The Association between Hand Disinfection Techniques and Their Barriers, as Well as the “Bare below the Elbows” Concept, among Healthcare Professionals—A Study Based on a Polish Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Experimental Methods
2.3. Ethical Statement
2.4. Statistics
3. Results
3.1. Participant Characteristics
3.2. Hand Hygiene—Assessment of the Correctness of Hand Disinfection Procedures
3.3. Risk Factor Determination—Assessment of Hand Preparation and Disinfection Procedure Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care; WHO Guidelines Approved by the Guidelines Review Committee; WHO: Geneva, Switzerland, 2009.
- Boyce, J.M.; Potter-Bynoe, G.; Opal, S.M.; Dziobek, L.; Medeiros, A.A. A common-source outbreak of Staphylococcus epidermidis infections among patients undergoing cardiac surgery. J. Infect. Dis. 1990, 161, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Pittet, D.; Allegranzi, B.; Sax, H.; Dharan, S.; Pessoa-Silva, C.L.; Donaldson, L.; Boyce, J.M.; Who Global Patient Safety Challenge, W.A.f.P.S. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect. Dis. 2006, 6, 641–652. [Google Scholar] [CrossRef]
- Jumaa, P.A. Hand hygiene: Simple and complex. Int. J. Infect. Dis. 2005, 9, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Widmer, A.F.; Conzelmann, M.; Tomic, M.; Frei, R.; Stranden, A.M. Introducing alcohol-based hand rub for hand hygiene: The critical need for training. Infect. Control Hosp. Epidemiol. 2007, 28, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.M. Update on hand hygiene. Am. J. Infect. Control 2013, 41, S94–S96. [Google Scholar] [CrossRef] [PubMed]
- Hautemaniere, A.; Cunat, L.; Diguio, N.; Vernier, N.; Schall, C.; Daval, M.C.; Ambrogi, V.; Tousseul, S.; Hunter, P.R.; Hartemann, P. Factors determining poor practice in alcoholic gel hand rub technique in hospital workers. J. Infect. Public Health 2010, 3, 25–34. [Google Scholar] [CrossRef]
- Pratt, R.J.; Pellowe, C.M.; Wilson, J.A.; Loveday, H.P.; Harper, P.J.; Jones, S.R.; McDougall, C.; Wilcox, M.H. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J. Hosp. Infect. 2007, 65, S1–S64. [Google Scholar] [CrossRef]
- Gupta, M.K.; Lipner, S.R. Hand hygiene in preventing COVID-19 transmission. Cutis 2020, 105, 233–234. [Google Scholar] [PubMed]
- Dancer, S.G.; Duerden, B.I. Changes to clinician attire have done more harm than good. J. R. Coll. Physicians Edinb. 2014, 44, 293–298. [Google Scholar] [CrossRef]
- Farrington, R.M.; Rabindran, J.; Crocker, G.; Ali, R.; Pollard, N.; Dalton, H.R. ‘Bare below the elbows’ and quality of hand washing: A randomised comparison study. J. Hosp. Infect. 2010, 74, 86–88. [Google Scholar] [CrossRef]
- Griffin, K.J.; Scott, D.J.; Foster, N. Bare below the elbows. Ann. R. Coll. Surg. Engl. 2011, 93, 181. [Google Scholar] [CrossRef]
- Pace-Asciak, P.; Bhimrao, S.K.; Kozak, F.K.; Westerberg, B.D. Health care professionals’ neckties as a source of transmission of bacteria to patients: A systematic review. CMAJ Open 2018, 6, E26–E30. [Google Scholar] [CrossRef][Green Version]
- Frei, A.S. Bow tie or no tie: A rule to reduce healthcare-acquired infections. J. Community Hosp. Intern. Med. Perspect. 2015, 5, 28808. [Google Scholar] [CrossRef]
- Yildirim, I.; Ceyhan, M.; Cengiz, A.B.; Bagdat, A.; Barin, C.; Kutluk, T.; Gur, D. A prospective comparative study of the relationship between different types of ring and microbial hand colonization among pediatric intensive care unit nurses. Int. J. Nurs. Stud. 2008, 45, 1572–1576. [Google Scholar] [CrossRef]
- Szilagyi, L.; Haidegger, T.; Lehotsky, A.; Nagy, M.; Csonka, E.A.; Sun, X.; Ooi, K.L.; Fisher, D. A large-scale assessment of hand hygiene quality and the effectiveness of the “WHO 6-steps”. BMC Infect. Dis. 2013, 13, 249. [Google Scholar] [CrossRef]
- Boyce, J.M.; Pittet, D. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Am. J. Infect. Control 2002, 30, S1–S46. [Google Scholar] [CrossRef]
- Nicolay, C.R. Hand hygiene: An evidence-based review for surgeons. Int. J. Surg. 2006, 4, 53–65. [Google Scholar] [CrossRef]
- Larson, E.L.; Eke, P.I.; Wilder, M.P.; Laughon, B.E. Quantity of soap as a variable in handwashing. Infect. Control 1987, 8, 371–375. [Google Scholar] [CrossRef]
- Francis, R.H.; Mudery, J.A.; Tran, P.; Howe, C.; Jacob, A. The Case for Using Evidence-Based Guidelines in Setting Hospital and Public Health Policy. Front. Surg. 2016, 3, 20. [Google Scholar] [CrossRef]
- Pittet, D.; Allegranzi, B.; Boyce, J.; World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of Experts. The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infect. Control Hosp. Epidemiol. 2009, 30, 611–622. [Google Scholar] [CrossRef]
- Wynd, C.A.; Samstag, D.E.; Lapp, A.M. Bacterial carriage on the fingernails of OR nurses. AORN J. 1994, 60, 799–805. [Google Scholar] [CrossRef]
- Foca, M.; Jakob, K.; Whittier, S.; Della Latta, P.; Factor, S.; Rubenstein, D.; Saiman, L. Endemic Pseudomonas aeruginosa infection in a neonatal intensive care unit. N. Engl. J. Med. 2000, 343, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Gordin, F.M.; Schultz, M.E.; Huber, R.; Zubairi, S.; Stock, F.; Kariyil, J. A cluster of hemodialysis-related bacteremia linked to artificial fingernails. Infect. Control Hosp. Epidemiol. 2007, 28, 743–744. [Google Scholar] [CrossRef]
- Gupta, A.; Della-Latta, P.; Todd, B.; San Gabriel, P.; Haas, J.; Wu, F.; Rubenstein, D.; Saiman, L. Outbreak of extended-spectrum beta-lactamase-producing Klebsiella pneumoniae in a neonatal intensive care unit linked to artificial nails. Infect. Control Hosp. Epidemiol. 2004, 25, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Parry, M.F.; Grant, B.; Yukna, M.; Adler-Klein, D.; McLeod, G.X.; Taddonio, R.; Rosenstein, C. Candida osteomyelitis and diskitis after spinal surgery: An outbreak that implicates artificial nail use. Clin. Infect. Dis. 2001, 32, 352–357. [Google Scholar] [CrossRef]
- Lin, C.M.; Wu, F.M.; Kim, H.K.; Doyle, M.P.; Michael, B.S.; Williams, L.K. A comparison of hand washing techniques to remove Escherichia coli and caliciviruses under natural or artificial fingernails. J. Food Prot. 2003, 66, 2296–2301. [Google Scholar] [CrossRef]
- Rupp, M.E.; Fitzgerald, T.; Puumala, S.; Anderson, J.R.; Craig, R.; Iwen, P.C.; Jourdan, D.; Keuchel, J.; Marion, N.; Peterson, D.; et al. Prospective, controlled, cross-over trial of alcohol-based hand gel in critical care units. Infect. Control Hosp. Epidemiol. 2008, 29, 8–15. [Google Scholar] [CrossRef]
- Skodova, M.; Garcia Urra, F.; Gimeno Benitez, A.; Jimenez Romano, M.R.; Gimeno Ortiz, A. Hand hygiene assessment in the workplace using a UV lamp. Am. J. Infect. Control 2015, 43, 1360–1362. [Google Scholar] [CrossRef]
- Field, E.A.; McGowan, P.; Pearce, P.K.; Martin, M.V. Rings and watches: Should they be removed prior to operative dental procedures? J. Dent. 1996, 24, 65–69. [Google Scholar] [CrossRef]
- Bhusal, Y.; Laza, S.; Lane, T.W.; Schultz, K.; Hansen, C. Bacterial colonization of wristwatches worn by health care personnel. Am. J. Infect. Control 2009, 37, 476–477. [Google Scholar] [CrossRef]
- Bartlett, G.E.; Pollard, T.C.; Bowker, K.E.; Bannister, G.C. Effect of jewellery on surface bacterial counts of operating theatres. J. Hosp. Infect. 2002, 52, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Fagernes, M.; Lingaas, E. Impact of finger rings on transmission of bacteria during hand contact. Infect. Control Hosp. Epidemiol. 2009, 30, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Fagernes, M.; Lingaas, E. Factors interfering with the microflora on hands: A regression analysis of samples from 465 healthcare workers. J. Adv. Nurs. 2011, 67, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, M.; Sahin, I.; Oksuz, S.; Sencan, I.; Kucukbayrak, A.; Cakir, S.; Ozaydin, C. Hand carriage of Candida occurs at lesser rates in hospital personnel who use antimicrobial hand disinfectant. Scand. J. Infect. Dis. 2014, 46, 633–636. [Google Scholar] [CrossRef] [PubMed]
| Physicians N = 1470 | Nurses N = 3801 | Others N = 2273 | Total N = 7544 | |
|---|---|---|---|---|
| Sex | ||||
| Female | 703 (47.8%) | 3724 (98.0%) | 1911 (84.1%) | 6338 (84.0%) |
| Male | 767 (52.2%) | 77 (2.0%) | 362 (15.9%) | 1206 (16.0%) |
| Time of Participation in the Study | ||||
| First time (1×) | 1323 (90.0%) | 3431 (90.3%) | 2018 (88.8%) | 6772 (89.8%) |
| Second time (2×) | 147 (10.0%) | 370 (9.7%) | 255 (11.2%) | 772 (10.3%) |
| Job Seniority | ||||
| ≤10 years | 911 (62.0%) | 2206 (58.0%) | 1344 (59.1%) | 4461 (59.1%) |
| >10 years | 559 (38.0%) | 1595 (42.0%) | 929 (40.9%) | 3083 (40.9%) |
| Location of Work | ||||
| Hospital | 1395 (94.9%) | 3436 (90.4%) | 2065 (90.8%) | 6896 (91.4%) |
| Clinic | 68 (4.6%) | 275 (7.2%) | 95 (4.2%) | 438 (5.8%) |
| LTCF | 7 (0.5%) | 90 (2.4%) | 113 (5.0%) | 210 (2.8%) |
| Hospital | ||||
| Surgical Departments | 577 (41.3%) | 1264 (36.7%) | 367 (17.8%) | 2208 (32.0%) |
| General Departments | 589 (42.2%) | 1514 (44.1%) | 868 (42.0%) | 2971 (43.1%) |
| ED | 32 (2.3%) | 174 (5.1%) | 185 (8.9%) | 391 (5.7%) |
| ICU | 91 (6.5%) | 261 (7.6%) | 47 (2.3%) | 399 (5.8%) |
| Other * | 106 (7.7%) | 223 (6.5%) | 598 (29.0%) | 927 (13.4%) |
| Level of Health Care Referral System | ||||
| Primary | 678 (48.6%) | 2071 (60.3%) | 1219 (59.0%) | 3968 (57.6%) |
| Secondary | 350 (25.1%) | 826 (24.0%) | 550 (26.7%) | 1726 (25.0%) |
| Tertiary | 367 (26.3%) | 539 (15.7%) | 296 (14.3%) | 1221 (22.0%) |
| Location of Work | Physicians | Nurses | ||||
|---|---|---|---|---|---|---|
| Proper N = 887 | Improper N = 508 | Total N = 1395 | Proper N = 2350 | Improper N = 1086 | Total N = 3436 | |
| Surgical Departments | 384 (66.6%) | 193 (33.4%) | 577 (100%) | 868 (68.7%) | 396 (31.3%) | 1264 (100%) |
| Operating Theatres | 83 (70.9%) | 34 (29.1%) | 117 (100%) | 190 (74.8%) | 64 (25.2%) | 254 (100%) |
| Orthopedics | 37 (63.8%) | 21 (36.2%) | 58 (100%) | 78 (60.9%) | 50 (39.1%) | 128 (100%) |
| Surgery | 178 (70.9%) | 73 (29.1%) | 251 (100%) | 385 (64.5%) | 212 (35.5%) | 597 (100%) |
| Ophtalmology | 86 (57.0%) | 65 (43.0%) | 151 (100%) | 215 (75.4%) | 70 (24.6%) | 285 (100%) |
| General Departments | 366 (62.1%) | 223 (37.9%) | 589 (100%) | 1048 (69.2%) | 466 (30.8%) | 1514 (100%) |
| Neonatology | 51 (63.8%) | 29 (36.2%) | 80 (100%) | 111 (66.5%) | 56 (33.5%) | 167 (100%) |
| Pediatrics | 55 (66.3%) | 28 (33.7%) | 83 (100%) | 101 (70.1%) | 43 (29.9%) | 144 (100%) |
| Internal medicine | 193 (59.2%) | 133 (40.8%) | 326 (100%) | 685 (71.4%) | 275 (28.6%) | 960 (100%) |
| Neurology | 43 (66.2%) | 22 (33.8%) | 65 (100%) | 58 (56.3%) | 45 (43.7%) | 103 (100%) |
| Rehabilitation | 24 (68.6%) | 11 (31.4%) | 35 (100%) | 93 (66.4%) | 47 (33.6%) | 140 (100%) |
| ICU | 56 (61.5%) | 35 (38.5%) | 91 (100%) | 184 (70.5%) | 77 (29.5%) | 261 (100%) |
| ED | 18 (56.3%) | 14 (43.7%) | 32 (100%) | 100 (57.5%) | 74 (42.5%) | 174 (100%) |
| Other * | 63 (59.4%) | 43 (40.6%) | 106 (100%) | 150 (67.3%) | 73 (32.7%) | 223 (100%) |
| Physicians N = 926 | Nurses N = 2579 | Others N = 1374 | Total N = 4879 | |
|---|---|---|---|---|
| Sex | ||||
| Female | 427/703 | 2536/3724 | 1160/1911 | 4123/6338 |
| (60.7%) | (68.1%) | (60.7%) | (65.1%) | |
| Male | 499/767 | 43/77 | 214/362 | 756/1206 |
| (65.1%) | (55.8%) | (59.1%) | (62.7%) | |
| Time of participation in the study | ||||
| First time | 844/1323 | 2345/3431 | 1242/2018 | 4431/6772 |
| (63.8%) | (68.3%) | (61.5%) | (65.4%) | |
| Second time | 82/147 | 234/370 | 132/255 | 448/772 |
| (55.8%) | (63.2%) | (51.8%) | (58.0%) | |
| Dominant Hand | ||||
| Right-handed | 875/1269 | 2498/3481 | 1310/2061 | 4683/6811 |
| (69.0%) | (71.8%) | (63.6%) | (68.8%) | |
| Left-handed | 51/201 | 81/320 | 64/212 | 196/733 |
| (25.4%) | (25.3%) | (30.2%) | (26.7%) | |
| Job seniority | ||||
| ≤10 years | 562/911 | 1525/2206 | 795/1344 | 2882/4461 |
| (61.7%) | (69.1%) | (59.2%) | (64.6%) | |
| >10 years | 364/559 | 1054/1595 | 579/929 | 1997/3083 |
| (65.1%) | (66.1%) | (62.3%) | (64.8%) | |
| Location of work | ||||
| Hospital | 887/1395 | 2350/3436 | 1241/2065 | 4478/6896 |
| (63.6%) | (68.4%) | (60.1%) | (64.9%) | |
| Clinic | 34/68 | 174/275 | 62/95 | 270/438 |
| (50.0%) | (63.3%) | (65.3%) | (61.6%) | |
| LTCF | 5/7 | 55/90 | 71/113 | 131/210 |
| (61.1%) | (62.8%) | (62.4%) | ||
| Level of Health Care Referral System | ||||
| Primary | 422/678 | 1419/2071 | 738/1219 | 2579/3968 |
| (62.2%) | (68.5%) | (60.5%) | (65.0%) | |
| Secondary | 235/350 | 558/826 | 346/550 | 1139/1726 |
| (67.1%) | (67.6%) | (62.9%) | (66.0%) | |
| Tertiary | 230/367 | 373/539 | 153/296 | 756/1221 |
| (62.7%) | (69.2%) | (51.7%) | (61.9%) |
| Risk Factor | Medical Personnel | Other N = 2273 | Total N = 7544 | ||
|---|---|---|---|---|---|
| Physicians N = 1470 | Nurses N = 3801 | Total N = 5271 | |||
| long nails | 69 (4.7%) | 278 (7.3%) | 347 (6.6%) | 138 (6.1%) | 485 (6.4%) |
| artificial/polished nails | 149 (10.1%) | 734 (19.3%) | 883 (16.8%) | 401 (17.6%) | 1284 (17.0%) |
| rings | 221 (15.0%) | 630 (16.6%) | 851 (16.1%) | 392 (17.2%) | 1243 (16.5%) |
| watches | 353 (24.0%) | 458 (12.0%) | 811 (15.4%) | 292 (12.8%) | 1103 (14.6%) |
| bracelets | 63 (4.3%) | 172 (4.5%) | 235 (4.5%) | 121 (5.3%) | 356 (4.7%) |
| irritated skin | 98 (6.7%) | 293 (7.7%) | 391 (7.4%) | 132 (5.8%) | 523 (6.9%) |
| long sleeves | 358 (24.4%) | 307 (8.1%) | 665 (12.6%) | 349 (15.4%) | 1014 (13.4%) |
| Risk Factor | Medical Personnel | Non-Medical Personnel | ||||
|---|---|---|---|---|---|---|
| ≤10 Years | >10 Years | Total | ≤10 Years | >10 Years | Total | |
| long nails | 213 (61.4%) | 134 (38.6%) | 347 | 89 (64.5%) | 49 (35.5%) | 138 |
| artificial/polished nails | 513 (58.1%) | 370 (41.9%) | 883 | 237 (59.1%) | 164 (40.9%) | 401 |
| rings | 540 (63.5%) | 311 (36.5%) | 851 | 230 (58.7%) | 162 (41.3%) | 392 |
| watches | 510 (62.9%) | 301 (37.1%) | 811 | 198 (67.8%) | 94 (32.2%) | 292 |
| bracelets | 143 (60.9%) | 92 (39.1%) | 235 | 79 (65.3%) | 42 (34.7%) | 121 |
| irritated skin | 267 (68.3%) | 124 (31.7%) | 391 | 94 (71.2%) | 38 (28.8%) | 132 |
| long sleeves | 367 (55.2%) | 298 (44.8%) | 665 | 221 (63.3%) | 128 (36.7%) | 349 |
| Risk Factor | Medical Personnel | Non-Medical Personnel | Total | |||
|---|---|---|---|---|---|---|
| 1× * N = 4754 | 2× N = 517 | 1× N = 2018 | 2× N = 255 | 1× N = 6772 | 2× N = 772 | |
| long nails | 322 (6.7%) | 25 (4.8%) | 124 (6.1%) | 14 (5.5%) | 446 (6.6%) | 39 (5.1%) |
| p = 0.0916 | p = 0.6801 | p = 0.0997 | ||||
| artificial/polished nails | 770 (16.2%) | 113 (21.9%) | 361 (17.9%) | 40 (15.7%) | 1131 (16.7%) | 153 (19.5%) |
| p = 0.0011 | p = 0.3846 | p = 0.0290 | ||||
| rings | 771 (68.4%) | 80 (69.6%) | 357 (31.6%) | 35 (30.4%) | 1128 (16.7%) | 115 (14.9%) |
| p = 0.6624 | p = 0.1143 | p = 0.2116 | ||||
| watches | 735 (15.5%) | 76 (14.7%) | 258 (12.8%) | 34 (13.3%) | 993 (14.7%) | 110 (14.2%) |
| p = 0.3472 | p = 0.8052 | p = 0.7574 | ||||
| bracelets | 201 (4.2%) | 34 (6.6%) | 103 (5.1%) | 18 (7.1%) | 304 (4.5%) | 52 (6.7%) |
| p = 0.0140 | p = 0.1902 | p = 0.0053 | ||||
| irritated skin | 341 (74.8%) | 50 (74.6%) | 115 (25.2%) | 17 (25.4%) | 456 (6.7%) | 67 (8.7%) |
| p = 0.0395 | p = 0.5335 | p = 0.0438 | ||||
| long sleeve | 617 (13.0%) | 48 (9.3%) | 327 (16.2%) | 22 (8.6%) | 944 (13.9%) | 70 (9.1) |
| p = 0.0163 | p = 0.0016 | p = 0.0002 | ||||
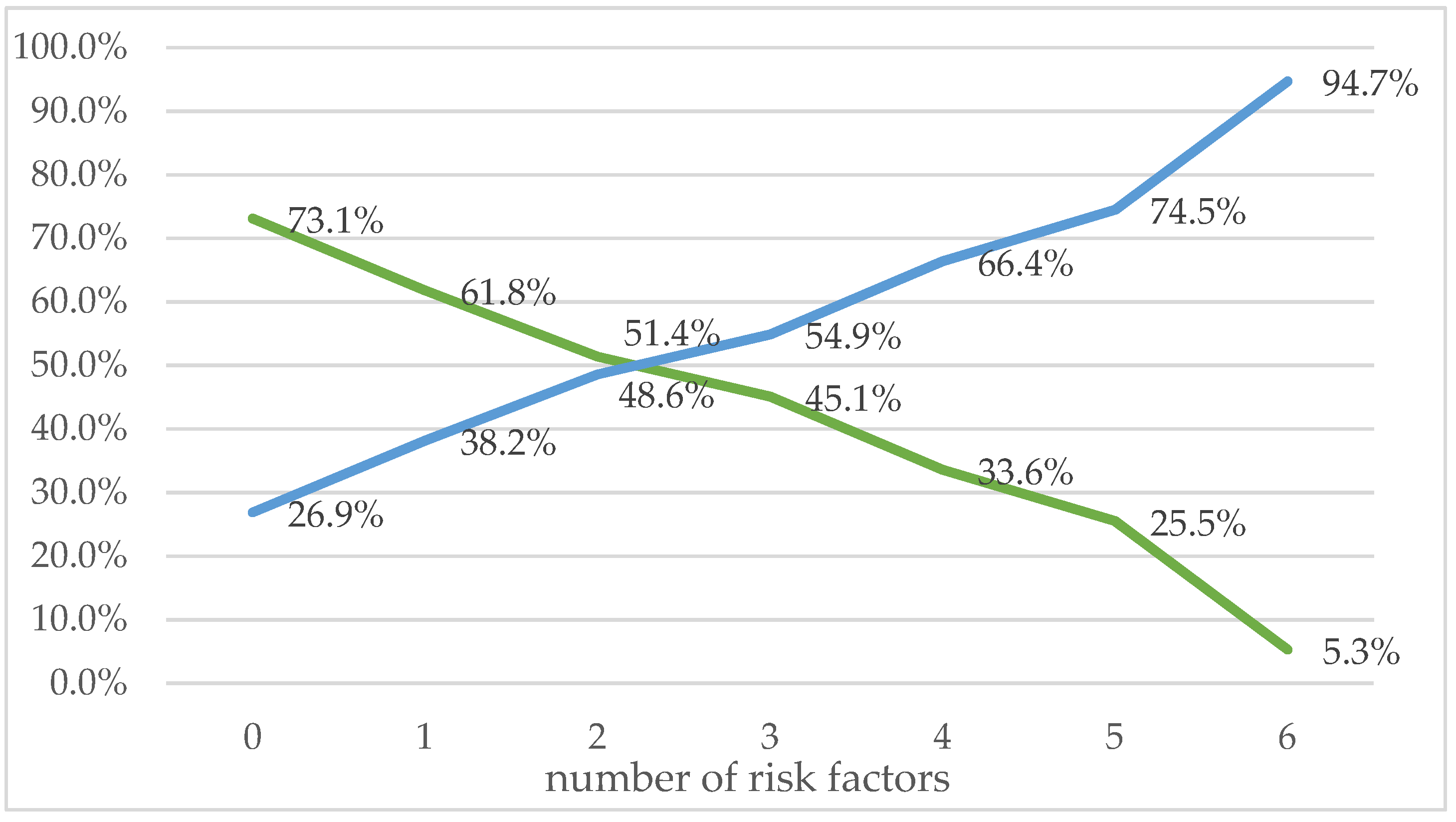
| The Number of Risk Factors | Proper Hand Disinfection | Improper Hand Disinfection | Total |
|---|---|---|---|
| 0 | 2875 (58.9%) | 1057 (39.7%) | 3932 (52.1%) |
| 1 | 1298 (26.6%) | 802 (30.1%) | 2100 (27.8%) |
| 2 | 482 (9.9%) | 456 (17.1%) | 938 (12.4%) |
| 3 | 161 (3.3%) | 196 (7.3%) | 357 (4.7%) |
| 4 | 48 (1.0%) | 95 (3.6%) | 143 (1.9%) |
| 5 | 14 (0.3%) | 41 (1.5%) | 55 (0.8%) |
| 6 | 1 (0.02%) | 18 (0.7%) | 19 (0.3%) |
| Total | 4879 (100%) | 2665 (100%) | 7544 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szumska, E.; Czajkowski, P.; Zablocki, M.; Rozkiewicz, D. The Association between Hand Disinfection Techniques and Their Barriers, as Well as the “Bare below the Elbows” Concept, among Healthcare Professionals—A Study Based on a Polish Population. Int. J. Environ. Res. Public Health 2022, 19, 11781. https://doi.org/10.3390/ijerph191811781
Szumska E, Czajkowski P, Zablocki M, Rozkiewicz D. The Association between Hand Disinfection Techniques and Their Barriers, as Well as the “Bare below the Elbows” Concept, among Healthcare Professionals—A Study Based on a Polish Population. International Journal of Environmental Research and Public Health. 2022; 19(18):11781. https://doi.org/10.3390/ijerph191811781
Chicago/Turabian StyleSzumska, Emilia, Przemyslaw Czajkowski, Michal Zablocki, and Dorota Rozkiewicz. 2022. "The Association between Hand Disinfection Techniques and Their Barriers, as Well as the “Bare below the Elbows” Concept, among Healthcare Professionals—A Study Based on a Polish Population" International Journal of Environmental Research and Public Health 19, no. 18: 11781. https://doi.org/10.3390/ijerph191811781
APA StyleSzumska, E., Czajkowski, P., Zablocki, M., & Rozkiewicz, D. (2022). The Association between Hand Disinfection Techniques and Their Barriers, as Well as the “Bare below the Elbows” Concept, among Healthcare Professionals—A Study Based on a Polish Population. International Journal of Environmental Research and Public Health, 19(18), 11781. https://doi.org/10.3390/ijerph191811781







