establishing roles and responsibilities |
3.3.2. Male vs. Female Patient Perspective
3.4. Parent Perspective
3.5. Race and Socioeconomic Status Perspective
3.6. Differences among Healthcare Providers
3.7. Therapeutic Alliance Regarding Telehealth vs. In-Person
| Factors Positively Associated with Therapeutic Alliance in Telehealth | ||
|---|---|---|
| Having an already established relationship with the provider (Allison et al., 2021 [21]) | Treatment time > 30 min (Hanna et al., 2021 [25]) | English-speaking provider (Hanna et al., 2021 [25]) |
3.8. Risk of Bias
4. Discussion
4.1. Patient Perspective
4.2. Male vs. Female Patient Perspective
4.3. Parent Perspective
4.4. Race and Socioeconomic Status Perspective
4.5. Differences among Healthcare Providers
4.6. Therapeutic Alliance Regarding Telehealth vs. In-Person
4.7. Limitations
4.8. Future Directions
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Luke, A.; Lazaro, R.M.; Bergeron, M.F.; Keyser, L.; Benjamin, H.; Brenner, J.; d’Hemecourt, P.; Grady, M.; Philpott, J.; Smith, A. Sports-related injuries in youth athletes: Is overscheduling a risk factor? Clin. J. Sports Med. 2011, 21, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Adirim, T.A.; Cheng, T.L. Overview of Injuries in the Young Athlete. Sports Med. 2003, 33, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.R.; Yamasaki, A.; Brown, K. Epidemiology of sports-related musculoskeletal injuries in young athletes in United States. Transl. Pediatrics 2017, 6, 160–166. [Google Scholar] [CrossRef]
- Merkel, D. Youth sport: Positive and negative impact on young athletes. Open Access J. Sports Med. 2013, 4, 151–160. [Google Scholar] [CrossRef]
- Micheli, L.J.; Glassman, R.; Klein, M. The prevention of sports injuries in children. Clin. Sports Med. 2000, 19, 821–834. [Google Scholar] [CrossRef]
- Kinney, M.; Seider, J.; Beaty, A. The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2020, 36, 886–898. [Google Scholar] [CrossRef]
- Ackerman, S.J.; Hilsenroth, M.J. A review of therapist characteristics and techniques positively impacting the therapeutic alliance. Clin. Psychol. Rev. 2003, 23, 1–33. [Google Scholar] [CrossRef]
- Horvath, A.O.; Luborsky, L. The role of the therapeutic alliance in psychotherapy. J. Consult. Clin. Psychol. 1993, 61, 561–573. [Google Scholar] [CrossRef]
- Hall, A.M.; Ferreira, P.H.; Maher, C.; Latimer, J.; Ferreira, M.L. The Influence of the Therapist-Patient Relationship on Treatment Outcome in Physical Rehabilitation: A Systematic Review. Phys. Ther. 2010, 90, 1099–1110. [Google Scholar] [CrossRef]
- Diener, I.; Kargela, M.; Louw, A. Listening is therapy: Patient interviewing from a pain science perspective. Physiother. Theory Pract. 2016, 32, 356–367. [Google Scholar] [CrossRef]
- George, S.I. What is the effectiveness of a biopsychosocial approach to individual physiotherapy care for chronic low back pain? Internet J. Allied Health Sci. Pract. 2008, 6, 1–10. [Google Scholar] [CrossRef]
- Charmant, W.M.; van der Wees, P.J.; Staal, J.B.; van Cingel, R.; Sieben, J.M.; de Bie, R.A. A framework exploring the therapeutic alliance between elite athletes and physiotherapists: A qualitative study. BMC Sports Sci. Med. Rehabil. 2021, 13, 122. [Google Scholar] [CrossRef] [PubMed]
- Kaye, E.C.; Rockwell, S.; Woods, C.; Lemmon, M.E.; Andes, K.; Baker, J.N.; Mack, J.W. Facilitators associated with building and sustained therapeutic alliance in advanced pediatric cancer. JAMA Netw. Open 2021, 4, e2120925. [Google Scholar] [CrossRef] [PubMed]
- Van Benthem, P.; Spijkerman, R.; Blanken, P.; Kleinjan, M.; Vermeiren, R.R.J.M.; Hendriks, V.M. A dual perspective on first-session therapeutic alliance: Strong predictor of youth mental health and addiction treatment outcome. Eur. Child Adolesc. Psychiatry 2020, 29, 1593–1601. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.E.; Ethier, K.A.; Hertz, M.; DeGue, S.; Le, V.D.; Thornton, J.; Lim, C.; Dittus, P.J.; Geda, S. Mental health, suicidality, and connectedness among high school students during the covid-19 pandemic—Adolescent behaviors and experiences survey, United States, January–June 2021. MMWR Suppl. 2022, 71, 16–21. [Google Scholar] [CrossRef]
- Bordin, E.S. The generalizability of the psychoanalytic concept of the working alliance. Psychother. Theory Res. Pract. 1979, 16, 252–260. [Google Scholar] [CrossRef]
- Gimigliano, F.; Resmini, G.; Moretti, A.; Aulicino, M.; Gargiulo, F.; Gimigliano, A.; Liguori, S.; Paoletta, M.; Iolascon, G. Epidiology of musculoskeletal injuries in adult athletes: A scoping review. Medicina 2021, 57, 1118. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of healthcare interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Singleton, I.M.; Garfinkel, R.J.; Malone, J.B.; Temkit, M.H.; Belthur, M.V. Perceived Physician Empathy in Pediatric Orthopedics: A Cross-Sectional Study. J. Patient Exp. 2022, 9, 1–6. [Google Scholar] [CrossRef]
- Beck, J.; Murray, M.; Christino, M. Clinical approach in youth sports medicine: Patients’ and guardians’ desired characteristics in sports medicine surgeons. J. Am. Acad. Orthop. Surg. 2019, 27, 479–485. [Google Scholar] [CrossRef]
- Allison, B.A.; Rea, S.; Mikesell, L.; Perry, M.F. Adolescent and Parent Perceptions of Telehealth Visits: A Mixed-Methods Study. J. Adolesc. Health 2022, 70, 403–413. [Google Scholar] [CrossRef]
- Peng, F.; Burrows, J.; Shirley, E.; Rosen, P. Unlocking the doors to patient satisfaction in pediatric orthopedics. J. Pediatric Orthop. 2018, 38, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Singleton, I.; Garfinkel, R.; Malone, J.; Temkit, M.H.; Belthur, M.V. Determinants of caregiver satisfaction in pediatric orthopedics. J. Pediatric Orthop. 2021, 30, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Adado, S.R.; Games, K.E. Parental Perceptions of the Importance and Effectiveness of Patient-Centered Care Delivery. Int. J. Athl. Ther. Train. 2021, 26, 326–331. [Google Scholar] [CrossRef]
- Hanna, G.; Siddiqui, B.; Jernigan, E.; Edobor-Osula, F. Telemedicine for pediatric orthopedic visits: Evaluating usability and satisfaction. J. Pediatric Orthop. 2022, 31, e75–e80. [Google Scholar] [CrossRef]
- Paterno, M.; Schmitt, L.; Thomas, S.; Duke, N.; Russo, R.; Quatman-Yates, C.C. Patient and parent perspectives of rehabiliatation factors that influence outcomes after anterior cruciate ligament reconstruction and clearance to return to sport in adolescents and young adults. J. Orthop. Sports Phys. Ther. 2019, 49, 576–583. [Google Scholar] [CrossRef]
- VanEtten, L.; Briggs, M.; DeWitt, J.; Mansfield, C.; Kaeding, C. The Implementation of Therapeutic Alliance in the Rehabilitation of an Elite Pediatric Athlete with Salter-Harris Fracture: A Case Report. Int. J. Sports Phys. Ther. 2021, 16, 539–551. [Google Scholar] [CrossRef]
- Elbin, R.J.; Stephenson, K.; Lipinski, D.; Maxey, K.; Womble, M.N.; Reynolds, E.; Covert, K.; Kontos, A.P. In-person versus telehealth for concussion clinical care in adolescents: A pilot study of therapeutic alliance and patient satisfaction. J. Head Trauma Rehabil. 2021, 37, 213–219. [Google Scholar] [CrossRef]
- Beck, J.; West, N.; Jackson, N.; Willimon, S.C.; Busch, M.T.; Christino, M.A. Gender and socioeconomic factors affect adolescent patient and guardian preferences in sports medicine physician characteristics and medical decision making. J. Am. Acad. Orthop. Surg. 2021, 5, 1–7. [Google Scholar] [CrossRef]
- Silverman, S.R.; Schertz, L.A.; Yuen, H.K.; Lowman, J.D.; Bickel, C.S. Systematic review of the methodological quality and outcome measures utilized in exercise interventions for adults with spinal cord injury. Spinal Cord 2012, 50, 718–727. [Google Scholar] [CrossRef]
- Pinto, R.; Ferreira, M.; Oliveira, V.; Franco, M.R.; Adams, R.; Maher, C.G.; Ferreira, P.H. Patient-centered communication is associated with positive therapeutic alliance: A systematic review. J. Physiother. 2012, 58, 77–87. [Google Scholar] [CrossRef]
- Jacobson, L.; Richardson, G.; Parry-Langdon, N. How do teenagers and primary healthcare providers view each other? An overview of key themes. Br. J. Gen. Pract. 2001, 51, 811–816. [Google Scholar] [PubMed]
- Jacobson, L.; Wilkinson, C.; Pill, R.; Hackett, P. Communication between teenagers and British general practitioners: A preliminary study of the teenage perspective. Ambul. Child Health 1996, 1, 291–301. [Google Scholar]
- Lephart, S.M.; Abt, J.P.; Ferris, C.M. Neuromuscular contributions to anterior cruciate ligament injuries in females. Curr. Opin. Rheumatol. 2002, 14, 168–173. [Google Scholar] [CrossRef]
- Lephart, S.M.; Abt, J.P.; Ferris, C.M.; Sell, T.C.; Nagai, T.; Myers, J.B.; Irrgang, J.J. Neuromuscular and biomechanical characteristic changes in high school athletes: A plyometric versus basic resistance program. Br. J. Sports Med. 2005, 39, 932–938. [Google Scholar] [CrossRef]
- Beischer, S.; Gustavsson, L.; Senorski, E.H.; Karlsson, J.; Thomeé, C.; Samuelsson, K.; Thomeé, R. Young Athletes Who Return to Sport Before 9 Months After Anterior Cruciate Ligament Reconstruction Have a Rate of New Injury 7 Times That of Those Who Delay Return. J. Orthop. Sports Phys. Ther. 2020, 50, 83–90. [Google Scholar] [CrossRef]
- Kelsey, J.; Abelson-Mitchell, N.; Skirton, H. Perceptions of young people about decision making in the acute healthcare environment. Nurs. Child. Young People 2007, 19, 14–18. [Google Scholar] [CrossRef]
- Fabien, C.; Crossman, J.; Jamieson, J. Injured athletes’ perceptions of the social support provided by their coaches and teammates during rehabilitation. J. Sport Behav. 2008, 31, 93–107. [Google Scholar]
- Kapphahn, C.; Wilson, K.; Klein, J.D. Adolescent girls’ and boys’ preferences for provider gender and confidentiality in their health care. J. Adolesc. Health 1999, 25, 131–142. [Google Scholar] [CrossRef]
- Koonin, L.; Hoots, B.; Tsang, C. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. MMWR Morb. Mortal. Wkly Rep. 2020, 69, 1595–1599. [Google Scholar] [CrossRef]
- Tenforde, A.S.; Iaccarino, M.A.; Borgstrom, H.; Hefner, J.E.; Silver, J.; Ahmed, M.; Babu, A.N.; Blauwet, C.A.; Elson, L.; Eng, C.; et al. Telemedicine during COVID-19 for outpatient sports and musculoskeletal medicine physicians. PM&R J. 2020, 12, 926–932. [Google Scholar]
- Atanda, A.; Pelton, M.; Fabricant, P.; Tucker, A.; Shah, S.A.; Slamon, N. Telemedicine utilization in a paediatric sports medicine practice: Decreased cost and wait times with increased satisfaction. J. ISAKOS 2018, 3, 94–97. [Google Scholar] [CrossRef]
- Ramani, S. Promoting the art of history taking. Med. Teach. 2004, 26, 374–376. [Google Scholar] [CrossRef]
- Ramsey, P.G.; Curtis, J.; Paauw, D.S.; Carline, J.D.; Wenrich, M.D. History-taking and Preventive Medicine Skills among Primary Care Physicians: An Assessment Using Standardized Patients. Am. J. Med. 1998, 104, 152–158. [Google Scholar] [CrossRef]
- Acheson, L.S.; Wiesner, G.L.; Zyzanski, S.J.; Goodwin, M.A.; Stange, K.C. Family history-taking in community family practice: Implications for genetic screening. Genet. Med. 2000, 2, 180–185. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meyers, R.N.; McHugh, R.B.; Conde, A.M. Factors That Foster Therapeutic Alliance in Pediatric Sports and Orthopedics: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 11813. https://doi.org/10.3390/ijerph191811813
Meyers RN, McHugh RB, Conde AM. Factors That Foster Therapeutic Alliance in Pediatric Sports and Orthopedics: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(18):11813. https://doi.org/10.3390/ijerph191811813
Chicago/Turabian StyleMeyers, Rachel N., Robyn B. McHugh, and Alissa M. Conde. 2022. "Factors That Foster Therapeutic Alliance in Pediatric Sports and Orthopedics: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 18: 11813. https://doi.org/10.3390/ijerph191811813
APA StyleMeyers, R. N., McHugh, R. B., & Conde, A. M. (2022). Factors That Foster Therapeutic Alliance in Pediatric Sports and Orthopedics: A Systematic Review. International Journal of Environmental Research and Public Health, 19(18), 11813. https://doi.org/10.3390/ijerph191811813






