Mapping Geographic Trends in Early Childhood Social, Emotional, and Behavioural Difficulties in Glasgow: 2010–2017
Abstract
1. Introduction
- Map the overall risk of preschool children’s social and emotional difficulties in an entire city from 2010–2017;
- Analyse the relationship between preschool children’s social, emotional, and behavioural difficulties in neighbouring areas across a whole city from 2010–2017;
- Investigate the extent to which the relationship between geography and preschool children’s social, emotional, and behavioural difficulties is explained by demographics;
- Explore the temporal and spatiotemporal trends in preschool children’s social, emotional, and behavioural difficulties across an entire city from 2010–2017.
2. Methods
2.1. Setting
2.2. Study Design
2.3. Variables
2.4. Outcome
2.5. Geographical Data
2.6. Statistical Methods
2.6.1. Disease Mapping Model
2.6.2. Multilevel Model
2.6.3. Inference
3. Results
3.1. Descriptive Data
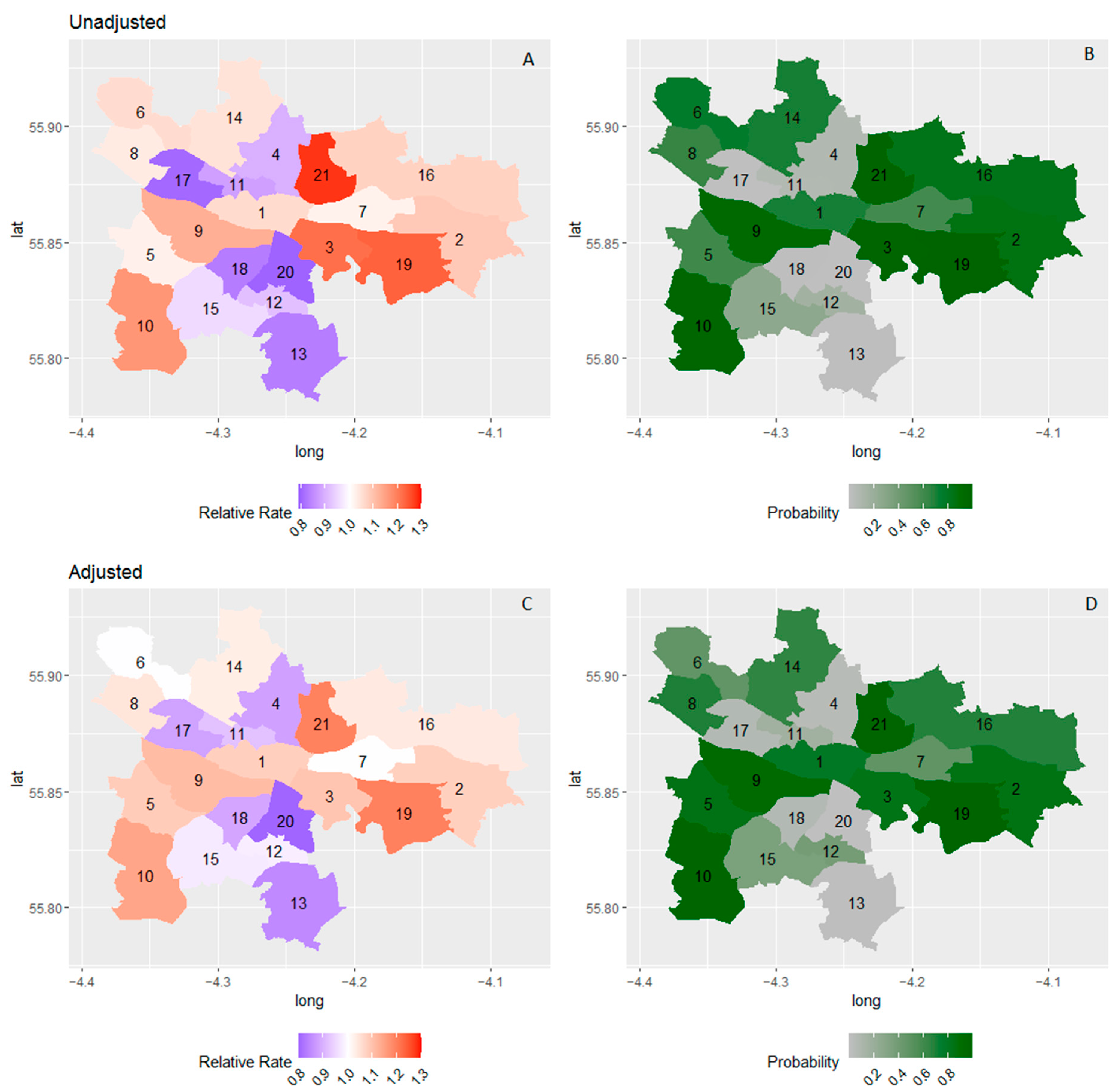
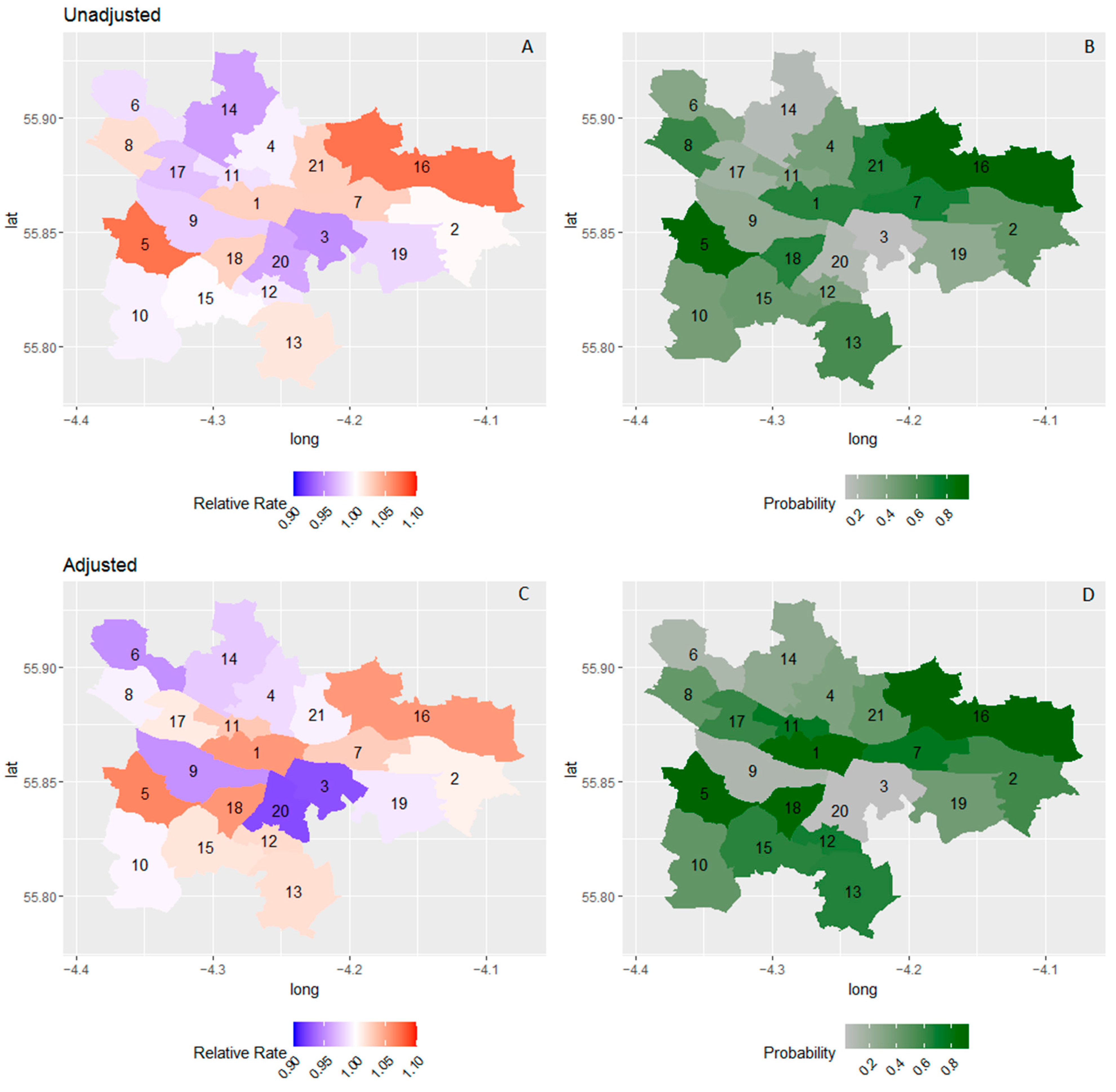
3.2. Disease Mapping Model Results
3.3. Multilevel Model Results
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vasileva, M.; Graf, R.K.; Reinelt, T.; Petermann, U.; Petermann, F. Research Review: A Meta-Analysis of the International Prevalence and Comorbidity of Mental Disorders in Children between 1 and 7 Years. J. Child Psychol. Psychiatry 2021, 62, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Egger, H.L.; Angold, A. Common Emotional and Behavioral Disorders in Preschool Children: Presentation, Nosology, and Epidemiology. J. Child Psychol. Psychiatry 2006, 47, 313–337. [Google Scholar] [CrossRef] [PubMed]
- Heckman, J.J. Invest in Early Childhood Development: Reduce Deficits, Strengthen the Economy. Heckman Equ. 2012, 7, 1–2. [Google Scholar]
- Warnick, E.M.; Bracken, M.B.; Kasl, S. Screening Efficiency of the Child Behavior Checklist and Strengths and Difficulties Questionnaire: A Systematic Review. Child Adolesc. Ment. Health 2008, 13, 140–147. [Google Scholar] [CrossRef]
- Feeney-Kettler, K.A.; Kratochwill, T.R.; Kaiser, A.P.; Hemmeter, M.L.; Kettler, R.J. Screening Young Children’s Risk for Mental Health Problems: A Review of Four Measures. Assess. Eff. Interv. 2010, 35, 218–230. [Google Scholar] [CrossRef]
- Cairney, D.G.; Kazmi, A.; Delahunty, L.; Marryat, L.; Wood, R. The Predictive Value of Universal Preschool Developmental Assessment in Identifying Children with Later Educational Difficulties: A Systematic Review. PLoS ONE 2021, 16, e0247299. [Google Scholar] [CrossRef]
- Fryers, T.; Brugha, T. Childhood Determinants of Adult Psychiatric Disorder. Clin. Pract. Epidemiol. Ment. Health CP EMH 2013, 9, 1–50. [Google Scholar] [CrossRef]
- Kohlboeck, G.; Romanos, M.; Teuner, C.M.; Holle, R.; Tiesler, C.M.; Hoffmann, B.; Schaaf, B.; Lehmann, I.; Herbarth, O.; Koletzko, S. Healthcare Use and Costs Associated with Children’s Behavior Problems. Eur. Child Adolesc. Psychiatry 2014, 23, 701–714. [Google Scholar] [CrossRef]
- Rissanen, E.; Kuvaja-Köllner, V.; Elonheimo, H.; Sillanmäki, L.; Sourander, A.; Kankaanpää, E. The Long-term Cost of Childhood Conduct Problems: Finnish Nationwide 1981 Birth Cohort Study. J. Child Psychol. Psychiatry 2021, 63, 683–692. [Google Scholar] [CrossRef]
- Rivenbark, J.G.; Odgers, C.L.; Caspi, A.; Harrington, H.; Hogan, S.; Houts, R.M.; Poulton, R.; Moffitt, T.E. The High Societal Costs of Childhood Conduct Problems: Evidence from Administrative Records up to Age 38 in a Longitudinal Birth Cohort. J. Child Psychol. Psychiatry 2018, 59, 703–710. [Google Scholar] [CrossRef]
- Leventhal, T.; Brooks-Gunn, J. The Neighborhoods They Live in: The Effects of Neighborhood Residence on Child and Adolescent Outcomes. Psychol. Bull. 2000, 126, 309. [Google Scholar] [CrossRef] [PubMed]
- Sellström, E.; Bremberg, S. The Significance of Neighbourhood Context to Child and Adolescent Health and Well-Being: A Systematic Review of Multilevel Studies. Scand. J. Public Health 2006, 34, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Minh, A.; Muhajarine, N.; Janus, M.; Brownell, M.; Guhn, M. A Review of Neighborhood Effects and Early Child Development: How, Where, and for Whom, Do Neighborhoods Matter? Health Place 2017, 46, 155–174. [Google Scholar] [CrossRef] [PubMed]
- Glover, J.; Samir, N.; Kaplun, C.; Rimes, T.; Edwards, K.; Schmied, V.; Katz, I.; Walsh, P.; Lingam, R.; Woolfenden, S. The Effectiveness of Place-Based Interventions in Improving Development, Health and Wellbeing Outcomes in Children Aged 0–6 Years Living in Disadvantaged Neighbourhoods in High-Income Countries–A Systematic Review. Wellbeing Space Soc. 2021, 2, 100064. [Google Scholar] [CrossRef]
- Ebener, S.; Guerra-Arias, M.; Campbell, J.; Tatem, A.J.; Moran, A.C.; Amoako Johnson, F.; Fogstad, H.; Stenberg, K.; Neal, S.; Bailey, P.; et al. The Geography of Maternal and Newborn Health: The State of the Art. Int. J. Health Geogr. 2015, 14, 19. [Google Scholar] [CrossRef]
- Villanueva, K.; Alderton, A.; Higgs, C.; Badland, H.; Goldfeld, S. Data to Decisions: Methods to Create Neighbourhood Built Environment Indicators Relevant for Early Childhood Development. Int. J. Environ. Res. Public Health 2022, 19, 5549. [Google Scholar] [CrossRef]
- Janus, M.; Enns, J.; Forer, B.; Raos, R.; Gaskin, A.; Webb, S.; Duku, E.; Brownell, M.; Muhajarine, N.; Guhn, M. A Pan-Canadian Data Resource for Monitoring Child Developmental Health: The Canadian Neighbourhoods and Early Child Development (CanNECD) Database. Int. J. Popul. Data Sci. 2018, 3, 431. [Google Scholar] [CrossRef][Green Version]
- Harris, F.; Dean, K.; Laurens, K.R.; Tzoumakis, S.; Carr, V.J.; Green, M.J. Regional Mapping of Early Childhood Risk for Mental Disorders in an Australian Population Sample. Early Interv. Psychiatry 2022, 1–9. [Google Scholar] [CrossRef]
- Caughy, M.O.; Leonard, T.; Beron, K.; Murdoch, J. Defining Neighborhood Boundaries in Studies of Spatial Dependence in Child Behavior Problems. Int. J. Health Geogr. 2013, 12, 24. [Google Scholar] [CrossRef]
- Li, M.; Baffour, B.; Richardson, A. Bayesian Spatial Modelling of Early Childhood Development in Australian Regions. Int. J. Health Geogr. 2020, 19, 43. [Google Scholar] [CrossRef]
- Barry, S.J.E.; Marryat, L.; Thompson, L.; Ellaway, A.; White, J.; McClung, M.; Wilson, P. Mapping Area Variability in Social and Behavioural Difficulties among G Lasgow Pre-schoolers: Linkage of a Survey of Pre-school Staff with Routine Monitoring Data. Child Care Health Dev. 2015, 41, 853–864. [Google Scholar] [CrossRef] [PubMed]
- Raos, R.; Janus, M. Examining Spatial Variations in the Prevalence of Mental Health Problems among 5-Year-Old Children in Canada. Soc. Sci. Med. 2011, 72, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Lekkas, P.; Paquet, C.; Daniel, M. Thinking in Time within Urban Health. SocArXiv. 2019. Available online: https://ideas.repec.org/p/osf/socarx/purmh.html (accessed on 1 July 2022).
- López-Quılez, A.; Munoz, F. Review of Spatio-Temporal Models for Disease Mapping. Final Rep. EUROHEIS 2009, 2, 1–19. [Google Scholar]
- Martinez-Beneito, M.A. A General Modelling Framework for Multivariate Disease Mapping. Biometrika 2013, 100, 539–553. [Google Scholar] [CrossRef]
- Leyland, A.H.; Groenewegen, P.P. Multilevel Modelling for Public Health and Health Services Research: Health in Context; Springer Nature: Berlin/Heidelberg, Germany, 2020; ISBN 3-030-34801-6. [Google Scholar]
- Djeudeu, D.; Moebus, S.; Ickstadt, K. Multilevel Conditional Autoregressive Models for Longitudinal and Spatially Referenced Epidemiological Data. Spat. Spatio-Temporal Epidemiol. 2022, 41, 100477. [Google Scholar] [CrossRef]
- Marryat, L.; Thompson, L.; Minnis, H.; Wilson, P. Exploring the Social, Emotional and Behavioural Development of Preschool Children: Is Glasgow Different? Int. J. Equity Health 2015, 14, 1–16. [Google Scholar] [CrossRef]
- Marryat, L.; Thompson, L.; Wilson, P. No Evidence of Whole Population Mental Health Impact of the Triple P Parenting Programme: Findings from a Routine Dataset. BMC Pediatr. 2017, 17, 40. [Google Scholar] [CrossRef]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Park, N. Population Estimates for the UK, England and Wales, Scotland and Northern Ireland, Provisional: 2001 to 2016 Detailed Time Series Edition of This Dataset. In Hamps. Off. Natl. Stat.; 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed on 4 August 2020).
- Care Inspectorate. Early Learning and Childcare Statistics 2014; The provision and use of registered daycare of children and childminding services in Scotland as at 31 December 2014; Care Inspectorate: Dundee, UK, 2015. [Google Scholar]
- Scottish Government. Scottish Index of Multiple Deprivation; Scottish Government: Edinburgh, UK, 2012. [Google Scholar]
- Tormod Bøe SDQ: Generating Scores in R. Available online: https://www.sdqinfo.org/c9.html (accessed on 28 January 2022).
- Youthinmind Scoring the Strengths & Difficulties Questionnaire for 2–4 Year-Olds. Available online: https://www2.oxfordshire.gov.uk/cms/sites/default/files/folders/documents/virtualschool/processesandforms/SDQp2-4Scoring.pdf (accessed on 1 February 2022).
- Bayes, T. An Essay towards Solving a Problem in the Doctrine of Chances. 1763. MD Comput. Comput. Med. Pract. 1991, 8, 157. [Google Scholar]
- Oldehinkel, A.J. Bayesian Benefits for Child Psychology and Psychiatry Researchers. J. Child Psychol. Psychiatry 2016, 57, 985–987. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Rue, H.; Martino, S.; Chopin, N. Approximate Bayesian Inference for Latent Gaussian Models by Using Integrated Nested Laplace Approximations. J. R. Stat. Soc. Ser. B Stat. Methodol. 2009, 71, 319–392. [Google Scholar] [CrossRef]
- Gelman, A. Prior Distributions for Variance Parameters in Hierarchical Models (Comment on Article by Browne and Draper). Bayesian Anal. 2006, 1, 515–534. [Google Scholar] [CrossRef]
- Bernardinelli, L.; Clayton, D.; Pascutto, C.; Montomoli, C.; Ghislandi, M.; Songini, M. Bayesian Analysis of Space—Time Variation in Disease Risk. Stat. Med. 1995, 14, 2433–2443. [Google Scholar] [CrossRef] [PubMed]
- Moran, P.A. Notes on Continuous Stochastic Phenomena. Biometrika 1950, 37, 17–23. [Google Scholar] [CrossRef]
- Hartig, F. DHARMa: Residual Diagnostics for Hierarchical (Multi-Level/Mixed) Regression Models; University of Regensburg: Regensburg, Germany, 2022. [Google Scholar]
- Spiegelhalter, D.J.; Best, N.G.; Carlin, B.P.; Van Der Linde, A. Bayesian Measures of Model Complexity and Fit. J. R. Stat. Soc. Ser. B Stat. Methodol. 2002, 64, 583–639. [Google Scholar] [CrossRef]
- Goodman, A.; Goodman, R. Population Mean Scores Predict Child Mental Disorder Rates: Validating SDQ Prevalence Estimators in Britain. J. Child Psychol. Psychiatry 2011, 52, 100–108. [Google Scholar] [CrossRef]
- Green, H.; McGinnity, Á.; Meltzer, H.; Ford, T.; Goodman, R. Mental Health of Children and Young People in Great Britain, 2004; Palgrave Macmillan: Basingstoke, UK, 2005; ISBN 1-4039-8637-1. [Google Scholar]
- Delucchi, K.L.; Bostrom, A. Methods for Analysis of Skewed Data Distributions in Psychiatric Clinical Studies: Working with Many Zero Values. Am. J. Psychiatry 2004, 161, 1159–1168. [Google Scholar] [CrossRef]
- Booth, J.G.; Casella, G.; Friedl, H.; Hobert, J.P. Negative Binomial Loglinear Mixed Models. Stat. Model. 2003, 3, 179–191. [Google Scholar] [CrossRef]
- Sellers, R.; Maughan, B.; Pickles, A.; Thapar, A.; Collishaw, S. Trends in Parent- and Teacher-Rated Emotional, Conduct and ADHD Problems and Their Impact in Prepubertal Children in Great Britain: 1999–2008. J. Child Psychol. Psychiatry 2015, 56, 49–57. [Google Scholar] [CrossRef]
- Gutman, L.M.; Joshi, H.; Parsonage, M.; Schoon, I. Trends in Parent- and Teacher-Rated Mental Health Problems among 10- and 11-Year-Olds in Great Britain: 1999–2012. Child Adolesc. Ment. Health 2018, 23, 26–33. [Google Scholar] [CrossRef]
- Pitchforth, J.; Fahy, K.; Ford, T.; Wolpert, M.; Viner, R.M.; Hargreaves, D.S. Mental Health and Well-Being Trends among Children and Young People in the UK, 1995–2014: Analysis of Repeated Cross-Sectional National Health Surveys. Psychol. Med. 2019, 49, 1275–1285. [Google Scholar] [CrossRef] [PubMed]
- Scottish Government. The Early Years Framework; Scottish Government: Edinburgh, UK, 2008. [Google Scholar]
- Collishaw, S. Annual Research Review: Secular Trends in Child and Adolescent Mental Health. J. Child Psychol. Psychiatry 2015, 56, 370–393. [Google Scholar] [CrossRef] [PubMed]
- Alderton, A.; Villanueva, K.; O’Connor, M.; Boulange, C.; Badland, H. Reducing Inequities in Early Childhood Mental Health: How Might the Neighborhood Built Environment Help Close the Gap? A Systematic Search and Critical Review. Int. J. Environ. Res. Public Health 2019, 16, 1516. [Google Scholar] [CrossRef] [PubMed]
- Peel, D.; Tanton, R. Spatial Targeting of Early Childhood Interventions: A Comparison of Developmental Vulnerability in Two Australian Cities. Aust. Geogr. 2020, 51, 489–507. [Google Scholar] [CrossRef]
- Burgemeister, F.C.; Crawford, S.B.; Hackworth, N.J.; Hokke, S.; Nicholson, J.M. Place-Based Approaches to Improve Health and Development Outcomes in Young Children: A Scoping Review. PLoS ONE 2021, 16, e0261643. [Google Scholar] [CrossRef]
- Smith, J.; McLaughlin, T.; Aspden, K. Teachers’ Perspectives of Children’s Social Behaviours in Preschool: Does Gender Matter? Australas. J. Early Child. 2019, 44, 408–422. [Google Scholar] [CrossRef]
- Ghandour, R.M.; Kogan, M.D.; Blumberg, S.J.; Jones, J.R.; Perrin, J.M. Mental Health Conditions among School-Aged Children: Geographic and Sociodemographic Patterns in Prevalence and Treatment. J. Dev. Behav. Pediatr. 2012, 33, 42–54. [Google Scholar] [CrossRef]
- Kershaw, P.; Forer, B.; Lloyd, J.E.; Hertzman, C.; Boyce, W.T.; Zumbo, B.D.; Guhn, M.; Milbrath, C.; Irwin, L.G.; Harvey, J. The Use of Population-level Data to Advance Interdisciplinary Methodology: A Cell-through-society Sampling Framework for Child Development Research. Int. J. Soc. Res. Methodol. 2009, 12, 387–403. [Google Scholar] [CrossRef]
- Tzavidis, N.; Salvati, N.; Schmid, T.; Flouri, E.; Midouhas, E. Longitudinal Analysis of the Strengths and Difficulties Questionnaire Scores of the Millennium Cohort Study Children in England Using M-quantile Random-effects Regression. J. R. Stat. Soc. Ser. A Stat. Soc. 2016, 179, 427. [Google Scholar] [CrossRef]
- Black, M.; Barnes, A.; Baxter, S.; Beynon, C.; Clowes, M.; Dallat, M.; Davies, A.R.; Furber, A.; Goyder, E.; Jeffery, C.; et al. Learning across the UK: A Review of Public Health Systems and Policy Approaches to Early Child Development since Political Devolution. J. Public Health Oxf. Engl. 2020, 42, 224–238. [Google Scholar] [CrossRef]
- Wood, R.; Stirling, A.; Nolan, C.; Chalmers, J.; Blair, M. Trends in the Coverage of ‘Universal’ Child Health Reviews: Observational Study Using Routinely Available Data. BMJ Open 2012, 2, e000759. [Google Scholar] [CrossRef] [PubMed]
- Wallace, J. Scotland: Wellbeing as Performance Management. In Wellbeing and Devolution: Reframing the Role of Government in Scotland, Wales and Northern Ireland; Wallace, J., Ed.; Wellbeing in Politics and Policy; Springer International Publishing: Cham, Switzerland, 2019; pp. 45–71. ISBN 978-3-030-02230-3. [Google Scholar]

| Demographics | N | High Score (%) | Median Score (IQR) | |
|---|---|---|---|---|
| Total | 35,171 | 3149 (9.0%) | ||
| Age (years) | 4–4.5 | 2112 | 212 (10.0%) | 6 (2–10) |
| 4.5–5 | 16,456 | 1541 (9.4%) | 5 (2–9) | |
| 5–5.5 | 15,297 | 1160 (7.6%) | 4 (1–8) | |
| 5.5–6 | 1306 | 236 (18.1%) | 6 (2–12) | |
| Sex | Female | 17,210 | 877 (5.1%) | 3 (1–7) |
| Male | 17,961 | 2272 (12.6%) | 6 (2–10) | |
| Deprivation Quintile | 5 (least deprived) | 5071 | 289 (5.7%) | 3 (0–7) |
| 4 | 5610 | 424 (7.6%) | 4 (1–8) | |
| 3 | 6696 | 605 (9.0%) | 4 (1–9) | |
| 2 | 8179 | 808 (9.9%) | 5 (2–9) | |
| 1 (most deprived) | 9615 | 1023 (10.6%) | 5 (2–10) | |
| Cohort | 2010 | 3082 | 232 (7.5%) | 4 (1–9) |
| 2011 | 3336 | 299 (9.0%) | 5 (2–9) | |
| 2012 | 3882 | 348 (9.0%) | 5 (2–9) | |
| 2013 | 3899 | 327 (8.4%) | 4 (1–8) | |
| 2014 | 5275 | 459 (8.7%) | 4 (1–9) | |
| 2015 | 5246 | 473 (9.0%) | 4 (1–9) | |
| 2016 | 5480 | 534 (9.7%) | 5 (2–9) | |
| 2017 | 4971 | 477 (9.6%) | 4 (1–9) |
| Unadjusted (95% CrI) | Adjusted (95% CrI) | |
|---|---|---|
| Intercept | 0.077 (0.069–0.087) | 0.033 (0.017–0.066) |
| Proportion > 5.5 AND <4.5 years | - | 1.467 (0.500–4.283) |
| Proportion boys | - | 3.462 (1.157–10.308) |
| Proportion most deprived | - | 1.326 (0.934–1.839) |
| Cohort | 1.026 (1.009–1.043) | 1.033 (1.015–1.050) |
| 0.026 (0.011–0.054) | 0.018 (0.006–0.041) | |
| DIC | 1022 | 1025 |
| Title 1 | Unadjusted (95% CrI) | Adjusted (95% CrI) |
|---|---|---|
| Intercept | 5.963 (5.647–6.297) | 4.079 (3.886–4.350) |
| Boys vs. Girls | - | 1.370 (1.344–1.396) |
| Age (centred and squared) | - | 1.003 (1.003–1.004) |
| 2nd least deprived vs. least | - | 1.115 (1.073–1.159) |
| middle deprived vs. least | - | 1.174 (1.128–1.222) |
| 2nd most deprived vs. least | - | 1.234 (1.186–1.284) |
| Most deprived vs. least | - | 1.243 (1.193–1.293) |
| Cohort | 1.007 (1.002–1.011) | 1.008 (1.003–1.012) |
| 0.071 (0.054–0.092) | 0.062 (0.045–0.082) | |
| 0.011(0.004–0.021) | 0.013 (0.008–0.020) | |
| DIC | 197,533 | 196,273 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ofili, S.; Thompson, L.; Wilson, P.; Marryat, L.; Connelly, G.; Henderson, M.; Barry, S.J.E. Mapping Geographic Trends in Early Childhood Social, Emotional, and Behavioural Difficulties in Glasgow: 2010–2017. Int. J. Environ. Res. Public Health 2022, 19, 11520. https://doi.org/10.3390/ijerph191811520
Ofili S, Thompson L, Wilson P, Marryat L, Connelly G, Henderson M, Barry SJE. Mapping Geographic Trends in Early Childhood Social, Emotional, and Behavioural Difficulties in Glasgow: 2010–2017. International Journal of Environmental Research and Public Health. 2022; 19(18):11520. https://doi.org/10.3390/ijerph191811520
Chicago/Turabian StyleOfili, Samantha, Lucy Thompson, Philip Wilson, Louise Marryat, Graham Connelly, Marion Henderson, and Sarah J. E. Barry. 2022. "Mapping Geographic Trends in Early Childhood Social, Emotional, and Behavioural Difficulties in Glasgow: 2010–2017" International Journal of Environmental Research and Public Health 19, no. 18: 11520. https://doi.org/10.3390/ijerph191811520
APA StyleOfili, S., Thompson, L., Wilson, P., Marryat, L., Connelly, G., Henderson, M., & Barry, S. J. E. (2022). Mapping Geographic Trends in Early Childhood Social, Emotional, and Behavioural Difficulties in Glasgow: 2010–2017. International Journal of Environmental Research and Public Health, 19(18), 11520. https://doi.org/10.3390/ijerph191811520







