The Impact of Dance Interventions on Patients with Noninfectious Pulmonary Diseases: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Selection Criteria
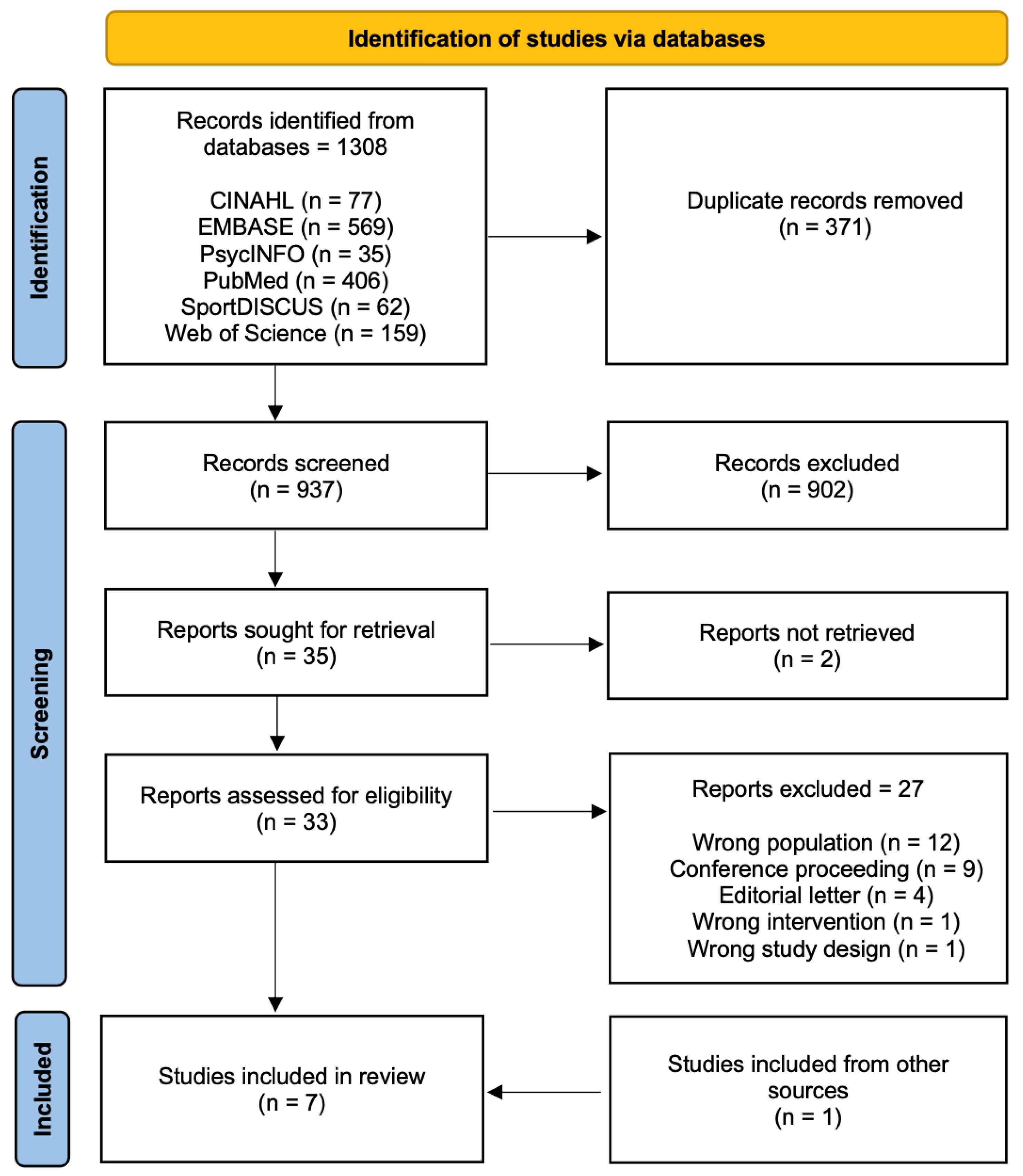
2.2. Search Strategy and Sources of Evidence
2.3. Data Extraction and Synthesis
2.4. Study Quality Assessment
3. Results
3.1. Overview of the Studies
3.2. Overview of the Risk of Bias
3.3. Study Findings
3.3.1. Physical Health findings
3.3.2. Mental Health Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ferkol, T.; Schraufnagel, D. The Global Burden of Respiratory Disease. Ann. Am. Thorac. Soc. 2014, 11, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, C.; Gott, M.; Payne, S.; Small, N.; Barnes, S.; Halpin, D.; Ruse, C.; Seamark, D. Exploring the Care Needs of Patients with Advanced COPD: An Overview of the Literature. Respir. Med. 2010, 104, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Yohannes, A.M.; Alexopoulos, G.S. Depression and Anxiety in Patients with COPD. Eur. Respir. Rev. 2014, 23, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Bu, F.; Philip, K.; Fancourt, D. Social Isolation and Loneliness as Risk Factors for Hospital Admissions for Respiratory Disease among Older Adults. Thorax 2020, 75, 597–599. [Google Scholar] [CrossRef] [PubMed]
- Yan, F.; Cobley, A.; Chan, S.; Pappas, C.; Nicholson, E.; Ward, L.L.; Murdoch, R.E.; Gu, R.E.; Vassallo, B.L.; Wewege, A.J.; et al. The Effectiveness of Dance Interventions on Physical Health Outcomes Compared to Other Forms of Physical Activity: A Systematic Review and Meta-Analysis. Sports Med 2018, 48, 933–951. [Google Scholar]
- Williams, M.T.; Lewis, L.K.; McKeough, Z.; Holland, A.E.; Lee, A.; McNamara, R.; Phillips, A.; Wiles, L.; Knapman, L.; Wootton, S.; et al. Reporting of Exercise Attendance Rates for People with Chronic Obstructive Pulmonary Disease: A Systematic Review: Exercise Attendance for People with COPD. Respirology 2014, 19, 30–37. [Google Scholar] [CrossRef]
- Fernandes-James, C.; Graham, C.D.; Batterham, A.M.; Harrison, S.L. Association of Psychological Flexibility with Engagement in Pulmonary Rehabilitation Following an Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Chron. Respir. Dis. 2019, 16, 1479973119880893. [Google Scholar] [CrossRef]
- Philip, K.E.J. Sing a Song of Lung Health-beyond the UK. BMJ 2019, 364, l652. [Google Scholar] [CrossRef]
- Hwang, P.W.-N.; Braun, K.L. The Effectiveness of Dance Interventions to Improve Older Adults’ Health: A Systematic Literature Review. Altern. Ther. Health Med. 2015, 21, 64–70. [Google Scholar]
- Hackney, M.E.; Earhart, G.M. Effects of Dance on Movement Control in Parkinson’s Disease: A Comparison of Argentine Tango and American Ballroom. J. Rehabil. Med. 2009, 41, 475–481. [Google Scholar] [CrossRef]
- Patterson, K.K.; Wong, J.S.; Prout, E.C.; Brooks, D. Dance for the Rehabilitation of Balance and Gait in Adults with Neurological Conditions Other than Parkinson’s Disease: A Systematic Review. Heliyon 2018, 4, e00584. [Google Scholar] [CrossRef] [PubMed]
- Patterson, K.K.; Wong, J.S.; Nguyen, T.-U.; Brooks, D. A Dance Program to Improve Gait and Balance in Individuals with Chronic Stroke: A Feasibility Study. Top. Stroke Rehabil. 2018, 25, 410–416. [Google Scholar] [CrossRef]
- Merom, D.; Ding, D.; Stamatakis, E. Dancing Participation and Cardiovascular Disease Mortality: A Pooled Analysis of 11 Population-Based British Cohorts. Am. J. Prev. Med. 2016, 50, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Belardinelli, R.; Lacalaprice, F.; Ventrella, C.; Volpe, L.; Faccenda, E. Waltz Dancing in Patients with Chronic Heart Failure: New Form of Exercise Training: New Form of Exercise Training. Circ. Heart Fail. 2008, 1, 107–114. [Google Scholar] [CrossRef]
- Hackney, M.E.; Hall, C.D.; Echt, K.V.; Wolf, S.L. Application of Adapted Tango as Therapeutic Intervention for Patients with Chronic Stroke. J. Geriatr. Phys. Ther. 2012, 35, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Koch, S.C.; Riege, R.F.F.; Tisborn, K.; Biondo, J.; Martin, L.; Beelmann, A. Effects of Dance Movement Therapy and Dance on Health-Related Psychological Outcomes. A Meta-Analysis Update. Front. Psychol. 2019, 10, 1806. [Google Scholar] [CrossRef]
- Murrock, C.J.; Graor, C.H. Effects of Dance on Depression, Physical Function, and Disability in Underserved Adults. J. Aging Phys. Act. 2014, 22, 380–385. [Google Scholar] [CrossRef]
- Rodrigues-Krause, J.; Krause, M.; Reischak-Oliveira, A. Dancing for Healthy Aging: Functional and Metabolic Perspectives. Altern. Ther. Health Med. 2019, 25, 44–63. [Google Scholar]
- Sharp, K.; Hewitt, J. Dance as an Intervention for People with Parkinson’s Disease: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2014, 47, 445–456. [Google Scholar] [CrossRef]
- Shanahan, J.; Morris, M.E.; Bhriain, O.N.; Saunders, J.; Clifford, A.M. Dance for People with Parkinson Disease: What Is the Evidence Telling Us? Arch. Phys. Med. Rehabil. 2015, 96, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Hackney, M.E.; Kantorovich, S.; Levin, R.; Earhart, G.M. Effects of Tango on Functional Mobility in Parkinson’s Disease: A Preliminary Study. J. Neurol. Phys. Ther. 2007, 31, 173–179. [Google Scholar] [CrossRef]
- Jeong, Y.-J.; Hong, S.-C.; Lee, M.S.; Park, M.-C.; Kim, Y.-K.; Suh, C.-M. Dance Movement Therapy Improves Emotional Responses and Modulates Neurohormones in Adolescents with Mild Depression. Int. J. Neurosci. 2005, 115, 1711–1720. [Google Scholar] [CrossRef] [PubMed]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S. The Well-Built Clinical Question: A Key to Evidence-Based Decisions. ACP J. Club 1995, 123, A12–A13. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 2013. [Google Scholar]
- Study Quality Assessment Tools. Nih.gov. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 2 May 2022).
- Philip, K.E.J.; Lewis, A.; Williams, S.; Buttery, S.C.; Polkey, M.I.; Man, W.; Fancourt, D.; Hopkinson, N.S. Dance for People with Chronic Respiratory Disease: A Qualitative Study. BMJ Open 2020, 10, e038719. [Google Scholar] [CrossRef]
- Gardiner, L.; Shannon, H.; Osman, L. Dance-Based versus Conventional Exercise in Pulmonary Rehabilitation: A Retrospective Service Evaluation. Physiotherapy 2021, 113, e54. [Google Scholar] [CrossRef]
- Harrison, S.; Bierski, K.; Burn, N.; Mclusky, S.; McFaull, V.; Russell, A.; Williams, G.; Williams, S.; Macnaughton, J. Dance for People with Chronic Breathlessness: A Transdisciplinary Approach to Intervention Development. BMJ Open Respir. Res. 2020, 7, e000696. [Google Scholar] [CrossRef]
- Wshah, A.; Butler, S.; Patterson, K.; Goldstein, R.; Brooks, D. Let’s Boogie": Feasibility of a Dance Intervention in Patients with Chronic Obstructive Pulmonary Disease. J. Cardiopulm. Rehabil. Prev. 2019, 39, E14–E19. [Google Scholar] [CrossRef]
- Philip, K.E.; Cartwright, L.L.; Westlake, D.; Nyakoojo, G.; Kimuli, I.; Kirenga, B.; Brakema, E.A.; Orme, M.W.; Fancourt, D.; Hopkinson, N.S.; et al. Music and Dance in Respiratory Disease Management in Uganda: A Qualitative Study of Patient and Healthcare Professional Perspectives. BMJ Open 2021, 11, e053189. [Google Scholar] [CrossRef]
- Schwartz, A.E.; Beemer, L.R.; Ajibewa, T.A.; Scott-Andrews, K.Q.; Lewis, T.C.; Robinson, L.E.; Hasson, R.E. Psychological Responses to Intermittent Activities in Children with and without Asthma. Pediatr. Exerc. Sci. 2022, 1–10. [Google Scholar] [CrossRef]
- Goodill, S.W. Dance/Movement Therapy for Adults with Cystic Fibrosis: Pilot Data on Mood and Adherence. Altern. Ther. Health Med. 2005, 11, 76–77. [Google Scholar] [PubMed]
- Fischer, M.J.; Scharloo, M.; Abbink, J.J.; van ’t Hul, A.J.; van Ranst, D.; Rudolphus, A.; Weinman, J.; Rabe, K.F.; Kaptein, A.A. Drop-out and Attendance in Pulmonary Rehabilitation: The Role of Clinical and Psychosocial Variables. Respir. Med. 2009, 103, 1564–1571. [Google Scholar] [CrossRef] [PubMed]
- May, T.; Chan, E.S.; Lindor, E.; McGinley, J.; Skouteris, H.; Austin, D.; McGillivray, J.; Rinehart, N.J. Physical, Cognitive, Psychological and Social Effects of Dance in Children with Disabilities: Systematic Review and Meta-Analysis. Disabil. Rehabil. 2021, 43, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Kiepe, M.-S.; Stöckigt, B.; Keil, T. Effects of Dance Therapy and Ballroom Dances on Physical and Mental Illnesses: A Systematic Review. Arts Psychother. 2012, 39, 404–411. [Google Scholar] [CrossRef]
- Ghram, A.; Briki, W.; Mansoor, H.; Al-Mohannadi, A.S.; Lavie, C.J.; Chamari, K. Home-Based Exercise Can Be Beneficial for Counteracting Sedentary Behavior and Physical Inactivity during the COVID-19 Pandemic in Older Adults. Postgrad. Med. 2021, 133, 469–480. [Google Scholar] [CrossRef]
- Chaabene, H.; Prieske, O.; Herz, M.; Moran, J.; Höhne, J.; Kliegl, R.; Ramirez-Campillo, R.; Behm, D.G.; Hortobágyi, T.; Granacher, U. Home-Based Exercise Programmes Improve Physical Fitness of Healthy Older Adults: A PRISMA-Compliant Systematic Review and Meta-Analysis with Relevance for COVID-19. Ageing Res. Rev. 2021, 67, 101265. [Google Scholar] [CrossRef]
- Singh, B.; Zopf, E.M.; Howden, E.J. Effect and Feasibility of Wearable Physical Activity Trackers and Pedometers for Increasing Physical Activity and Improving Health Outcomes in Cancer Survivors: A Systematic Review and Meta-Analysis. J. Sport Health Sci. 2022, 11, 184–193. [Google Scholar] [CrossRef]
- Gallou-Guyot, M.; Nuic, D.; Mandigout, S.; Compagnat, M.; Welter, M.L.; Daviet, J.C.; Perrochon, A. Effectiveness of Home-Based Rehabilitation Using Active Video Games on Quality of Life, Cognitive and Motor Functions in People with Parkinson’s Disease: A Systematic Review. Disabil. Rehabil. 2022, 1–12. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: Web Annex: Evidence Profiles; World Health Organization: Geneve, Switzerland, 2020. [Google Scholar]
- Physical Activity Guidelines. HSE.ie. Available online: https://www.hse.ie/eng/about/who/healthwellbeing/our-priority-programmes/heal/physical-activity-guidelines/ (accessed on 19 August 2022).
- O’Mahony, C. Sport Ireland Publishes Policy on Sport and Physical Activity in the Outdoors. Sport Ireland. Available online: https://www.sportireland.ie/outdoors/news/sport-ireland-publishes-policy-on-sport-and-physical-activity-in-the-outdoors (accessed on 19 August 2022).
- Hokkanen, L.; Rantala, L.; Remes, A.M.; Härkönen, B.; Viramo, P.; Winblad, I. Dance and Movement Therapeutic Methods in Management of Dementia: A Randomized, Controlled Study: Letters to the Editor. J. Am. Geriatr. Soc. 2008, 56, 771–772. [Google Scholar] [CrossRef]
- Murrock, C.J.; Higgins, P.A.; Killion, C. Dance and Peer Support to Improve Diabetes Outcomes in African American Women. Diabetes Educ. 2009, 35, 995–1003. [Google Scholar] [CrossRef]
- Hackney, M.E.; Earhart, G.M. Health-Related Quality of Life and Alternative Forms of Exercise in Parkinson Disease. Parkinsonism Relat. Disord. 2009, 15, 644–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Author(s), Year | Country | Setting | Study Design and Data Collection Method | Sample Characteristics | Health Condition | Intervention | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Size | Age | Gender | Type | Weekly Sessions | Total Duration | |||||
| Gardiner et al., 2020 [28] | UK | Urban health Centre | Experimental pre–post. Survey | 4 | 69 ± N/A | 4F | 4 × COPD | Latin-style dance | 2 × 60 min | 8 weeks |
| Goodill 2005 [33] | USA | Urban hospital | Experimental pre–post. Survey | 42 | 17 or older | N/A | CF | Dance and movement therapy | 1 × 60 min | 3 sessions |
| Harrison et al., 2020 [29] | UK | Urban health centre | Experimental mixed method. Survey | 8 | 70 ± 24 | 7F, 1M | N/A | Dance | 1 × 90 min | 10 weeks |
| Philip et al., 2021 [31] | Uganda | Urban health centre | Cross-sectional (qualitative). Semistructured interviews | 11 | 43 (20–63) | 8F, 3M | 6 × PTBLD 1 × post-infection LD 2 × asthma 1 × COPD 1 × pulmonary fibrosis | Singing and dancing | 1 × 20–40 min | N/A |
| Philip et al., 2020 [27] | UK | Urban health centre | Cross-sectional (qualitative). Semi-structured interviews | 8 | 75 ± N/A | N/A | 5 × COPD 2 × asthma 1 × bronchiectasis | Group dance | 1 × 75 min | N/A |
| Schwartz et al., 2022 [32] | USA | Urban | Experimental pre–post. Survey | 17 | 11.1 ± 0.6 | 8F, 9M | Asthma | Just dance | 1 × 5 min | 1 session |
| Wshah et al., 2019 [30] | Canada | Urban health centre | Experimental pre–post. Survey | 20 | 73.4 ± 7.6 | 14F, 6M | 20 × COPD | Dance | 2 × 60 min | 8 weeks |
| Quality Assessment Tool for before–after (Pre–Post) Studies with No Control Group | |||||||
|---|---|---|---|---|---|---|---|
| Criteria | Gardiner et al., 2020 [28] | Goodill 2005 [33] | Harrison et al., 2020 [29] | Philip et al., 2020 [31] | Philip et al., 2021 [27] | Schwartz et al., 2022 [32] | Wshah et al., 2019 [30] |
| 1. Study question clear | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 2. Selection of the population clearly described | Yes | CD | No | Yes | Yes | Yes | Yes |
| 3. Participant representative of the population | Yes | Yes | CD | Yes | Yes | Yes | Yes |
| 4. Participant meeting entry criteria | Yes | Yes | CD | Yes | Yes | Yes | Yes |
| 5. Adequate sample size | No | Yes | No | Yes | Yes | Yes | Yes |
| 6. Intervention clearly described and delivered | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7. Outcome measures clearly defined and valid | Yes | Yes | Yes | NA | NA | Yes | Yes |
| 8. People assessing the outcome blinded to exposure | No | No | CD | No | No | No | No |
| 9. Loss to follow-up less than 20% | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 10. Adequate analysis | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 11. Outcome measures taken multiple times before and after intervention | No | Yes | No | No | No | NA | NA |
| 12. Intervention taken at a group level with appropriate statistical analysis | NA | No | Yes | Na | NA | Yes | NA |
| Total Score | 8 | 7 | 6 | 8 | 8 | 10 | 9 |
| Quality Rating | Fair | Fair | Fair | Fair | Fair | Good | Good |
| Study | Physical Health Findings | Mental Health Findings | ||||
|---|---|---|---|---|---|---|
| Functional Exercise Capacity | Respiratory Capacity | Other Physical Health Findings | Anxiety | Depression | Other Mental Health Findings | |
| Gardiner et al., 2020 [28] | ISWT, 6MWT, handgrip | CAT, dyspnoea | HADS Anxiety | HADS Depression | ||
| Goodill 2005 [33] | POMS | |||||
| Harrison et al., 2020 [29] | 6MWT, TUG, 30-STS | CAT | Physical benefits | GAD-7 | PHQ-9 | MAIA, social benefits, enjoyment |
| Philip et al., 2021 [31] | Physical health, health benefits | Social benefits, appropriateness, enjoyment, mental health | ||||
| Philip et al., 2020 [27] | Experience of respiratory illness and impact on life; experience of dance group; perceived impacts of dance group participation | |||||
| Schwartz et al., 2022 [32] | In-task RPE, HR reserve | In-task mood and enjoyment | ||||
| Wshah et al., 2019 [30] | 6MWT, BEST-est, BBS, ABC Scale, step count | Dyspnoea | Fatigue | HADS Anxiety | HADS Depression | HR-CRDQ, emotional function |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niranjan, V.; Tarantino, G.; Kumar, J.; Stokes, D.; O’Connor, R.; O’Regan, A. The Impact of Dance Interventions on Patients with Noninfectious Pulmonary Diseases: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 11115. https://doi.org/10.3390/ijerph191711115
Niranjan V, Tarantino G, Kumar J, Stokes D, O’Connor R, O’Regan A. The Impact of Dance Interventions on Patients with Noninfectious Pulmonary Diseases: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(17):11115. https://doi.org/10.3390/ijerph191711115
Chicago/Turabian StyleNiranjan, Vikram, Giampiero Tarantino, Jaspal Kumar, Diarmuid Stokes, Ray O’Connor, and Andrew O’Regan. 2022. "The Impact of Dance Interventions on Patients with Noninfectious Pulmonary Diseases: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 17: 11115. https://doi.org/10.3390/ijerph191711115
APA StyleNiranjan, V., Tarantino, G., Kumar, J., Stokes, D., O’Connor, R., & O’Regan, A. (2022). The Impact of Dance Interventions on Patients with Noninfectious Pulmonary Diseases: A Systematic Review. International Journal of Environmental Research and Public Health, 19(17), 11115. https://doi.org/10.3390/ijerph191711115






