Sexual Risk Behavior and Lifetime HIV Testing: The Role of Adverse Childhood Experiences
Abstract
:1. Introduction
1.1. ACES and HIV Risk
1.2. ACEs and HIV Testing
2. Materials and Methods
2.1. Exposure Variable
2.2. Outcome Variable
2.3. Moderator Variable
2.4. Covariates
2.5. Analyses
2.6. Missing Data
2.7. Quality Assurance
3. Results
3.1. Sample Characteristics
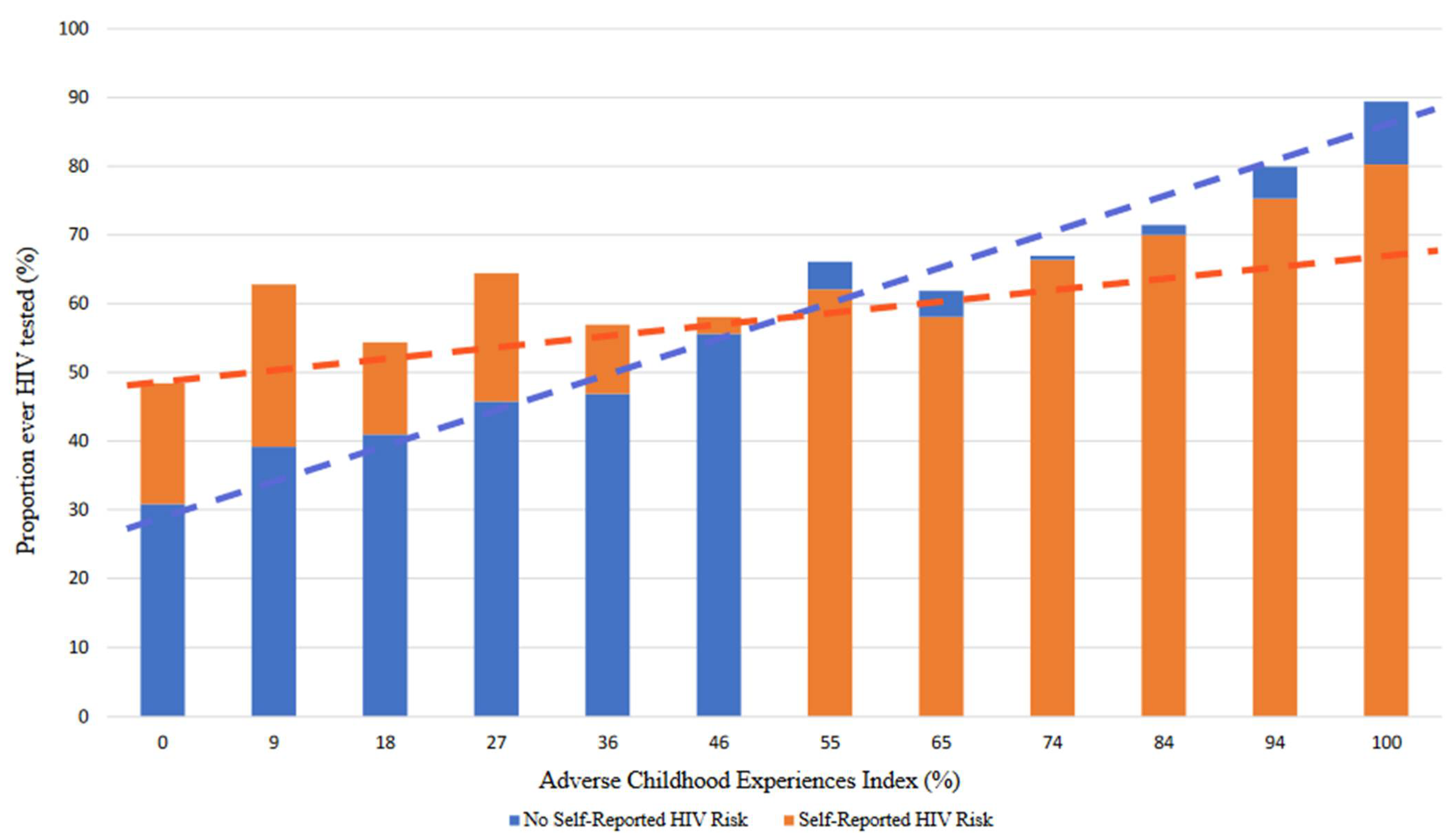
3.2. ACEs Bivariate Analyses
3.3. Regression Modeling
3.4. Post Hoc Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beyrer, C. A Pandemic Anniversary: 40 Years of HIV/AIDS. Lancet 2021, 397, 2142–2143. [Google Scholar] [CrossRef]
- CDC. Basic Statistics. Available online: https://www.cdc.gov/hiv/basics/statistics.html (accessed on 22 December 2021).
- Dyer, T.V.; Turpin, R.E.; Stall, R.D.; Khan, M.R.; Nelson, L.E.; Brewer, R.A.; Friedman, M.R.; Mimiaga, M.J.; Cook, R.L.; O’Cleirigh, C. Latent Profile Analysis of a Syndemic of Vulnerability Factors on Incident STI in a Cohort of Black Men Who Have Sex with Men Only (BMSMO) and Black Men Who Have Sex with Men and Women (BMSMW) in the HPTN061 Study. Sex. Transm. Dis. 2020, 47, 571. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.G.; Park, J.N.; Galai, N.; Allen, S.T.; Huettner, S.S.; Silberzahn, B.E.; Decker, M.R.; Poteat, T.C.; Footer, K.H. Drivers of HIV Infection among Cisgender and Transgender Female Sex Worker Populations in Baltimore City: Results from the SAPPHIRE Study. JAIDS J. Acquir. Immune Defic. Syndr. 2019, 80, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Turpin, R.E.; Slopen, N.; Chen, S.; Boekeloo, B.; Dallal, C.; Dyer, T. Latent Class Analysis of a Syndemic of Risk Factors on HIV Testing among Black Men. AIDS Care 2019, 31, 216–223. [Google Scholar] [CrossRef]
- Chang, J.L.; Tsai, A.C.; Musinguzi, N.; Haberer, J.E.; Boum, Y.; Muzoora, C.; Bwana, M.; Martin, J.N.; Hunt, P.W.; Bangsberg, D.R. Depression and Suicidal Ideation among HIV-Infected Adults Receiving Efavirenz versus Nevirapine in Uganda: A Prospective Cohort Study. Ann. Intern. Med. 2018, 169, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Turpin, R.E.; Salerno, J.P.; Rosario, A.D.; Boekeloo, B. Victimization, Substance Use, Depression, and Sexual Risk in Adolescent Males Who Have Sex with Males: A Syndemic Latent Profile Analysis. Arch. Sex. Behav. 2021, 50, 961–971. [Google Scholar] [CrossRef]
- Tyree, G.A.; Vaida, F.; Zisook, S.; Mathews, W.C.; Grelotti, D.J. Clinical Correlates of Depression Chronicity among People Living with HIV: What Is the Role of Suicidal Ideation? J. Affect. Disord. 2019, 258, 163–171. [Google Scholar] [CrossRef]
- Chan, R.C.; Mak, W.W.; Ma, G.Y.; Cheung, M. Interpersonal and Intrapersonal Manifestations of HIV Stigma and Their Impacts on Psychological Distress and Life Satisfaction among People Living with HIV: Toward a Dual-Process Model. Qual. Life Res. 2021, 30, 145–156. [Google Scholar] [CrossRef]
- Krueger, E.A.; Holloway, I.W.; Lightfoot, M.; Lin, A.; Hammack, P.L.; Meyer, I.H. Psychological Distress, Felt Stigma, and HIV Prevention in a National Probability Sample of Sexual Minority Men. LGBT Health 2020, 7, 190–197. [Google Scholar] [CrossRef]
- Gurung, S.; Ventuneac, A.; Cain, D.; Mirzayi, C.; Ferraris, C.; Rendina, H.J.; Sparks, M.A.; Parsons, J.T. Alcohol and Substance Use Diagnoses among HIV-Positive Patients Receiving Care in NYC Clinic Settings. Drug Alcohol Depend. 2017, 180, 62–67. [Google Scholar] [CrossRef]
- Nydegger, L.A.; Claborn, K.R. Exploring Patterns of Substance Use among Highly Vulnerable Black Women At-Risk for HIV through a Syndemics Framework: A Qualitative Study. PLoS ONE 2020, 15, e0236247. [Google Scholar] [CrossRef] [PubMed]
- Torres, T.S.; Bastos, L.S.; Kamel, L.; Bezerra, D.R.; Fernandes, N.M.; Moreira, R.I.; Garner, A.; Veloso, V.G.; Grinsztejn, B.; De Boni, R.B. Do Men Who Have Sex with Men Who Report Alcohol and Illicit Drug Use before/during Sex (Chemsex) Present Moderate/High Risk for Substance Use Disorders? Drug Alcohol Depend. 2020, 209, 107908. [Google Scholar] [CrossRef] [PubMed]
- Fredericksen, R.J.; Fitzsimmons, E.; Gibbons, L.E.; Dougherty, S.; Loo, S.; Shurbaji, S.; Batey, D.S.; Avendano-Soto, S.; Mathews, W.C.; Christopoulos, K. Development and Content Validation of the Multifactoral Assessment of Perceived Social Support (MAPSS), a Brief, Patient-Reported Measure of Social Support for Use in HIV Care. AIDS Care 2019, 31, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geter, A.; Sutton, M.Y.; Hubbard McCree, D. Social and Structural Determinants of HIV Treatment and Care among Black Women Living with HIV Infection: A Systematic Review: 2005–2016. AIDS Care 2018, 30, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Luo, D.; Chen, X.; Zhang, D.; Huang, Z.; Xiao, S. HIV-Related Stress Experienced by Newly Diagnosed People Living with HIV in China: A 1-Year Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 2681. [Google Scholar] [CrossRef] [Green Version]
- Quinn, K.G.; Spector, A.; Takahashi, L.; Voisin, D.R. Conceptualizing the Effects of Continuous Traumatic Violence on HIV Continuum of Care Outcomes for Young Black Men Who Have Sex with Men in the United States. AIDS Behav. 2021, 25, 758–772. [Google Scholar] [CrossRef]
- Jones, C.M.; Merrick, M.T.; Houry, D.E. Identifying and Preventing Adverse Childhood Experiences: Implications for Clinical Practice. JAMA 2020, 323, 25–26. [Google Scholar] [CrossRef]
- Kajeepeta, S.; Gelaye, B.; Jackson, C.L.; Williams, M.A. Adverse Childhood Experiences Are Associated with Adult Sleep Disorders: A Systematic Review. Sleep Med. 2015, 16, 320–330. [Google Scholar] [CrossRef] [Green Version]
- Merrick, M.T.; Ports, K.A.; Ford, D.C.; Afifi, T.O.; Gershoff, E.T.; Grogan-Kaylor, A. Unpacking the Impact of Adverse Childhood Experiences on Adult Mental Health. Child Abuse Negl. 2017, 69, 10–19. [Google Scholar] [CrossRef]
- Kelly-Irving, M.; Mabile, L.; Grosclaude, P.; Lang, T.; Delpierre, C. The Embodiment of Adverse Childhood Experiences and Cancer Development: Potential Biological Mechanisms and Pathways across the Life Course. Int. J. Public Health 2013, 58, 3–11. [Google Scholar] [CrossRef]
- Nemeroff, C.B. Paradise Lost: The Neurobiological and Clinical Consequences of Child Abuse and Neglect. Neuron 2016, 89, 892–909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.J.; Thacker, L.R.; Cohen, S.A. Association between Adverse Childhood Experiences and Diagnosis of Cancer. PLoS ONE 2013, 8, e65524. [Google Scholar] [CrossRef]
- Holman, D.M.; Ports, K.A.; Buchanan, N.D.; Hawkins, N.A.; Merrick, M.T.; Metzler, M.; Trivers, K.F. The Association Between Adverse Childhood Experiences and Risk of Cancer in Adulthood: A Systematic Review of the Literature. Pediatrics 2016, 138, S81–S91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, L.A.; Filipp, S.L.; Mack, J.A.; Mercado, R.E.; Barnes, A.; Bright, M.; Shenkman, E.A.; Gurka, M.J. Specific Adverse Childhood Experiences and Their Association with Other Adverse Childhood Experiences, Asthma and Emotional, Developmental and Behavioral Problems in Childhood. Pediatr. Res. 2020, 88, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.; Gjelsvik, A.; Nocera, M.; McQuaid, E.L. Association between Adverse Childhood Experiences in the Home and Pediatric Asthma. Ann. Allergy Asthma Immunol. 2015, 114, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Anda, R.F.; Brown, D.W.; Dube, S.R.; Bremner, J.D.; Felitti, V.J.; Giles, W.H. Adverse Childhood Experiences and Chronic Obstructive Pulmonary Disease in Adults. Am. J. Prev. Med. 2008, 34, 396–403. [Google Scholar] [CrossRef]
- Cunningham, T.J.; Ford, E.S.; Croft, J.B.; Merrick, M.T.; Rolle, I.V.; Giles, W.H. Sex-Specific Relationships between Adverse Childhood Experiences and Chronic Obstructive Pulmonary Disease in Five States. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 1033–1043. [Google Scholar] [CrossRef] [Green Version]
- Chapman, D.P.; Dube, S.R.; Anda, R.F. Adverse Childhood Events as Risk Factors for Negative Mental Health Outcomes. Psychiatr. Ann. 2007, 37, 359. [Google Scholar]
- Wade Jr, R.; Cronholm, P.F.; Fein, J.A.; Forke, C.M.; Davis, M.B.; Harkins-Schwarz, M.; Pachter, L.M.; Bair-Merritt, M.H. Household and Community-Level Adverse Childhood Experiences and Adult Health Outcomes in a Diverse Urban Population. Child Abuse Negl. 2016, 52, 135–145. [Google Scholar] [CrossRef]
- Collins, P.Y.; Velloza, J.; Concepcion, T.; Oseso, L.; Chwastiak, L.; Kemp, C.G.; Simoni, J.; Wagenaar, B.H. Intervening for HIV Prevention and Mental Health: A Review of Global Literature. J. Int. AIDS Soc. 2021, 24 (Suppl. 2), e25710. [Google Scholar] [CrossRef]
- Remien, R.H.; Stirratt, M.J.; Nguyen, N.; Robbins, R.N.; Pala, A.N.; Mellins, C.A. Mental Health and HIV/AIDS: The Need for an Integrated Response. AIDS 2019, 33, 1411–1420. [Google Scholar] [CrossRef] [PubMed]
- Schilling, E.A.; Aseltine, R.H.; Gore, S. Adverse Childhood Experiences and Mental Health in Young Adults: A Longitudinal Survey. BMC Public Health 2007, 7, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheffler, J.L.; Stanley, I.; Sachs-Ericsson, N. Chapter 4—ACEs and Mental Health Outcomes. In Adverse Childhood Experiences; Asmundson, G.J.G., Afifi, T.O., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 47–69. ISBN 978-0-12-816065-7. [Google Scholar]
- Campbell, J.A.; Walker, R.J.; Egede, L.E. Associations Between Adverse Childhood Experiences, High-Risk Behaviors, and Morbidity in Adulthood. Am. J. Prev. Med. 2016, 50, 344–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, L.; Chuang, D.-M.; Lee, Y. Adverse Childhood Experiences, Gender, and HIV Risk Behaviors: Results from a Population-Based Sample. Prev. Med. Rep. 2016, 4, 113–120. [Google Scholar] [CrossRef] [Green Version]
- Hillis, S.D.; Anda, R.F.; Felitti, V.J.; Marchbanks, P.A. Adverse Childhood Experiences and Sexual Risk Behaviors in Women: A Retrospective Cohort Study. Fam. Plan. Perspect. 2001, 33, 206–211. [Google Scholar] [CrossRef]
- CDC. HIV Testing. Available online: https://www.cdc.gov/hiv/testing/index.html (accessed on 9 January 2022).
- Gamarel, K.E.; Nelson, K.M.; Stephenson, R.; Santiago Rivera, O.J.; Chiaramonte, D.; Miller, R.L. Anticipated HIV Stigma and Delays in Regular HIV Testing Behaviors among Sexually-Active Young Gay, Bisexual, and Other Men Who Have Sex with Men and Transgender Women. AIDS Behav. 2018, 22, 522–530. [Google Scholar] [CrossRef]
- Gwadz, M.; Leonard, N.R.; Honig, S.; Freeman, R.; Kutnick, A.; Ritchie, A.S. Doing Battle with “the Monster”: How High-Risk Heterosexuals Experience and Successfully Manage HIV Stigma as a Barrier to HIV Testing. Int. J. Equity Health 2018, 17, 46. [Google Scholar] [CrossRef]
- Kutner, B.A.; Simoni, J.M.; Aunon, F.M.; Creegan, E.; Balán, I.C. How Stigma toward Anal Sexuality Promotes Concealment and Impedes Health-Seeking Behavior in the US among Cisgender Men Who Have Sex with Men. Arch. Sex. Behav. 2021, 50, 1651–1663. [Google Scholar] [CrossRef]
- Pantelic, M.; Sprague, L.; Stangl, A.L. It’s Not “All in Your Head”: Critical Knowledge Gaps on Internalized HIV Stigma and a Call for Integrating Social and Structural Conceptualizations. BMC Infect. Dis. 2019, 19, 210. [Google Scholar] [CrossRef]
- Koblin, B.A.; Tieu, H.-V.; Frye, V. Disparities in HIV/AIDS in Black Men Who Have Sex with Men. Lancet 2012, 380, 316–318. [Google Scholar] [CrossRef]
- Millett, G.A.; Jeffries, W.L., 4th; Peterson, J.L.; Malebranche, D.J.; Lane, T.; Flores, S.A.; Fenton, K.A.; Wilson, P.A.; Steiner, R.; Heilig, C.M. Common Roots: A Contextual Review of HIV Epidemics in Black Men Who Have Sex with Men across the African Diaspora. Lancet 2012, 380, 411–423. [Google Scholar] [CrossRef]
- Vermund, S.H. The Continuum of HIV Care in the Urban United States: Black Men Who Have Sex with Men (MSM) Are Less Likely than White MSM to Receive Antiretroviral Therapy. J. Infect. Dis. 2017, 216, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Hermanstyne, K.A.; Green, H.D., Jr.; Cook, R.; Tieu, H.-V.; Dyer, T.V.; Hucks-Ortiz, C.; Wilton, L.; Latkin, C.; Shoptaw, S. Social Network Support and Decreased Risk of Seroconversion in Black MSM: Results of the BROTHERS (HPTN 061) Study. J. Acquir. Immune Defic. Syndr. 2018, 78, 163. [Google Scholar] [CrossRef] [PubMed]
- Heaney, C.; Israel, B. Social Networks and Social Support. In Health Behavior and Health Education: Theory, Research and Practice; Glanz, K., Lewis, F.M., Rimer, B.K., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 1997; pp. 179–205. [Google Scholar]
- Baytop, C.; Royal, S.; Hubbard McCree, D.; Simmons, R.; Tregerman, R.; Robinson, C.; Johnson, W.D.; McLaughlin, M.; Price, C. Comparison of Strategies to Increase HIV Testing among African-American Gay, Bisexual, and Other Men Who Have Sex with Men in Washington, DC. AIDS Care 2014, 26, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Frye, V.; Wilton, L.; Hirshfield, S.; Chiasson, M.A.; Usher, D.; Lucy, D.; McCrossin, J.; Greene, E.; Koblin, B. All About Me Study Team “Just Because It’s out There, People Aren’t Going to Use It.” HIV Self-Testing among Young, Black MSM, and Transgender Women. AIDS Patient Care STDs 2015, 29, 617–624. [Google Scholar] [CrossRef] [Green Version]
- Farnham, P.G.; Gopalappa, C.; Sansom, S.L.; Hutchinson, A.B.; Brooks, J.T.; Weidle, P.J.; Marconi, V.C.; Rimland, D. Updates of Lifetime Costs of Care and Quality-of-Life Estimates for HIV-Infected Persons in the United States: Late versus Early Diagnosis and Entry into Care. JAIDS J. Acquir. Immune Defic. Syndr. 2013, 64, 183–189. [Google Scholar] [CrossRef] [Green Version]
- Kidman, R.; Kohler, H.-P. Adverse Childhood Experiences, Sexual Debut and HIV Testing among Adolescents in a Low-Income High HIV-Prevalence Context. AIDS 2019, 33, 2245–2250. [Google Scholar] [CrossRef]
- Bertolino, D.F.; Sanchez, T.H.; Zlotorzynska, M.; Sullivan, P.S. Adverse Childhood Experiences and Sexual Health Outcomes and Risk Behaviors among a Nationwide Sample of Men Who Have Sex with Men. Child Abuse Negl. 2020, 107, 104627. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. Behavioral Risk Factor Surveillance System (BRFSS), 2019; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2019. [Google Scholar]
- Young-Wolff, K.C.; Sarovar, V.; Sterling, S.A.; Leibowitz, A.; McCaw, B.; Hare, C.B.; Silverberg, M.J.; Satre, D.D. Adverse Childhood Experiences, Mental Health, Substance Use, and HIV-Related Outcomes among Persons with HIV. AIDS Care 2019, 31, 1241–1249. [Google Scholar] [CrossRef]
- Ujhelyi Nagy, A.; Kuritár Szabó, I.; Hann, E.; Kósa, K. Measuring the Prevalence of Adverse Childhood Experiences by Survey Research Methods. Int. J. Environ. Res. Public Health 2019, 16, 1048. [Google Scholar] [CrossRef] [Green Version]
- Woodring, J.V.; Kruszon-Moran, D.; Oster, A.M.; McQuillan, G.M. Did CDC’s 2006 Revised HIV Testing Recommendations Make a Difference? Evaluation of HIV Testing in the US Household Population, 2003–2010. J. Acquir. Immune Defic. Syndr. 2014, 67, 331. [Google Scholar] [CrossRef] [PubMed]
- Bond, L.; Lauby, J.; Batson, H. HIV Testing and the Role of Individual-and Structural-Level Barriers and Facilitators. AIDS Care 2005, 17, 125–140. [Google Scholar] [CrossRef] [PubMed]
- Crosby, R.A.; Miller, K.H.; Staten, R.R.; Noland, M. Prevalence and Correlates of HIV Testing among College Students: An Exploratory Study. Sex. Health 2005, 2, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Alcalá, H.E.; Valdez-Dadia, A.; von Ehrenstein, O.S. Adverse Childhood Experiences and Access and Utilization of Health Care. J. Public Health 2018, 40, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Sales, J.M.; Swartzendruber, A.; Phillips, A.L. Trauma-Informed HIV Prevention and Treatment. Curr. HIV/AIDS Rep. 2016, 13, 374–382. [Google Scholar] [CrossRef] [Green Version]
- Afifi, T.O.; Boman, J.; Fleisher, W.; Sareen, J. The Relationship between Child Abuse, Parental Divorce, and Lifetime Mental Disorders and Suicidality in a Nationally Representative Adult Sample. Child Abuse Negl. 2009, 33, 139–147. [Google Scholar] [CrossRef]
- Nelson, C.A.; Scott, R.D.; Bhutta, Z.A.; Harris, N.B.; Danese, A.; Samara, M. Adversity in Childhood Is Linked to Mental and Physical Health throughout Life. BMJ 2020, 371, m3048. [Google Scholar] [CrossRef]
- Meade, C.S.; Sikkema, K.J. Voluntary HIV Testing among Adults with Severe Mental Illness: Frequency and Associated Factors. AIDS Behav. 2005, 9, 465–473. [Google Scholar] [CrossRef]
- Evangeli, M.; Pady, K.; Wroe, A.L. Which Psychological Factors Are Related to HIV Testing? A Quantitative Systematic Review of Global Studies. AIDS Behav. 2016, 20, 880–918. [Google Scholar] [CrossRef] [Green Version]
- Bacon, H.; Richardson, S. Attachment Theory and Child Abuse: An Overview of the Literature for Practitioners. Child Abuse Rev. J. Br. Assoc. Study Prev. Child Abuse Negl. 2001, 10, 377–397. [Google Scholar] [CrossRef]
- Choi, K.R.; Stewart, T.; Fein, E.; McCreary, M.; Kenan, K.N.; Davies, J.D.; Naureckas, S.; Zima, B.T. The Impact of Attachment-Disrupting Adverse Childhood Experiences on Child Behavioral Health. J. Pediatr. 2020, 221, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Maguire, S.A.; Williams, B.; Naughton, A.M.; Cowley, L.E.; Tempest, V.; Mann, M.K.; Teague, M.; Kemp, A.M. A Systematic Review of the Emotional, Behavioural and Cognitive Features Exhibited by School-aged Children Experiencing Neglect or Emotional Abuse. Child Care Health Dev. 2015, 41, 641–653. [Google Scholar] [CrossRef] [PubMed]
- Westermair, A.L.; Stoll, A.M.; Greggersen, W.; Kahl, K.G.; Hüppe, M.; Schweiger, U. All Unhappy Childhoods Are Unhappy in Their Own Way—Differential Impact of Dimensions of Adverse Childhood Experiences on Adult Mental Health and Health Behavior. Front. Psychiatry 2018, 9, 198. [Google Scholar] [CrossRef] [PubMed]
- Brezing, C.; Ferrara, M.; Freudenreich, O. The Syndemic Illness of HIV and Trauma: Implications for a Trauma-Informed Model of Care. Psychosomatics 2015, 56, 107–118. [Google Scholar] [CrossRef]
- Mersky, J.P.; Janczewski, C.E.; Topitzes, J. Rethinking the Measurement of Adversity: Moving Toward Second-Generation Research on Adverse Childhood Experiences. Child Maltreat. 2017, 22, 58–68. [Google Scholar] [CrossRef]
| Total | No Self-Reported HIV Risk (n = 55,941, 96.0%) | Self-Reported HIV Risk (n = 2317, 4.0%) | p Value | |
|---|---|---|---|---|
| Sexual/Gender Identity 1 | <0.001 | |||
| Cisgender Bisexual Women | 1.40 | 1.81 | 7.58 | |
| Cisgender Bisexual Men | 0.69 | 0.76 | 3.48 | |
| Cisgender Gay Women | 0.57 | 0.67 | 0.61 | |
| Cisgender Gay Men | 0.77 | 0.73 | 7.14 | |
| Cisgender Heterosexual Women | 52.39 | 48.76 | 30.17 | |
| Cisgender Heterosexual Men | 41.56 | 43.92 | 47.59 | |
| Cisgender Other Sexual Identity Women | 0.59 | 0.56 | 0.87 | |
| Cisgender Other Sexual Identity Men | 0.37 | 0.48 | 0.82 | |
| Cisgender Questioning Women | 0.64 | 0.91 | 0.03 | |
| Cisgender Questioning Men | 0.31 | 0.41 | 0.33 | |
| Non-Binary | 0.41 | 0.64 | 0.47 | |
| Transgender Women | 0.14 | 0.19 | 0.59 | |
| Transgender Men | 0.14 | 0.16 | 0.32 | |
| Age2 | <0.001 | |||
| 18–24 | 11.06 | 9.67 | 32.19 | |
| 25–34 | 14.44 | 13.44 | 29.46 | |
| 35–44 | 15.12 | 15.05 | 16.22 | |
| 45–54 | 15.93 | 16.24 | 11.3 | |
| 55–64 | 18.01 | 18.69 | 7.61 | |
| 65 and older | 25.44 | 26.91 | 3.21 | |
| Race/Ethnicity 1 | <0.001 | |||
| Non-Hispanic White | 69.49 | 70.29 | 57.42 | |
| Non-Hispanic Black | 14.37 | 14.04 | 19.3 | |
| Non-Hispanic Multiracial | 0.73 | 0.72 | 0.89 | |
| Non-Hispanic Other Race | 2.21 | 2.28 | 1.18 | |
| Hispanic | 11.56 | 11.09 | 18.58 | |
| Income 2 | <0.001 | |||
| Less than $15,000 | 4.97 | 4.93 | 5.57 | |
| $15,000 to less than $20,000 | 8.14 | 8.01 | 10.16 | |
| $20,000 to less than $25,000 | 10.58 | 10.61 | 10.22 | |
| $25,000 to less than $35,000 | 12.01 | 11.96 | 12.74 | |
| $35,000 to less than $50,000 | 14.15 | 13.94 | 17.34 | |
| $50,000 to less than $75,000 | 15.8 | 15.78 | 16.08 | |
| $75,000 or more | 29.15 | 29.51 | 23.81 | |
| Education 2 | <0.001 | |||
| Did not graduate High School | 12.2 | 12.24 | 11.7 | |
| Graduated High School | 29.81 | 29.71 | 31.23 | |
| Attended College or Technical School | 32.01 | 31.55 | 39.13 | |
| Graduated from College or Technical School | 25.96 | 26.49 | 17.91 | |
| Ever Diagnosed with Depression 1 | 20.3 | 19.33 | 34.98 | <0.001 |
| Any Binge Drinking in the past 30 days 1 | 17.62 | 16.16 | 39.72 | <0.001 |
| Ever HIV Tested 1 | 42.89 | 41.18 | 68.72 | <0.001 |
| Total | Any Self-Reported HIV Risk | Any Self-Reported HIV Testing | Difference % in Risk Incongruent with Difference % in Testing 1 | |||
|---|---|---|---|---|---|---|
| No | Yes | No | Yes | |||
| Adverse Childhood Experiences 2 | ||||||
| Did you live with anyone who was depressed, mentally ill, or suicidal? | 18.16 | 16.96 | 36.24 | 14.31 | 23.28 | 53.48 |
| Did you live with anyone who was a problem drinker or alcoholic? | 24.11 | 23.27 | 36.82 | 20.77 | 28.55 | 42.58 |
| Did you live with anyone who used illegal street drugs or who abused prescription medications? | 11.33 | 10.22 | 28.15 | 7.65 | 16.24 | 52.09 |
| Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility? | 9.15 | 8.19 | 23.62 | 5.71 | 13.73 | 48.02 |
| Were your parents separated or divorced? | 31.26 | 29.92 | 51.47 | 24.13 | 40.76 | 22.83 |
| How often did your parents or adults in your home ever slap, hit, kick, punch or beat each other up? | 17.56 | 16.91 | 27.44 | 14.08 | 22.19 | 22.98 |
| Before age 18, how often did a parent or adult in your home ever hit, beat, kick, or physically hurt you in any way? Do not include spanking. | 24.95 | 24.00 | 39.25 | 21.04 | 30.15 | 40.26 |
| Did a parent or adult in your home ever swear at you, insult you, or put you down? | 33.88 | 32.38 | 56.57 | 28.79 | 40.66 | 50.93 |
| Did anyone at least 5 years older than you or an adult, ever touch you sexually? | 11.74 | 11.04 | 22.4 | 8.28 | 16.35 | 28.96 |
| Did anyone at least 5 years older than you or an adult, try to make you touch sexually? | 8.86 | 8.25 | 18.1 | 5.95 | 12.74 | 31.07 |
| Did anyone at least 5 years older than you or an adult, force you to have sex? | 5.25 | 4.79 | 12.29 | 2.96 | 8.31 | 28.67 |
| Median Adverse Childhood Experiences Index 2 | 9.01 | 9.01 | 27.27 | 9.01 | 18.18 | 33.33 |
| No Interactions | Interactions | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Self-Reported HIV Risk | 1.67 (1.58, 1.76) | 1.24 (1.17, 1.31) | 1.90 (1.74, 2.07) | 1.51 (1.38, 1.65) |
| ACEs Index | 2.77 (2.58, 2.97) | 2.19 (2.03, 2.37) | ||
| Self-Reported HIV Risk * ACEs Index 1 | 0.44 (0.37, 0.54) | 0.51 (0.42, 0.62) | ||
| Sexual and Gender Identity | ||||
| Cisgender Bisexual Women | 0.74 (0.64, 0.85) | 0.70 (0.61, 0.80) | ||
| Cisgender Bisexual Men | 0.80 (0.68, 0.93) | 0.79 (0.67 0.93) | ||
| Cisgender Gay Women | 1.00 (0.86, 1.17) | 0.92 (0.78, 1.07) | ||
| Cisgender Heterosexual Women | 0.75 (0.67, 0.83) | 0.77 (0.69, 0.85) | ||
| Cisgender Heterosexual Men | 0.69 (0.62, 0.77) | 0.72 (0.64, 0.80) | ||
| Cisgender Other Sexual Identity Women | 0.63 (0.47, 0.83) | 0.61 (0.47, 0.80) | ||
| Cisgender Other Sexual Identity Men | 0.51 (0.32, 0.80) | 0.53 (0.34 0.84) | ||
| Cisgender Questioning Women | 0.63 (0.45, 0.88) | 0.66 (0.47, 0.93) | ||
| Cisgender Questioning Men | 0.37 (0.23, 0.61) | 0.40 (0.24, 0.66) | ||
| Non-Binary | 0.48 (0.33, 0.70) | 0.52 (0.36, 0.75) | ||
| Transgender Women | 0.97 (0.73, 1.29) | 0.95 (0.74, 1.22) | ||
| Transgender Men | 0.77 (0.54, 1.08) | 0.78 (0.54, 1.12) | ||
| Cisgender Gay Men | Reference | Reference | ||
| Annual Household Income (Ordinal: Per $10,000 k) | 1.00 (0.99, 1.01) | 0.99 (0.98, 1.00) | ||
| Age (Ordinal: Per 10-years) | 0.90 (0.89, 0.92) | 0.91 (0.90, 0.92) | ||
| Highest Education Level (Ordinal: Per category 2) | 1.06 (1.04, 1.08) | 1.07 (1.05, 1.09) | ||
| Race/Ethnicity | ||||
| Non-Hispanic Black | 1.75 (1.67, 1.82) | 1.74 (1.67, 1.82) | ||
| Non-Hispanic Multiracial | 0.92 (0.76, 1.13) | 0.98 (0.79, 1.20) | ||
| Non-Hispanic Other Race | 1.55 (1.45, 1.66) | 1.56 (1.46, 1.67) | ||
| Hispanic | 1.40 (1.28, 1.53) | 1.33 (1.22, 1.46) | ||
| Non-Hispanic White | Reference | Reference | ||
| Ever Diagnosed with Depression | 1.31 (1.26, 1.36) | 1.18 (1.14, 1.23) | ||
| Binge Drinking past 30 days | 1.09 (1.04, 1.14) | 1.07 (1.02, 1.11) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dyer, T.V.; Turpin, R.E.; Hawthorne, D.J.; Jain, V.; Sayam, S.; Mittal, M. Sexual Risk Behavior and Lifetime HIV Testing: The Role of Adverse Childhood Experiences. Int. J. Environ. Res. Public Health 2022, 19, 4372. https://doi.org/10.3390/ijerph19074372
Dyer TV, Turpin RE, Hawthorne DJ, Jain V, Sayam S, Mittal M. Sexual Risk Behavior and Lifetime HIV Testing: The Role of Adverse Childhood Experiences. International Journal of Environmental Research and Public Health. 2022; 19(7):4372. https://doi.org/10.3390/ijerph19074372
Chicago/Turabian StyleDyer, Typhanye V., Rodman E. Turpin, David J. Hawthorne, Vardhmaan Jain, Sonica Sayam, and Mona Mittal. 2022. "Sexual Risk Behavior and Lifetime HIV Testing: The Role of Adverse Childhood Experiences" International Journal of Environmental Research and Public Health 19, no. 7: 4372. https://doi.org/10.3390/ijerph19074372
APA StyleDyer, T. V., Turpin, R. E., Hawthorne, D. J., Jain, V., Sayam, S., & Mittal, M. (2022). Sexual Risk Behavior and Lifetime HIV Testing: The Role of Adverse Childhood Experiences. International Journal of Environmental Research and Public Health, 19(7), 4372. https://doi.org/10.3390/ijerph19074372






