Aerobic or Resistance Exercise for Improved Glycaemic Control and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
- -
- Participants: women, pregnancy, gestational diabetes, hyperglycaemia, diabetes
- -
- Intervention: exercise, aerobic, resistance
- -
- Comparison: physical activity, aerobic, resistance, control
- -
- Outcome: medication (insulin, metformin), glycaemic control, maternal outcome
- Randomised controlled trials
- Gestational diabetes mellitus
- Intervention of resistance exercise or aerobic exercise alone or in combination
- Comparator or control of either resistance, aerobic or no exercise
- Review or opinion articles
- Studies without published results
- Studies involving women with pre-existing diabetes
2.2. Study Selection
2.3. Data Extraction
2.4. Quality Assessment
3. Results
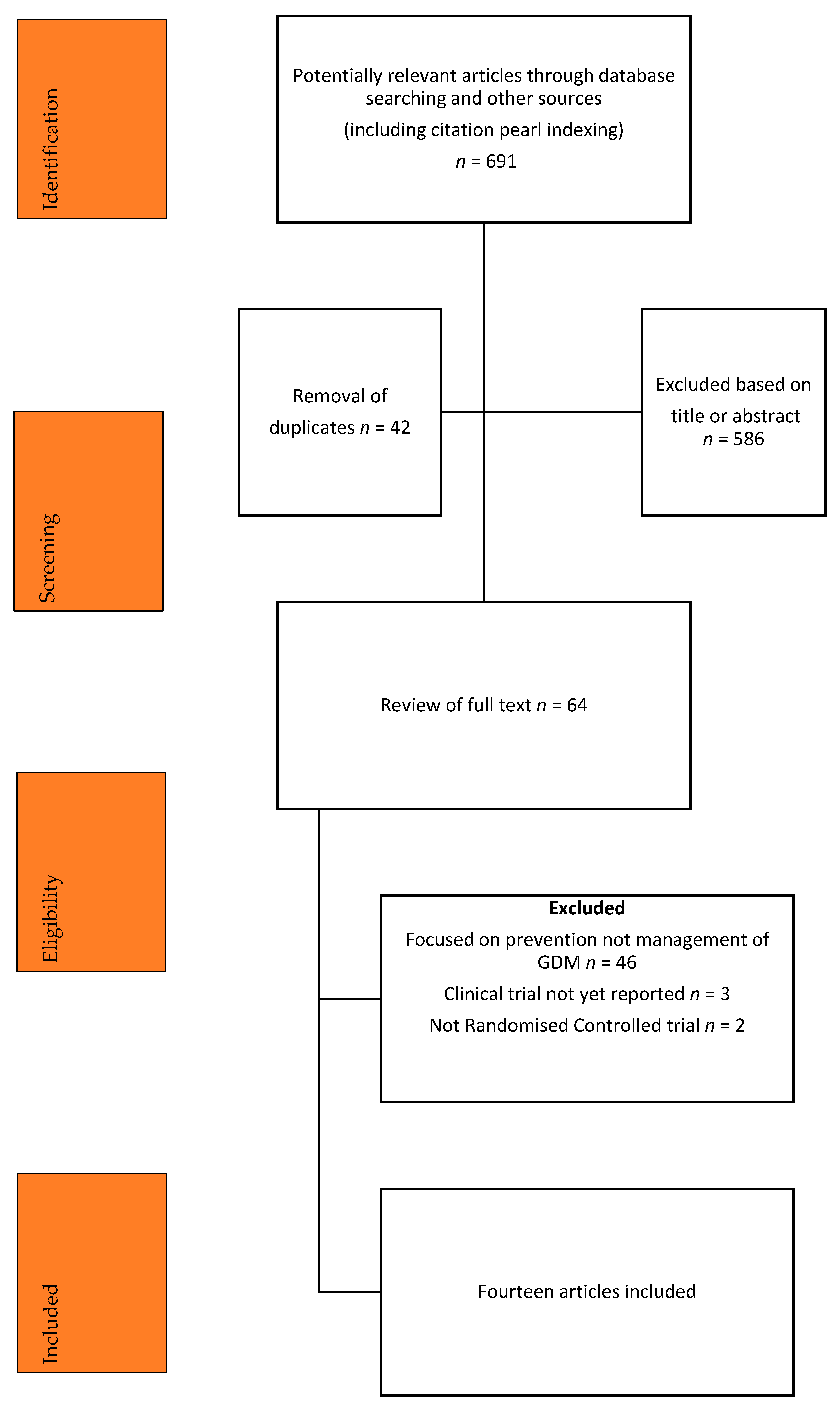
3.1. Literature Search
3.2. Characteristics
3.3. Fasting Glucose
3.4. Postprandial Glucose
3.5. Average Glucose
3.6. HbA1C
3.7. Insulin Use
3.8. Maternal Hypoglycaemia
3.9. Caesarean Section
3.10. Induction of Labour Rates and Labour Duration
3.11. Other Outcomes
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021, 44 (Suppl. 1), S200–S210. [Google Scholar]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar]
- Khalifeh, A.; Breathnach, F.; Coulter-Smith, S.; Robson, M.; Fitzpatrick, C.; Malone, F. Changing trends in diabetes mellitus in pregnancy. J. Obstet. Gynaecol. 2014, 34, 135–137. [Google Scholar] [CrossRef]
- Egan, A.M.; Dennedy, M.C.; Al-Ramli, W.; Heerey, A.; Avalos, G.; Dunne, F. ATLANTIC-DIP: Excessive gestational weight gain and pregnancy outcomes in women with gestational or pregestational diabetes mellitus. J. Clin. Endocrinol. Metab. 2014, 99, 212–219. [Google Scholar]
- Bogdanet, D.; Egan, A.; Reddin, C.; Kirwan, B.; Carmody, L.; Dunne, F. ATLANTIC DIP: Despite insulin therapy in women with IADPSG diagnosed GDM, desired pregnancy outcomes are still not achieved. What are we missing? Diabetes Res. Clin. Pract. 2018, 136, 116–123. [Google Scholar]
- Lowe, W.L.; Scholtens, D.M.; Lowe, L.P.; Kuang, A.; Nodzenski, M.; Talbot, O.; Catalano, P.M.; Linder, B.; Brickman, W.J.; Clayton, P.; et al. Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA 2018, 320, 1005–1016. [Google Scholar]
- Kgosidialwa, O.; Egan, A.M.; Carmody, L.; Kirwan, B.; Gunning, P.; Dunne, F.P. Treatment with diet and exercise for women with gestational diabetes mellitus diagnosed using IADPSG criteria. J. Clin. Endocrinol. Metab. 2015, 100, 4629–4636. [Google Scholar]
- Wang, C.; Zhu, W.; Wei, Y.; Feng, H.; Su, R.; Yang, H. Exercise intervention during pregnancy can be used to manage weight gain and improve pregnancy outcomes in women with gestational diabetes mellitus. BMC Pregnancy Childbirth 2015, 15, 255. [Google Scholar] [CrossRef]
- Hayashi, A.; Oguchi, H.; Kozawa, Y.; Ban, Y.; Shinoda, J.; Suganuma, N. Daily walking is effective for the management of pregnant women with gestational diabetes mellitus. J. Obstet. Gynaecol. Res. 2018, 44, 1731–1738. [Google Scholar] [CrossRef]
- Umpierre, D.; Ribeiro, P.A.; Kramer, C.K.; Leitão, C.B.; Zucatti, A.T.; Azevedo, M.J.; Gross, J.L.; Ribeiro, J.P.; Schaan, B.D. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: A systematic review and meta-analysis. JAMA 2011, 305, 1790–1799. [Google Scholar] [CrossRef]
- Röhling, M.; Herder, C.; Roden, M.; Stemper, T.; Müssig, K. Effects of Long-Term Exercise Interventions on Glycaemic Control in Type 1 and Type 2 Diabetes: A Systematic Review. Exp. Clin. Endocrinol. Diabetes 2016, 124, 487–494. [Google Scholar] [CrossRef]
- Yang, Z.; Scott, C.A.; Mao, C.; Tang, J.; Farmer, A.J. Resistance exercise versus aerobic exercise for type 2 diabetes: A systematic review and meta-analysis. Sports Med. 2014, 44, 487–499. [Google Scholar] [CrossRef]
- Ryan, A.S.; Pratley, R.E.; Elahi, D.; Goldberg, A.P. Changes in plasma leptin and insulin action with resistive training in postmenopausal women. Int. J. Obes. 2000, 24, 27–32. [Google Scholar]
- Miller, J.P.; Pratley, R.E.; Goldberg, A.P.; Gordon, P.; Rubin, M.; Treuth, M.S.; Ryan, A.S.; Hurley, B.F. Strength training increases insulin action in healthy 50- to 65-yr-old men. J. Appl. Physiol. 1994, 77, 1122–1127. [Google Scholar] [CrossRef]
- Stewart, K.J. Role of exercise training on cardiovascular disease in persons who have type 2 diabetes and hypertension. Cardiol. Clin. 2004, 22, 569–586. [Google Scholar] [CrossRef]
- Syngelaki, A.; Sequeira Campos, M.; Roberge, S.; Andrade, W.; Nicolaides, K.H. Diet and exercise for preeclampsia prevention in overweight and obese pregnant women: Systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2019, 32, 3495–3501. [Google Scholar] [CrossRef]
- Magro-Malosso, E.R.; Saccone, G.; Di Tommaso, M.; Roman, A.; Berghella, V. Exercise during pregnancy and risk of gestational hypertensive disorders: A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2017, 96, 921–931. [Google Scholar] [CrossRef] [Green Version]
- Almousa, S.; Lamprianidou, E.; Kitsoulis, G. The effectiveness of stabilising exercises in pelvic girdle pain during pregnancy and after delivery: A systematic review. Physiother. Res. Int. 2018, 23, e1699. [Google Scholar] [CrossRef]
- Davenport, M.H.; Marchand, A.A.; Mottola, M.F.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Sobierajski, F.; James, M.; Meah, V.L.; et al. Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 90–98. [Google Scholar] [CrossRef]
- Hu, X.; Ma, M.; Zhao, X.; Sun, W.; Liu, Y.; Zheng, Z.; Xu, L. Effects of exercise therapy for pregnancy-related low back pain and pelvic pain: A protocol for systematic review and meta-analysis. Medicine 2020, 99, e17318. [Google Scholar] [CrossRef]
- Magro-Malosso, E.R.; Saccone, G.; Di Mascio, D.; Di Tommaso, M.; Berghella, V. Exercise during pregnancy and risk of preterm birth in overweight and obese women: A systematic review and meta-analysis of randomized controlled trials. Acta Obstet. Gynecol. Scand. 2017, 96, 263–273. [Google Scholar] [CrossRef]
- Di Mascio, D.; Magro-Malosso, E.R.; Saccone, G.; Marhefka, G.D.; Berghella, V. Exercise during pregnancy in normal-weight women and risk of preterm birth: A systematic review and meta-analysis of randomized controlled trials. Am. J. Obstet. Gynecol. 2016, 215, 561–571. [Google Scholar] [CrossRef]
- Davenport, M.H.; Nagpal, T.S.; Mottola, M.F.; Skow, R.J.; Riske, L.; Poitras, V.J.; Jaramillo Garcia, A.; Gray, C.E.; Barrowman, N.; Meah, V.L.; et al. Prenatal exercise (including but not limited to pelvic floor muscle training) and urinary incontinence during and following pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1397–1404. [Google Scholar] [CrossRef]
- Woodley, S.J.; Lawrenson, P.; Boyle, R.; Cody, J.D.; Mørkved, S.; Kernohan, A.; Hay-Smith, E.J.C. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2020, 5, Cd007471. [Google Scholar] [CrossRef]
- Davenport, M.H.; McCurdy, A.P.; Mottola, M.F.; Skow, R.J.; Meah, V.L.; Poitras, V.J.; Jaramillo Garcia, A.; Gray, C.E.; Barrowman, N.; Riske, L.; et al. Impact of prenatal exercise on both prenatal and postnatal anxiety and depressive symptoms: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1376–1385. [Google Scholar] [CrossRef]
- Kołomańska, D.; Zarawski, M.; Mazur-Bialy, A. Physical Activity and Depressive Disorders in Pregnant Women-A Systematic Review. Medicina 2019, 55, 212. [Google Scholar] [CrossRef]
- Davenport, M.H.; Ruchat, S.M.; Poitras, V.J.; Jaramillo Garcia, A.; Gray, C.E.; Barrowman, N.; Skow, R.J.; Meah, V.L.; Riske, L.; Sobierajski, F.; et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1367–1375. [Google Scholar] [CrossRef]
- Yu, Y.; Xie, R.; Shen, C.; Shu, L. Effect of exercise during pregnancy to prevent gestational diabetes mellitus: A systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2018, 31, 1632–1637. [Google Scholar] [CrossRef]
- Ming, W.K.; Ding, W.; Zhang, C.J.P.; Zhong, L.; Long, Y.; Li, Z.; Sun, C.; Wu, Y.; Chen, H.; Chen, H.; et al. The effect of exercise during pregnancy on gestational diabetes mellitus in normal-weight women: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2018, 18, 440. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Bmj 2009, 339, b2535. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Keating, N.; Coveney, C. Aerobic or Resistance Exercise for Improved Glycaemic Control and Obstetric Outcomes in Women with Gestational Diabetes. A Protocol for a Systematic Review. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020161454 (accessed on 11 May 2021).
- Adam, C.; L’Abbe, C.; Lachapelle, J.; Ourabah, S.; Rakel, A.; De Guise, M. Impact of an individualised counselling on physical activity in women with Gestational Diabetes: Interim analysis of a randomised controlled trial. Endocr. Rev. 2014, 35, SUN-1035. [Google Scholar]
- Avery, M.D.; Leon, A.S.; Kopher, R.A. Effects of a partially home-based exercise program for women with gestational diabetes. Obstet. Gynecol. 1997, 89, 10–15. [Google Scholar] [CrossRef]
- Bambicini, J.T.; Soares, V.C.M.; Zanetti, M.R.D.; Torloni, M.R.; Ribeiro, M.C.; Mattar, R. M221 effects of aerobic and resistance exercises on glycemic levels of patients with gestational diabetes: Pilot study. Int. J. Gynecol. Obstet. 2012, 119, S603. [Google Scholar]
- Bo, S.; Rosato, R.; Ciccone, G.; Canil, S.; Gambino, R.; Poala, C.B.; Leone, F.; Valla, A.; Grassi, G.; Ghigo, E.; et al. Simple lifestyle recommendations and the outome of gestational diabetes. A 2 × 2 factorial randomized trial. Diabetes Obes. Metab. 2014, 16, 1032. [Google Scholar]
- Brankston, G.N.; Mitchell, B.F.; Ryan, E.A.; Okun, N.B. Resistance exercise decreases the need for insulin in overweight women with gestational diabetes mellitus. Am. J. Obstet. Gynecol. 2004, 190, 188–193. [Google Scholar] [CrossRef]
- Bung, P.; Artal, R.; Khodiguian, N.; Kjos, S. Exercise in gestational diabetes. An optional therapeutic approach? Diabetes 1991, 40 (Suppl. 2), 182–185. [Google Scholar] [CrossRef]
- De Barros, M.C.; Lopes, M.A.; Francisco, R.P.; Sapienza, A.D.; Zugaib, M. Resistance exercise and glycaemic control in women with gestational daibetes mellitus. Am. J. Obstet. Gynecol. 2010, 203, e551–e556. [Google Scholar]
- Halse, R.E.; Wallman, K.E.; Newnham, J.P.; Guelfi, K.J. Home-based exercise training improves capillary glucose profile in women with gestational diabetes. Med. Sci. Sports Exerc. 2014, 46, 1702–1709. [Google Scholar] [CrossRef]
- Jovanovic-Peterson, L.; Durak, E.P.; Peterson, C.M. Randomized trial of diet versus diet plus cardiovascular conditioning on glucose levels in gestational diabetes. Am. J. Obstet. Gynecol. 1989, 161, 415–419. [Google Scholar] [CrossRef]
- Ramos, J.G.; Bgeginski, R.; Opperman, M.L.; Martins-Costa, S.; Delevatti, R.; Schuch, R.; Kruel, L.F. Effect of aerobic training in pregnant women diagnosed with gestational diabetes: A preliminary report. Pregnancy Hypertens 2015, 5, 105. [Google Scholar]
- Qadir, D.E.W. Effects of structured exercise on HbA1c level in Gestational Diabetes Mellitus—A Pilot Study. Int. J. Gynecol. Obstet. 2018, 143, 569–579. [Google Scholar]
- Sklempe Kokic, I.; Ivanisevic, M.; Kokic, T.; Simunic, B.; Pisot, R. Acute responses to structured aerobic and resistance exercise in women with gestational diabetes mellitus. Scand. J. Med. Sci. Sports 2018, 28, 1793–1800. [Google Scholar] [CrossRef]
- Youngwanichsetha, S.; Phumdoung, S.; Ingkathawornwong, T. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl. Nurs. Res. 2014, 27, 227–230. [Google Scholar] [CrossRef]
- Halse, R.E.; Wallman, K.E.; Dimmock, J.A.; Newnham, J.P.; Guelfi, K.J. Home-Based Exercise Improves Fitness and Exercise Attitude and Intention in Women with GDM. Med. Sci. Sports Exerc. 2015, 47, 1698–1704. [Google Scholar] [CrossRef]
- Awad, E.; Ahmed, H.; Yousef, A.; Saab, I.M. Effect of antenatal exercise on mode of delivery in gestational diabetic females: A single-blind randomized controlled trial. Physiother. Q. 2019, 27, 1–5. [Google Scholar] [CrossRef]
- Hawley, J.A.; Lessard, S.J. Exercise training-induced improvements in insulin action. Acta Physiol. 2008, 192, 127–135. [Google Scholar] [CrossRef]
- Abd El-Kader, S.M. Aerobic versus resistance exercise training in modulation of insulin resistance, adipocytokines and inflammatory cytokine levels in obese type 2 diabetic patients. J. Adv. Res. 2011, 2, 179–183. [Google Scholar]
- Maiorana, A.; O’Driscoll, G.; Goodman, C.; Taylor, R.; Green, D. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diabetes Res. Clin. Pract. 2002, 56, 115–123. [Google Scholar] [CrossRef]
- Barakat, R.; Pelaez, M.; Cordero, Y.; Perales, M.; Lopez, C.; Coteron, J.; Mottola, M.F. Exercise during pregnancy protects against hypertension and macrosomia: Randomized clinical trial. Am. J. Obstet. Gynecol. 2016, 214, 649.e1–649.e8. [Google Scholar] [CrossRef]
- Beetham, K.S.; Giles, C.; Noetel, M.; Clifton, V.; Jones, J.C.; Naughton, G. The effects of vigorous intensity exercise in the third trimester of pregnancy: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2019, 19, 281. [Google Scholar] [CrossRef]
- The International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. BMJ 2017, 358, j3119. [Google Scholar] [CrossRef]
- Physical Activity and Exercise During Pregnancy and the Postpartum Period: ACOG Committee Opinion, Number 804. Obstet Gynecol. 2020, 135, e178–e188.
- Duncombe, D.; Wertheim, E.H.; Skouteris, H.; Paxton, S.J.; Kelly, L. Factors related to exercise over the course of pregnancy including women’s beliefs about the safety of exercise during pregnancy. Midwifery 2009, 25, 430–438. [Google Scholar]
- Bauer, P.W.; Broman, C.L.; Pivarnik, J.M. Exercise and pregnancy knowledge among healthcare providers. J. Womens Health 2010, 19, 335–341. [Google Scholar] [CrossRef]
- Wiebe, H.W.; Boule, N.G.; Chari, R.; Davenport, M.H. The effect of supervised prenatal exercise on fetal growth: A meta-analysis. Obstet. Gynecol. 2015, 125, 1185–1194. [Google Scholar] [CrossRef]
- Wang, C.; Wei, Y.; Zhang, X.; Zhang, Y.; Xu, Q.; Sun, Y.; Su, S.; Zhang, L.; Liu, C.; Feng, Y.; et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am. J. Obstet. Gynecol. 2017, 216, 340–351. [Google Scholar] [CrossRef]
- Daly, N.; Farren, M.; McKeating, A.; O’Kelly, R.; Stapleton, M.; Turner, M.J. A Medically Supervised Pregnancy Exercise Intervention in Obese Women: A Randomized Controlled Trial. Obstet. Gynecol. 2017, 130, 1001–1010. [Google Scholar] [CrossRef]
- Nobles, C.; Marcus, B.H.; Stanek, E.J., 3rd; Braun, B.; Whitcomb, B.W.; Solomon, C.G.; Manson, J.E.; Markenson, G.; Chasan-Taber, L. Effect of an exercise intervention on gestational diabetes mellitus: A randomized controlled trial. Obstet Gynecol. 2015, 125, 1195–1204. [Google Scholar]
- The HAPO Study Cooperative Research Group. Hyperglycaemia and Adverse Pregnancy Outcomes. N. Engl. J. Med. 2008, 358, 1991–2002. [Google Scholar]
- Billionnet, C.; Mitanchez, D.; Weill, A.; Nizard, J.; Alla, F.; Hartemann, A.; Jacqueminet, S. Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012. Diabetologia 2017, 60, 636–644. [Google Scholar]
- Egan, A.M.; Bogdanet, D.; Griffin, T.P.; Kgosidialwa, O.; Cervar-Zivkovic, M.; Dempsey, E.; Allotey, J.; Alvarado, F.; Clarson, C.; Cooray, S.D.; et al. A core outcome set for studies of gestational diabetes mellitus prevention and treatment. Diabetologia 2020, 63, 1120–1127. [Google Scholar] [CrossRef]
- Cremona, A.; O’Gorman, C.; Cotter, A.; Saunders, J.; Donnelly, A. Effect of exercise modality on markers of insulin sensitivity and blood glucose control in pregnancies complicated with gestational diabetes mellitus: A systematic review. Obes. Sci. Pract. 2018, 4, 455–467. [Google Scholar]
- Huang, X.; Huang, J.; Wu, J.; Li, M.; Yang, Z.; Liu, L.; Lin, T.; Lan, Y.; Chen, K. Different exercises for pregnant women with gestational diabetes: A meta-analysis of randomized controlled trials. J. Sports Med. Phys. Fitness 2020, 60, 464–471. [Google Scholar]
- Brown, J.; Ceysens, G.; Boulvain, M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst. Rev. 2017, 6, Cd012202. [Google Scholar] [CrossRef]
- Harrison, A.L.; Shields, N.; Taylor, N.F.; Frawley, H.C. Exercise improves glycaemic control in women diagnosed with gestational diabetes mellitus: A systematic review. J. Physiother. 2016, 62, 188–196. [Google Scholar]
- Bgeginski, R.; Ribeiro, P.A.B.; Mottola, M.F.; Ramos, J.G.L. Effects of weekly supervised exercise or physical activity counseling on fasting blood glucose in women diagnosed with gestational diabetes mellitus: A systematic review and meta-analysis of randomized trials. J. Diabetes 2017, 9, 1023–1032. [Google Scholar] [CrossRef]
- Allehdan, S.S.; Basha, A.S.; Asali, F.F.; Tayyem, R.F. Dietary and exercise interventions and glycemic control and maternal and newborn outcomes in women diagnosed with gestational diabetes: Systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2775–2784. [Google Scholar] [CrossRef]
| Parameter | Inclusion | Exclusion |
|---|---|---|
| Population/ participant | Women Pregnancy Gestational diabetes Hyperglycaemia Diabetes in pregnancy Treatment of Gestational Diabetes | Pre-gestational Diabetes Type 1 Diabetes Type 2 Diabetes Prevention of Gestational Diabetes |
| Intervention | Exercise, aerobic, resistance Lasting at least two weeks | |
| Comparison | Normal physical activity Aerobic exercise Resistance Control Lasting at least two weeks | |
| Outcome | Glycaemic control Maternal outcomes | |
| Study Design | Randomised controlled trial No language restriction Published paper Published abstract | Case report Case-control study Cohort study Commentary Guideline |
| Author of RCT; Year Published Country | Sample Characteristics | Duration of Intervention | Intervention (Exercise) Characteristics | Outcomes |
|---|---|---|---|---|
| Adam 2014 [34] | Control n − 4 Intervention n = 39 | Duration of pregnancy | Standard counselling for physical activity Supervised individuals follow up with kinesiologist | Addition of insulin Mean dose of insulin Time to start insulin Weight gain |
| Avery 1997 [35] United States | Control n = 14 GDM diagnosis 26.3 ± 8 weeks Intervention n = 15 GDM diagnosis 28.7 ± 3 weeks | Six weeks | Usual physical activity 30 min supervised cycling with 30 min unsupervised walking | Addition of insulin Caesarean birth Hypertensive disorders Maternal weight gain |
| Awad 2019 [48] Egypt | Control n = 30 Diet plus insulin Intervention n = 30 Moderate intensity aerobic and circuit resistance exercise 3–4 times/week in addition to diet plus insulin | 24 weeks’ gestation until delivery | Diet plus insulin alone compared with combined strength and aerobic exercise plus diet plus insulin | Mode of delivery |
| Bambicini 2012 [36] | Control n = 6 Intervention (aerobic) n = 6 Intervention (resistance) n = 5 | Duration of pregnancy | Seated listening to explanations about exercise Aerobic or resistance exercises | Mean glucose immediately after session and one hour later |
| Bo 2014 [37] Italy | Control n = 99 GDM diagnosis 24–26 weeks Intervention n = 101 GDM diagnosis 24–26 weeks | 12–14 weeks | Not applicable Twenty minutes of unsupervised brisk walking seven times a week | Addition of insulin Caesarean birth Glycaemic control |
| Brankston 2004 [38] Canada | Control n = 16 GDM diagnosis: not reported Intervention n = 16 GDM diagnosis: not reported | Eight weeks | Usual physical activity Resistance exercise on circuit: supervised for three sessions then supervised for three sessions per week | Additional medications Glycaemic control |
| Bung 1991 [39] United States | Control n = 17 GDM diagnosis: 30.3 ± 2 weeks Intervention n = 17 GDM diagnosis: 30.3 ± 1.9 weeks Note: control was diet and insulin; diagnosis of GDM was persistent fasting glucose >5.88 mM but <7.22 mM and “failed diet therapy for a week” | Remainder of the pregnancy | Standard care Supervised in exercise laboratory: 45 min with breaks on recumbent bicycle | Adherence to intervention Caesarean birth Hypoglycaemia Glycaemic control |
| De Barros 2010 [40] Brazil | Control n = 32 GDM Diagnosis 27.5 ± 3 weeks Intervention n = 32 GDM Diagnosis 28.4 ± 2.5 weeks | Eight weeks | Usual physical activity Resistance exercise (two supervised and one unsupervised) for 30–40 min | Additional medications Caesarean birth Weight gain |
| Halse 2014 [41] Australia | Control n = 20 GDM Diagnosis 28.8 ± 1 week Intervention n = 20 GDM Diagnosis 28.9 ± 1 week | Six weeks | Usual physical activity Home cycle ergometer supervised three times a week and unsupervised for two sessions a week | Additional medications Caesarean birth Induction of labour Patient views Weight gain |
| Jovanovic-Peterson 1989 [42] United States | Control n = 9 GDM diagnosis at 28 weeks Intervention n = 10 GDM diagnosis at 28 weeks | Six weeks | Usual physical activity Aerobic exercise: 20 min for three times a week, supervised, using ergometer | Additional medications Adherence to intervention Hypertensive disorders Glycaemic control |
| Qadir 2018 [44] Singapore | Control n = 5 GDM “newly diagnosed” Intervention n = 5 GDM “newly diagnosed” | Eight weeks | Usual physical activity measured by pedometer Patient education and structured exercise class once a week Usual physical activity measured by pedometer | Average daily steps Glycaemic control |
| Ramos 2015 [43] | Control n = 4 Intervention n = 2 | Ten weeks | 50 min stretching and relaxation once a week 50 min aerobic session three times a week | Mean HbA1c Homeostatic model assessment (HOMA) |
| Sklempe Kocic 2018 [45] Croatia | Control n = 20 GDM diagnosis: 20.8 ± 6 weeks Intervention n = 18 GDM diagnosis 22.2 ± 6 weeks | Six weeks | Usual physical activity Combined aerobic and resistance exercise (two supervised sessions) plus seven sessions of unsupervised walking | Additional medications Caesarean Birth Glycaemic control Weight gain |
| Youngwanichsetha 2014 [46] Thailand | Control n = 85 GDM diagnosis: 24–30 weeks Intervention n = 85 GDM diagnosis: 24–30 weeks | Eight weeks | Not applicable Fifteen to twenty minutes of supervised yoga five times a week | Glycaemic control |
| Author of RCT; Year Published | Selection Bias (Random Sequence Generation) | Selection Bias (Allocation Concealment) | Performance Bias (Double Blinding) | Detection Bias (Blinding of Outcome Assessment) | Attrition Bias (Incomplete Outcome Data) | Reporting Bias (Selective Reporting) | Other Bias |
|---|---|---|---|---|---|---|---|
| Adam 2014 [34] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Avery 1997 [35] | Low | Unclear | High | Unclear | High | Unclear | Low |
| Awad 2019 [48] | Unclear | Unclear | High | Unclear | Unclear | Unclear | Low |
| Bambicini 2012 [36] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Bo 2014 [37] | Unclear | Low | High | Low | Low | Low | Low |
| Brankston 2004 [38] | Low | Low | High | High | Unclear | High | Unclear |
| Bung 1991 [39] | Unclear | Unclear | Unclear | Unclear | High | Unclear | Unclear |
| De Barros 2010 [40] | Low | Low | High | High | Low | Unclear | Low |
| Halse 2014 [41] | Unclear | Low | High | High | High | High | Low |
| Jovanovic-Peterson 1989 [42] | Low | Unclear | High | Unclear | Low | High | High |
| Qadir [44] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Ramos 2015 [43] | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Sklempe Kocic 2018 [45] | Low | Unclear | High | Low | Low | High | Low |
| Youngwanichsetha 2014 [46] | Unclear | Unclear | High | Low | Low | High | Low |
| Paper | Intervention | Sample Characteristics | Main Outcome | Findings |
|---|---|---|---|---|
| Adam et al. [34] | Standard counselling for physical activity compared with supervised individual follow up with kinesiologist | Control n − 40 Intervention n = 39 | Addition of insulin Mean dose of insulin Time to start insulin Weight gain | No difference |
| Avery et al. [35] | Usual physical activity compared with supervised cycling and unsupervised walking | Control n = 14 GDM diagnosis 26.3 ± 8 weeks Intervention n = 15 GDM diagnosis 28.7 ± 3 weeks | Addition of insulin Apgar < 7 at 1 min Apgar < 7 at 5 min Birthweight Caesarean birth Gestation at birth Hypertensive disorders Maternal weight gain | No difference in insulin requirement No difference in CS, hypertensive disorders |
| Awad et al. [48] | Diet plus insulin alone compared with combined strength and aerobic exercise plus diet plus insulin | Control n = 30 Diet plus insulin Intervention = 30 Moderate intensity aerobic and circuit resistance exercise 3–4 times/week in addition to diet plus insulin | Mode of delivery | Reduced CS rate in control group |
| Bambicini et al. [36] | Explanation about exercise compared with aerobic or strength-based exercise | Control n = 6 Intervention (aerobic) n = 6 Intervention (resistance) n = 5 | Mean glucose immediately after session and one hour later | No difference |
| Bo et al. [37] | Twenty minutes of brisk walking 7 times per week | Control n = 99 GDM diagnosis 24–26 weeks Intervention n = 101 GDM diagnosis 24–26 weeks | Addition of insulin Caesarean birth Glycaemic control | No difference in insulin requirements, CS, macrosomia, fasting glucose Reduction in postprandial glucose and HbA1C with intervention |
| Brankston et al. [38] | Usual physical activity Resistance exercise on circuit: supervised for three sessions then supervised for three sessions per week | Control n = 16 GDM diagnosis: not reported Intervention n = 16 GDM diagnosis: not reported | Additional medications Glycaemic control | Increased latency to insulin treatment in intervention group No difference in number of women requiring insulin or the dose used No difference in fasting or postprandial glucose levels |
| Bung et al. [39] | Standard care Supervised 45 min session on recumbent bicycle | Control n = 17 GDM diagnosis: 30.3 ± 2 weeks Intervention n = 17 GDM diagnosis: 30.3 ± 1.9 weeks Note: control was diet and insulin; diagnosis of GDM was persistent fasting glucose >5.88 mM but <7.22 mM and “failed diet therapy for a week” | Adherence intervention Caesarean birth Hypoglycaemia Glycaemic control | No difference in CS, average glucose levels |
| De Barros et al. [40] | Usual physical activity Resistance exercise (two supervised and one unsupervised) for 30–40 min | Control n = 32 GDM Diagnosis 27.5 ± 3 weeks Intervention n = 32 GDM Diagnosis 28.4 ± 2.5 weeks | Additional medications Caesarean birth Weight gain | No difference in latency to use of insulin or dose required Reduction in number of women requiring insulin No difference in caesarean section |
| Halse et al. [41] | Usual physical activity Home cycle ergometer supervised three times a week and unsupervised for two sessions a week | Control n = 20 GDM Diagnosis 28.8 ± 1 week Intervention n = 20 GDM Diagnosis 28.9 ± 1 week | Compliance, maternal attitudes to exercise, aerobic fitness, onset of labour, mode of delivery, duration of labour | No difference in maternal obstetric outcomes, improved fitness, attitude, and exercise intention |
| Halse et al. [47] | Usual physical activity Home cycle ergometer supervised three times a week and unsupervised for two sessions a week | Control n = 9 GDM diagnosis at 28 weeks Intervention n = 10 GDM diagnosis at 28 weeks | Glycaemic control | No difference in fasting glucose, HbA1C, insulin use, dose, or latency to starting insulin Improved post prandial glucose and average glucose |
| Jovanovic-Peterson et al. [42] | Usual physical activity Aerobic exercise: 20 min for three times a week, supervised, using ergometer | Control n = 5 GDM “newly diagnosed” Intervention n = 5 GDM “newly diagnosed” | Additional medications Adherence to intervention Hypertensive disorders Glycaemic control | Improved fasting glucose with intervention No difference in obstetric or maternal outcomes |
| Qadir et al. [44] | Usual physical activity measured by pedometer Patient education and structured exercise class once a week Usual physical activity measured by pedometer | Control n = 4 Intervention n = 2 | Average daily steps Glycaemic control | No difference in glycaemic control |
| Ramos et al. [43] | 50 min stretching and relaxation once a week 50 min aerobic session three times a week | Control n = 20 GDM diagnosis: 20.8 ± 6 weeks Intervention n = 18 GDM diagnosis 22.2 ± 6 weeks | Improved HbA1C in intervention | |
| Sklempe Kokic [45] | Usual physical activity Combined aerobic and resistance exercise (two supervised sessions) plus seven sessions of unsupervised walking | Control n = 85 GDM diagnosis: 24–30 weeks Intervention n = 85 GDM diagnosis: 24–30 weeks | Additional medications Caesarean Birth Glycaemic control Weight gain | Improved postprandial glucose with intervention, no difference in maternal obstetric outcomes |
| Youngwanichsetha et al. [46] | Not applicable Fifteen to twenty minutes of supervised yoga five times a week | Glycaemic control | Improved fasting glucose, post prandial glucose, HbA1C with intervention |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keating, N.; Coveney, C.; McAuliffe, F.M.; Higgins, M.F. Aerobic or Resistance Exercise for Improved Glycaemic Control and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10791. https://doi.org/10.3390/ijerph191710791
Keating N, Coveney C, McAuliffe FM, Higgins MF. Aerobic or Resistance Exercise for Improved Glycaemic Control and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(17):10791. https://doi.org/10.3390/ijerph191710791
Chicago/Turabian StyleKeating, Niamh, Ciara Coveney, Fionnuala M. McAuliffe, and Mary F. Higgins. 2022. "Aerobic or Resistance Exercise for Improved Glycaemic Control and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 17: 10791. https://doi.org/10.3390/ijerph191710791
APA StyleKeating, N., Coveney, C., McAuliffe, F. M., & Higgins, M. F. (2022). Aerobic or Resistance Exercise for Improved Glycaemic Control and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus: A Systematic Review. International Journal of Environmental Research and Public Health, 19(17), 10791. https://doi.org/10.3390/ijerph191710791






