Abstract
One of the most significant innovations in HIV prevention is the use of HIV treatment to prevent HIV transmission. This information has been disseminated as the “Undetectable = Untransmittable” (U = U) message. Despite evidence of effectiveness, U = U awareness, belief, and understanding remains limited in some communities. In this study, we examine whether having an LGBTQ affirming healthcare provider increases U = U awareness, belief, and understanding among midlife and older gay and bisexual men in the US south, an understudied and underserved population and region where new HIV infections are increasing. We used data from the Vanderbilt University Social Networks Aging and Policy Study (VUSNAPS) on sexual minority men aged 50 to 76 from four southern US states collected in 2020–2021. We found that only one in four men reported prior awareness of U = U, but awareness was higher among men who have an LGBTQ affirming provider. Among HIV negative men, those with an affirming provider were more likely to believe and understand U = U, have more accurate risk perception, and have ever tested for HIV. Improving access to LGBTQ affirming healthcare may improve U = U awareness, belief, and understanding, which could help to curb HIV transmission in the US south.
1. Introduction
One of the most significant innovations in HIV prevention in the last two decades has been the use of HIV treatment to prevent HIV transmission. The resulting global public health campaign, “Undetectable equals Untransmittable”, or U = U, underscores the importance of achieving and maintaining viral suppression in people living with HIV to prevent HIV transmission. By taking antiretroviral therapy (ART) daily as prescribed, people living with HIV cannot sexually transmit the virus to others [1]. In the US, this campaign has been widely supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, and the American Medical Association [1,2,3].
Large-scale survey studies using data collected from community-based samples of people living with HIV and men who have sex with men generally find very high levels of awareness of the U = U concept in the US [4,5] and observe increases in awareness of U = U over the last decade, especially among men living with HIV [5,6]. Among HIV negative men surveyed from 2017 and 2018 in the US, 85% report being aware of U = U [7].
However, several studies of men who have sex with men in the US suggest that understanding and application of U = U are substantially more limited. Online surveys of men who have sex with men consistently find that just three to four out of every ten men who have sex with men correctly identify HIV treatment or viral suppression as providing protection against transmission [8,9,10].
Importantly, existing studies have not generally focused on U = U awareness and understanding among midlife and older sexual minority men. The median age of most U = U awareness studies that include sexual minority men in the US is consistently younger than 40 and, for some, younger than 35 or even 30 [4,7,9,10]. One study that explicitly assessed age-cohort differences in HIV prevention knowledge, risk perception, and behaviors among gay and bisexual men in the US found that men in younger age-cohorts had greater functional knowledge of HIV prevention strategies, including condom use, pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP), and Treatment as Prevention/U = U [8].
Additionally, among studies with adequate sample sizes to test geographic variation within the US, HIV negative men living in southern states in the US were significantly less likely to have heard of U = U [7], and men living with HIV in southern states were less likely to rate the U = U concept as accurate compared to men living with HIV in the northeast and western states [11]. These gaps are important because southern states comprise more than 50% of new HIV infections, most of which are among men who have sex with men [12]. Additionally, fewer people in the south are aware that they are living with HIV compared to other US regions, delaying access to treatment, and there has been a lower uptake of other medical prevention technologies, such as PrEP [12,13].
In this study, we address gaps in the U = U landscape and expand on existing work by examining healthcare-related determinants of U = U awareness, understanding, and impact among midlife and older sexual minority men in the US south. Although many sexual minority men hear about the U = U message from sources other than a healthcare provider, healthcare providers remain an important source of information about U = U [4] and points of regular contact for HIV-positive men on treatment and HIV-negative men seeking sexual healthcare services or who are taking PrEP. However, a substantial share of sexual minority men do not talk to healthcare providers about sexual behavior and, thus, may not be receiving adequate sexual health care [14,15]. A recent national study found that, among men who have sex with men in the US, 30% of those with a primary care provider reported that they had not disclosed their sexual orientation to their primary healthcare provider [7].
Patients may not disclose their sexual behavior or identity for several reasons, including because providers do not ask, past negative experiences, fear of homophobia and stigmatization, internalized stigma, and belief that health is not related to their identity [16,17,18]. In a study of the Veterans Health Care Administration (VHA), more than one-third of gay, lesbian, and bisexual veterans (36.9%) reported that VHA staff “definitely does not know” about their sexual orientation and a quarter (25.1%) reported avoiding seeking services because of concerns about confidentiality, stigma, or acceptance of their sexual orientation [19].
There are also challenges to providing culturally and clinically appropriate care to LGBTQ people on the provider side. Today, the American Medical Association openly advocates for inclusion and nondiscrimination of LGBTQ+ patients and providers [20]. Although acceptance of LGBTQ people varies by physician specialty [21] and by reported versus implicitly held beliefs [22], studies generally find that many providers’ attitudes towards LGBTQ people are positive and have improved over time [23,24]. Nonetheless, many physicians still have difficulty providing LGBTQ affirming care—care that is respectful and meets the specific health needs of LGBTQ people--because they were not trained to do so. Half of US medical schools dedicate fewer than 5 hours to LGBTQ topics and decisions to include LGBTQ-related curricula at all are largely made by individual institutions [25,26]. As a result, many practitioners find it difficult to use unfamiliar sexual and gender terms, decide on which ward to nurse a transgender patient, discuss interpersonal violence and abuse with same-sex partners, and identify LGBTQ health care resources, despite otherwise holding positive attitudes toward LGBTQ people [16,27].
A lack of fluency in LGBTQ health, identities, and behaviors among providers can lead patients to delay or forgo care, even care that is not related to their LGBTQ identity or sexual health, and to not disclose their LGBTQ identities to providers [16,17,28]. Older sexual minority adults are particularly likely to report personal experiences or expectations of discrimination in healthcare settings, leading to delays in accessing care or forgone care [18]. For providers, patient nondisclosure or lack of comfort discussing sexual health issues can lead to the provision of inappropriate care, inattention to specific health care needs, missed diagnostic screenings, and less focus overall on creating LGBTQ inclusive healthcare environments in entire practices [29,30]. Specifically, for sexual health, sexual minority men who do not disclose their sexual orientation to their primary care provider are less likely to have been tested for HIV in the previous two years, less likely to have been tested for gonorrhea and syphilis, and less likely to have been vaccinated against hepatitis A and B [15,31,32]. The lack of affirming care options for sexual minorities can also lead to healthcare fragmentation. Gay and bisexual men often seek care from providers outside of primary care contexts, especially for their sexual health needs, because of gaps in provider knowledge, greater comfort with community providers, financial cost, or expectations of discrimination [33].
The barriers to accessing and providing LGBTQ affirming care may be particularly acute in southern US states. Southern states are more likely than northeastern and western states to have laws that explicitly exclude or do not provide adequate care for sexual and gender minorities in healthcare [34]. Southern states also have fewer “LGBTQ Healthcare Equality Leaders” compared to northeast and western states, according to the Human Rights Campaign 2020 Healthcare Equality Index [35]. LGBTQ affirming healthcare providers are more likely to have explicit employee and patient nondiscrimination policies as well as staff training in LGBTQ patient-centered care [35]. Lack of nondiscrimination policies perpetuates discriminatory behaviors such as verbal abuse and refusal to provide care, which deter patients and limit them from obtaining essential care [16].
Based on this prior work, we expect that gay and bisexual men with LGBTQ affirming providers may have different outcomes in relation to key sexual health and HIV prevention outcomes. We tested this hypothesis using original data on U = U awareness, understanding, and belief among midlife and older gay and bisexual men in four southern states in the US.
2. Data and Methods
To examine the relationship among access to LGBTQ affirming care and knowledge and support of U = U among gay and bisexual men in the US south, we used data from the Vanderbilt University Social Networks, Aging, and Policy Study (VUSNAPS). VUSNAPS is a panel study of 1256 midlife and older LGBTQ adults aged 50 to 76 residing in Alabama, Georgia, North Carolina, and Tennessee. The VUSNAPS panel generally reflects the demographic characteristics of the LGBTQ population in the 50 to 76 age range for sample states and the US south as measured by the US Census Household Pulse Survey (HPS), Phase 3.2, weeks 34–39 (see Appendix A, Table A1). Compared to weighted HPS estimates of demographic characteristics of LGBTQ people in the US south census region, VUSNAPS participants are more educated, less likely to identify as bisexual, and less likely to identify as Latino/Hispanic. This study was approved by the Vanderbilt University Institutional Review Board.
VUSNAPS participants were recruited using purposeful online and venue-based sampling, linked referral, and community outreach to organizations serving LGBTQ, men who have sex with men, and seniors in each state. Wave 1 was fielded from 1 April 2020 to 30 September 2021. In this study, we restricted analyses to VUSNAPS respondents who identify as gay or bisexual men assigned male at birth with complete information on all independent and dependent variables (N = 633).
2.1. U = U Measures
The VUSNAPS survey instrument includes several items to gauge awareness, belief, application, and impact of the U = U message.
We measured awareness using the item, “Have you heard about U = U?” (1 = yes, 0 = no/don’t know). We also asked respondents who indicated having heard of U = U to identify where they heard of the concept. We also assessed general awareness with treatment as prevention using the item “I believe that HIV treatment makes people less likely to transmit the HIV virus”, rated on a 5-point Likert scale from 1 “disagree strongly” to 5 “agree very strongly”.
We measured belief in U = U using a detailed item that explains the U = U concept: “U = U means ‘Undetectable equals Untransmittable’, that is, HIV-positive people who take medication and bring their HIV viral load down to the point at which it is undetectable using standard medical tests cannot sexually transmit HIV to an HIV-negative partner. Please use the scale below to rate how much you believe the U = U concept”. Respondents were then presented with a Likert scale from 1 “Very unbelievable” to 5 “Very believable”. This item was recoded to 1 = ”Somewhat believable” or “Very believable” versus all others = 0.
To measure understanding of U = U, participants read the following vignette: “Please imagine a situation in which an HIV-positive man, who is taking medications and reduced his viral load to a point where it is undetectable, has unprotected anal sex with an HIV-negative man. The HIV-positive man is the top and he ejaculates inside the HIV-negative man. How likely do you think it is that the HIV-negative man will get the HIV virus from this encounter?” Response categories included a 7-point Likert scale from 1 “No chance or almost no chance”, 2 “Very unlikely”, 3 “Somewhat unlikely”, 4 “Not sure”, 5 “Somewhat likely”, 6 “Very likely”, 7 “Certain or almost certain”. For logistic analyses, we collapse responses “No chance” and “Very unlikely = 1 (correct understanding) versus all others = 0.
Finally, we measured the impact of U = U on risk perception using the item “I would feel safe having sex with someone who is HIV-positive as long as he is receiving treatment and has reduced his viral load to a point where it is undetectable”. Respondents rated their level of agreement on a 5-point Likert scale from 1 “Strongly disagree” to 5 “Strongly agree”. For logistic analyses, we collapsed “Agree” and “Strongly agree” = 1 versus all others = 0.
2.2. Affirming Care Measures
The VUSNAPS instrument includes several measures to assess healthcare access and utilization, including whether the respondent has a usual source of care, whether the respondent has a primary or secondary health care provider whom they perceive as LGBTQ affirming, and reasons for not having an LGBTQ affirming provider if no affirming provider is identified.
To assess access to an LGBTQ affirming provider, respondents were asked, “Do you have an LGBT affirming health care provider?” with response options: “Yes, they are my primary health care provider”; “Yes, I see them in addition to another health care provider”; “No, I don’t need or want an LGBT affirming health care provider”; “No, I cannot find an LGBT affirming health care provider in my area”; “I don’t know”; and “No answer”. Respondents who reported “Yes” were coded as having access to an LGBTQ affirming health care provider. No answer was coded as missing. All others were coded as no.
2.3. Covariates
We included demographic characteristics including age, education (high school or less, some college, college degree, and graduate or professional degree), partnered, race/ethnicity (white, black, other\multiracial), HIV status, and, for HIV negative men, whether they have ever had an HIV test.
2.4. Analytic Strategy
We conduct descriptive analyses and logistic regression analyses stratified by HIV status for each U = U outcome identified above, controlling for state of residence, age, education, race/ethnicity, whether the respondent has a partner or spouse, whether the respondent reported hearing of U = U prior to the survey, and whether they have ever tested for HIV (HIV negative men only).
3. Results
Table 1 presents the distribution of the sample across demographic and geographic characteristics for gay and bisexual men in the VUSNAPS sample stratified by HIV status. Men living with HIV were significantly more likely to have an LGBTQ affirming care provider, to be Black or other\multiracial compared to White, and to have less education than men who were HIV negative.

Table 1.
Characteristics of older gay and bisexual men in the US south by HIV status, VUSNAPS.
3.1. LGBTQ Affirming Care
About two of every three men in the study (64.8%) identified a primary or secondary healthcare provider as LGBTQ affirming. Just over half of HIV negative men (59.0%) identified their healthcare provider as LGBTQ affirming compared with almost all (87.3%) of men living with HIV. After adjusting for state of residence and demographic characteristics (age, education, race/ethnicity), men living with HIV were more than seven times more likely to identify their healthcare provider as LGBTQ affirming compared with HIV negative men (OR = 7.10; 95% CI = 3.94–12.80; see Table 2). Having an LGBTQ affirming care provider increased the odds that HIV negative men reported ever testing for HIV by more than two times (OR = 2.26; 95% CI = 1.38–3.72).

Table 2.
Odds of reporting an LGBTQ affirming provider and ever testing for HIV among a sample of midlife and older gay and bisexual men in the US south, VUSNAPS.
3.2. Awareness of U = U
The most well-studied dimension of the U = U concept is sexual minority men’s awareness of U = U. Only about one in four (25.4%) gay and bisexual men in the four sample states had previously heard of the U = U concept specifically; a majority (70.5%) had not heard of the U = U concept or were uncertain (4.4%). Men living with HIV (56.3%) were significantly more likely to have heard of U = U specifically compared with HIV negative men (17.5%; χ2 = 85.83; p < 0.001). Both HIV negative men and men living with HIV who had an LGBTQ affirming provider were significantly more likely to have heard about U = U specifically compared to men of the same HIV status without an affirming provider (p < 0.001; see Table 3). While most had not heard of U = U specifically, a larger share of gay and bisexual men (76.0%) was generally aware of the idea of treatment as prevention—that HIV treatment makes people less likely to transmit the virus. Again, men were more likely to have general awareness of U = U when they had an LGBTQ+ affirming provider (χ2 = 11.24; p ≤ 0.001).

Table 3.
Characteristics of midlife and older gay and bisexual men in the US south by HIV status, VUSNAPS.
In logistic regression analyses adjusting for other respondent characteristics and geographic variation (see Table 4), we found that HIV negative men with an affirming care provider were more than three times more likely to have heard of U = U (OR = 3.13; 95% CI = 1.75–5.61). Even among men living with HIV, who had high overall awareness of U = U, those with an affirming care provider were almost five times more likely to report having heard of U = U (OR = 4.87; 95% CI = 1.31–18.05).

Table 4.
Estimates of U = U awareness among a sample of midlife and older gay and bisexual men in the US south by HIV status, VUSNAPS.
Among those who had heard of U = U specifically (N = 160), the most common sources of initial information were 1) the internet (26.3%), 2) a television or print advertisement or story (23.1%), or 3) a health care provider (19.4%). Respondents also indicated that they had heard about U = U from community outreach and meetings, family or friends, and social networking or dating apps. We observed significant differences in how participants heard about U = U by whether the respondent also reported having an LGBTQ affirming healthcare provider (χ2 = 18.11; p < 0.01). Among those with an LGBTQ affirming provider, 21.2% heard about U = U from their healthcare provider compared with just 8.7% among those not reporting an LGBTQ affirming healthcare provider. Among HIV negative men, those who reported hearing about U = U from a healthcare provider all indicated that their provider was LGBTQ affirming. Sample size limitations prohibit us from further disaggregation or adjusted analyses of information sources.
We found similar results for general awareness of treatment as prevention among HIV negative gay and bisexual men. In logistic regression analyses adjusting for other respondent characteristics and geographic variation (see Table 5), we found that HIV negative men with an affirming care provider were almost two times more likely to be aware of the idea of treatment as prevention (OR = 1.78; 95% CI = 1.16–2.72).

Table 5.
Estimates of general awareness of treatment as prevention among a sample of midlife and older gay and bisexual men in the US south by HIV status, VUSNAPS.
3.3. Believability of U = U
Following a short description of the U = U concept, a majority of sexual minority men rated U = U as “very believable” (35.1%) or “somewhat believable” (26.5%). About a quarter (23.4%) were unsure and a nontrivial minority rated U = U as “very unbelievable” (5.8%) or somewhat unbelievable (9.3%). In bivariate analyses, individuals with an LGBTQ affirming care provider were significantly more likely than individuals without an affirming care provider to rate U = U as “somewhat” or “very believable” (67.0% versus 51.6%; χ2 = 31.35; p < 0.001). This difference remains when bivariate analyses are restricted to just HIV negative men (63.3% vs. 49.0%; χ2 = 16.37; p < 0.001).
After controlling for other demographic and geographic factors in an adjusted logistic regression model (see Table 6), we found that HIV negative men with an LGBTQ affirming provider are one-and-a-half times more likely to rate the U = U concept as “somewhat” or “very believable” (OR = 1.53; 95% CI = 1.02–2.30).

Table 6.
Estimates of U = U belief among a sample of midlife and older gay and bisexual men in the US south by HIV status, VUSNAPS.
3.4. Understanding of U = U
Participants were asked to apply the U = U concept to assess the likelihood that an HIV negative man would contract HIV in a hypothetical, condomless sexual encounter with a man living with HIV who was on treatment and had an undetectable viral load. Individuals with an LGBTQ affirming provider were more likely to correctly identify that the HIV negative man had “no chance or almost no chance” of contracting the virus during the described sexual encounter (26.3% vs. 9.4%; χ2 = 39.39; p < 0.001). Although men living with HIV were more likely to correctly understand the U = U concept in this context, the gap in understanding by whether individuals had an affirming care provider was present for both HIV negative men and men living with HIV.
In adjusted logistic regression analyses (see Table 7), we found that HIV negative men with an LGBTQ affirming care provider were about one-and-a-half times more likely to understand and correctly apply the U = U concept to a hypothetical scenario significant at the p < 0.1 level (OR = 1.45; 95% CI = 0.96–2.20).

Table 7.
Estimates of understanding of U = U among a sample of midlife and older gay and bisexual men in the US south by HIV status, VUSNAPS.
3.5. Impact of U = U on Risk Perception
To assess the impact of U = U on perceived risk, we asked participants to rate their level of agreement with the statement “I would feel safe having sex with someone who is HIV-positive as long as they are receiving treatment and have reduced their viral load to a point where it is undetectable”. A majority (57.0%) of sexual minority men agreed or strongly agreed with this statement. HIV positive men (87.9%) were significantly more likely to agree or strongly agree compared with HIV negative men (49.1%; χ2 = 64.42; p < 0.001). Among HIV negative men, those with an LGBTQ affirming care provider (56.1%) were significantly more likely to view having sex with someone who is HIV positive and undetectable as “safe” compared with HIV negative men who did not report an LGBTQ affirming provider (37.0%; χ2 = 17.66; p < 0.001). After controlling for other respondent demographic characteristics and geographic location (see Table 8), we found that having an LGBTQ affirming care provider increased the odds of feeling safe having sex with someone who is HIV positive and undetectable by almost two-and-a-half times (OR = 2.02; 95% CI = 1.33–3.05).

Table 8.
Estimates of impact of U = U on risk perception among a sample of midlife and older gay and bisexual men in the US south by HIV status, VUSNAPS.
4. Discussion
In this paper, we examined the relationship between having an LGBTQ affirming provider and several U = U related outcomes, including awareness, belief, understanding, and impact on risk perception. About two-thirds of sexual minority men in the study reported having an LGBTQ affirming healthcare provider as their primary or secondary provider. Unsurprisingly, men living with HIV were several times more likely to report having an LGBTQ affirming healthcare provider compared with HIV negative men.
Strikingly, the midlife and older gay and bisexual men in the US south surveyed by VUSNAPS were largely unaware of “U = U” and the “undetectable = untransmittable” language, even though a majority were generally familiar with the idea of treatment as prevention. This was especially true of HIV negative men in this study, only 17.5% of whom reported being aware of U = U specifically prior to the study. Awareness of U = U in this study was substantially lower than in other international and US surveys of people living with HIV and men who have sex with men that find high (70–90%) awareness of U = U [4,5,7]. Higher awareness in other studies may be due to sampling strategies that primarily engage individuals attached to organizations for people living with HIV, use of measures that assess general understanding of treatment as prevention rather than U = U specific awareness, or lack of disaggregation of HIV negative from men living with HIV in some samples. In other work, HIV negative and unknown status men who have sex with men are significantly less likely to be aware of U = U [5]. Additionally, VUSNAPS is a study of midlife and older LGBTQ adults aged 50 to 76 in a region that is disproportionately growing in HIV cases relative to the rest of the US [12], has fewer HIV and LGBTQ affirming providers [35], has more rural and suburban LGBTQ adults [36,37], and has poorer access to healthcare overall [38]. Unlike other convenience sample studies, VUSNAPS purposefully recruited from a range of online and community venues that included but were not limited to HIV and LGBTQ community organizations, and, thus, the sample may reflect a population that is less well-connected to HIV care and information. Unlike other samples of substantially younger men who have sex with men, VUSNAPS also focuses exclusively on midlife and older sexual and gender minority populations in the US south.
On all U = U outcomes—awareness, belief, understanding, and impact on risk perception—we observe that HIV negative men with an affirming care provider have a greater likelihood of a positive outcome (see Figure 1). This result is replicated when examining general awareness of treatment as prevention, the idea behind the U = U message. HIV negative men with an LGBTQ affirming care provider are also more than two times more likely to have ever received an HIV test compared to HIV negative men without an affirming care provider. Importantly, we also observe significant improvement in awareness of the U = U concept among men living with HIV who have an LGBTQ affirming care provider compared with men living with HIV who do not have an affirming care provider.
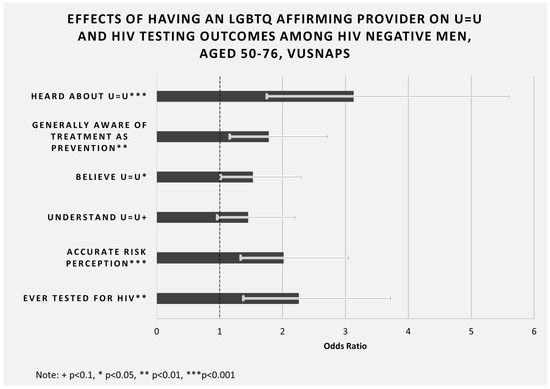
Figure 1.
Effects of having an LGBTQ affirming provider on U = U and HIV testing outcomes among HIV negative men, aged 50--76, VUSNAPS. Note: Adjusted odds ratios are presented for HIV negative men only from the analyses presented in Table 2, Table 4, Table 5, Table 6 and Table 7. Analyses control for state of residence, age, education, race/ethnicity, partner status, ever tested for HIV (except for models where this is the outcome), and ever heard of U = U (except for models where this is the outcome). All odds ratios are significant at the p < 0.05 level or higher, except “Understand U = U”, which is significant at the p < 0.1 level.
There may be several mechanisms that produce these improved U = U outcomes. We find that those with an LGBTQ affirming care provider were more likely to have heard about U = U from a healthcare provider. This finding is consistent with broader findings that sexual minority patients are more likely to communicate about their specific health needs and behaviors in affirming care contexts [39]. LGBTQ affirming providers may also be more comfortable having conversations about HIV and sexual health with sexual minority men.
These findings have important implications for clinical guidance and medical education. Most physicians are comfortable treating gay patients, especially more recent medical school graduates [23,24,28,40]. However, additional clinical training and medical education courses on how to provide LGBTQ affirming care would likely decrease gaps in U = U awareness and understanding and may increase HIV testing among midlife and older HIV negative men in the US south. Other institution and practice level changes, such as the adoption of explicit nondiscrimination policies for patients and employees and the use of inclusive language and images in health care settings, may improve LGBTQ patient outcomes. In this study, healthcare providers were among the top three sources of information about U = U, and men reporting an LGBTQ affirming provider were significantly more likely to have heard about U = U from their healthcare provider.
Improving access to and provision of LGBTQ affirming care among sexual minority men may also reduce HIV stigma within the LGBTQ community. We find that having an LGBTQ affirming care provider increased the odds of feeling safe having sex with someone who is living with HIV and has an undetectable viral load by almost two-and-a-half times (OR = 2.02; 95% CI = 1.33–3.05). Decreasing HIV stigma is important for the well-being of men living with HIV and increases testing among HIV negative men [41].
This study has some limitations. First, assessment of whether respondents had access to an LGBTQ affirming provider did not provide a definition or example. Future work should unpack the behaviors or cues that underpin patient perceptions of affirming or nonaffirming care. Second, while we see strong signals of the effects of having an LGBTQ affirming provider for HIV negative men, we lack the power to assess differences among men living with HIV, the vast majority of whom report an LGBTQ affirming provider as their primary or secondary healthcare provider. We are also unable to disaggregate experiences across race/ethnicity and sexual identity among HIV negative men. New HIV infections in southern states are growing fastest among Black men who have sex with men. Our findings suggest but cannot confirm that greater access to LGBTQ affirming care would be particularly beneficial for increasing U = U awareness and HIV testing among Black sexual minority men in the south.
5. Conclusions
The southern region has the greatest burden of HIV-related deaths in the US. Compared with those unaware of U = U, people living with HIV who have U = U-related discussions with a health care provider have better odds of adherence to HIV treatments and viral suppression [4]. This paper demonstrates that expanding LGBTQ affirming care may help reduce HIV-related mortality in the south by improving U = U awareness and uptake of HIV testing among midlife and older HIV negative men.
Author Contributions
Conceptualization, T.M., E.-R.A. and J.H.; methodology, T.M. and E.-R.A.; software, T.M.; validation, T.M. and E.-R.A.; formal analysis, T.M.; investigation, T.M. and J.H.; resources, T.M. and J.H.; data curation, T.M.; writing—original draft preparation, T.M., A.C., I.G. and N.K.; writing—review and editing, E.-R.A., J.H., A.C., I.G. and N.K.; visualization, T.M.; supervision, T.M.; project administration, T.M.; funding acquisition, T.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Institute on Aging, grant number R01AG063771, and Vanderbilt University.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Human Research Protections Program of Vanderbilt University and Vanderbilt University Medical Center (#200117, approved 03/03/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We thank the participants; the Project Coordinator, Katerri Kelly; study management staff at The Henne Group, Inc., especially Sergio Garcia and Nyree Young; Co-Investigators on the VUSNAPS project; and members of the Vanderbilt LGBTQ+ Policy Lab who provided valuable feedback on the project.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A

Table A1.
Comparison of VUSNAPS Sample Characteristics with Census Household Pulse Survey Estimates for LGBT Adults Aged 50–76 in 2021.
Table A1.
Comparison of VUSNAPS Sample Characteristics with Census Household Pulse Survey Estimates for LGBT Adults Aged 50–76 in 2021.
| US Census Household Pulse Survey, Weeks 34–39 | |||||
|---|---|---|---|---|---|
| VUSNAPS Wave 1 | South | Difference | Sample States Only | National | |
| Gender | |||||
| Male | 0.5470 | 0.5394 | −0.0076 | 0.5014 | 0.5459 |
| Female | 0.3798 | 0.3915 | 0.0117 | 0.3895 | 0.3862 |
| Transgender | 0.0629 | 0.0575 | −0.0054 | 0.0897 | 0.0580 |
| None of these | 0.0104 | 0.0116 | 0.0012 | 0.0193 | 0.0099 |
| Sexual Orientation | |||||
| Gay or lesbian | 0.8591 | 0.6232 | −0.2359 | 0.5581 | 0.6202 |
| Straight | 0.0080 | 0.0643 | 0.0563 | 0.0864 | 0.0588 |
| Bisexual | 0.1091 | 0.2584 | 0.1493 | 0.2731 | 0.2829 |
| Something else | 0.2070 | 0.0198 | −0.1872 | 0.0494 | 0.0180 |
| I don’t know | 0.0032 | 0.0334 | 0.0302 | 0.0329 | 0.0189 |
| Age | |||||
| 50–54 | 0.2158 | 0.2433 | 0.0275 | 0.1921 | 0.2176 |
| 55–59 | 0.3392 | 0.2777 | −0.0615 | 0.3094 | 0.2986 |
| 60–64 | 0.2205 | 0.1956 | −0.0249 | 0.2013 | 0.2000 |
| 65–69 | 0.1481 | 0.1803 | 0.0322 | 0.1794 | 0.1652 |
| 70–74 | 0.0709 | 0.0774 | 0.0065 | 0.0805 | 0.0938 |
| 75–76 | 0.0056 | 0.0258 | 0.0202 | 0.0373 | 0.0249 |
| Race | |||||
| White only | 0.8615 | 0.6636 | −0.1979 | 0.6139 | 0.6689 |
| African American/Black only | 0.0796 | 0.1143 | 0.0347 | 0.1691 | 0.0914 |
| Latino/Hispanic | 0.0104 | 0.1694 | 0.1590 | 0.1406 | 0.1578 |
| Asian only | 0.0040 | 0.0143 | 0.0103 | 0.0147 | 0.0315 |
| Other/Multiracial | 0.0446 | 0.0384 | −0.0062 | 0.0318 | 0.0504 |
| Education | |||||
| High school or less | 0.0537 | 0.3873 | 0.3336 | 0.4505 | 0.3515 |
| Some college/AA | 0.2384 | 0.2931 | 0.0547 | 0.2629 | 0.2945 |
| College degree | 0.3157 | 0.1572 | −0.1585 | 0.1184 | 0.1640 |
| Graduate degree | 0.3922 | 0.1624 | −0.2298 | 0.1682 | 0.1899 |
| Marital Status | |||||
| Married | 0.4307 | 0.4112 | −0.0195 | 0.4000 | 0.4202 |
| Widowed | 0.0358 | 0.0623 | 0.0265 | 0.0652 | 0.0496 |
| Divorced | 0.1513 | 0.1829 | 0.0316 | 0.2095 | 0.1694 |
| Separated | 0.0183 | 0.0306 | 0.0123 | 0.0173 | 0.0313 |
| Never married | 0.3639 | 0.3131 | −0.0508 | 0.3080 | 0.3294 |
Note: Census Household Pulse Survey (HPS) estimates incorporate data from Phase 3.2, Weeks 34 to 39, which covers the period of 21 July 2021 to 11 October 2021. We pool HPS data to account for smaller sample sizes among older adults and LGBTQ populations in the Southern US Census Region. Sample states include Alabama, Georgia, North Carolina, and Tennessee. For estimation purposes, the HPS sample is limited to older adults aged 50–76 at time of interview who are cisgender and lesbian, gay, or bisexual, or who are transgender and any sexual orientation. Transgender includes individuals who self-identify their gender as “transgender” and any individual whose sex assigned at birth is different from their current gender identity. Estimates exclude individuals who report their sexual orientation as “Something Else or “Don’t Know” who are not transgender.
References
- National Institute of Allergy and Infectious Diseases HIV Undetectable=Untransmittable (U=U), or Treatment as Prevention. Available online: https://www.niaid.nih.gov/diseases-conditions/treatment-prevention (accessed on 9 December 2021).
- American Medical Association AMA Adopts New Public Health Policies to Improve Health of National American Medical Association. Available online: https://www.ama-assn.org/press-center/press-releases/ama-adopts-new-public-health-policies-improve-health-nation-3 (accessed on 9 December 2021).
- US Centers for Disease Control and Prevention HIV Treatment as Prevention. Available online: https://www.cdc.gov/hiv/risk/art/index.html (accessed on 9 December 2021).
- Okoli, C.; Van De Velde, N.; Richman, B.; Allan, B.; Castellanos, E.; Young, B.; Brough, G.; Eremin, A.; Corbelli, G.M.; Britton, M.M.; et al. Undetectable equals untransmittable (U = U): Awareness and associations with health outcomes among people living with HIV in 25 countries. Sex Transm. Infect. 2021, 97, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Bor, J.; Fischer, C.; Modi, M.; Richman, B.; Kinker, C.; King, R.; Calabrese, S.K.; Mokhele, I.; Sineke, T.; Zuma, T.; et al. Changing Knowledge and Attitudes Towards HIV Treatment-as-Prevention and “Undetectable = Untransmittable”: A Systematic Review. AIDS Behav. 2021, 25, 4209–4224. [Google Scholar] [CrossRef] [PubMed]
- Holt, M.; Lea, T.; Schmidt, H.M.; Murphy, D.; Rosengarten, M.; Crawford, D.; Ellard, J.; Kolstee, J.; de Wit, J. Increasing Belief in the Effectiveness of HIV Treatment as Prevention: Results of Repeated, National Surveys of Australian Gay and Bisexual Men, 2013–2015. AIDS Behav. 2016, 20, 1564–1571. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, P.B.; Westmoreland, D.A.; Patel, V.V.; Grov, C. Awareness and Acceptability of Undetectable = Untransmittable Among a U.S. National Sample of HIV-Negative Sexual and Gender Minorities. AIDS Behav. 2021, 25, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Kahle, E.M.; Sullivan, S.P.; Stephenson, R. Birth Cohort Variations Across Functional Knowledge of HIV Prevention Strategies, Perceived Risk, and HIV-Associated Behaviors Among Gay, Bisexual, and Other Men Who Have Sex with Men in the United States. Am. J. Mens Health 2018, 12, 1824–1834. [Google Scholar] [CrossRef]
- Siegel, K.; Meunier, É. Awareness and Perceived Effectiveness of HIV Treatment as Prevention Among Men Who Have Sex with Men in New York City. AIDS Behav. 2019, 23, 1974–1983. [Google Scholar] [CrossRef]
- Carter, A.; Lachowsky, N.; Rich, A.; Forrest, J.I.; Sereda, P.; Cui, Z.; Roth, E.; Kaida, A.; Moore, D.; Montaner, J.S.G.; et al. Gay and bisexual men’s awareness and knowledge of treatment as prevention: Findings from the Momentum Health Study in Vancouver, Canada. J. Int. AIDS Soc. 2015, 18, 20039. [Google Scholar] [CrossRef]
- Rendina, H.J.; Parsons, J.T. Factors associated with perceived accuracy of the Undetectable = Untransmittable slogan among men who have sex with men: Implications for messaging scale-up and implementation. J. Int. AIDS Soc. 2018, 21, e25055. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. HIV in the Southern United States; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019; Volume 29, pp. 1–4. [Google Scholar]
- Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States, 2015–2019; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2021; Volume 26. [Google Scholar]
- Petroll, A.E.; Mosack, K.E. Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sex. Transm. Dis. 2011, 38, 63–67. [Google Scholar] [CrossRef]
- Ng, B.E.; Moore, D.; Michelow, W.; Hogg, R.; Gustafson, R.; Robert, W.; Kanters, S.; Thumath, M.; McGuire, M.; Gilbert, M. Relationship between disclosure of same-sex sexual activity to providers, HIV diagnosis and sexual health services for men who have sex with men in Vancouver, Canada. Can. J. Public Health 2014, 105, e186–e191. [Google Scholar] [CrossRef]
- Khalili, J.; Leung, L.B.; Diamant, A.L. Finding the Perfect Doctor: Identifying Lesbian, Gay, Bisexual, and Transgender–Competent Physicians. Am. J. Public Health 2015, 105, 1114. [Google Scholar] [CrossRef] [PubMed]
- Rossman, K.; Salamanca, P.; Macapagal, K. A Qualitative Study Examining Young Adults’ Experiences of Disclosure and Nondisclosure of LGBTQ Identity to Health Care Providers. J. Homosex. 2017, 64, 1390–1410. [Google Scholar] [CrossRef]
- MetLife Mature Market Institute. Still Out, Still Aging: The MetLife Study of Lesbian, Gay, Bisexual, and Transgender Baby Boomers; MetLife: Westport, CT, USA, 2010. [Google Scholar]
- Simpson, T.L.; Balsam, K.F.; Cochran, B.N.; Lehavot, K.; Gold, S.D. Veterans administration health care utilization among sexual minority veterans. Psychol. Serv. 2013, 10, 223–232. [Google Scholar] [CrossRef] [PubMed]
- American Medical Association Creating an LGBTQ-Friendly Practice. Available online: https://www.ama-assn.org/delivering-care/population-care/creating-lgbtq-friendly-practice (accessed on 13 December 2021).
- Sitkin, N.A.; Pachankis, J.E. Specialty Choice Among Sexual and Gender Minorities in Medicine: The Role of Specialty Prestige, Perceived Inclusion, and Medical School Climate. LGBT Health 2016, 3, 451. [Google Scholar] [CrossRef] [PubMed]
- Sabin, J.A.; Riskind, R.G.; Nosek, B.A. Health Care Providers’ Implicit and Explicit Attitudes Toward Lesbian Women and Gay Men. Am. J. Public Health 2015, 105, 1831. [Google Scholar] [CrossRef]
- Aleshire, M.E.; Ashford, K.; Fallin-Bennett, A.; Hatcher, J. Primary Care Providers’ Attitudes Related to LGBTQ People: A Narrative Literature Review. Health Promot. Pract. 2019, 20, 173–187. [Google Scholar] [CrossRef]
- Marlin, R.; Kadakia, A.; Ethridge, B.; Mathews, W.C. Physician Attitudes Toward Homosexuality and HIV: The PATHH-III Survey. LGBT Health 2018, 5, 431. [Google Scholar] [CrossRef]
- Obedin-Maliver, J.; Goldsmith, E.S.; Stewart, L.; White, W.; Tran, E.; Brenman, S.; Wells, M.; Fetterman, D.M.; Garcia, G.; Lunn, M.R. Lesbian, Gay, Bisexual, and Transgender–Related Content in Undergraduate Medical Education. JAMA 2011, 306, 971–977. [Google Scholar] [CrossRef]
- Keuroghlian, A.S.; Ard, K.L.; Makadon, H.J. Advancing health equity for lesbian, gay, bisexual and transgender (LGBT) people through sexual health education and LGBT-affirming health care environments. Sex Health 2017, 14, 119–122. [Google Scholar] [CrossRef]
- Parameshwaran, V.; Cockbain, B.C.; Hillyard, M.; Price, J.R. Is the Lack of Specific Lesbian, Gay, Bisexual, Transgender and Queer/Questioning (LGBTQ) Health Care Education in Medical School a Cause for Concern? Evidence From a Survey of Knowledge and Practice Among UK Medical Students. J. Homosex. 2017, 64, 367–381. [Google Scholar] [CrossRef]
- Mimiaga, M.J.; Goldhammer, H.; Belanoff, C.; Tetu, A.M.; Mayer, K.H. Men who have sex with men: Perceptions about sexual risk, HIV and sexually transmitted disease testing, and provider communication. Sex Transm. Dis. 2007, 34, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Makadon, H.J. Improving Health Care for the Lesbian and Gay Communities. New Engl. J. Med. 2006, 354, 895–897. [Google Scholar] [CrossRef] [PubMed]
- Mayer, K.H.; Bradford, J.B.; Makadon, H.J.; Stall, R.; Goldhammer, H.; Landers, S. Sexual and Gender Minority Health: What We Know and What Needs to Be Done. Am. J. Public Health 2008, 98, 989. [Google Scholar] [CrossRef]
- Stupiansky, N.W.; Liau, A.; Rosenberger, J.; Rosenthal, S.L.; Tu, W.; Xiao, S.; Fontenot, H.; Zimet, G.D. Young Men’s Disclosure of Same Sex Behaviors to Healthcare Providers and the Impact on Health: Results from a US National Sample of Young Men Who Have Sex with Men. AIDS Patient Care 2017, 31, 342–347. [Google Scholar] [CrossRef]
- Metheny, N.; Stephenson, R. Disclosure of Sexual Orientation and Uptake of HIV Testing and Hepatitis Vaccination for Rural Men Who Have Sex with Men. Ann. Fam. Med. 2016, 14, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Nahata, L.; Quinn, G.P.; Caltabellotta, N.M.; Tishelman, A.C. Mental Health Concerns and Insurance Denials among Transgender Adolescents. LGBT Health 2017, 4, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Movement Advancement Project Equality Maps: Healthcare Laws and Policies. Available online: https://www.lgbtmap.org/equality-maps/healthcare_laws_and_policies (accessed on 22 August 2022).
- Human Rights Campaign. Healthcare Equality Index 2020; Human Rights Campaign Foundation: Washington, DC, USA, 2020. [Google Scholar]
- Stone, A.L. The Geography of Research on LGBTQ Life: Why sociologists should study the South, rural queers, and ordinary cities. Sociol. Compass 2018, 12, e12638. [Google Scholar] [CrossRef]
- The Williams Institute LGBT Data & Demographics. Available online: https://williamsinstitute.law.ucla.edu/visualization/lgbt-stats/?topic=LGBT&area=4#density (accessed on 29 May 2020).
- Artiga, S.; Damico, A. Health and Health Coverage in the South: A Data Update; Kaiser Family Foundation: Washington, DC, USA, 2016. [Google Scholar]
- Mendoza, N.S.; Moreno, F.A.; Hishaw, G.A.; Gaw, A.C.; Fortuna, L.R.; Skubel, A.; Porche, M.V.; Roessel, M.H.; Shore, J.; Gallegos, A. Affirmative Care Across Cultures: Broadening Application. Focus Am. Psychiatr. Publ. 2020, 18, 31–39. [Google Scholar] [CrossRef]
- Smith, D.M.; Mathews, W.C. Physicians’ attitudes toward homosexuality and HIV: Survey of a California Medical Society- revisited (PATHH-II). J. Homosex. 2007, 52, 1–9. [Google Scholar] [CrossRef]
- Young, S.D.; Bendavid, E. The relationship between HIV testing, stigma, and health service usage. AIDS Care 2010, 22, 373–380. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).