The Impact of a Communication Training on the Birth Experience: Qualitative Interviews with Mothers after Giving Birth at Obstetric University Departments in Germany
Abstract
1. Introduction
- To what extent does the communication training impact the preparation for childbirth and communication during childbirth from the mothers’ subjective views?
- How was the quality of communication and mutual understanding in the hospital perceived by the mothers-to-be and their partners?
2. Materials and Methods
- Risk perceptions and outcome expectancies: awareness about personal wishes for the birthing process and the role of communication.
- Intention: understanding communication strategies (four sides of communication—communication square) [29].
- Planning and self-efficacy: expressing personal needs and wishes, inquiring (close-the-loop) and speaking up.
- Support: building empathy for professionals by taking their perspectives (empathy maps) and mobilizing/accepting support.
Data Analysis
3. Results
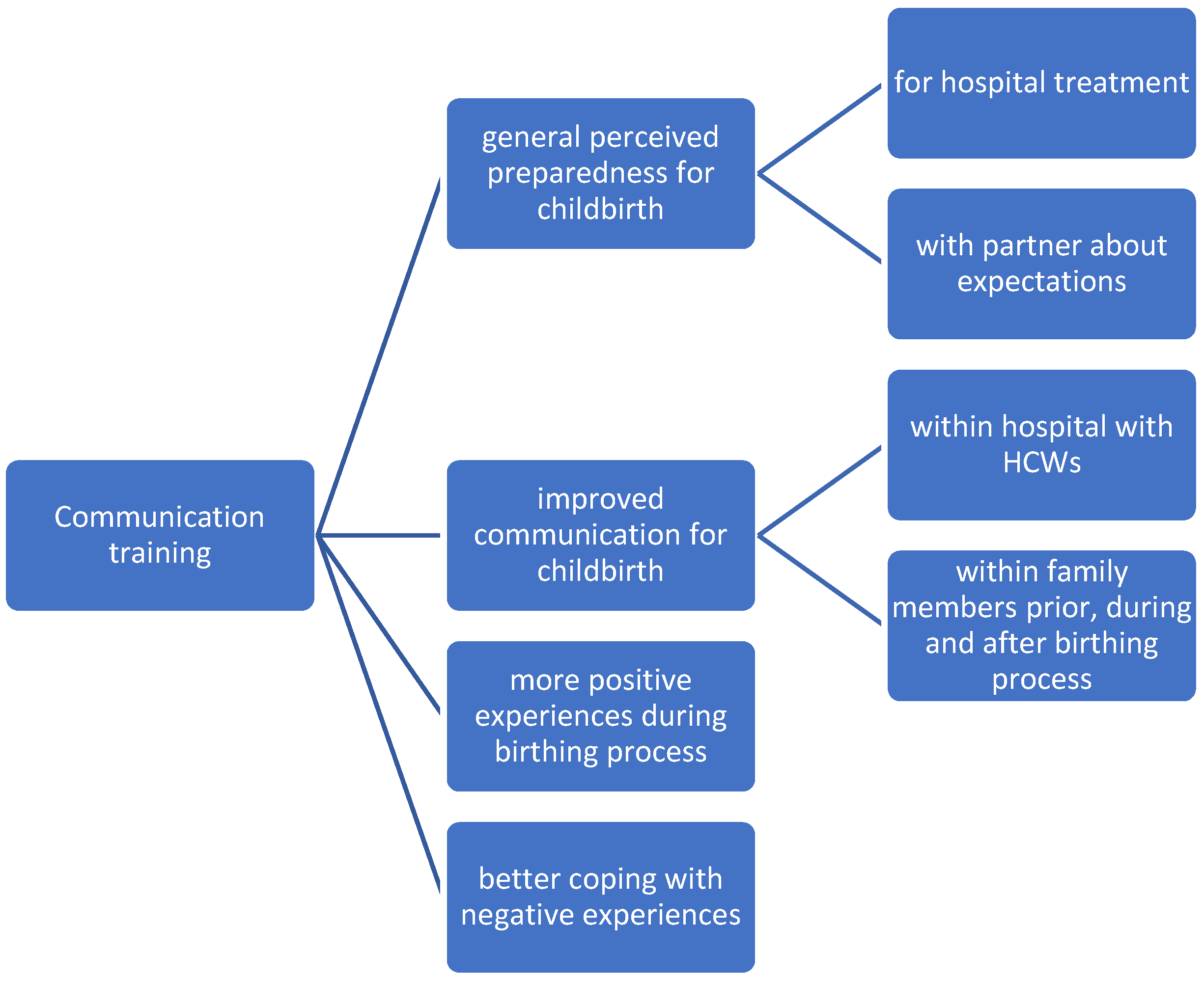
3.1. Impact of the Training on Preparation for Childbirth and Communication during Childbirth
“So I have dealt with it (senders and receivers) quite intensively during my studies. And even for me, I thought at during this training, ah, yes, that was true. And I don’t think I would have thought about it in advance, without that. So that’s our (partner included) opinion, it would probably be very, very useful for every expectant parent to do such a training”(P_21).
“This exchange with the other pregnant women and the course instructor was important because you could see that other women wanted completely different things for the birth than I did (…). Other mothers have said, I want to be left alone as much as possible. Then the thought came to me, ‘YES; how should the midwife know that? How should she know my wishes if I never express them?’ And then it occurred to me that I might have to communicate more”(P_08).
“For us, this training was actually a start to prepare the birth more intensively. And we just took that as a hanger, okay, we have to know exactly what we want, that we can communicate what we want. And then I started to talk very clearly with my husband. These are my worries, these are my fears”(P_21).
“I was so afraid of the pain (…) I then learned during communication training that I should express my feelings beforehand. That’s why I then said, I’m so afraid of pain, please help me have less pain during birth. Exactly. That was very good”(P_22).
3.2. Perceived Quality of Communication and Understanding in the Hospital
“Before the birth, I may have wanted a doctor, but that was not necessary for us and that was okay, but I think I would have felt even safer with the doctor. I don’t doubt the competence of midwives either. But maybe it is also because in (participant’s country of origin) it is usual that the doctor is present at the birth”(P_16).
“And she was also a bit of a mediator, I suppose, between the doctors and me, in case something had happened. She would probably have said, I don’t think the patient is doing so well or something. Whereas the gynecologist, she didn’t see me at all, I was already covered”(P_05).
“When the water broke at some point during the birth, the amniotic fluid was quite dark green and then the senior physician was immediately called in and she also stayed there the whole time, that was, so nothing against the resident, but the senior physician has even more experience, she also brought more calm into the whole thing, I found that very pleasant”(P_01).
“So as a positive example, a midwife student comes to mind. How patiently she listened to me every time I had questions. And she didn’t make me feel like I was asking stupid questions. (…) Even if she didn’t know something, she said with so much respect: ‘Mrs. (name), I don’t know, but please give me two hours. I will clarify this with the experienced colleague and then I will come back.’ Two hours later she was back and provided me with an answer”(P_06).
“What I found particularly good about the training was that we put ourselves in the shoes of the professionals. (...) Because when you were in the delivery room, you remembered that, ok, they have a lot to do right now and for you it’s such an exceptional situation, but for them it’s everyday life, what they’re doing right now. And that was, especially in terms of communication, that you weren’t too demanding, but rather took into account a little bit, ok, let them do their rounds now and if you have another detailed question, then they will take the time, if they have it. And that has already helped me. Absolutely”(P_10).
3.3. Positive Experiences with Sufficient Communication Competence and Perceived Empathy
“We noticed exactly, all have read this sheet (questionnaire regarding wishes for birth). Even the midwives, they knew exactly what was going on. Things like ‘we want to take our placenta home with us’ or ‘we don’t want an epidural at first’. I wasn’t offered an epidural until I asked for one. And then I realized that the doctors and midwives had read it. Or one of them had read it and told the others”(P_03).
“And then a really great midwife team came. That was actually the most beautiful phase of the birth. That was a trainee and an instructor. And they did a really, really good job. They explained everything in detail. And you also noticed that they had time. They spent quite a lot of time in the room with me. (…) One of them, the student, came two days later to the maternity ward and asked how we were doing. Visited us”(P_17).
“A psychologist was also there one day later. She talked with me for half an hour. This was ordered by the doctor who operated on me. I also thought that was great. And the doctor was there again on the next day. She told me that it was a good decision (C-section). She didn’t want me to go out with a trauma. (...) She really took her time again”(P_30).
“And my midwife took over a lot of this prepartum talk, so I had the wish for a birthing stool. In the end, I didn’t use it. But she had already set everything up. And I had checked fragrance would be nice. Then she asked me which fragrance I would like and then she added it (...)So she was not the midwife with whom I had spoken before. But she knew the file. And I just felt like I was in such good hands. She was also there the whole time, because I had told her, I’m always afraid when no one is there”(P_08).
3.4. Negative Experiences with Insufficient Communication and a Lack of Interpersonal Adaption and Empathy
“What I found problematic was that some nurses still went through their program at night. It’s 11:30 p.m. and you’ve just gone to sleep for the first time, your baby doesn’t want to be breastfed and you’re glad you can close your eyes. Then the nurse comes in, turns on all the lights, cheerfully says “Hello”, wakes everyone up and says “So, we’re going to do the Hessel Screening” or whatever there is. We’re going to prick your child’s heel now or we’re going to do a hearing test or things like that, which I would have expected in the morning”(P_03).
“And then it was so intense that I said, now I need an epidural. Because I can’t stand it for that long again. And then it took an insanely long time. At first no one came. There was no real information about how long it would take. So I would have liked to know a time horizon. ‘You have to hold out for about half an hour’ or something like that. I then sent my husband there several times and said, go and have another look. Let me know, somehow. Because that is now really unbearable”(P_14).
“I had been a mother for 20 h and I have no idea about diseases as far as children are concerned and blood values. I’m not from that area. And the nurse comes in the second morning. And tells me, ‘Mrs. (name), the bili has gone up.’ And I look at her and I say, ‘What?’ ‘Yes, the bili has risen, the child has to go under the lamp’”(P_06).
“So the resident came and listed the factors that are not so optimal and that they also discuss this again with the leading physician. In retrospect, I thought that at that moment I knew what she wanted to tell me. She had already listed the issues that were in favor of a C-section, but she hadn’t made it clear at that moment”(P_04).
“I had these really bad contractions after the induction and in retrospect I think to myself, yes, you have pain, but it doesn’t have to be that bad and I should have gotten help beforehand. I should have simply let them know beforehand. But then I was shy because the midwife said at the beginning, ‘Well, I have to stay on the ward, I couldn’t go down to the delivery room’”(P_37).
“My hands were shaking and I was somehow not really on-top. You need a little sleep after four days. And she (midwife) noticed how I was feeling and she said, it’s no wonder that my child cries so much when I’m in such a bad mood (...) I think if you’re overwhelmed, you should try to communicate differently. Or maybe ask for understanding that she now has to do everything quickly because they are understaffed or whatever. I have understanding for something like that, if someone tells me that, but if someone is simply unfriendly with me, I don’t understand that”(P_06).
4. Discussion
4.1. Impact of the Training on Preparedness for Childbirth and Communication during Childbirth
4.2. Perceived Roles of Professionals and Commitments during Childbirth
4.3. Positive and Negative Experiences with the Quality of Communication
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kohn, L.T.; Corrigan, J.M.; Donaldson, M.S. To Err is Human: Building a Safer Health System. In Institute of Medicine Committee on Quality of Health Care in America; National Academies Press (US): Washington, DC, USA, 2000. [Google Scholar]
- Iflaifel, M.; Lim, R.H.; Ryan, K.; Crowley, C. Resilient Health Care: A systematic review of conceptualisations, study methods and factors that develop resilience. BMC Health Serv. Res. 2020, 20, 324. [Google Scholar] [CrossRef] [PubMed]
- Hollnagel, E.; Lears, R.L.; Braithwaite, J. From Safety-I to Safety-II: A White Paper. 2015. Available online: https://www.england.nhs.uk/signuptosafety/wp-content/uploads/sites/16/2015/10/safety-1-safety-2-whte-papr.pdf (accessed on 7 September 2022).
- Davis, R.E.; Jacklin, R.; Sevdalis, N.; Vincent, C.A. Patient involvement in patient safety: What factors influence patient participation and engagement? Health Expect. 2007, 10, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Vincent, C.A.; Coulter, A. Patient safety: What about the patient? Qual. Saf. Health Care 2002, 11, 76–80. [Google Scholar] [CrossRef]
- Brennan, T.; Leape, L.; Laird, N.; Hebert, L.; Localio, A.; Lawthers, A.; Newhouse, J.; Weiler, P.; Hiatt, H. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N. Engl. J. Med. 1991, 324, 370–376. [Google Scholar] [CrossRef]
- Strametz, R.; Fendel, J.C.; Koch, P.; Roesner, H.; Zilezinski, M.; Bushuven, S.; Raspe, M. Prevalence of Second Victims, Risk Factors, and Support Strategies among German Nurses (SeViD-II Survey). Int. J. Environ. Res. Public Health 2021, 18, 10594. [Google Scholar] [CrossRef] [PubMed]
- Schwendimann, R.; Blatter, C.; Dhaini, S.; Simon, M.; Ausserhofer, D. The occurrence, types, consequences and preventability of in-hospital adverse events–a scoping review. BMC Health Serv. Res. 2018, 18, 521. [Google Scholar] [CrossRef]
- NHS Improvement. Never Events Policy and Framework; NHS Improvement: London, UK, 2019.
- Burgener, A.M. Enhancing Communication to Improve Patient Safety and to Increase Patient Satisfaction. Health Care Manag. Frederick 2020, 39, 128–132. [Google Scholar] [CrossRef]
- Aibar, L.; Rabanaque, M.J.; Aibar, C.; Aranaz, J.M.; Mozas, J. Patient safety and adverse events related with obstetric care. Arch. Gynecol. Obstet. 2015, 291, 825–830. [Google Scholar] [CrossRef]
- Panagioti, M.; Khan, K.; Keers, R.N.; Abuzour, A.; Phipps, D.; Kontopantelis, E.; Bower, P.; Campbell, S.; Haneef, R.; Avery, A.J.; et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: Systematic review and meta-analysis. BMJ 2019, 366, 14185. [Google Scholar] [CrossRef]
- Słabuszewska-Jóźwiak, A.; Szymański, J.K.; Ciebiera, M.; Sarecka-Hujar, B.; Jakiel, G. Pediatrics Consequences of Caesarean Section-A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8031. [Google Scholar] [CrossRef]
- Holopainen, A.; Verhage, M.L.; Oosterman, M. Childbirth Experience Associated With Maternal and Paternal Stress During the First Year, but Not Child Attachment. Front. Psychiatry 2020, 11, 562394. [Google Scholar] [CrossRef] [PubMed]
- Dingley, C.; Daugherty, K.; Derieg, M.K.; Persing, R. Improving Patient Safety Through Provider Communication Strategy Enhancements. In Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools); Henriksen, K., Battles, J.B., Keyes, M.A., Grady, M.L., Eds.; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- McCormick, M.; Pollock, W.; Kapp, S.; Gerdtz, M. Organizational strategies to optimize women’s safety during labor and birth: A scoping review. Birth 2021, 48, 285–300. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.; Ritter, G.A.; Hefele, J.L.; Hendrich, A.; McCoy, C.K. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J. Healthc. Risk Manag. 2015, 34, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Kruijver, I.P.; Kerkstra, A.; Francke, A.L.; Bensing, J.M.; van de Wiel, H.B. Evaluation of communication training programs in nursing care: A review of the literature. Patient Educ. Couns. 2000, 39, 129–145. [Google Scholar] [CrossRef]
- Lippke, S.; Wienert, J.; Keller, F.M.; Derksen, C.; Welp, A.; Kotting, L.; Hofreuter-Gatgens, K.; Muller, H.; Louwen, F.; Weigand, M.; et al. Communication and patient safety in gynecology and obstetrics-study protocol of an intervention study. BMC Health Serv. Res. 2019, 19, 908. [Google Scholar] [CrossRef]
- Franzon, A.C.A.; Oliveira-Ciabati, L.; Bonifácio, L.P.; Vieira, E.M.; Andrade, M.S.; Sanchez, J.A.C.; Braga, G.C.; Nogueira-Pileggi, V.; Fernandes, M.; Souza, J.P. A communication and information strategy in health and preparation for childbirth: A randomized cluster trial (PRENACEL). Cad. Saude Publica 2019, 35, e00111218. [Google Scholar] [CrossRef]
- Baijens, S.W.E.; Huppelschoten, A.G.; van Dillen, J.; Aarts, J.W.M. Improving shared decision-making in a clinical obstetric ward by using the three questions intervention, a pilot study. BMC Pregnancy Childbirth 2018, 18, 283. [Google Scholar] [CrossRef]
- Roter, D.L.; Erby, L.H.; Rimal, R.N.; Smith, K.C.; Larson, S.; Bennett, I.M.; Cole, K.W.; Guan, Y.; Molloy, M.; Bienstock, J. Empowering Women′s Prenatal Communication: Does Literacy Matter? J. Health Commun. 2015, 20, 60–68. [Google Scholar] [CrossRef]
- Lippke, S.; Derksen, C.; Keller, F.M.; Kötting, L.; Schmiedhofer, M.; Welp, A. Effectiveness of Communication Interventions in Obstetrics—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2616. [Google Scholar] [CrossRef]
- Schwarzer, R.; Lippke, S.; Luszczynska, A. Mechanisms of health behavior change in persons with chronic illness or disability: The Health Action Process Approach (HAPA). Psychology 2011, 56, 161–170. [Google Scholar] [CrossRef]
- Huener, B.; Derksen, C.; Schmiedhofer, M.; Lippke, S.; Janni, W.; Scholz, C. Preventable Adverse Events in Obstetrics—Systemic Assessment of Their Incidence and Linked Risk Factors. Healthcare 2022, 10, 97. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Woods, M.; Agarwal, S.; Jones, D.; Young, B.; Sutton, A. Synthesising qualitative and quantitative evidence: A review of possible methods. J. Health Serv. Res. Policy 2005, 10, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Guest, G.; Fleming, P. Public Health Research Methods; SAGE Publications, Inc.: London, UK, 2015. [Google Scholar]
- Schwarzer, R.; Hamilton, K. Changing Behavior Using the Health Action Process Approach. In The Handbook of Behavior Change; Hamilton, K., Cameron, L.D., Hagger, M.S., Hankonen, N., Lintunen, T., Eds.; Cambridge University Press: Cambridge, UK, 2020; pp. 89–103. [Google Scholar]
- von Thun, S. Institut für Kommunikation. Available online: http://www.schulz-von-thun.de/index (accessed on 6 September 2022).
- Derksen, C.; Dietl, J.E.; Häussler, S.; Steinherr-Zazo, M.; Schmiedhofer, M.; Lippke, S. Communication training for pregnant women: Application of the Health Action Process Approach. Appl. Psychol. Health Well-Being, 2022; under review. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Schmiedhofer, M.; Derksen, C.; Keller, F.M.; Dietl, J.E.; Haussler, F.; Strametz, R.; Koester-Steinebach, I.; Lippke, S. Barriers and Facilitators of Safe Communication in Obstetrics: Results from Qualitative Interviews with Physicians, Midwives and Nurses. Int. J. Environ. Res. Public Health 2021, 18, 915. [Google Scholar] [CrossRef] [PubMed]
- Derksen, C.; Kötting, L.; Keller, F.M.; Schmiedhofer, M.; Lippke, S. Psychological Intervention to Improve Communication and Patient Safety in Obstetrics: Examination of the Health Action Process Approach. Front. Psychol. 2022, 13, 771626. [Google Scholar] [CrossRef]
- Schreier, M. Sampling and generalization. In The Sage Handbook of Qualitative Data Collection; Flick, U., Ed.; SAGE: London, UK, 2018; pp. 84–98. [Google Scholar]
- Schreier, M. Qualitative Content Analysis in Practice; SAGE Publications Ltd.: London, UK, 2012. [Google Scholar]
- Schmiedhofer, M.; Derksen, C.; Dietl, J.E.; Häussler, F.; Louwen, F.; Hüner, B.; Reister, F.; Strametz, R.; Lippke, S. Birthing under the Condition of the COVID-19 Pandemic in Germany: Interviews with Mothers, Partners, and Obstetric Health Care Workers. Int. J. Environ. Res. Public Health 2022, 19, 1486. [Google Scholar] [CrossRef]
- Anderson, T. Feeling Safe Enough to Let Go: The Relationship Between a Woman and Her Midwife During the Second Stage of Labour; Macmillan Press: Basingstoke, UK, 2010. [Google Scholar] [CrossRef]
- Huener, B.; Derksen, C.; Schmiedhofer, M.; Lippke, S.; Janni, W.; Scholz, C. Reducing Preventable Adverse Events in Obstetrics by Improving Interprofessional Communication Skills—Results of an Intervention Study; University Ulm: Ulm, Germany, 2022. [Google Scholar]
- Hurtig, R.R.; Alper, R.M.; Bryant, K.N.T.; Davidson, K.R.; Bilskemper, C. Improving Patient Safety and Patient—Provider Communication. Perspect. ASHA Spec. Interest Groups 2019, 4, 1017–1027. [Google Scholar] [CrossRef]
- Wu, M.; Tang, J.; Etherington, N.; Walker, M.; Boet, S. Interventions for improving teamwork in intrapartum care: A systematic review of randomised controlled trials. BMJ Qual. Saf. 2020, 29, 77. [Google Scholar] [CrossRef]
- Cheng, E.R.; Carroll, A.E.; Iverson, R.E.; Declercq, E.R. Communications between Pregnant Women and Maternity Care Clinicians. JAMA Netw. Open 2020, 3, e206636. [Google Scholar] [CrossRef]
- Street, R.L.; Makoul, G.; Arora, N.K.; Epstein, R.M. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ. Couns. 2009, 74, 295–301. [Google Scholar] [CrossRef]
- Bartlett, G.; Blais, R.; Tamblyn, R.; Clermont, R.J.; MacGibbon, B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Can. Med. Assoc. J. 2008, 178, 1555–1562. [Google Scholar] [CrossRef] [PubMed]
- Coughlan, B.; Powell, D.; Higgins, M.F. The Second Victim: A Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 213, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Thorstensson, S.; Ekström, A.; Lundgren, I.; Wahn, E.H. Exploring Professional Support Offered by Midwives during Labour: An Observation and Interview Study. Nurs. Res. Pract. 2012, 2012, 648405. [Google Scholar] [CrossRef] [PubMed]
- Carmody, D.; Tregonning, A.; Nathan, E.; Newnham, J.P. Patient perceptions of medical students’ involvement in their obstetrics and gynaecology health care. Aust. N. Z. J. Obstet. Gynecol. 2011, 51, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Mackert, M.; Ball, J.; Lopez, N. Health literacy awareness training for healthcare workers: Improving knowledge and intentions to use clear communication techniques. Patient Educ. Couns. 2011, 85, e225–e228. [Google Scholar] [CrossRef]
- Howick, J.; Moscrop, A.; Mebius, A.; Fanshawe, T.R.; Lewith, G.; Bishop, F.L.; Mistiaen, P.; Roberts, N.W.; Dieninytė, E.; Hu, X.-Y.; et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J. Royal Soc. Med. 2018, 111, 240–252. [Google Scholar] [CrossRef]
- Winter, V.; Dietermann, K.; Schneider, U.; Schreyögg, J. Nurse staffing and patient-perceived quality of nursing care: A cross-sectional analysis of survey and administrative data in German hospitals. BMJ Open 2021, 11, e051133. [Google Scholar] [CrossRef]
- Baranowska, B.; Pawlicka, P.; Kiersnowska, I.; Misztal, A.; Kajdy, A.; Sys, D.; Doroszewska, A. Woman’s Needs and Satisfaction Regarding the Communication with Doctors and Midwives during Labour, Delivery and Early Postpartum. Healthcare 2021, 9, 382. [Google Scholar] [CrossRef]
- Davis, R.E.; Sevdalis, N.; Vincent, C.A. Patient involvement in patient safety: How willing are patients to participate? BMJ Qual. Saf. 2011, 20, 108–114. [Google Scholar] [CrossRef]
- Nydoo, P.; Pillay, B.J.; Naicker, T.; Moodley, J. The second victim phenomenon in health care: A literature review. Scand. J. Public Health 2019, 48, 629–637. [Google Scholar] [CrossRef]
- Agbabiaka, T.B.; Lietz, M.; Mira, J.J.; Warner, B. A literature-based economic evaluation of healthcare preventable adverse events in Europe. Int. J. Qual. Health Care 2017, 29, 9–18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Herzog-Petropaki, N.; Derksen, C.; Lippke, S. Health Behaviors and Behavior Change during Pregnancy: Theory-Based Investigation of Predictors and Interrelations. Sexes 2022, 3, 351–366. [Google Scholar] [CrossRef]
| Age of the study participant | range = 27–46 years; median 33 years; mean 34 years (SD = 4) |
| Migration status | 5 (21%), of which: 3 (12.5%) < 10 years immigrated themselves and 2 (8.5%) second generation |
| Parity | 18 (75%) first-time mothers 6 (25%) second and multiple birth |
| Birth mode | 18 (75%) vaginal 6 (25%) C-section |
| Twin birth | 1 (4%) |
| Child with disability | 1 (4%) |
| COVID-19 tested positive | 2 (8%) |
| Interview duration | 21–95 min; median 37; mean 36 min (SD = 15) |
| Interview format | 21 (88%) via TEAMS with camera on; 3 (12%) by telephone/TEAMS camera off |
| Interview period | February to July 2021 |
| Period of giving birth | July 2020 to May 2021 |
| Interview time after delivery | 3.5 to 33 weeks; median 11; mean 13 weeks (SD = 8) |
| Do you remember getting your first information about births in your life, and if yes from whom? Do you recall an emotional association to your recent birth experience—what describes the feeling you associate with your birth the best? How and with whom did you prepare for your birth—giving process? (doctors, midwives, nurses, friends, relatives) |
| You attended an online communication training at (date). If you recall, what impact did the training have on your preparation for the delivery? |
| What kind of thoughts have you given to the delivery process? To what extent have you considered how to articulate your needs? |
| Now it’s about your recent birth experience: Could you please recall the whole process of delivery from the moment you decided you have to go to the hospital to the time of discharge? |
| What kind of support did you receive, what was sufficient, what was lacking, how did you feel? |
| How did you perceive the communication with the professionals? Were your questions answered? |
| How far do you perceive your mental preparation as helpful? How would you express your needs? |
| Which persons or professions (midwives, doctors, nurses, partners) were most important in providing or lacking support |
| What could have been better? And who should have done something differently? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmiedhofer, M.; Derksen, C.; Dietl, J.E.; Haeussler, F.; Strametz, R.; Huener, B.; Lippke, S. The Impact of a Communication Training on the Birth Experience: Qualitative Interviews with Mothers after Giving Birth at Obstetric University Departments in Germany. Int. J. Environ. Res. Public Health 2022, 19, 11481. https://doi.org/10.3390/ijerph191811481
Schmiedhofer M, Derksen C, Dietl JE, Haeussler F, Strametz R, Huener B, Lippke S. The Impact of a Communication Training on the Birth Experience: Qualitative Interviews with Mothers after Giving Birth at Obstetric University Departments in Germany. International Journal of Environmental Research and Public Health. 2022; 19(18):11481. https://doi.org/10.3390/ijerph191811481
Chicago/Turabian StyleSchmiedhofer, Martina, Christina Derksen, Johanna Elisa Dietl, Freya Haeussler, Reinhard Strametz, Beate Huener, and Sonia Lippke. 2022. "The Impact of a Communication Training on the Birth Experience: Qualitative Interviews with Mothers after Giving Birth at Obstetric University Departments in Germany" International Journal of Environmental Research and Public Health 19, no. 18: 11481. https://doi.org/10.3390/ijerph191811481
APA StyleSchmiedhofer, M., Derksen, C., Dietl, J. E., Haeussler, F., Strametz, R., Huener, B., & Lippke, S. (2022). The Impact of a Communication Training on the Birth Experience: Qualitative Interviews with Mothers after Giving Birth at Obstetric University Departments in Germany. International Journal of Environmental Research and Public Health, 19(18), 11481. https://doi.org/10.3390/ijerph191811481








