Enhancing Existing Formal Home Care to Improve and Maintain Functional Status in Older Adults: Results of a Feasibility Study on the Implementation of Care to Move (CTM) in an Irish Healthcare Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Procedures
2.4. The Care to Move Approach
2.5. Primary Outcomes
2.6. Secondary Outcomes
2.7. Data Analysis
2.8. Acceptability and Feasibility Outcomes
2.9. Health Economic Evaluation
2.10. Ethical Approval and Trial Registration
3. Results
3.1. Training of Home Care Staff in CTM Approach
3.2. Feasibility Outcomes
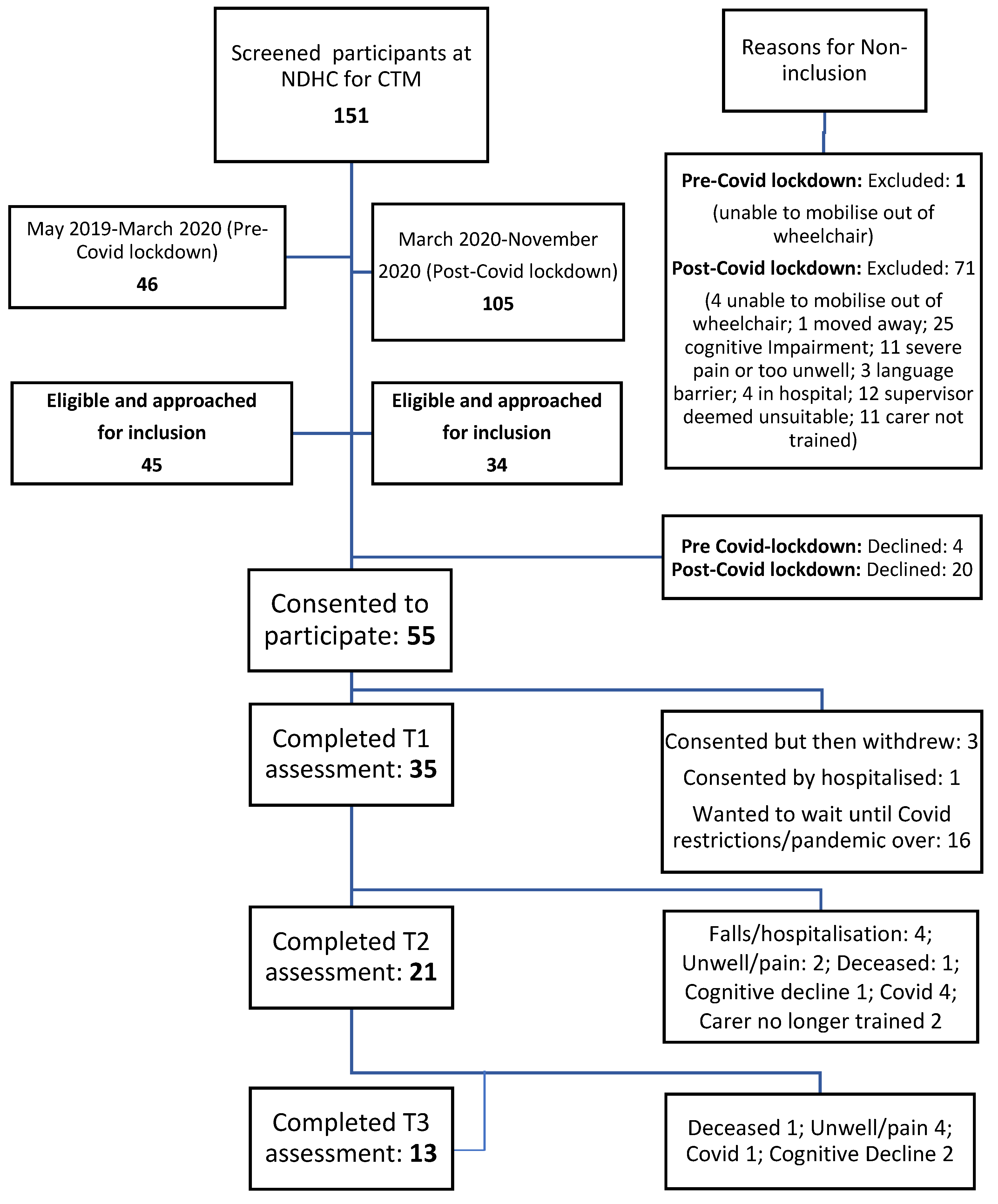
3.2.1. Recruitment
3.2.2. Adherence
3.2.3. Retention
3.2.4. Data Loss in Questionnaires and Tests; Time Taken
3.2.5. Adverse Events
3.2.6. Perceptions of Home Care Managers; Acceptability
3.2.7. Perceptions and Views of the CTM Approach Implementation by Home Care Managers: Feasibility
3.3. Secondary Outcomes
3.4. Cost Analysis of CTM Implementation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wren, M.A.; Keegan, C.; Walsh, B.; Bergin, A.; Eighan, J.; Brick, A.; Connolly, S.; Watson, D. Projections of demand for Healthcare in Ireland, 2015–2030, First Report from the Hippocrates Model. Economic and Social Research Institute (ESRI). October 2017 [Viewed 2 May 2022]. Available online: http://www.esri.ie/publications/projections-of-demand-for-healthcare-in-ireland-2015-2030-first-report-from-the-hippocrates-model/ (accessed on 1 August 2022).
- National Library of Medicine. Home Care Services. January 2017 [Viewed 2 May 2022]. Available online: https://medlineplus.gov/homecareservices.html (accessed on 1 August 2022).
- Walsh, B.; Lyons, S. Demand for the Statutory Home Support Scheme. 2022. Available online: https://www.esri.ie/system/files/publications/RS122.pdf (accessed on 1 August 2022).
- Health Services Executive Ireland Service Plan. National Service Plan 2021; Health Service Executive: Dublin, Ireland, 2021; Available online: https://www.hse.ie/eng/services/publications/serviceplans/national-service-plan-2021.pdf (accessed on 1 August 2022).
- Kelly, S.; O’Brien, I.; Smuts, K.; O’Sullivan, M.; Warters, A. Prevalence of frailty among community dwelling older adults in receipt of low level home support: A cross-sectional analysis of the North Dublin Cohort. BMC Geriatr. 2017, 17, 121. [Google Scholar] [CrossRef] [PubMed]
- Aspell, N.; O’Sullivan, M.; O’Shea, E.; Irving, K.; Duffy, C.; Gorman, R.; Warters, A. Predicting admission to long-term care and mortality among community-based, dependent older people in Ireland. Int. J. Geriatr. Psychiatry 2019, 34, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Turner, G. Introduction to Frailty, Fit for Frailty Part 1. 2014. Available online: https://www.bgs.org.uk/resources/introduction-to-frailty (accessed on 1 August 2022).
- Burton, E.; Farrier, K.; Galvin, R.; Johnson, S.; Horgan, N.F.; Warters, A.; Hill, K.D. Physical activity programs for older people in the community receiving home care services: Systematic review and meta-analysis. Clin. Interv. Aging 2019, 6, 1045–1064. [Google Scholar] [CrossRef] [PubMed]
- Burton, E.; Lewin, G.; Boldy, D. Physical activity preferences of older home care clients. Int. J. Older People Nurs. 2015, 10, 170–178. [Google Scholar] [CrossRef]
- Later Life Training UK Care To Move Training. [Viewed 2 May 2022]. Available online: https://www.laterlifetraining.co.uk/courses/care-move-ctm-course/ (accessed on 1 August 2022).
- Horgan, N.F.; Cummins, V.; Doyle, F.; O’Sullivan, M.; Galvin, R.; Burton, E.; Sorensen, J.; Skelton, D.A.; Townley, B.; Rooney, D.; et al. Enhancing existing formal home care to improve and maintain functional status in older adults: Protocol for a feasibility study on the implementation of the Care to Move (CTM) programme in an Irish healthcare setting. J. Frailty Sarcopenia Falls 2020, 5, 10–16. [Google Scholar] [CrossRef]
- Azim, F.T.; Burton, E.; Ariza-Vega, P.; Asadian, M.; Bellwood, P.; Burns, J.; Clemson, L.; Grover, S.; Hoppmann, C.A.; Langford, D.; et al. Exploring behavior change techniques for reablement: A scoping review. Braz. J. Phys. Ther. 2022, 26, 100401. [Google Scholar] [CrossRef]
- Swan, L.; Burton, E.; Horgan, N.F.; Galvin, R.; Skelton, D.A.; Townley, B.; Doyle, F.; Jabakhanji, S.B.; Sorensen, J.; Rooney, D.; et al. Embedding physical activity within community home support services for older adults in Ireland–a qualitative study of barriers and facilitators. Clin. Interv. Aging 2022, 17, 223–234. [Google Scholar] [CrossRef]
- Burton, E.; Horgan, N.F.; Cummins, V.; Warters, A.; Swan, L.; O’Sullivan, M.; Skelton, D.A.; Townley, B.; Doyle, F.; Jabakhanji, S.B.; et al. A qualitative study of older adults’ experiences of embedding physical activity within their home care services. J. Multidiscip. Healthcare. 2022, 15, 1163–1173. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpe, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Thabane, L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud. 2019, 5, 114. [Google Scholar] [CrossRef] [Green Version]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council Guidance. BMJ 2008, 337, 1655. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Howlett, S.E.; MacKnight, C.; Beattie, B.L.; Bergman, H.; Hébert, R.; Hogan, D.B.; Wolfson, C.; McDowell, L. Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: Report from the Canadian study of Health and Aging. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; van Straten, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The Timed “Up and Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Rickli, R.; Jones, C. Functional fitness normative scores for community-residing older adults, ages 60-94. J. Aging Phys. Act. 1999, 7, 162–181. [Google Scholar] [CrossRef]
- Nouri, F.M.; Lincoln, N.B. An extended activities of daily living scale for stroke patients. Clin. Rehabil. 1987, 1, 301–305. [Google Scholar] [CrossRef]
- Powell, L.E.; Myers, A.M. The Activities-specific Balance Confidence (ABC) Scale. J. Gerontol. A Biol. Sci. Med. Sci. 1995, 50, 28–34. [Google Scholar] [CrossRef]
- Simpson, J.M.; Worsfold, C.; Fisher, K.D.; Valentine, J.D. The CONFbal scale; a measure of balance–a key outcome of rehabilitation. Physiotherapy 2009, 95, 103–109. [Google Scholar] [CrossRef]
- Gill, D.P.; Jones, G.R.; GuangYong, Z.; Speechley, M. The Phone-FITT: A brief physical activity interview for older adults. J. Aging Phys. Act. 2008, 16, 292–315. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Marcus, B.H.; Selby, V.C.; Niaura, R.S.; Rossi, J.S. Self-efficacy and the stages of exercise behaviour change. Res. Q. Exerc. Sport 1992, 63, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Moschny, A.; Platen, P.; Klaassen-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults in Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef] [PubMed]
- Wójcicki, T.R.; White, S.M.; McAuley, E. Assessing outcome expectations in older adults: The multidimensional outcome expectations for exercise scale. J. Gerontol Psychol. Sci. 2009, 64, 33–40. [Google Scholar] [CrossRef]
- Ziegelmann, J.P.; Lippke, S. Planning and strategy use in health behavior change: A lifespan view. Int. J. Behav. Med. 2007, 14, 30–39. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Miles, M.; Huberman, A. An Expanded Source Book: Qualitative Data Analysis, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 1994. [Google Scholar]
- Bailey, L.; Ward, M.; DiCosimo, A.; Baunta, S.; Cunningham, C.; Romero-Ortuno, R.; Kenny, R.A.; Purcell, R.; Lannon, R.; McCarroll, K.; et al. Physical and mental health of older people while cocooning during the COVID-19 pandemic. QJM 2021, 114, 648–653. [Google Scholar] [CrossRef]
- Glendinning, C.; Jones, K.; Baxter, K.; Rabiee, P.; Curtis, L.A.; Wilde, A.; Arksey, H.; Forder, J.E. Home Care Re-Ablement Services: Investigating the Longer-Term Impacts (Prospective Longitudinal Study); York University: York, UK, 2010. Available online: https://www.york.ac.uk/inst/spru/research/pdf/Reablement.pdf (accessed on 1 August 2022).
- McLeod, B.; Mair, M.; RP&M Associates Ltd. Evaluation of City of Edinburgh Council Home Care Re-Ablement Service; Scottish Government Social Research: Edinburgh, UK, 2009; Available online: https://scvo.scot/policy/research/evidence-library/2009-evaluation-of-city-of-edinburgh-council-home-care-re-ablement-service (accessed on 1 August 2022).
- Further Education and Training Awards Council of Ireland (FETAC) 2022. Available online: https://en.wikipedia.org/wiki/Further_Education_and_Training_Awards_Council (accessed on 1 August 2022).
- Myers, A.M.; Fletcher, P.C.; Myers, A.H.; Sherk, W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J. Gerontol. A Biol. Sci. Med. Sci. 1998, 53, M287–M294. [Google Scholar] [CrossRef]
- Lajoie, Y.; Gallagher, S.P. Predicting falls within the elderly community: Comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004, 38, 11–26. [Google Scholar] [CrossRef]
- Gill, D.P.; Zou, G.Y.; Jones, G.R.; Speechley, M. Injurious falls are associated with lower household but higher recreational physical activities in community-dwelling older male veterans. Gerontology 2008, 54, 106–115. [Google Scholar] [CrossRef]
- Home Support Service for Older People: 2018 Service Specification. Available online: https://www.hse.ie/eng/services/list/4/olderpeople/service-specifications-home-support-services-2018.pdf (accessed on 1 August 2022).
- Institute of Public Health in Ireland. Improving Home Care Services in Ireland: An Overview of the Findings of the Department of Health’s Public Consultation; Institute of Public Health: Dublin, Ireland, 2018. Available online: https://assets.gov.ie/9990/1e6ec3b04d8a4c1480c6637cce471c88.pdf (accessed on 1 August 2022).
- Health Information and Quality Authority. Regulation of Homecare: A Position Paper. HIQA: 2021. Available online: https://www.hiqa.ie/sites/default/files/2021-12/Regulation-of-Homecare-A-Position-Paper.pdf (accessed on 1 August 2022).
- Department of Health of Ireland. Cross-Departmental Strategic Workforce Advisory Group on Home Carers and Nursing Home Health Care Assistants. Available online: https://www.gov.ie/en/press-release/df590-minister-for-mental-health-and-older-people-mary-butler-td-launches-the-first-meeting-of-the-cross-departmental-strategic-workforce-advisory-group-on-home-carers-and-nursing-home-health-care-assistants/ (accessed on 1 August 2022).
- Healthcare Improvement Scotland. Focus on Dementia Supporting Improvements for People with Dementia in Acute Care. 2016. Available online: https://ihub.scot/media/4737/2016001-fod-acute-case-study-report-web.pdf (accessed on 1 August 2022).


| Variable | Variable Description | N(%) out of Total 35 |
|---|---|---|
| Gender | Male | 5 (14.3%) |
| Female | 30 (85.7%) | |
| Marital status | Married | 9 (25.7%) |
| Single | 10 (28.6%) | |
| Widowed | 16 (45.7%) | |
| Living status | Lives alone | 24 (68.6%) |
| Lives with other | 11 (31.4%) | |
| Uses mobility aid | No aid | 12 (34.3%) |
| Stick | 12 (34.3%) | |
| Frame 1 | 10 (28.6%) | |
| Wheelchair | 1 (2.9%) | |
| Rockwood Score | 3 | 1 (2.9%) |
| 4 | 3 (8.6%) | |
| 5 | 12 (34.3%) | |
| 6 | 19 (54.2%) |
| Outcome Measure | Time 1 | Time 2 | Time 3 |
|---|---|---|---|
| Baseline | 8 Weeks | 6 Months or Later | |
| Timed Up and Go (secs) $: n (% of total) | |||
| Mean (SD) | 33 (94.3%) | 20 (95.2%) | 11 (84.6%) |
| Median (IQR) | 21.8 (10.8) | 19.1 (9.3) | 22.8 (11.3) |
| Cohens ds | 19.6 (10.9) | 18.8 (11.0) | 18.8 (11.0) |
| _ | −0.26 a | 0.1 | |
| 30 s sit to stand (number) ¶: n (% of total) | |||
| Mean (SD) | 33 (94.3%) | 18 (85.7%) | 12 (92.3%) |
| Median (IQR) | 7.0 (2.7) | 7.8 (3.4) | 8.0 (4.4) |
| Cohens ds | 7.0 (4.0) | 7.0 (5.5) | 7.0 (4.5) |
| - | 0.28 a | 0.31 a | |
| Nottingham Extended ADL (score) ¶: | |||
| n (% of total) | |||
| Mean (SD) | 35 (100%) | 21 (100%) | 13 (100%) |
| Median (IQR) | 55.8 (13.0) | 52.3 (11.5) | 51.9 (9.3) |
| Cohens ds | 57.0 (19.0) | 57.0 (19.0) | 53.0 (12.0) |
| - | −0.28 a | −0.32 a | |
| ConfBal (score) $: n (% of total) | |||
| Mean (SD) | 35 (100%) | 20 (95.2%) | 13 (100%) |
| Median (IQR) | 21.3 (4.3) | 19.3 (3.7) | 20.2 (3.8) |
| Cohens ds | 21.0 (6.0) | 19.0 (3.3) | 20.0 (5.0) |
| - | −0.49 a | −0.28 a | |
| ABC balance confidence (%) ¶: n (% of total) | 34 (97.1%) | 18 (85.7%) | 12 (92.3%) |
| Mean (SD) | 48.3 (18.5) | 44.9 (13.7) | 41.9 (19.5) |
| Median (IQR) | 45.9 (16.9) | 45.3 (23.0) | 38.8 (30.3) |
| Cohens ds | - | −0.20 a | −0.34 a |
| EQ-5D-5L (%) ¶: n (% of total) | 35 (100%) | 20 (95.2%) | 12 (92.3%) |
| Mean (SD) | 0.549 (0.195) | 0.693 (0.195) | 0.764 (0.143) |
| Median (IQR) | 0.0683 (0.440) | 0.742 (0.201) | 0.778 (0.190) |
| Cohens ds | _ | 0.50 a | 0.74 a |
| EQ-VAS (%) ¶: n (% of total) | 33 (94.3%) | 20 (95.2%) | 13 (100%) |
| Mean (SD) | 62.6 (21.7) | 72.0 (17.8) | 65.8 (23.8) |
| Median (IQR) | 60.0 (30.0) | 75.0 (22.5) | 70.0 (35.0) |
| Cohens ds | - | 0.46 a | 0.14 |
| Exercise Self Efficacy (score) ¶: n (% of total) | 35 (100%) | 16 (76.2%) | 8 (61.5%) |
| Mean (SD) | 18.9 (4.1) | 21.3 (5.3) | 21.8 (6.1) |
| Median (IQR) | 18.0 (5.0) | 19.5 (9.3) | 23.0 (9.8) |
| Cohens ds | - | 0.54 b | 0.63 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horgan, F.; Cummins, V.; Skelton, D.A.; Doyle, F.; O’Sullivan, M.; Galvin, R.; Burton, E.; Sorensen, J.; Jabakhanji, S.B.; Townley, B.; et al. Enhancing Existing Formal Home Care to Improve and Maintain Functional Status in Older Adults: Results of a Feasibility Study on the Implementation of Care to Move (CTM) in an Irish Healthcare Setting. Int. J. Environ. Res. Public Health 2022, 19, 11148. https://doi.org/10.3390/ijerph191811148
Horgan F, Cummins V, Skelton DA, Doyle F, O’Sullivan M, Galvin R, Burton E, Sorensen J, Jabakhanji SB, Townley B, et al. Enhancing Existing Formal Home Care to Improve and Maintain Functional Status in Older Adults: Results of a Feasibility Study on the Implementation of Care to Move (CTM) in an Irish Healthcare Setting. International Journal of Environmental Research and Public Health. 2022; 19(18):11148. https://doi.org/10.3390/ijerph191811148
Chicago/Turabian StyleHorgan, Frances, Vanda Cummins, Dawn A. Skelton, Frank Doyle, Maria O’Sullivan, Rose Galvin, Elissa Burton, Jan Sorensen, Samira Barbara Jabakhanji, Bex Townley, and et al. 2022. "Enhancing Existing Formal Home Care to Improve and Maintain Functional Status in Older Adults: Results of a Feasibility Study on the Implementation of Care to Move (CTM) in an Irish Healthcare Setting" International Journal of Environmental Research and Public Health 19, no. 18: 11148. https://doi.org/10.3390/ijerph191811148
APA StyleHorgan, F., Cummins, V., Skelton, D. A., Doyle, F., O’Sullivan, M., Galvin, R., Burton, E., Sorensen, J., Jabakhanji, S. B., Townley, B., Rooney, D., Jackson, G., Murphy, L., Swan, L., O’Neill, M., & Warters, A. (2022). Enhancing Existing Formal Home Care to Improve and Maintain Functional Status in Older Adults: Results of a Feasibility Study on the Implementation of Care to Move (CTM) in an Irish Healthcare Setting. International Journal of Environmental Research and Public Health, 19(18), 11148. https://doi.org/10.3390/ijerph191811148









