Description of ROM-SPORT I Battery: Keys to Assess Lower Limb Flexibility
Abstract
1. Introduction
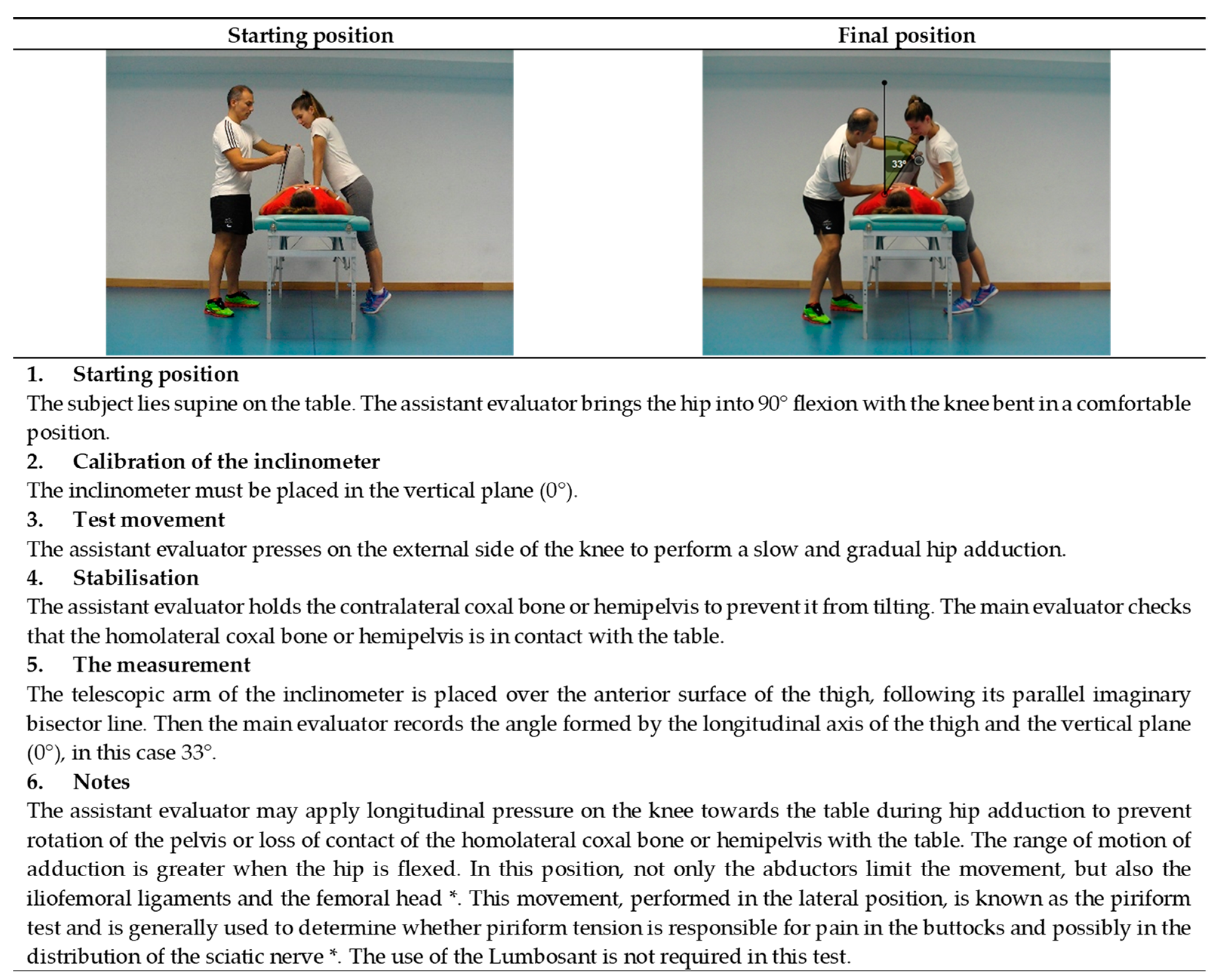
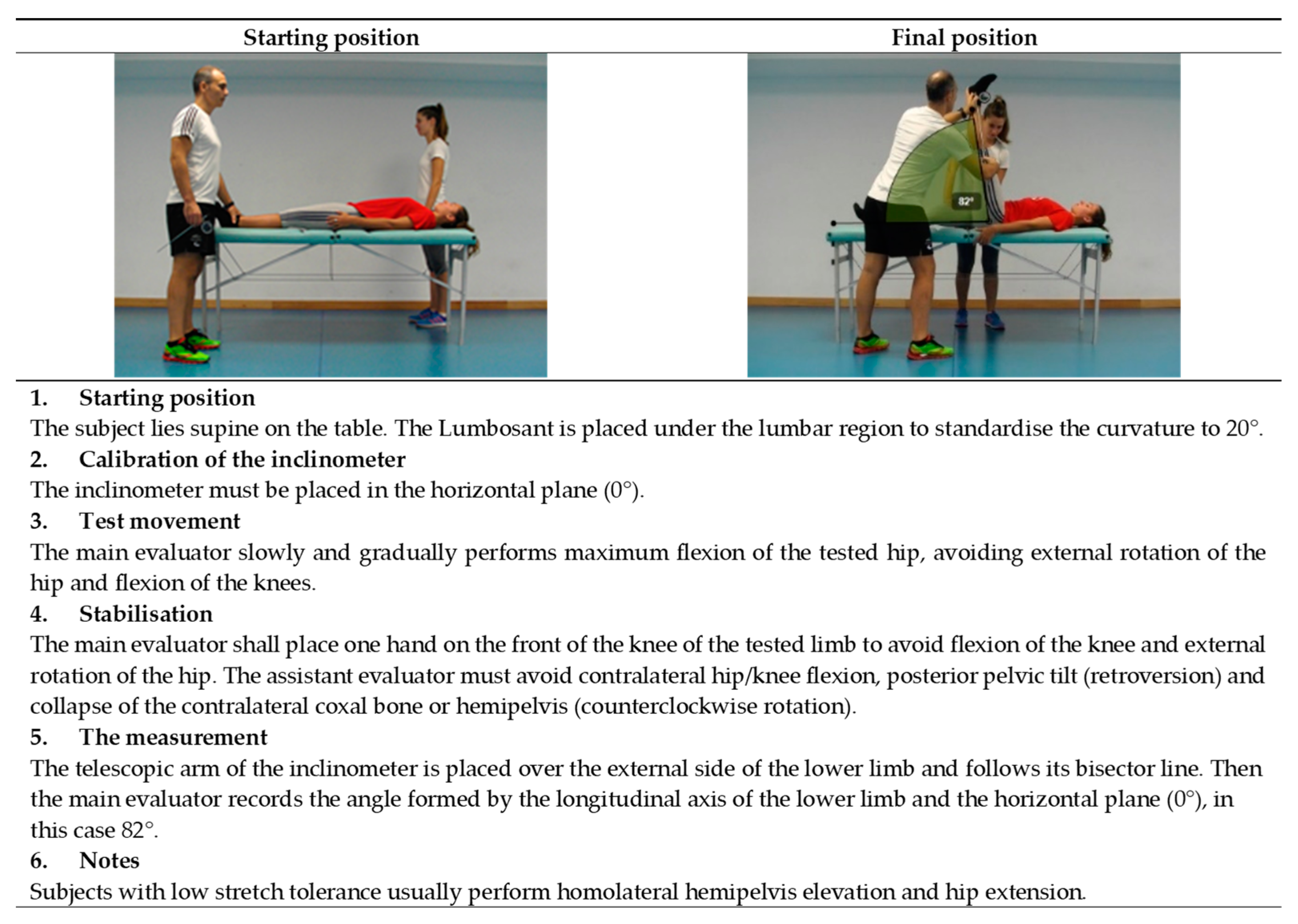
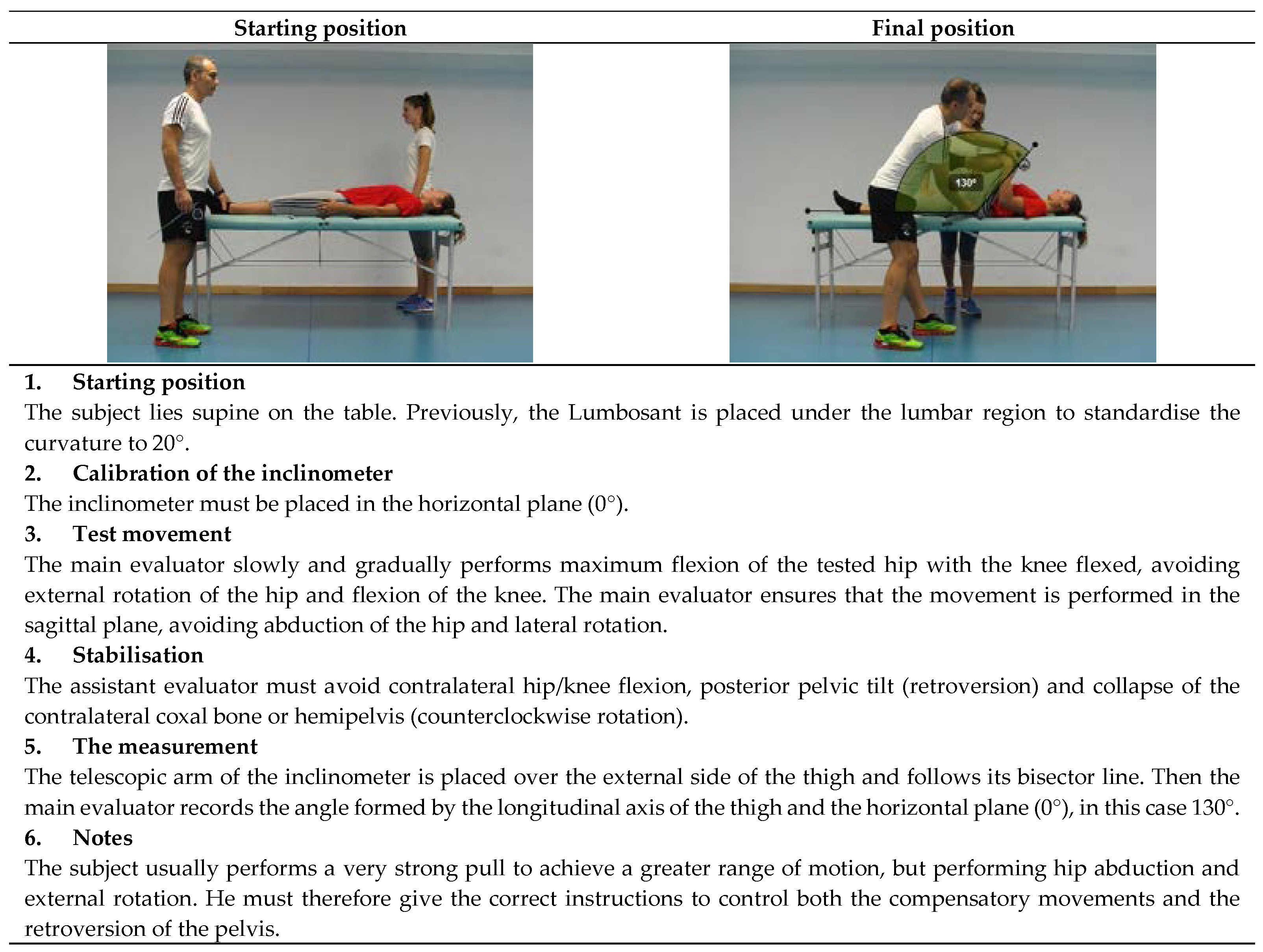
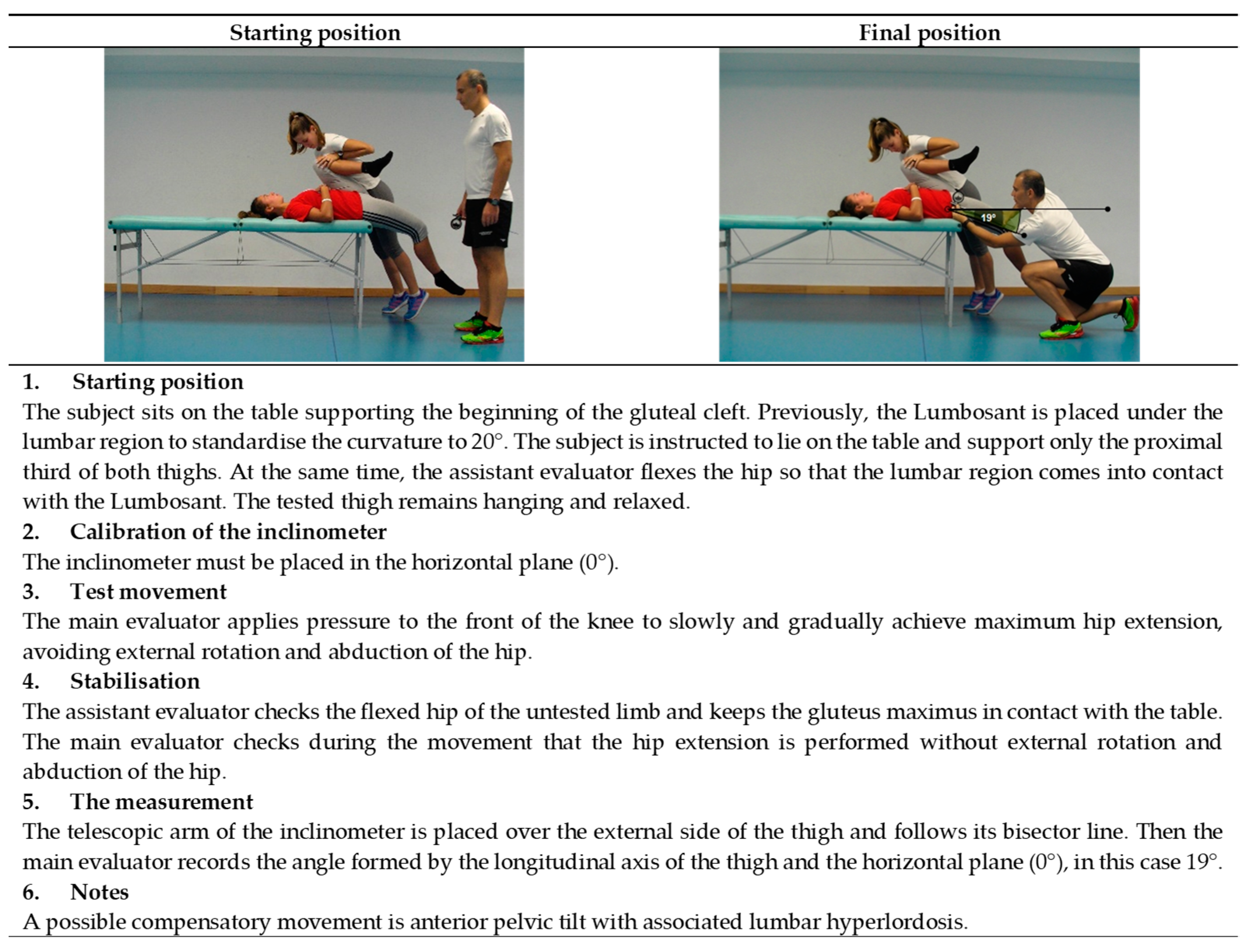
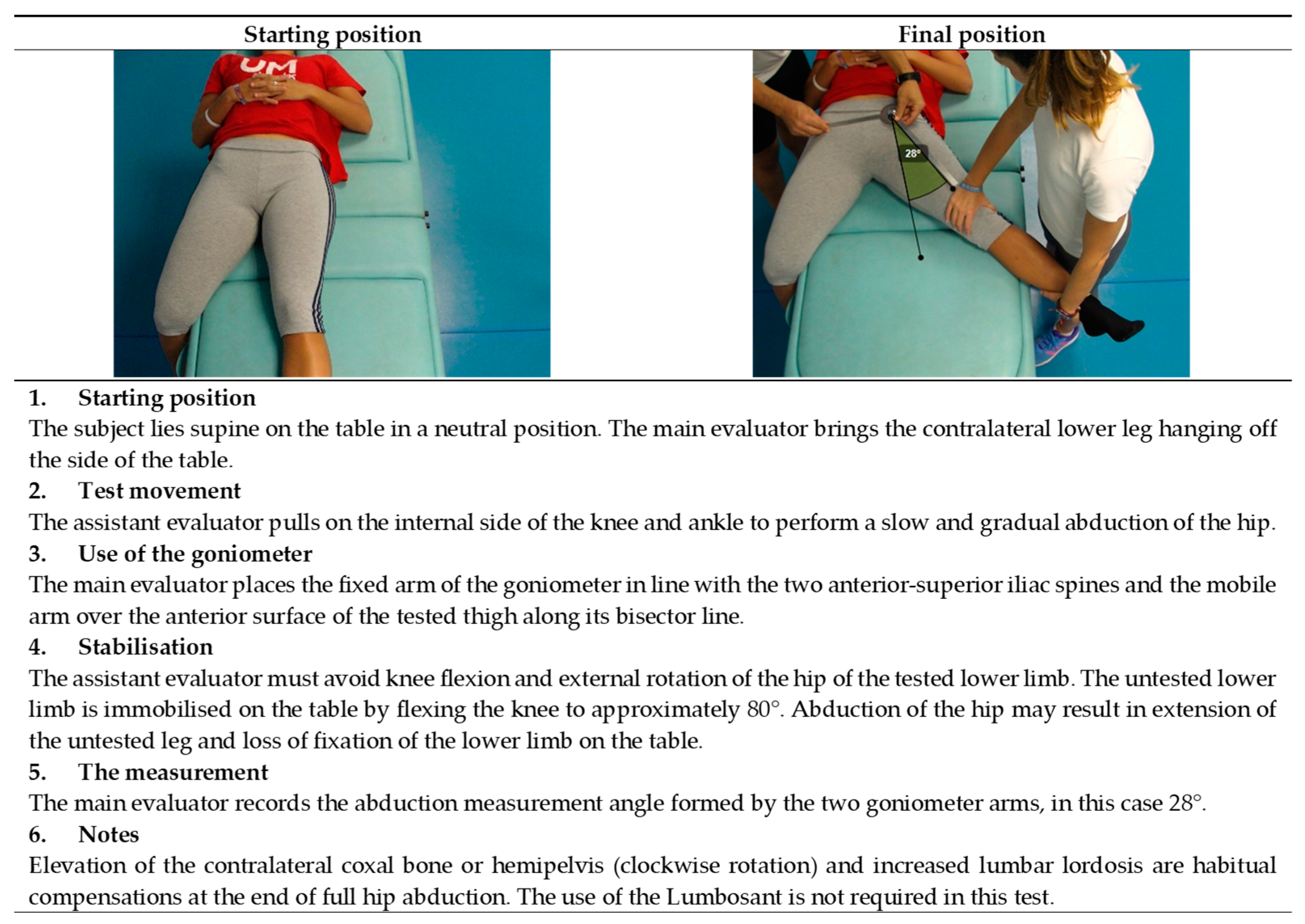
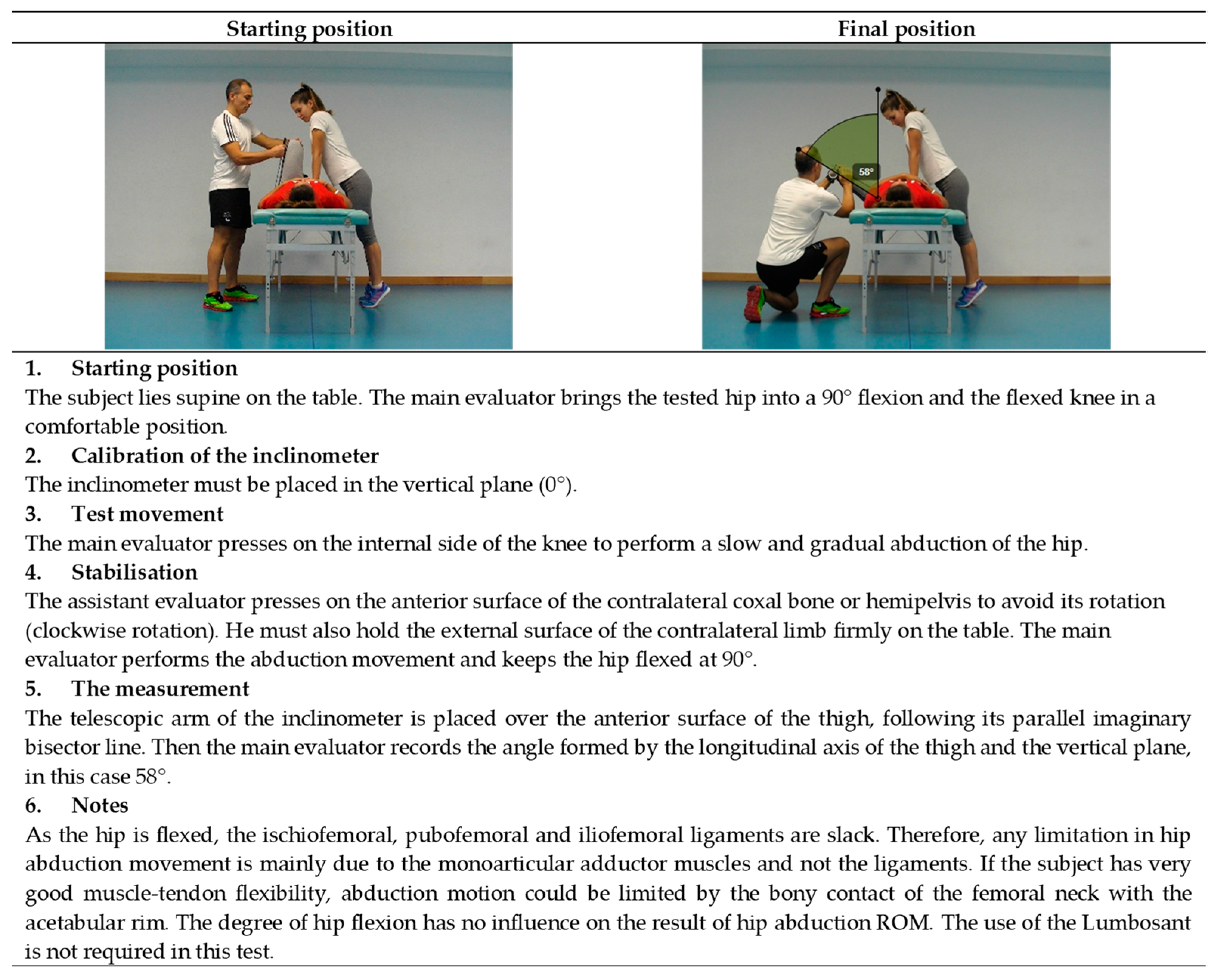
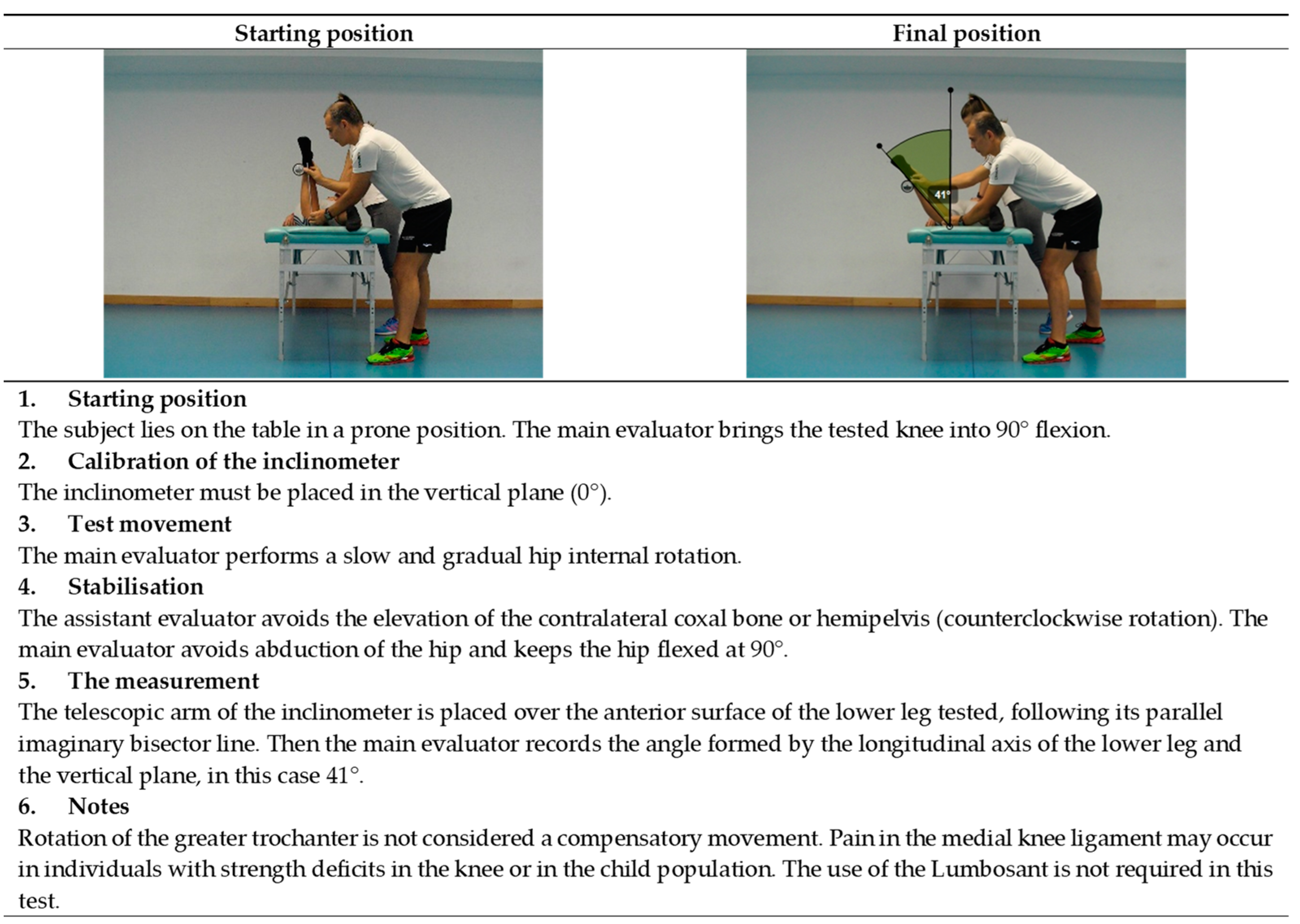
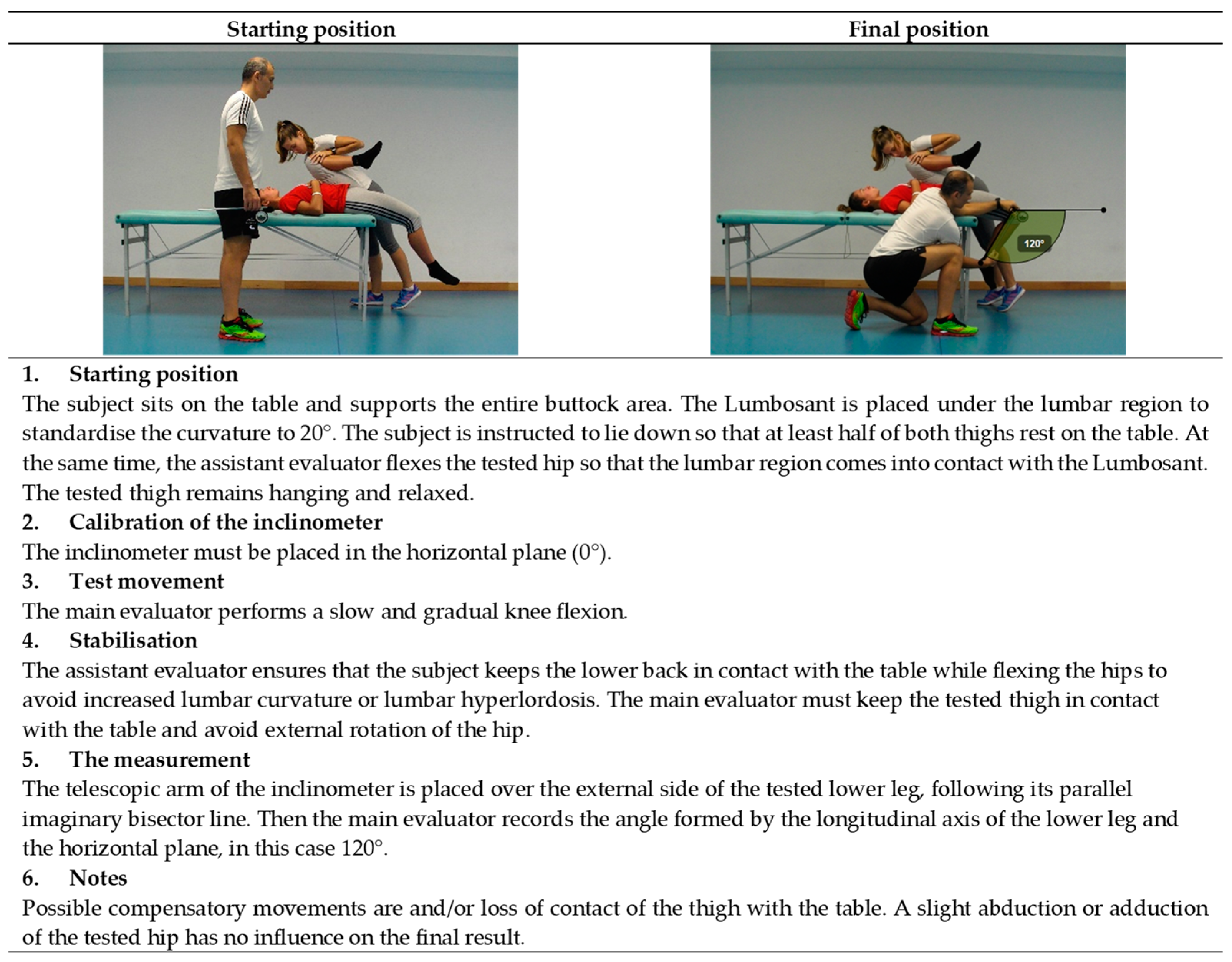
2. Description of the Tests of ROM-SPORT Battery I
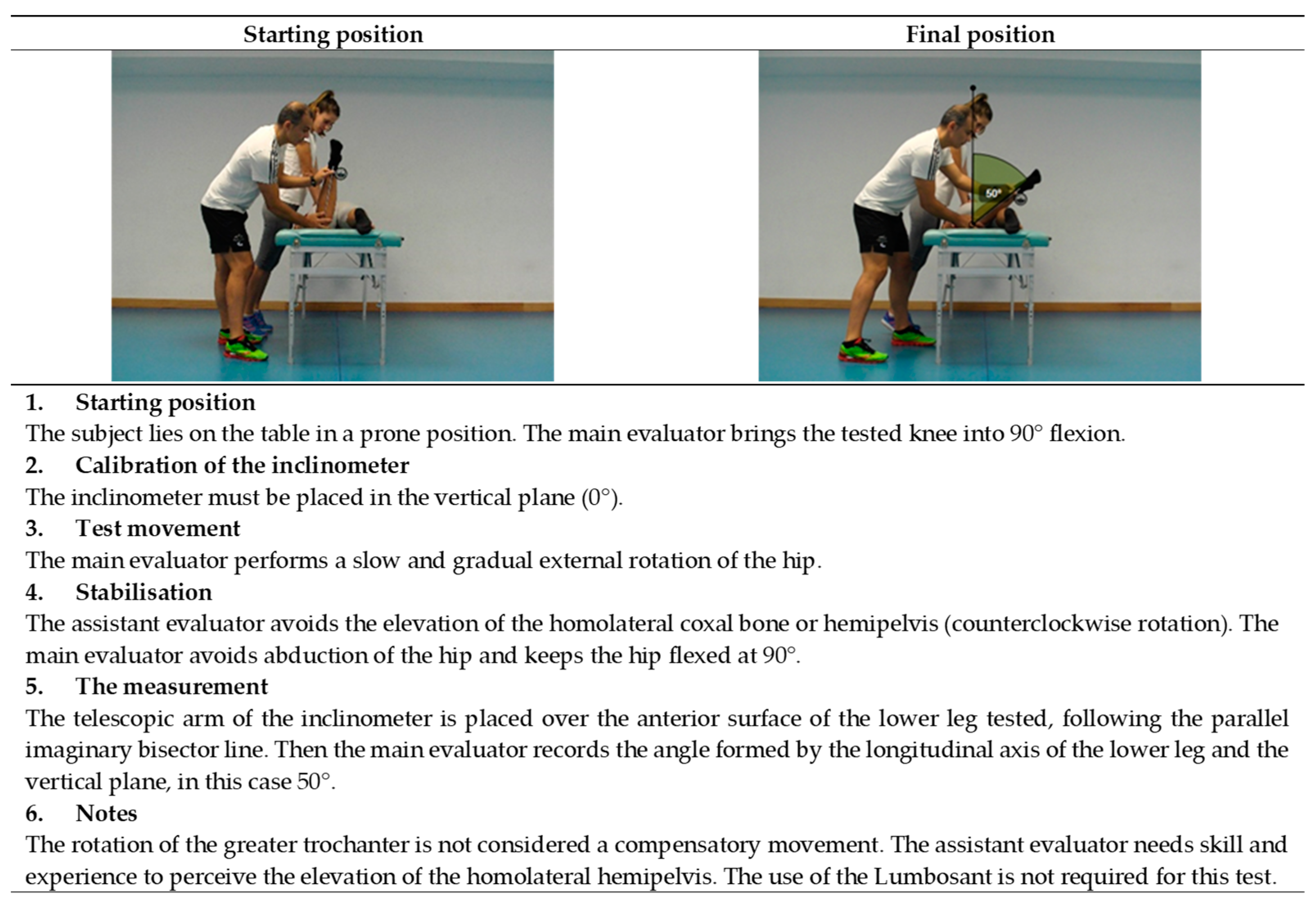
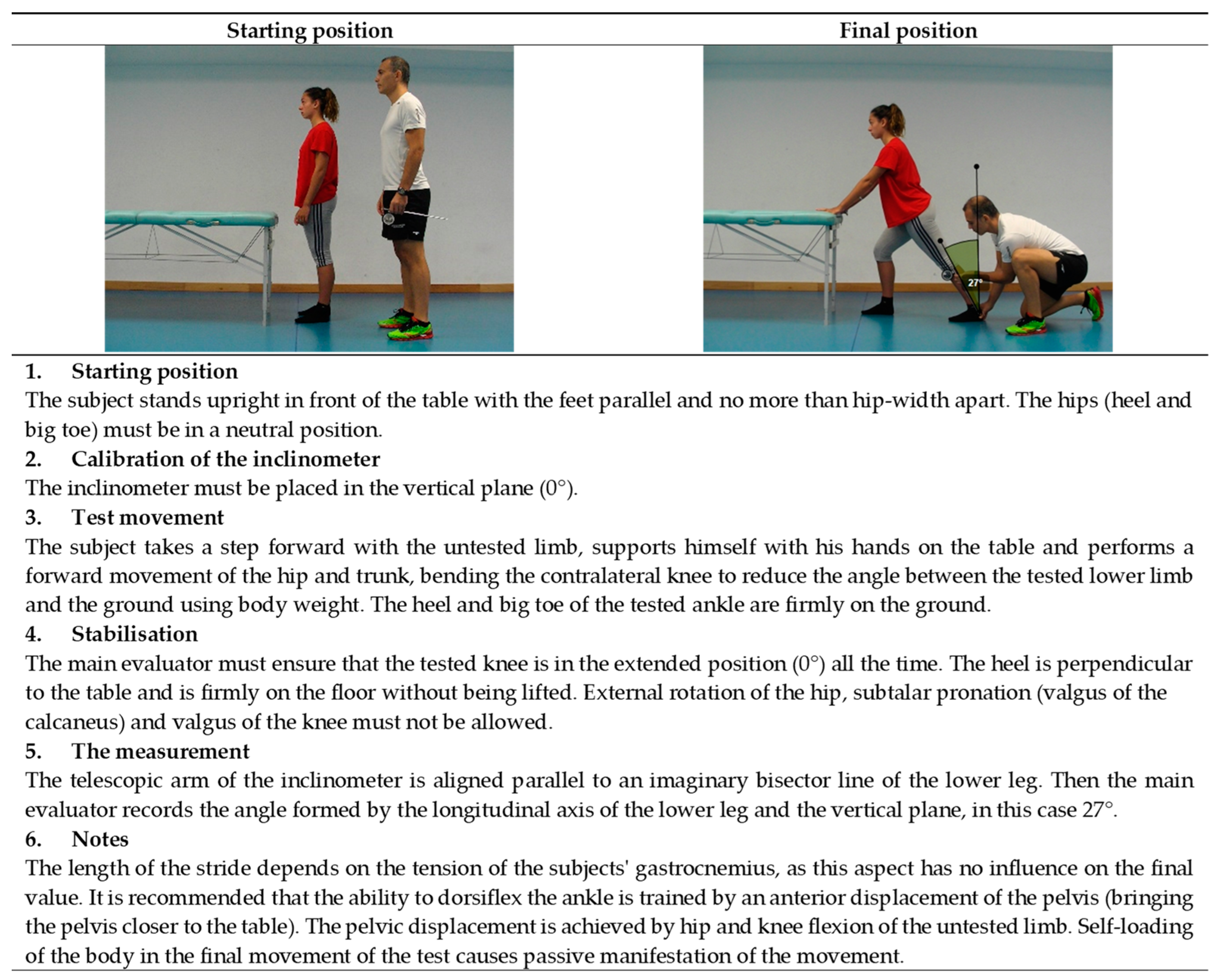
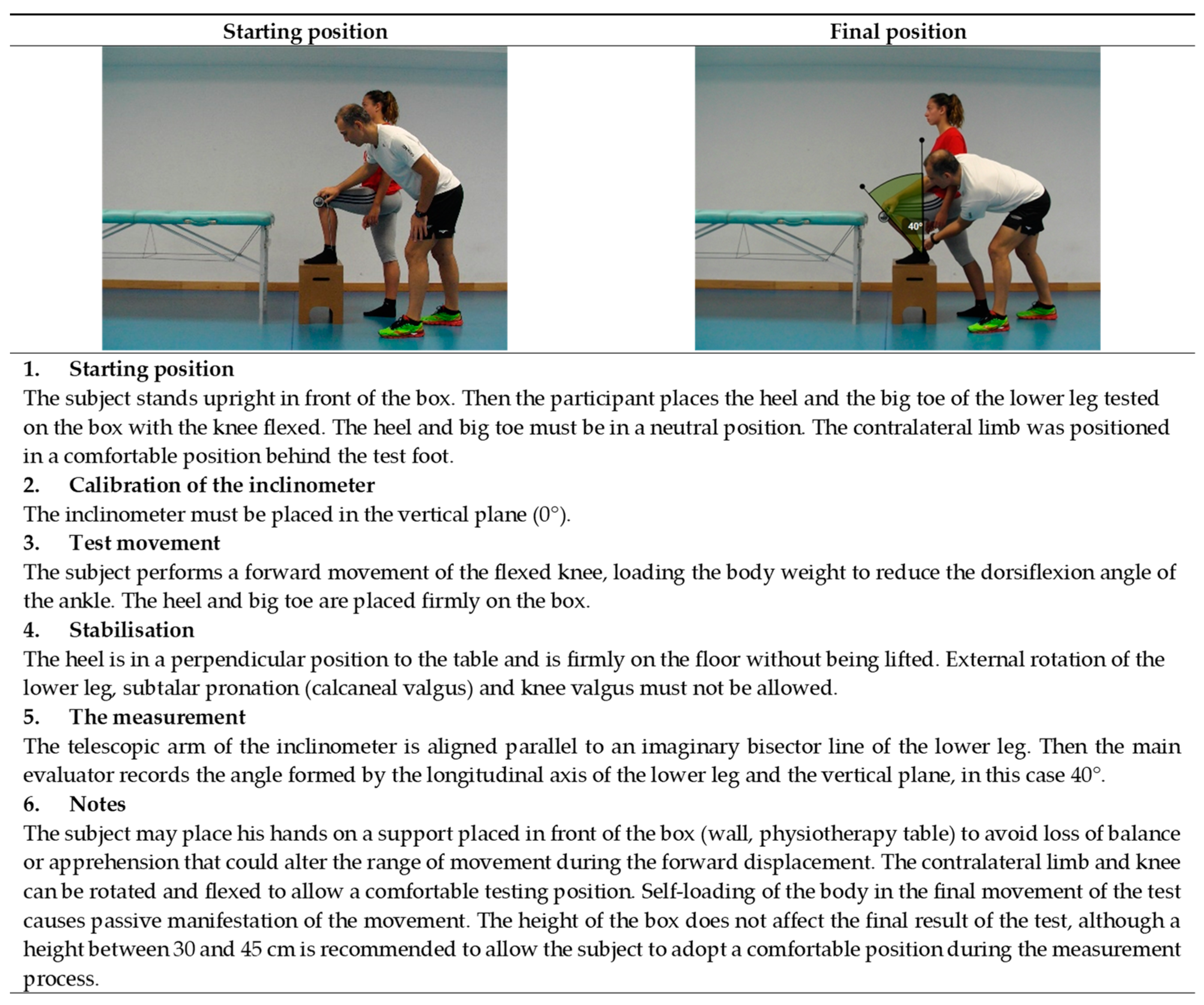
3. Highlights of the ROM-SPORT I Procedure
3.1. Familiarisation and Warm-Up Phase
3.2. Human Resources
3.3. Athlete’s Starting Position
3.4. Measuring Instrument and Its Calibration
3.5. Movement of the Assessment
3.6. Stabilisation
3.7. Criteria for the End of the Range of Motion
3.8. Measurement
3.9. Notes
4. The Validity of the ROM-SPORT I Battery
5. Reliability of the ROM-SPORT I Battery
6. Practical Applications of the ROM-SPORT I Battery
- −
- −
- −
- −
- To quantify the effectiveness of intervention programs or significant chronic ROM changes (e.g., stretching and foam rolling intervention) aimed at maintaining or improving muscle flexibility in both healthy and injured individuals [110].
- −
- In physical therapy processes, to determine whether the ROM of the injured joint has been fully restored, which may contribute to a safe return to play (athletes) or activities of daily living (general population) [111].
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Baarveld, F.; Visser, C.; Kollen, B.; Backx, F. Sports-related injuries in primary health care. Fam. Pract. 2011, 28, 29–33. [Google Scholar] [CrossRef]
- Bahr, R.; Holme, I. Risk Factors for Sports Injuries—A Methodological Approach; British Association of Sport and Excercise Medicine: Auckley, UK, 2003; Volume 37. [Google Scholar]
- Lindqvist, K.; Timpka, T.; Bjurulf, P. Injuries during leisure physical activity in a Swedish municipality. Scand. J. Soc. Med. 1996, 24, 282–292. [Google Scholar] [CrossRef]
- Baechle, T.R.; Earle, R.W. Essentials of Strength Training and Conditioning; Human kine.: Champaign, IL, USA, 2008. [Google Scholar]
- American College of Sports Medicine. ACSM’s Health-Related Physical Fitness Assessment Manual; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2013. [Google Scholar]
- Thacker, S.; Gilchrist, J.; Stroup, D.; Kimsey, C.; Thacker, S.; Gilchrist, J.; Stroup, D.; Kimsey, C. The Impact of Stretching on Sports Injury Risk: A Systematic Review of the Literature. Med. Sci. Sports Exerc. 2004, 36, 371–378. [Google Scholar] [CrossRef]
- Ekstrand, J.; Spreco, A.; Bengtsson, H.; Bahr, R. Injury rates decreased in men’s professional football: An 18-year prospective cohort study of almost 12 000 injuries sustained during 1.8 million hours of play. Br. J. Sports Med. 2021, 55, 1084–1092. [Google Scholar] [CrossRef]
- Hägglund, M.; Waldén, M.; Ekstrand, J. Risk factors for lower extremity muscle injury in professional soccer: The UEFA injury study. Am. J. Sports Med. 2013, 41, 327–335. [Google Scholar] [CrossRef]
- Verrall, G.; Slavotinek, J.; Barnes, P.; Esterman, A.; Oakeshott, R.; Spriggins, A. Hip joint range of motion restriction precedes athletic chronic groin injury. J. Sci. Med. Sport 2007, 10, 463–466. [Google Scholar] [CrossRef]
- Arnason, A.; Sigurdsson, S.; Gudmundsson, A.; Holme, I.; Engebretsen, L.; Bahr, R. Risk Factors for Injuries in Football. Am. J. Sports Med. 2004, 32, 5S–16S. [Google Scholar] [CrossRef]
- Emery, C.; Meeuwisse, W. Risk factors for groin injuries in hockey. Med. Sci. Sports Exerc. 2001, 33, 1423–1433. [Google Scholar] [CrossRef]
- Ibrahim, A.; Murrell, G.; Knapman, P. Adductor Strain and Hip Range of Movement in Male Professional Soccer Players. J. Orthop. Surg. 2007, 15, 46–49. [Google Scholar] [CrossRef]
- Nevin, F.; Delahunt, E. Adductor squeeze test values and hip joint range of motion in Gaelic football athletes with longstanding groin pain. J. Sci. Med. Sport 2014, 17, 155–159. [Google Scholar] [CrossRef]
- Okamura, S.; Wada, N.; Tazawa, M.; Sohmiya, M.; Ibe, Y.; Shimizu, T.; Usuda, S.; Shirakura, K. Injuries and disorders among young ice skaters: Relationship with generalized joint laxity and tightness. Open Access J. Sports Med. 2014, 5, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Backman, L.; Danielson, P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: A 1-year prospective study. Am. J. Sports Med. 2011, 39, 2626–2633. [Google Scholar] [CrossRef]
- Scattone Silva, R.; Nakagawa, T.H.; Ferreira, A.L.G.; Garcia, L.C.; Santos, J.E.M.; Serrão, F.V. Lower limb strength and flexibility in athletes with and without patellar tendinopathy. Phys. Ther. Sport 2016, 20, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Wilder, R.; Sethi, S. Overuse injuries: Tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin. Sports Med. 2004, 23, 55–81. [Google Scholar] [CrossRef]
- Witvrouw, E.; Danneels, L.; Asselman, P.; D’Have, T.; Cambier, D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players: A prospective study. Am. J. Sports Med. 2003, 31, 41–46. [Google Scholar] [CrossRef]
- Ekstrand, J.; Gillquist, J. The frequency of muscle tightness and injuries in soccer players. Am. J. Sports Med. 1982, 10, 75–78. [Google Scholar] [CrossRef]
- Gabbe, B.; Finch, C.; Wajswelner, H.; Bennell, K. Predictors of lower extremity injuries at the community level of Australian football. Clin. J. Sport Med. 2004, 14, 56–63. [Google Scholar] [CrossRef]
- Tainaka, K.; Takizawa, T.; Kobayashi, H.; Umimura, M. Limited hip rotation and non-contact anterior cruciate ligament injury: A case–control study. Knee 2014, 21, 86–90. [Google Scholar] [CrossRef]
- Lopes, O.; Gomes, J.; Freitas Spinelli, L. Range of motion and radiographic analysis of the hip in patients with contact and non-contact anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2868–2873. [Google Scholar] [CrossRef]
- VandenBerg, C.; Crawford, E.; Enselman, E.; Robbins, B.; Wojtys, E.; Bedi, A. Restricted Hip Rotation Is Correlated With an Increased Risk for Anterior Cruciate Ligament Injury. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 317–325. [Google Scholar] [CrossRef]
- Bedi, A.; Warren, R.; Wojtys, E.; Oh, Y.; Ashton-Miller, J.; Oltean, H.; Kelly, B. Restriction in hip internal rotation is associated with an increased risk of ACL injury. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2024–2031. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, A.; Centenera-Centenera, J.; Santonja-Medina, F. The Potential Role of Hamstring Extensibility on Sagittal Pelvic Tilt, Sagittal Spinal Curves and Recurrent Low Back Pain in Team Sports Players: A Gender Perspective Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8654. [Google Scholar] [CrossRef] [PubMed]
- Vad, V.; Bhat, A.; Basrai, D.; Gebeh, A.; Aspergren, D.; Andrews, J. Low Back Pain in Professional Golfers: The Role of Associated Hip and Low Back Range-of-Motion Deficits. Am. J. Sports Med. 2004, 32, 494–497. [Google Scholar] [CrossRef]
- Moreno-Pérez, V.; López-Valenciano, A.; Ayala, F.; Fernandez-Fernandez, J.; Vera-Garcia, F. Comparison of hip extension and rotation ranges of motion in young elite tennis players with and without history of low back pain. J. Back Musculoskelet. Rehabil. 2019, 32, 629–638. [Google Scholar] [CrossRef]
- Cejudo, A.; Moreno-Alcaraz, V.J.; Izzo, R.; Santonja-Medina, F.; Sainz de Baranda, P. External and Total Hip Rotation Ranges of Motion Predispose to Low Back Pain in Elite Spanish Inline Hockey Players. Int. J. Environ. Res. Public Health 2020, 17, 4858. [Google Scholar] [CrossRef]
- Van Dillen, L.; Bloom, N.; Gombatto, S.; Susco, T. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys. Ther. Sport 2008, 9, 72–81. [Google Scholar] [CrossRef]
- Kanchanomai, S.; Janwantanakul, P.; Pensri, P.; Jiamjarasrangsi, W. A prospective study of incidence and risk factors for the onset and persistence of low back pain in Thai university students. Asia-Pac. J. Public Health 2015, 27, NP106–NP115. [Google Scholar] [CrossRef]
- Roach, S.; San Juan, J.; Suprak, D.; Lyda, M.; Boydston, C. Patellofemoral pain subjects exhibit decreased passive hip range of motion compared to controls. Int. J. Sports Phys. Ther. 2014, 9, 468–475. [Google Scholar]
- Witvrouw, E.; Van Tiggelen, D.; Willems, T. Risk factors and prevention of anterior knee pain. In Anterior knee pain and patellar instability. Anterior Knee Pain and Patellar Instability; Springer: London, UK, 2006; pp. 135–145. [Google Scholar]
- Sainz de Baranda, P.; Cejudo, A.; Ayala, F.; Santonja, F. Perfil óptimo de flexibilidad del miembro inferior en jugadoras de fútbol sala. Rev. Int. Med. Cienc. Act. Fis. Deporte 2015, 15, 647–662. [Google Scholar] [CrossRef][Green Version]
- Gonzalo-Skok, O.; Serna, J.; Rhea, M.; Marín, P. Relationships between functional movement tests and performance tests in young elite male basketball players. Int. J. Sports Phys. Ther. 2015, 10, 628–638. [Google Scholar]
- Panoutsakopoulos, V.; Kotzamanidou, M.C.; Papaiakovou, G.; Kollias, I.A. The Ankle Joint Range of Motion and Its Effect on Squat Jump Performance with and without Arm Swing in Adolescent Female Volleyball Players. J. Funct. Morphol. Kinesiol. 2021, 6, 14. [Google Scholar] [CrossRef]
- Hogg, J.; Schmitz, R.; Nguyen, A.-D.; Shultz, S.J. Lumbo-Pelvic-Hip Complex Passive Hip Range-of-Motion Values Across Sex and Sport. J. Athl. Train. 2018, 53, 560–567. [Google Scholar] [CrossRef]
- Cejudo, A.; Robles-Palazón, F.; Sainz De Baranda, P. Fútbol sala de élite: Diferencias de flexibilidad según sexo. E-Balonmano.Com. Rev. De Cienc. Del Deporte 2019, 15, 37–48. [Google Scholar]
- Canda Moreno, A.; Gómez Martín, A.; Heras Gómez, E. Valoración de la flexibilidad de tronco mediante el test del cajón en diferentes modalidades deportivas. Selección 2004, 13, 148–154. [Google Scholar]
- Sprague, H. Relationship of certain physical measurements to swimming speed. Am. Alliance Health Phys. Educ. Recreat. 1976, 47, 810–814. [Google Scholar] [CrossRef]
- Pilianidis, T.; Douda, H.; Smilios, I.; Nikolaidis, K.; Tsarouchas, E.; Tokmakidis, S. Changes in muscular flexibility and performance during an ultra-marathon. J. Hum. Mov. Stud. 2002, 43, 417–427. [Google Scholar]
- Oberg, B.; Ekstrand, J.; Moller, M.; Gillquist, J. Muscle strength and flexibility in different positions of soccer players. Int. J. Sports Med. 1984, 5, 213–216. [Google Scholar] [CrossRef]
- López-Valenciano, A.; Ayala, F.; Vera-García, F.; De Ste Croix, M.; Hernández-Sánchez, S.; Ruiz-Pérez, I.; Cejudo, A.; Santonja, F. Comprehensive profile of hip, knee and ankle ranges of motion in professional football players. J. Sports Med. Phys. Fit. 2019, 59, 102–109. [Google Scholar] [CrossRef]
- Fousekis, K.; Tsepis, E.; Poulmedis, P.; Athanasopoulos, S.; Vagenas, G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: A prospective study of 100 professional players. Br. J. Sports Med. 2011, 45, 709–714. [Google Scholar] [CrossRef]
- Cejudo, A.; Ruiz-Pérez, I.; Hernández-Sánchez, S.; De Ste Croix, M.; Sainz de Baranda, P.; Ayala, F. Comprehensive Lower Extremities Joints Range of Motion Profile in Futsal Players. Front. Psychol. 2021, 12, 658996. [Google Scholar] [CrossRef]
- Battista, R.; Pivarnik, J.; Dummer, G.; Sauer, N.; Malina, R. Comparisons of physical characteristics and performances among female collegiate rowers. J. Sports Sci. 2007, 25, 651–657. [Google Scholar] [CrossRef]
- Gannon, L.; Bird, H.; Gan Non, L. The quantification of joint laxity in dancers and gymnasts The quantification of joint laxity in dancers and gymnasts. J. Sports Sci. 1999, 17, 743–750. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, J.; Pérez, A.; Boada, P.; García, M.; Moreno, C.; Carretero, M. Estudio de la flexibilidad de luchadores de kickboxing de nivel internacional. Arch. Med. Deporte 2014, 31, 85–91. [Google Scholar]
- De la Fuente, A.; Gómez-Landero, L. Motor differences in cadet taekwondo athletes according to competition level. Rev. Int. Med. Cienc. Act. Fis. Deporte 2019, 19, 63–75. [Google Scholar] [CrossRef]
- Robles-Palazón, F.; Ayala, F.; Cejudo, A.; De Ste Croix, M.; Sainz de Baranda, P.; Santonja, F. Effects of age and maturation on lower extremity range of motion in male youth soccer players. J. Strength Cond. Res. 2020, 36, 1417–1425. [Google Scholar] [CrossRef]
- Lloyd, R.; Oliver, J.; Faigenbaum, A.; Myer, G.; Croix, M. Chronological age vs. biological maturation: Implications for exercise programming in youth. J. Strength Cond. Res. 2014, 28, 1454–1464. [Google Scholar] [CrossRef]
- Gómez-Jiménez, F.; Ayala, F.; Cejudo, A.; Sainz de Baranda, P.; Santonja, F. Efecto del nivel de experiencia clínica del examinador sobre la validez de criterio y fiabilidad inter-sesión de cinco medidas del rango de movimiento de la flexión. Cuad. De Psicol. Del Deporte 2015, 15, 123–134. [Google Scholar] [CrossRef]
- Iwata, M.; Yamamoto, A.; Matsuo, S.; Hatano, G.; Miyazaki, M.; Fukaya, T.; Fujiwara, M.; Asai, Y.; Suzuki, S. Dynamic Stretching Has Sustained Effects on Range of Motion and Passive Stiffness of the Hamstring Muscles. J. Sci. Med. Sport 2019, 18, 13–20. [Google Scholar]
- De Souza, A.; Sanchotene, C.; da Silva Lopes, C.; Beck, J.; da Silva, A.; Pereira, S.; Ruschel, C. Acute effect of 2 self-myofascial release protocols on hip and ankle range of motion. J. Sport Rehabil. 2019, 28, 159–164. [Google Scholar] [CrossRef]
- Hopkins, W. How to interpret changes in an athletic performance test. Sport Sci. 2004, 8, 1–7. [Google Scholar]
- Hopkins, W. Measures of Reliability in Sports Medicine and Science. Sports Med. 2000, 30, 1–15. [Google Scholar] [CrossRef]
- Hopkins, W.; Marshall, S.; Batterham, A.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef]
- Cejudo, A.; Sainz de Baranda, P.; Ayala, F.; De Ste Croix, M.; Santonja-Medina, F. Assessment of the Range of Movement of the Lower Limb in Sport: Advantages of the ROM-SPORT I Battery. Int. J. Environ. Res. Public Health 2020, 17, 7606. [Google Scholar] [CrossRef]
- Gerhardt, J.; Cocchiarella, L.; Lea, R. The Practical Guide to Range of Motion Assessment; American Medical Association: Chicago, IL, USA, 2002. [Google Scholar]
- Palmer, M.; Epler, M. Fundamentos de Las Técnicas de Evaluación Musculoesquelética; Paidotribo: Barcelona, Spain, 2002. [Google Scholar]
- Alter, M. Los Estiramientos; Paidotribo: Barcelona, Spain, 2004. [Google Scholar]
- Bishop, D. Warm Up I Potential Mechanisms and the Effects of Passive Warm Up on Exercise Performance. Sports Med. 2003, 33, 439–454. [Google Scholar] [CrossRef]
- Bishop, D. Warm-up II: Performance changes following active warm up and how to structure the warm-up. Sport Med. 2003, 33, 483–498. [Google Scholar] [CrossRef]
- Murphy, J.; Di Santo, M.; Alkanani, T.; Behm, D. Aerobic activity before and following short-duration static stretching improves range of motion and performance vs. a traditional warm-up Impact of 10-Minute Interval Roller Massage on Performance and Active Range of Motion View project Metastability Stre. Appl. Physiol. Nutr. Metab. 2010, 35, 679–690. [Google Scholar] [CrossRef]
- Castro-Pinero, J.; Chillon, P.; Ortega, F.; Montesinos, J.; Sjostrom, M.; Ruiz, J. Criterion-related validity of sit-and-reach and modified sit-and-reach test for estimating hamstring flexibility in children and adolescents aged 6–17 years. Int. J. Sports Med. 2009, 30, 658–662. [Google Scholar] [CrossRef]
- Dixon, J.; Keating, J. Variability in straight leg raise measurements. Physiotherapy 2000, 86, 361–370. [Google Scholar] [CrossRef]
- Cejudo, A.; Sainz De Baranda, P.; Ayala, F.; Santonja, F. A simplified version of the weight-bearing ankle lunge test: Description and test-retest reliability. Man. Ther. 2014, 19, 355–359. [Google Scholar] [CrossRef]
- Santonja-Medina, F.; Santonja-Renedo, S.; Cejudo, A.; Ayala, F.; Ferrer, V.; Pastor, A.; Collazo-Diéguez, M.; Rodríguez-Ferrán, O.; Andújar, P.; Sainz de Baranda, P. Straight Leg Raise Test: Influence of Lumbosant© and Assistant Examiner in Hip, Pelvis Tilt and Lumbar Lordosis. Symmetry 2020, 12, 927. [Google Scholar] [CrossRef]
- Cejudo, A.; Sainz de Baranda, P.; Ayala, F.; Santonja, F. Test-retest reliability of seven common clinical tests for assessing lower extremity muscle flexibility in futsal and handball players. Phys. Ther. Sport 2015, 16, 107–113. [Google Scholar] [CrossRef]
- Clapis, P.; Davis, S.; Davis, R. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiother. Theory Pract. 2008, 24, 135–141. [Google Scholar] [CrossRef]
- Fredriksen, H.; Dagfinrud, H.; Jacobsen, V.; Maehlum, S. Passive knee extension test to measure hamstring muscle tightness. Scand. J. Med. Sci. Sports 1997, 7, 279–282. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz de Baranda, P.; De Ste Croix, M.; Santonja, F. Reproducibility and criterion-related validity of the sit and reach test and toe touch test for estimating hamstring flexibility in recreationally active young adults. Phys. Ther. Sport 2012, 13, 219–226. [Google Scholar] [CrossRef]
- Hahn, T.; Foldspang, A.; Vestergaard, E.; Ingemann-Hansen, T. Active knee joint flexibility and sports activity. Scand. J. Med. Sci. Sports 1999, 9, 74–80. [Google Scholar] [CrossRef]
- Bogduk, N.; Pearcy, M.; Hadfield, G. Anatomy and biomechanics of psoas major. Clin. Biomech. 1992, 7, 109–119. [Google Scholar] [CrossRef]
- Kendall, F.; McCreary, E.; Provance, P.; Rodgers, M.; Romani, W. Muscles: Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005; ISBN 0781747805. [Google Scholar]
- Norris, C.; Matthews, M. Correlation between hamstring muscle length and pelvic tilt range during forward bending in healthy individuals: An initial evaluation. J. Bodyw. Mov. Ther. 2006, 10, 122–126. [Google Scholar] [CrossRef]
- Hayen, A.; Dennis, R.; Finch, C. Determining the intra-and inter-observer reliability of screening tools used in sports injury research. J. Sci. Med. Sport 2007, 10, 201–210. [Google Scholar] [CrossRef]
- Greene, W.; Heckman, J. Clinical Assessment of Joint Movement; Edika Med.: Barcelona, Spain, 1997. [Google Scholar]
- Magee, D. Orthopedic Physical Assessment; Elsevier Health Sciences: Philadelphia, PA, USA, 2013. [Google Scholar]
- Enwemeka, C. Radiographic verification of knee goniometry. Scand. J. Rehabil. Med. 1986, 18, 47–49. [Google Scholar]
- Gogia, P.; Braatz, J.; Rose, S.; Norton, B. Reliability and Validity of Goniometric Measurements at the Knee. Phys. Ther. 1987, 67, 192–195. [Google Scholar] [CrossRef]
- Vigotsky, A.; Lehman, G.; Beardsley, C.; Contreras, B.; Chung, B.; Feser, E. The modified Thomas test is not a valid measure of hip extension unless pelvic tilt is controlled. PeerJ 2016, 4, e2325. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, A. El perfil óptimo de flexibilidad en jóvenes jugadores de fútbol durante su periodo sensible del desarrollo físico. Batería ROM-SPORT. JUMP 2020, 2, 16–25. [Google Scholar] [CrossRef]
- Cejudo, A.; Robles-Palazón, F.; Ayala, F.; De Ste Croix, M.; Ortega-Toro, E.; Santonja, F.; Sainz de Baranda, P. Age-related differences in flexibility in soccer players 8-19 years old. PeerJ 2019, 7, e6236. [Google Scholar] [CrossRef]
- Sainz De Baranda, P.; Cejudo, A.; Ayala, F.; Santonja, F. Perfil de flexibilidad de la extremidad inferior en jugadoras senior de fútbol sala. Rev. Española De Educ. Física Y Deportes 2015, 409, 35–48. [Google Scholar]
- Cejudo, A.; Sainz De Baranda, P.; Ayala, F.; Santonja, F. Normative data of lower-limb muscle flexibility in futsal players. Rev. Int. Med. Cienc. Act. Fis. Deporte 2014, 14, 509–525. [Google Scholar]
- Cejudo, A. Lower Extremity Flexibility Profile in Basketball Players: Gender Differences and Injury Risk Identification. Int. J. Environ. Res. Public Health 2021, 18, 11956. [Google Scholar] [CrossRef]
- Cejudo, A.; Sainz De Baranda, P.; Ayala, F.; Santonja, F. Perfil de flexibilidad de la extremidad inferior en jugadores senior de balonmano. Cuad. De Psicol. Del Deporte 2014, 14, 111–120. [Google Scholar] [CrossRef]
- Cejudo, A.; Moreno-Alcaraz, V.; Izzo, R.; Robles-Palazón, F.J.; Sainz de Baranda, P.; Santonja-Medina, F. Flexibility in Spanish Elite Inline Hockey Players: Profile, Sex, Tightness and Asymmetry. Int. J. Environ. Res. Public Health 2020, 17, 3295. [Google Scholar] [CrossRef]
- Cejudo, A.; Moreno-Alcaraz, V.; De Ste Croix, M.; Santonja-Medina, F.; Sainz de Baranda, P. Lower-Limb Flexibility Profile Analysis in Youth Competitive Inline Hockey Players. Int. J. Environ. Res. Public Health 2020, 17, 4338. [Google Scholar] [CrossRef]
- Cejudo, A.; Ruiz, I.; Sainz de Baranda, P.; Ayala, F. Rango de movimiento de la extremidad inferior en atletas de duatlón. SPORT TK-Rev. EuroAmericana De Cienc. Del Deporte 2013, 2, 31–40. [Google Scholar] [CrossRef][Green Version]
- Cejudo, A.; San Cirilo-Soriano, B.; Robles Palazón, F.J.; Sainz de Baranda, P. Análisis del perfil de flexibilidad en jóvenes taekwondistas. Rev. De Artes Marciales Asiáticas 2018, 11, 30–33. [Google Scholar] [CrossRef]
- Lichota, M.; Plandowska, M.; Mil, P. The Shape of Anterior-Posterior Curvatures of the Spine in Athletes Practising Selected Sports. Pol. J. Sport Tour. 2011, 2, 112–121. [Google Scholar] [CrossRef]
- Cejudo, A.; Ginés-Díaz, A.; Sainz de Baranda, P. Asymmetry and Tightness of Lower Limb Muscles in Equestrian Athletes: Are They Predictors for Back Pain? Symmetry 2020, 12, 1679. [Google Scholar] [CrossRef]
- Kibler, W.; McQueen, C. Fitness evaluations and fitness findings in competitive junior tennis players. Clin. Sports Med. 1988, 7, 403–416. [Google Scholar] [CrossRef]
- L’hermette, M.; Polle, G.; Tourny-Chollet, C.; L’hermette, M. Hip passive range of motion and frequency of radiographic hip osteoarthritis in former elite handball players. Br. J. Sports Med. 2006, 40, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Holla, J.; Van Der Leeden, M.; Roorda, L.; Bierma-Zeinstra, S.; Damen, J.; Dekker, J.; Steultjens, M. Diagnostic accuracy of range of motion measurements in early symptomatic hip and/or knee osteoarthritis. Arthritis Care Res. 2012, 64, 59–65. [Google Scholar] [CrossRef]
- Young, S.; Harris, A.; Safran, M. Hip Range of Motion and Association With Injury in Female Professional Tennis Players Hip Systematic Review View project New Zealand Rotator Cuff Registry View project. Artic. Am. J. Sports Med. 2014, 42, 2654–2658. [Google Scholar] [CrossRef]
- Peterson, F.; Kendall, E.; Geise, P. Kendall’s Músculos. Pruebas, Funciones y Dolor Postural; Marbán, Ed.: Madrid, Spain, 2005. [Google Scholar]
- Shah, S.; Testa, E.; Gammal, I.; Sullivan, J.; Gerland, R.; Goldstein, J.; Cohn, R. Hip Range of Motion: Which Plane of Motion Is More Predictive of Lower Extremity Injury in Elite Soccer Players? A Prospective Study. J. Surg. Orthop. Adv. 2019, 28, 201–208. [Google Scholar] [PubMed]
- Peat, G.; Thomas, E.; Duncan, R.; Wood, L.; Wilkie, R.; Hill, J.; Hay, E.; Croft, P. Estimating the probability of radiographic osteoarthritis in the older patient with knee pain. Arthritis Rheum. 2007, 57, 794–802. [Google Scholar] [CrossRef]
- Malliaras, P.; Cook, J.; Kent, P. Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players. J. Sci. Med. Sport 2006, 9, 304–309. [Google Scholar] [CrossRef]
- Kottner, J.; Gajewski, B.; Streiner, D. Guidelines for Reporting Reliability and Agreement Studies (GRRAS). Int. J. Nurs. Stud. 2011, 48, 659–660. [Google Scholar] [CrossRef] [PubMed]
- Prather, H.; Harris-Hayes, M.; Hunt, H.; Steger-May, K.; Clohisy, J. Hip range of motion and provocative physical examination tests reliability and agreement in asymptomatic volunteers. PMR J. Inj. Funct. Rehabil. 2010, 2, 888–895. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz de Baranda, P.; De Ste Croix, M.; Santonja, F. Absolute reliability of five clinical tests for assessing hamstring flexibility in professional futsal players. J. Sci. Med. Sport 2012, 15, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, A.; Ayala, F.; Sainz de Baranda, P.; Santonja, F. Reliability of two methods of clinical examination of the flexibility of the hip adductor muscles. Int. J. Sports Phys. Ther. 2015, 10, 976–983. [Google Scholar] [PubMed]
- Reese, N.; Bandy, W. Use of an inclinometer to measure flexibility of the iliotibial band using the Ober test and the modified Ober test: Differences in magnitude and reliability of measurements. J. Orthop. Sports Phys. Ther. 2003, 33, 326–330. [Google Scholar] [CrossRef] [PubMed]
- LaRoche, D.; Connolly, D. Effects of stretching on passive muscle tension and response to eccentric exercise. Am. J. Sports Med. 2006, 34, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Law, R.; Harvey, L.; Nicholas, M.; Tonkin, L.; Se Sousa, M.; Finniss, D. Stretch exercises increase tolerance to stretch in patients with chronic musculoskeletal pain: A randomized controlled trial. Am. Phys. Ther. Assoc. 2009, 89, 1016–1026. [Google Scholar] [CrossRef]
- Rubini, E.; Costa, A.; Gomes, P. The Effects of Stretching on Strength Performance. Sports Med. 2007, 37, 213–224. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz De Baranda, P. Calidad metodológica de los programas de estiramiento: Revisión sistemática. Int. J. Med. Sci. Phys. Act. Sport 2013, 13, 163–181. [Google Scholar]
- Kim, G.; Kim, H.; Kim, W.; Kim, J. Effect of stretching-based rehabilitation on pain, flexibility and muscle strength in dancers with hamstring injury: A single-blind, prospective, randomized clinical trial. J. Sports Med. Phys. Fit. 2017, 59, 1287–1295. [Google Scholar] [CrossRef]
| ROM Test | Restricted ROM/High Risk of Injury (Predictive Validity) |
|---|---|
| Hip flexion with the knee extended | ≤68° [19] ≤70–71° [14,25,94] ≤88° [18] |
| Hip flexion with the knee flexed | ≤111° [95] ≤114° [96] ≤120° [59] |
| Hip extension with the knee relaxed | <0° [97,98] ≤13° [19] |
| Hip adduction with the 90° hip flexion | ≤19° [95] ≤20° [98] ≤26° [93] |
| Hip abduction with the knee extended | ≤28° [19] ≤45° [10,58,77] |
| Abduction with the 90° hip flexion | ≤50° [58] ≤80° [77] |
| Hip internal rotation | ≤23° [23] ≤28–30° [22,24,29,99] |
| Hip external rotation | ≤24–26° [9,13,95] |
| Knee flexion | ≤120–121° [18,100] ≤128° [93] ≤132° [19,96] |
| Ankle dorsi-flexion with the knee extended | ≤17° [19] |
| Ankle dorsi-flexion with the knee flexed | ≤28° [19] ≤35–37° [15,16] ≤45° [101] |
| Reference/Sample | Test | Human and Material Resources | Procedure | N° of Measurements and Time Interval | Results |
|---|---|---|---|---|---|
| Ayala et al. (2012) [104] M (n = 70) Recreational athletes | Hip flexion with the knee extended | 2 evaluators Inclinometer Lumbosant | 5 min cicloergometer and stretching 2 trials, mean | 3 sessions 4 weeks | SEM = 4.1° ICC = 0.88 |
| Cejudo et al. (2014) [66] M (n = 24) F (n = 26) Recreational athletes | Ankle dorsiflexion with the knee flexed | One evaluator Inclinometer | No warm-up 2 trials, mean | 3 sessions 2 weeks | SEM = 1.3° MDC95% = 3.8° ICC = 0.95 |
| Cejudo et al. (2015) [68] M (n = 60) F (n = 30) Futsal players Handball players | (a) Hip flexion with the knee flexed (b) Hip flexion with the knee extended (c) Hip extension with the knee relaxed (d) Hip abduction with the knee extended (e) Knee flexion | 2 evaluators Inclinometer Lumbosant | 5 min jogging and stretching 2 trials, mean | 3 sessions 2 weeks | (a) SEM = 2.5°; MDC95% = 6.9° (b) SEM = 1.9°; MDC95% = 5.3° (c) SEM = 1.3°; MDC95% = 3.6° (d) SEM = 1.8°; MDC95% = 5.0° (e) SEM = 2.8°; MDC95% = 7.8° |
| Cejudo et al. (2015) [105] M (n = 25) F (n = 25) Recreational athletes | (a) Hip abduction with the knee extended (b) Hip abduction with the 90° hip flexion | Two evaluators Inclinometer | No warm-up 2 trials, mean | 4 sessions 2 weeks | (a) SEM = 2.0°; MDC95% = 5.5° (b) SEM = 2.1°; MDC95 = 5.8° |
| Cejudo et al. (unpublished data) M (n = 40) F (n = 18) Recreational athletes | (a) Hip adduction with the 90° hip flexion (b) Hip internal rotation with the knee flexed (c) Hip external rotation with the knee flexed | Two evaluators Inclinometer | No warm-up 2 trials, mean | 4 sessions 6–8 day apart | (a) SEM = 1.8°; MDC95% = 4.5° (b) SEM = 1.9°; MDC95% = 5.5° (c) SEM = 2.1°; MDC95% = 5.9° |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cejudo, A. Description of ROM-SPORT I Battery: Keys to Assess Lower Limb Flexibility. Int. J. Environ. Res. Public Health 2022, 19, 10747. https://doi.org/10.3390/ijerph191710747
Cejudo A. Description of ROM-SPORT I Battery: Keys to Assess Lower Limb Flexibility. International Journal of Environmental Research and Public Health. 2022; 19(17):10747. https://doi.org/10.3390/ijerph191710747
Chicago/Turabian StyleCejudo, Antonio. 2022. "Description of ROM-SPORT I Battery: Keys to Assess Lower Limb Flexibility" International Journal of Environmental Research and Public Health 19, no. 17: 10747. https://doi.org/10.3390/ijerph191710747
APA StyleCejudo, A. (2022). Description of ROM-SPORT I Battery: Keys to Assess Lower Limb Flexibility. International Journal of Environmental Research and Public Health, 19(17), 10747. https://doi.org/10.3390/ijerph191710747