What Makes Urban Communities More Resilient to COVID-19? A Systematic Review of Current Evidence
Abstract
:1. Introduction
2. Materials and Methods
- (1)
- The articles in this study were collected from Web of Science, Scopus, and Springer Link, the main databases of global scientific articles. The keywords were set as “social resilience” AND “epidemic” (OR “pandemic”) (for the years 2012 to 2022) and set as “social resilience” (OR “social vulnerability”) AND “COVID-19*” (OR “coronavirus*” OR “SARS-CoV-2 virus”) (for the years 2019 to 2022). After removing duplicates, the search scope was limited to full-text published articles in English academic journals.
- (2)
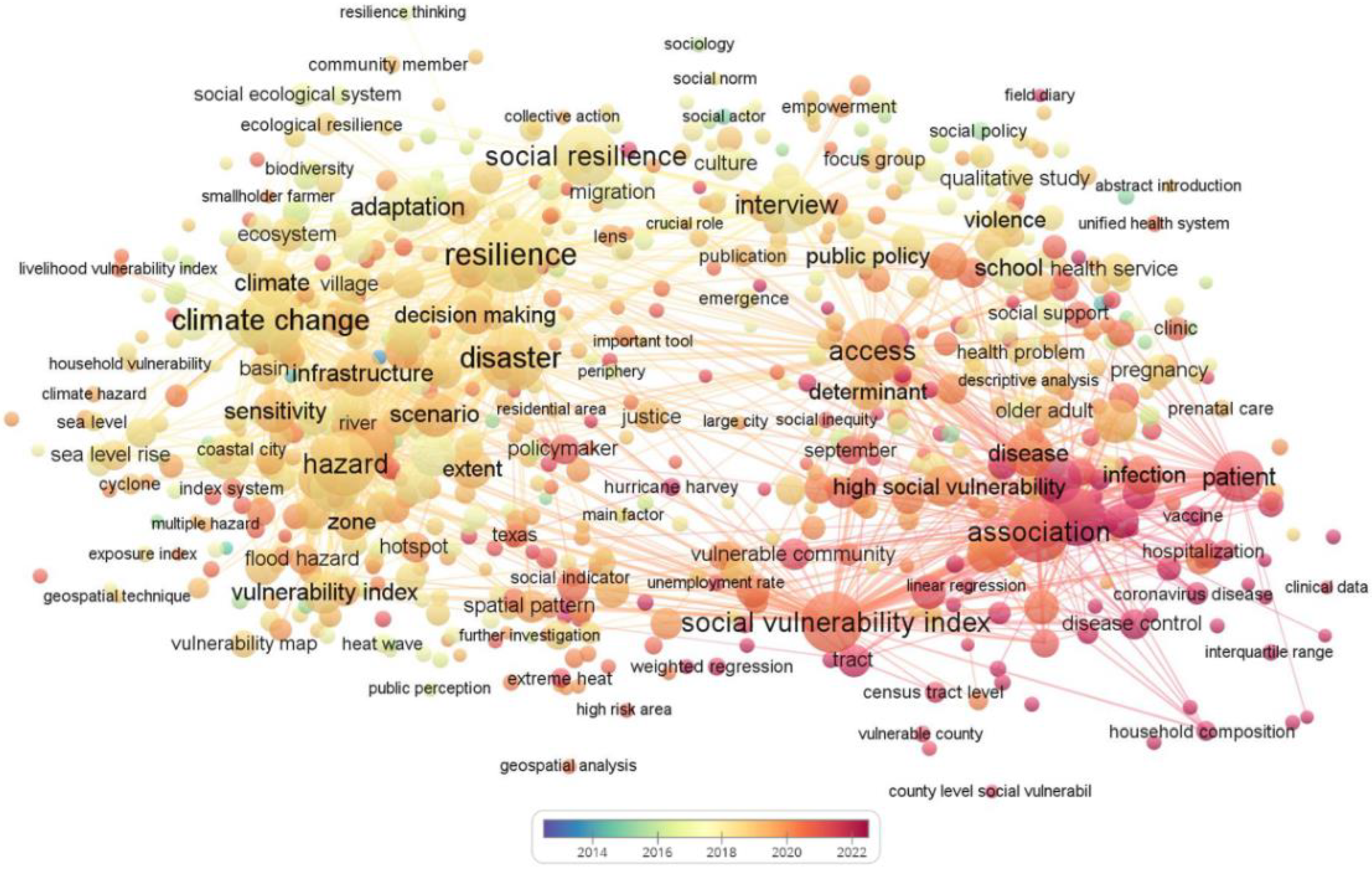
- VOSviewer software was used to visualize the articles’ “social resilience” AND “epidemic” (OR “pandemic”) (2012–2022). The articles were used as a data source for the knowledge mapping analysis after suggesting material, corrections, and other content not related to the research topic. The minimum number of occurrences of a term was selected as 10 and the most relevant term was chosen based on the relevance score. In this paper, 1600 terms were selected for inclusion in the glossary. In order to obtain a clearer visual description, less-used and irrelevant terms such as “age, year, etc.” were excluded, and the final number of relevant terms was determined to be 767.
- (3)
- The title, authors, source, keywords, and abstract of the papers were screened. At this stage, papers that were not related to “community governance in the context of COVID-19” were excluded.
- (4)
- In addition, articles were also excluded if they did not focus on social resilience in the COVID-19 context, or only used social resilience as a background for other activities; for example, just using the social vulnerability index (SVI) as a calculated metric to calculate metrics that evaluate other directions.
- (5)
- The authors conducted content analysis on the selected papers. Statistical and quantitative analyses on the framework, research level, and evaluation indicators were undertaken. In addition, the policies, recommendations and implementations, and influencing factors of social resilience in the COVID-19 context were summarized. For policy, we divided its content into positive and negative aspects. Bruneau summarized resilience as having the characteristics of robustness, redundancy, rapidity, and resourcefulness (i.e., the 4R characteristics), which can be relied upon to reduce the impact of disasters and to recover more quickly to the original state, or an even better state, in the face of shocks and stresses [34]. This paper discerns how social resilience can help communities withstand COVID-19 by summarizing the four characteristics of social resilience based on the impact of recommendations and implementation.
3. Results
3.1. VOSviewer Visual Analysis of Social Resilience (2012–2022)
3.2. Searching Process of Social Resilience (2019–2022)
3.3. The Policies about Social Resilience to the COVID-19
3.4. The Recommendations and Measures of Social Resilience to the COVID-19
| 4R | Recommendations and Measures | Citation |
|---|---|---|
| Rapidity | Improve current “stay-at-home” policies that can have a psychiatric impact on community residents Focus on vulnerable groups and maintain appropriate neighborhood relations Establishing an URI (Urban Resilience Index) | [58,59,60,61] |
| Redundancy | Accessibility measures for COVID-19 patients need additional medical resources to improve Adopt comprehensive policies and measures to address substandard vaccine coverage for migrant workers and minorities Increasing vaccination rates among frontline workers | [62,63,64,65,66] |
| Resourcefulness | A strong system of local institutions working in concert with the state is needed to build a community-based, resilience-centered social resilience framework, a district-level CPVI, a conceptual model of CHASMS Government recommended to use digital telemedicine divide to address barriers to online treatment The importance of monitoring society through community questionnaires to prevent future COVID-19 transmission Government needs targeted vaccines for strategic vaccination to reduce inequities (focus on older populations), active advocacy and increased trust in vaccines among groups hesitant to vaccinate | [67,68,69,70,71,72,73,74,75] |
| Robustness | Improving coverage of emergency treatment response calls for low social resilience Governments need to balance policy and social side effects to strengthen the resilience of the system and facilitate the process of modeling the socio-spatial structure of urban space Prioritize public health and public support to control COVID-19 when chronic disease and COVID-19 coexist People’s daily lives have changed, and social sharing platforms should learn from each other about effective COVID-19 responses to provide more sustainable consumption and production patterns Social practice can strengthen community beliefs, improve collective effectiveness, and increase the strength of social resilience | [50,51,52,53,54,55,56,57,76,77,78] |
- (1)
- Robustness generally starts with community health services, organizations and community solidarity to improve their resistance to COVID-19;
- (2)
- Redundancy is measured in terms of medical coverage, vaccination rates, and the distribution of vulnerable populations that are able to maintain good life-sustaining treatment and livelihoods despite exposure to COVID-19;
- (3)
- Resourcefulness starts with the resilience framework and evaluation system, in addition to scientific and technological support, to grasp the overall situation of the whole community at a macro level and facilitate the development of policies;
- (4)
- Rapidity is coupled with resourcefulness to enhance the community’s mastery of information, the rapid promulgation of policies, and the rational deployment of resources; these work together to achieve effective prevention and rapid control of COVID-19.
3.5. The Factors Influencing Social Resilience to the COVID-19
4. Discussion
5. Conclusions
- (1)
- After the COVID-19 pandemic, many communities incurred unrecoverable losses, and there was a purposeful effort to combine social resilience with epidemic preparedness, focusing on major public health events as a social resilience direction to promote the expansion of the social resilience field.
- (2)
- Existing policies must be able to effectively control the spread of COVID-19, and the inadequacies of the policies should be investigated and evaluated, with additional recommendations and measures based on the resilience characteristics that need to be enhanced. Governments need to recognize that COVID-19 will be a near-term, ongoing epidemic, and need to take a long-term, dynamic approach to policy development. Furthermore, larger influences should be identified to fundamentally improve social resilience to COVID-19.
- (3)
- Increasing the strength and regulatory precision of social resilience requires both external intervention and its own regulation. External hard interventions of policy, capital, and health care coverage are complemented by moderate healing, such as public trust and sociocultural characteristics. This can keep the level of social resilience within a manageable range and help society to control COVID-19 on a large scale. Thus, social resilience can be gradually increased at a reasonable rate. The self-regulation of natural and human conditions can fundamentally produce positive improvements in social resilience. In particular, the regulation of the human condition serves as the basis for the regulation of social resilience. It also focuses on larger influencing factors such as vulnerable groups and spatial heterogeneity to solidify the social resilience against COVID-19 from the “ground up”. People can learn from each other to help each other and gradually become connected to form urban resilience, and eventually achieve national consolidation and stability.
Funding
Data Availability Statement
Conflicts of Interest
References
- Yang, C.; Sha, D.; Liu, Q.; Li, Y.; Lan, H.; Guan, W.W.; Hu, T.; Li, Z.; Zhang, Z.; Thompson, J.H.; et al. Taking the pulse of COVID-19: A spatiotemporal perspective. Int. J. Digit. Earth 2020, 13, 1186–1211. [Google Scholar] [CrossRef]
- Orea, L.; Álvarez, I.C. How effective has been the Spanish lockdown to battle COVID-19? A spatial analysis of the coronavirus propagation across provinces. Health Econ. 2020, 31, 154–173. [Google Scholar] [CrossRef]
- Giuliani, D.; Dickson, M.M.; Espa, G.; Santi, F. Modelling and Predicting the Spatio-Temporal Spread of Coronavirus Disease 2019 (COVID-19) in Italy. BMC Infect. Dis. 2020, 20, 700. [Google Scholar] [CrossRef] [Green Version]
- Arab-Mazar, Z.; Sah, R.; Rabaan, A.A.; Dhama, K.; Rodriguez-Morales, A.J. Mapping the incidence of the COVID-19 hotspot in Iran—Implications for Travellers. Travel Med. Infect. Dis. 2020, 34, 101630. [Google Scholar] [CrossRef]
- Franch-Pardo, I.; Napoletano, B.M.; Rosete-Verges, F.; Billa, L. Spatial analysis and GIS in the study of COVID-19. A review. Sci. Total Environ. 2020, 739, 140033. [Google Scholar] [CrossRef]
- Elavarasan, R.M.; Pugazhendhi, R.; Shafiullah, G.M.; Irfan, M.; Anvari-Moghaddam, A. A hover view over effectual approaches on pandemic management for sustainable cities-The endowment of prospective technologies with revitalization strategies. Sustain. Cities Soc. 2021, 68, 102789. [Google Scholar] [CrossRef]
- Mostafa, M.K.; Gamal, G.; Wafiq, A. The impact of COVID 19 on air pollution levels and other environmental indicators—A case study of Egypt. J. Environ. Manag. 2021, 277, 111496. [Google Scholar] [CrossRef]
- Chirwa, G.C.; Dulani, B.; Sithole, L.; Chunga, J.J.; Alfonso, W.; Tengatenga, J. Malawi at the Crossroads: Does the Fear of Contracting COVID-19 Affect the Propensity to Vote? Eur. J. Dev. Res. 2022, 34, 409–431. [Google Scholar] [CrossRef]
- Makhmudov, N.; Alisherovna, A.G.; Kazakov, A. Analysis of the effect of coronavirus (COVID-19) on the development of the world economic system. Int. J. Integr. Educ. 2020, 3, 143–156. [Google Scholar] [CrossRef]
- Coppola, F.; Faggiono, L.; Neri, E.; Grassi, R.; Miele, V. Impact of the COVID-19 outbreak on the profession and psychological wellbeing of radiologists: A nationwide online survey. Insights into Imaging 2021, 12, 23. [Google Scholar] [CrossRef]
- Vollono, C.; Rollo, E.; Romozzi, M.; Frisullo, G.; Servidei, S.; Borghetti, A.; Calabresi, P. Focal status epilepticus as unique clinical feature of COVID-19: A case report. Seizure Eur. J. Epilepsy 2020, 78, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Kresch, E.; Achua, J.; Saltzman, R.; Khodamoradi, K.; Arora, H.; Ibrahim, E.; Kryvenko, O.N.; Almeida, V.W.; Firdaus, F.; Hare, J.M.; et al. COVID-19 Endothelial Dysfunction Can Cause Erectile Dysfunction: Histopathological, Immunohistochemical, and Ultrastructural Study of the Human Penis. World J. Mens Health 2021, 39, 466–469. [Google Scholar] [CrossRef] [PubMed]
- Werthman-Ehrenreich, A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am. J. Emerg. Med. 2021, 42, 264.e5–264.e8. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.R.; Lee, R.D. Demographic perspectives on the mortality of COVID-19 and other epidemics. Proc. Natl. Acad. Sci. USA 2020, 117, 22035–22041. [Google Scholar] [CrossRef] [PubMed]
- Tönnies, F.; Loomis, C.P. Community and Society; Harper: Manhattan, NY, USA, 1963. [Google Scholar]
- Deng, P.; Ouyang, Y. Research on the Method of Improving Community Governance Capability Based on Block-Chain Technology. In Proceedings of the 2021 IEEE International Conference on Consumer Electronics and Computer Engineering (ICCECE), Guangzhou, China, 15–17 January 2021; pp. 706–709. [Google Scholar] [CrossRef]
- Van Belle, S.; Affun-Adegbule, C.; Soors, W.; Srinivas, P.N.; Hegel, G.; Van Damme, W.; Saluja, D.; Abejirinde, I.; Wouters, E.; Masquillier, C.; et al. COVID-19 and informal settlements: An urgent call to rethink urban governance. Int. J. Equity Health 2020, 19, 81. [Google Scholar] [CrossRef] [PubMed]
- Gu, E.; Li, L. Crippled community governance and suppressed scientific/professional communities: A critical assessment of failed early warning for the COVID-19 outbreak in China. J. Chin. Gov. 2020, 5, 160–177. [Google Scholar] [CrossRef] [Green Version]
- Zaman, S.; Hossain, F.; Matin, I. Ethnography of community governance: A case of COVID-19 response of an urban slum in Bangladesh. Community Dev. J. 2022. [Google Scholar] [CrossRef]
- Wang, F.; Fang, Y.Y.; Deng, H.D.; Wei, F.Z. How community medical facilities can promote resilient community constructions under the background of pandemics. Indoor Built Environ. 2022, 31, 1018–1027. [Google Scholar] [CrossRef]
- Cui, J.; Liu, X. Study on Community Integration and Community Governance of Korean Residents in Tianjin International Community Amid the COVID-19 Pandemic. Stud. Koreans Abroad 2021, 55, 129–161. [Google Scholar] [CrossRef]
- Turner, B.L. Vulnerability and resilience: Coalescing or paralleling approaches for sustainability science? Glob. Environ. Chang. Hum. Policy Dimens. 2010, 20, 570–576. [Google Scholar] [CrossRef]
- Klein, R.J.T.; Nicholls, R.; Thomalla, F.J. Hazards, Resilience to natural hazards: How useful is this concept? Glob. Environ. Chang. Part B Environ. Hazards 2003, 5, 35–45. [Google Scholar] [CrossRef]
- Béné, C.; Evans, L.; Mills, D.; Ovie, S.; Raji, A.; Tafida, A.; Kodio, A.; Sinaba, F.; Morand, P.; Lemoalle, J.; et al. Testing resilience thinking in a poverty context: Experience from the Niger River basin. Glob. Environ. Chang. Hum. Policy Dimens. 2011, 21, 1173–1184. [Google Scholar] [CrossRef]
- Davis, R.; Cook, D.; Cohen, L. A community resilience approach to reducing ethnic and racial disparities in health. Am. J. Public Health 2005, 95, 2168–2173. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.M.; Zhang, L.; Ye, L.J.; Yang, J.W.; Liu, Y.L.; Song, S.L. To take the initiative in the prevention and control of the coronavirus disease 2019 epidemic in the changing and unchanged strategies. Zhonghua Yi Xue Za Zhi 2022, 102, 463–467. [Google Scholar] [CrossRef]
- Moya, J.; Goenechea, M. An Approach to the Unified Conceptualization, Definition, and Characterization of Social Resilience. Int. J. Environ. Res. Public Health 2022, 19, 5746. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.L.; Lin, S.N.; Lu, T.T.; Shen, Y.; Liang, S.S. Towards a constructed order of co-governance: Understanding the state-society dynamics of neighbourhood collaborative responses to COVID-19 in urban China. Urban Stud. 2022. [Google Scholar] [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Aldhahi, M.I.; Akil, S.; Zaidi, U.; Mortada, E.; Award, S.; Al Awaji, N. Effect of Resilience on Health-Related Quality of Life during the COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 11394. [Google Scholar] [CrossRef]
- Myers, N. Information Sharing and Community Resilience: Toward a Whole Community Approach to Surveillance and Combatting the “Infodemic”. World Med. Health Policy 2021, 13, 581–592. [Google Scholar] [CrossRef]
- Ranjbari, M.; Esfandabadi, Z.S.; Zanetti, M.C.; Scagnelli, S.D.; Siebers, P.O.; Aghbashlo, M.; Peng, W.X.; Quatraro, F.; Tabatabaei, M. Three pillars of sustainability in the wake of COVID-19: A systematic review and future research agenda for sustainable development. J. Clean. Prod. 2021, 297, 126660. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruneau, M.; Chang, S.E.; Eguchi, R.T.; Lee, G.C.; O’Rourke, T.D.; Reinhorn, A.M.; Shinozuka, M.; Tierney, K.; Wallace, W.A.; Von Winterfeldt, D. A Framework to Quantitatively Assess and Enhance the Seismic Resilience of Communities. Earthq. Spectra 2019, 19, 733–752. [Google Scholar] [CrossRef] [Green Version]
- Keck, M.; Sakdapolrak, P. What is social resilience? Lessons learned and ways forward. Erdkunde 2013, 67, 5–19. [Google Scholar] [CrossRef]
- Miao, C.; Ding, M.T. Social vulnerability assessment of geological hazards based on entropy method in Lushan earthquake-stricken area. Arab. J. Geosci. 2015, 8, 10241–10253. [Google Scholar] [CrossRef]
- Aerts, J.; Botzen, W.J.; Clarke, K.C.; Cutter, S.L.; Hall, J.W.; Merz, B.; Michel-Kerjan, E.; Mysiak, J.; Surminski, S.; Kunreuther, H. Integrating human behaviour dynamics into flood disaster risk assessment. Nat. Clim. Chang. 2018, 8, 193–199. [Google Scholar] [CrossRef] [Green Version]
- Rufat, S.; Tate, E.; Emrich, C.T.; Antolini, F. How Valid Are Social Vulnerability Models? Ann. Am. Assoc. Geogr. 2019, 109, 1131–1153. [Google Scholar] [CrossRef]
- Luo, Z.W.; Li, L.; Ma, J.F.; Tang, Z.; Shen, H.; Zhu, H.H.; Wu, B. Moderating Effect of a Cross-Level Social Distancing Policy on the Disparity of COVID-19 Transmission in the United States. ISPRS Int. J. Geo Inf. 2022, 11, 229. [Google Scholar] [CrossRef]
- Huang, Q.; Jackson, S.; Derakhshan, S.; Lee, L.; Pham, E.; Jackson, A.; Cutter, S.L. Urban-rural differences in COVID-19 exposures and outcomes in the South: A preliminary analysis of South Carolina. PLoS ONE 2021, 16, e0246548. [Google Scholar] [CrossRef]
- Page-Tan, C.; Corbin, T.B. Protective policies for all? An analysis of COVID-19 deaths and protective policies among low-, medium-, and high-vulnerability groups. Disasters 2021, 45, S119–S145. [Google Scholar] [CrossRef]
- Fernandez-Prados, J.S.; Lozano-Diaz, A.; Muyor-Rodriguez, J. Factors explaining social resilience against COVID-19: The case of Spain. Eur. Soc. 2021, 23, S111–S121. [Google Scholar] [CrossRef]
- Mladenov, T.; Brennan, C.S. Social vulnerability and the impact of policy responses to COVID-19 on disabled people. Sociol. Health Illn. 2021, 43, 2049–2065. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.M.; Wang, A.L.C.; Grossman, M.K.; Pun, E.; Whiteman, A.; Deng, L.; Hallisey, E.; Shape, J.D.; Ussery, E.N.; Stokley, S.; et al. County-Level COVID-19 Vaccination Coverage and Social Vulnerability—United States, December 14, 2020–March 1, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Antonio-Villa, N.E.; Fernandez-Chirino, L.; Pisanty-Alatorre, J.; Mancilla-Galindo, J.; Kammar-Garcia, A.; Vargas-Vazquez, A.; Gonzalez-Diaz, A.; Fermin-Martinez, C.A.; Marquez-Salinas, A.; Guerra, E.C.; et al. Comprehensive Evaluation of the Impact of Sociodemographic Inequalities on Adverse Outcomes and Excess Mortality During the Coronavirus Disease 2019 (COVID-19) Pandemic in Mexico City. Clin. Infect. Dis. 2022, 74, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Raymundo, C.E.; Oliveira, M.C.; Eleuterio, T.D.; Andre, S.R.; da Silva, M.G.; Queiroz, E.R.D.; Medronho, R.D. Spatial analysis of COVID-19 incidence and the sociodemographic context in Brazil. PLoS ONE 2021, 16, e0247794. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, R.J.; Buttell, F.; Cannon, C. COVID-19: Immediate Predictors of Individual Resilience. Sustainability 2020, 12, 6495. [Google Scholar] [CrossRef]
- Fletcher, K.M.; Espey, J.; Grossman, M.K.; Sharpe, J.D.; Curriero, F.C.; Wilt, D.E.; Sunshine, G.; Moreland, A.; Howard-Williams, M.; Ramos, J.G.; et al. Social vulnerability and county stay-at-home behavior during COVID-19 stay-at-home orders, United States, April 7-April 20, 2020. Ann. Epidemiol. 2021, 64, 76–82. [Google Scholar] [CrossRef]
- Karacsonyi, D.; Dyrting, S.; Taylor, A. A spatial interpretation of Australia’s COVID-vulnerability. Int. J. Disaster Risk Reduct. 2021, 61, 102299. [Google Scholar] [CrossRef]
- Fatmawati; Dewantara, J.A. Social resilience of indigenous community on the border: Belief and confidence in anticipating the spread of COVID-19 through the Besamsam custom in the Dayak community. J. Community Appl. Soc. Psychol. 2022, 1–18. [Google Scholar] [CrossRef]
- Popa, N.; Pop, A.M.; Marian-Potra, A.C.; Cocean, P.; Hognogi, G.G.; David, N.A. The Impact of the COVID-19 Pandemic on Independent Creative Activities in Two Large Cities in Romania. Int. J. Environ. Res. Public Health 2021, 18, 7674. [Google Scholar] [CrossRef]
- Minguez Garcia, B. Integrating culture in post-crisis urban recovery: Reflections on the power of cultural heritage to deal with crisis. Int. J. Disaster Risk Reduct. 2021, 60, 102277. [Google Scholar] [CrossRef]
- Valizadeh, N.; Ghazani, E.; Akbari, M.; Shekarkhah, J. How Do Collective Efficiency and Norms Influence the Social Resilience of Iranian Villagers Against the COVID-19? The Mediating Role of Social Leadership. Front. Public Health 2022, 10, 861325. [Google Scholar] [CrossRef] [PubMed]
- Duarte, R.; Aguiar, A.; Pinto, M.; Furtado, I.; Tiberi, S.; Lonnroth, K.; Migliori, G.B. Different disease, same challenges: Social determinants of tuberculosis and COVID-19. Pulmonology 2021, 27, 338–344. [Google Scholar] [CrossRef]
- Haas, E.J.; Furek, A.; Casey, M.; Yoon, K.N.; Moore, S.M. Applying the Social Vulnerability Index as a Leading Indicator to Protect Fire-Based Emergency Medical Service Responders’ Health. Int. J. Environ. Res. Public Health 2021, 18, 8049. [Google Scholar] [CrossRef]
- Mont, O.; Curtis, S.K.; Voytenko Palgan, Y. Organisational Response Strategies to COVID-19 in the Sharing Economy. Sustain. Prod. Consum. 2021, 28, 52–70. [Google Scholar] [CrossRef] [PubMed]
- Douglas, M.; Katikireddi, S.V.; Taulbut, M.; McKee, M.; McCartney, G. Mitigating the wider health effects of COVID-19 pandemic response. BMJ Br. Med. J. 2020, 369, m1557. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.Y.; Zhai, W. Examining the spatial and temporal relationship between social vulnerability and stay-at-home behaviors in New York City during the COVID-19 pandemic. Sustain. Cities Soc. 2021, 67, 102757. [Google Scholar] [CrossRef]
- Ulimwengu, J.; Kibonge, A. Spatial spillover and COVID-19 spread in the US. BMC Public Health 2021, 21, 1765. [Google Scholar] [CrossRef]
- Xiong, J.Q.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Chen, Y.; Su, X.Y.; Zhou, Q. Study on the Spatiotemporal Evolution and Influencing Factors of Urban Resilience in the Yellow River Basin. Int. J. Environ. Res. Public Health 2021, 18, 10231. [Google Scholar] [CrossRef]
- Kang, J.Y.; Michels, A.; Lyu, F.Z.; Wang, S.H.; Agbodo, N.; Freeman, V.L.; Wang, S.W. Rapidly measuring spatial accessibility of COVID-19 healthcare resources: A case study of Illinois, USA. Int. J. Health Geogr. 2020, 19, 1–17. [Google Scholar] [CrossRef]
- Mofleh, D.; Almohamad, M.; Osaghae, I.; Bempah, S.; Zhang, Q.Z.; Tortolero, G.; Ebeidat, A.; Ramphul, R.; Sharma, S.V. Spatial Patterns of COVID-19 Vaccination Coverage by Social Vulnerability Index and Designated COVID-19 Vaccine Sites in Texas. Vaccines 2022, 10, 574. [Google Scholar] [CrossRef] [PubMed]
- Gharpure, R.; Yi, S.H.; Li, R.R.; Slifka, K.M.J.; Tippins, A.; Jaffe, A.; Guo, A.; Kent, A.G.; Gouin, K.A.; Whitworth, J.C.; et al. COVID-19 Vaccine Uptake Among Residents and Staff Members of Assisted Living and Residential Care Communities-Pharmacy Partnership for Long-Term Care Program, December 2020–April 2021. J. Am. Med. Dir. Assoc. 2021, 22, 2016–2020. [Google Scholar] [CrossRef]
- Sohn, H.; Aqua, J.K. Geographic variation in COVID-19 vulnerability by legal immigration status in California: A prepandemic cross-sectional study. BMJ Open 2022, 12, e054331. [Google Scholar] [CrossRef]
- Blukacz, A.; Cabieses, B.; Mezones-Holguin, E.; Arias, J.M.C. Healthcare and social needs of international migrants during the COVID-19 pandemic in Latin America: Analysis of the Chilean case. Glob. Health Promot. 2022, 17579759211067562. [Google Scholar] [CrossRef] [PubMed]
- Mouliou, D.S.; Kotsiou, O.S.; Gourgoulianis, K.I. Estimates of COVID-19 Risk Factors among Social Strata and Predictors for a Vulnerability to the Infection. Int. J. Environ. Res. Public Health 2021, 18, 8701. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Fischer, H.; Shrestha, S.; Ali, S.S.; Chhatre, A.; Devkota, K.; Fleischman, F.; Khatri, D.B.; Rana, P. Dark and bright spots in the shadow of the pandemic: Rural livelihoods, social vulnerability, and local governance in India and Nepal. World Dev. 2021, 141, 105370. [Google Scholar] [CrossRef]
- Zhang, F.X. The community resilience measurement throughout the COVID-19 pandemic and beyond -an empirical study based on data from Shanghai, Wuhan and Chengdu. Int. J. Disaster Risk Reduct. 2022, 67, 102664. [Google Scholar] [CrossRef]
- Thomas, D.S.K.; Jang, S.; Scandlyn, J. The CHASMS conceptual model of cascading disasters and social vulnerability: The COVID-19 case example. Int. J. Disaster Risk Reduct. 2020, 51, 101828. [Google Scholar] [CrossRef] [PubMed]
- Saghapour, T.; Giles-Corti, B.; Jafari, A.; Qaisrani, M.A.; Turrell, G. Supporting pandemic disease preparedness: Development of a composite index of area vulnerability. Health Place 2021, 70, 102629. [Google Scholar] [CrossRef]
- Wang, H.; Xu, R.; Qu, S.J.; Schwatz, M.; Adams, A.; Chen, X. Health inequities in COVID-19 vaccination among the elderly: Case of Connecticut. J. Infect. Public Health 2021, 14, 1563–1565. [Google Scholar] [CrossRef]
- Khairat, S.; Zou, B.M.; Adler-Milstein, J. Factors and reasons associated with low COVID-19 vaccine uptake among highly hesitant communities in the US. Am. J. Infect. Control 2022, 50, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Lewis, B.; Berney, K.; Hallisey, E.; Williams, A.M.; Whiteman, A.; Rivera-Gonzalez, L.O.; Clarke, K.E.N.; Clayton, H.B.; Tincher, T.; et al. Social Vulnerability and Rurality Associated With Higher Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection-Induced Seroprevalence: A Nationwide Blood Donor Study-United States, July 2020–June 2021. Clin. Infect. Dis. 2022. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.L.; Zhu, H.; Xue, P.D.; Hu, X.; Guo, X.T.; Liu, B.S. Eye-tracking study of public acceptance of 5G base stations in the context of the COVID-19 pandemic. Eng. Constr. Archit. Manag. 2022. [Google Scholar] [CrossRef]
- Wieringa, S.; Neves, A.L.; Rushforth, A.; Ladds, E.; Husain, L.; Finlay, T.; Pope, C.; Greenhalgh, T. Safety implications of remote assessments for suspected COVID-19: Qualitative study in UK primary care. BMJ Qual. Saf. 2022. [Google Scholar] [CrossRef] [PubMed]
- Islam, N.; Lacey, B.; Shabnam, S.; Erzurumluoglu, A.M.; Dambha-Miller, H.; Chowell, G.; Kawachi, I.; Marmot, M. Social inequality and the syndemic of chronic disease and COVID-19: County-level analysis in the USA. J. Epidemiol. Community Health 2021, 75, 496–500. [Google Scholar] [CrossRef]
- Galacho-Jimenez, F.B.; Carrunan-Herrera, D.; Molina, J.; Ruiz-Sinoga, J.D. Evidence of the Relationship between Social Vulnerability and the Spread of COVID-19 in Urban Spaces. Int. J. Environ. Res. Public Health 2022, 19, 5336. [Google Scholar] [CrossRef]
- Gaynor, T.S.; Wilson, M.E. Social Vulnerability and Equity: The Disproportionate Impact of COVID-19. Public Adm. Rev. 2020, 80, 832–838. [Google Scholar] [CrossRef]
- Prodanuk, M.; Wagner, S.; Orkin, J.; Noone, D. Social vulnerability and COVID-19: A call to action for paediatric clinicians Comment. Paediatr. Child Health 2021, 26, 1–3. [Google Scholar] [CrossRef]
- Tummalapalli, S.L.; Silberzweig, J.; Cukor, D.; Lin, J.T.; Barbar, T.; Liu, Y.; Kim, K.; Parker, T.S.; Levine, D.M.; Ibrahim, S.A. Racial and Neighborhood-Level Disparities in COVID-19 Incidence among Patients on Hemodialysis in New York City. J. Am. Soc. Nephrol. 2021, 32, 2048–2056. [Google Scholar] [CrossRef]
- Akter, S.; Dhar, T.K.; Rahman, A.I.A.; Uddin, M.K. Investigating the resilience of refugee camps to COVID-19: A case of Rohingya settlements in Bangladesh. J. Migr. Health 2021, 4, 100052. [Google Scholar] [CrossRef]
- Martin-Sanchez, F.J.; Carbo, A.V.; Miro, O.; Llorens, P.; Jimenez, S.; Pinera, P.; Burillo-Putze, G.; Martin, A.; Garcia-Lamberechts, J.E.; Jacob, J. Socio-Demographic Health Determinants Are Associated with Poor Prognosis in Spanish Patients Hospitalized with COVID-19. J. Gen. Intern. Med. 2021, 36, 3737–3742. [Google Scholar] [CrossRef] [PubMed]
- Oates, G.R.; Juarez, L.D.; Horswell, R.; Chu, S.; Miele, L.; Fouad, M.N.; Curry, W.A.; Fort, D.; Hillegass, W.B.; Danos, D.M. The Association Between Neighborhood Social Vulnerability and COVID-19 Testing, Positivity, and Incidence in Alabama and Louisiana. J. Community Health 2021, 46, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- De Souza, C.D.F.; Machado, M.F.; do Carmo, R.F. Human development, social vulnerability and COVID-19 in Brazil: A study of the social determinants of health. Infect. Dis. Poverty 2020, 9, 50. [Google Scholar] [CrossRef]
- Karaye, I.M.; Horney, J.A. The Impact of Social Vulnerability on COVID-19 in the US: An Analysis of Spatially Varying Relationships. Am. J. Prev. Med. 2020, 59, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.Y.; Liao, L.; Li, H.; Su, Z.H. Which urban communities are susceptible to COVID-19? An empirical study through the lens of community resilience. BMC Public Health 2022, 22, 70. [Google Scholar] [CrossRef] [PubMed]
- Falkenhain, M.; Flick, U.; Hirseland, A.; Naji, S.; Seidelsohn, K.; Verlage, T. Setback in labour market integration due to the Covid-19 crisis? An explorative insight on forced migrants’ vulnerability in Germany. Eur. Soc. 2021, 23, S448–S463. [Google Scholar] [CrossRef]
- Troppy, S.; Wilt, G.E.; Whiteman, A.; Hallisey, E.; Crockett, M.; Sharpe, J.D.; Haney, G.; Cranston, K.; Klevens, R.M. Geographic Associations Between Social Factors and SARS-CoV-2 Testing Early in the COVID-19 Pandemic, February–June 2020, Massachusetts. Public Health Rep. 2021, 136, 765–773. [Google Scholar] [CrossRef]
- Neelon, B.; Mutiso, F.; Mueller, N.T.; Pearce, J.L.; Benjamin-Neelon, S.E. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. PLoS ONE 2021, 16, e0248702. [Google Scholar] [CrossRef]
- Coelho, F.C.; Lana, R.M.; Cruz, O.G.; Villela, D.A.M.; Bastos, L.S.; Piontti, A.P.Y.; Davis, J.T.; Vespignani, A.; Codeco, C.T.; Gomes, M.F.C. Assessing the spread of COVID-19 in Brazil: Mobility, morbidity and social vulnerability. PLoS ONE 2020, 15, e0238214. [Google Scholar] [CrossRef]
- Karmakar, M.; Lantz, P.M.; Tipirneni, R. Association of Social and Demographic Factors With COVID-19 Incidence and Death Rates in the US. JAMA Netw. Open 2021, 4, e2036462. [Google Scholar] [CrossRef]
- Park, Y.M.; Kearney, G.D.; Wall, B.; Jones, K.; Howard, R.J.; Hylock, R.H. COVID-19 Deaths in the United States: Shifts in Hot Spots over the Three Phases of the Pandemic and the Spatiotemporally Varying Impact of Pandemic Vulnerability. Int. J. Environ. Res. Public Health 2021, 18, 8987. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.L.; Derakhshan, S.; Blackwood, L.; Lee, L.; Huang, Q.; Habets, M.; Cutter, S.L. Spatial Disparities of COVID-19 Cases and Fatalities in United States Counties. Int. J. Environ. Res. Public Health 2021, 18, 8259. [Google Scholar] [CrossRef] [PubMed]
- Baggio, J.A.O.; Machado, M.F.; do Carmo, R.F.; Armstrong, A.D.; dos Santos, A.D.; de Souza, C.D.F. COVID-19 in Brazil: Spatial risk, social vulnerability, human development, clinical manifestations and predictors of mortality—A retrospective study with data from 59 695 individuals. Epidemiol. Infect. 2021, 149, e100. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.P.; Ravi, N.; Braneon, C.V. Spatiotemporal Associations Between Social Vulnerability, Environmental Measurements, and COVID-19 in the Conterminous United States. Geohealth 2021, 5, e2021GH000423. [Google Scholar] [CrossRef]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. How bad is it? Suicidality in the middle of the COVID-19 pandemic. Suicide Life Threat. Behav. 2020, 50, 1241–1249. [Google Scholar] [CrossRef]
- Syed, A.A.; Gupta, S.; Rai, D. Psychological, social and economic impact of COVID 19 on the working population of India: Exploratory factor analysis approach. Int. J. Disaster Risk Reduct. 2021, 66, 102617. [Google Scholar] [CrossRef]
- Krings, V.C.; Steeden, B.; Abrams, D.; Hogg, M.A. Social attitudes and behavior in the COVID-19 pandemic: Evidence and prospects from research on group processes and intergroup relations. Group Process. Intergroup Relat. 2021, 24, 195–200. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Kjaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Bin Kashem, S.; Baker, D.M.; Gonzalez, S.R.; Lee, C.A. Exploring the nexus between social vulnerability, built environment, and the prevalence of COVID-19: A case study of Chicago. Sustain. Cities Soc. 2021, 75, 103261. [Google Scholar] [CrossRef]
- Martins, P.R.; Quintans-Junior, L.J.; Araujo, A.A.D.; Sposato, K.B.; Tavares, C.S.S.; Gurgel, R.Q.; Leite, D.C.F.; de Paiva, S.M.; Santos, H.P.; Santos, V.S. Socio-economic inequalities and COVID-19 incidence and mortality in Brazilian children: A nationwide register-based study. Public Health 2021, 190, 4–6. [Google Scholar] [CrossRef]
- Alizadeh, H.; Sharifi, A. Analysis of the state of social resilience among different socio-demographic groups during the COVID- 19 pandemic. Int. J. Disaster Risk Reduct. 2021, 64, 102514. [Google Scholar] [CrossRef]
- Castro, R.R.; Santos, R.S.C.; Sousa, G.J.B.; Pinheiro, Y.T.; Martins, R.R.I.M.; Pereira, M.L.D.; Silva, R.A.R. Spatial dynamics of the COVID-19 pandemic in Brazil. Epidemiol. Infect. 2021, 149, e60. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Huang, X.; Li, D.Y.; Xu, Y. Aggravated social segregation during the COVID-19 pandemic: Evidence from crowdsourced mobility data in twelve most populated US metropolitan areas. Sustain. Cities Soc. 2022, 81, 103869. [Google Scholar] [CrossRef]
- Fraser, T.; Aldrich, D.P. The dual effect of social ties on COVID-19 spread in Japan. Sci. Rep. 2021, 11, 1596. [Google Scholar] [CrossRef] [PubMed]
- Fraser, T.; Page-Tan, C.; Aldrich, D.P. Social capital’s impact on COVID-19 outcomes at local levels. Sci. Rep. 2022, 12, 6566. [Google Scholar] [CrossRef]
- Tipirneni, R.; Karmakar, M.; O’Malley, M.; Prescott, H.C.; Chopra, V. Contribution of Individual- and Neighborhood-Level Social, Demographic, and Health Factors to COVID-19 Hospitalization Outcomes. Ann. Intern. Med. 2022, 175, 505–512. [Google Scholar] [CrossRef]

| Related Policies | Effects (Positive +/Negative −) | Citation |
|---|---|---|
| Social Distancing Policy | (+) Internal regulatory policy restrictions at the national level have inhibited the spread of COVID-19. | [39] |
| Mitigation Actions | (+) Mitigation policies can effectively control the spread of the epidemic | [40] |
| National Prevention Policies | (+) Policies (masks, home orders, congregation restrictions, social distance) had a significantly lower average mortality rate for low resilience communities. | [41] |
| (+) Good political communication helps to improve political messages and thus social resilience. | [42] | |
| COVID-19 policies applied to disabled people | (−) Policy responses should focus on social resilience and disabling barriers that force disabled people into states of vulnerability. | [43] |
| COVID-19 vaccination | (−) Vaccination resources are allocated with attention to community-level adaptation to ensure rationalization of vaccine supply. | [44] |
| Urban medical allocation policy | (−) Government action has resulted in an uneven distribution of the quality impact of access to the COVID-19 due to social inequalities at the individual and municipal levels. | [45] |
| Non-pharmacological intervention policies | (−) Many of these measures are not feasible for people living in socially maladjusted areas. | [46] |
| Stay-at-home | (−) Difficulties in complying with policies during “stay-at-home” periods are associated with less social resilience, maintaining it for a long time will have a negative impact on the psychology of the public. | [47,48] |
| The lockdowns | (−) COVID-19 exposed Australia’s systemic, demographic, and spatial vulnerabilities, while embargo policies led to reduced economic resilience. | [49] |
| Influencing Factors and Percentage | Main Conclusions | Citation |
|---|---|---|
| Vulnerable Groups (33%) | Vulnerable groups as a key factor affecting social resilience during COVID-19 Patients living in resource-poor areas, especially among the elderly, children, minorities, homeless, and disadvantaged groups without transportation, expose public management practices and structures to higher rates of morbidity and mortality Middle-class and even affluent areas that lack the space, capital, and governance resilience can become “vulnerable” to COVID-19 Social resilience changes when refugees integrate into a new social system, and trauma-tized refugees are at increased risk of COVID-19 infection due to severe distrust and dis-respect for aid agencies, in addition to inadequate building infrastructure and unsanitary living conditions | [79,80,81,82,83,84,85,86,87,88] |
| Spatial Heterogeneity (27%) | Spatial heterogeneity of social resilience indicators (lower social resilience and lack of policies) was highly correlated with the spread of COVID-19 Socioeconomic status, racial/minority status, family composition, and environmental fac-tors are associated with COVID-19 morbidity and mortality Hot spots range from states with high percentages of densely populated and socially vul-nerable populations, to states with lax policy requirements and states with low vaccina-tion rates The impact of COVID-19 is dynamic, spreading first to large urban centers and more de-veloped cities, then to smaller and less developed cities, and then shifting back again | [89,90,91,92,93,94,95,96] |
| Social Psychological (13%) | The spread of COVID-19 has a negative psychological impact on people and seriously af-fects social resilience Female groups are more vulnerable to psychosocial and organizational pressures due to the economic and employment problems during the pandemic Social psychology is central to helping us understand the impact and resolution of COVID-19 on social attitudes and behaviors | [97,98,99,100] |
| Socioeconomic (13%) | Socioeconomic factors are strong predictors of COVID-19 outcomes, with housing density, the Municipal Human Development Index (MHDI) and SVI being the most influential fac-tors, and class segregation being a greater threat to the social and economic resilience Socioeconomic inequalities contribute to disparities in the COVID-19 population, espe-cially among children Cities in developing countries have weak social resilience due to lack of adequate facilities | [101,102,103,104] |
| Social Ties (7%) | Resilient communities have much lower case-fatality rates of COVID-19, and the most- and least-resilient groups in the community are prone to interact with communities similar to theirs, with increased mortality once the disease invades | [105,106] |
| Social Capital (3%) | Social capital helps residents adopt new behavioral norms | [107] |
| Social Assistance (4%) | Patients with poor social resilience were sicker, but with no difference in mortality or discharge disposition after hospital admission | [108] |
| Levels | Dimensions | Indicators | Explanations |
|---|---|---|---|
| Intervention Angle | Hard strength | Development Capacity | Social development adjustments affected by COVID-19 |
| Capital | The current economic state, ensuring redundancy in the economic aspects of resilience | ||
| Policy Strength | Scope of policy enactment and effectiveness of governance | ||
| Regulatory Capability | The extent to which policy regulates and can intervene | ||
| Infrastructure Status | State and distribution of the social own infrastructure | ||
| Medical Coverage | Social paramedical aid available | ||
| Vaccinations | Vaccination status and distribution | ||
| Soft Power | Public Assistance | Distribution of community benefit organizations and other service categories | |
| Neighborhood | The degree of harmony and organization among neighbors | ||
| Trust Level | The degree of trust citizens has in a policy reflects the degree of willingness to implement it | ||
| Cultural Resonance | Some positive customs that have a cohesive effect | ||
| Security and Equity | Equitable and secure human survival | ||
| Internal Regulation | Natural Conditions | Natural Conditions | The physical geography in which the community itself is located |
| Human conditions | Living Systems | The impact of the social labor production and living conditions | |
| Education level | Percentage of population with educational attainment | ||
| Population Density | The average number of people on a certain unit of land at a certain time | ||
| Percentage of vulnerable Groups | Percentage of vulnerable groups as a whole | ||
| Diseases | Whether the individual has been ill during the epidemic and whether he or she has had other prior medical conditions such as chronic diseases | ||
| Language Communication | A person’s language situation and ability to communicate properly with that community | ||
| Mental state | Psychological situation of individuals during COVID-19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cui, P.; Dong, Z.; Yao, X.; Cao, Y.; Sun, Y.; Feng, L. What Makes Urban Communities More Resilient to COVID-19? A Systematic Review of Current Evidence. Int. J. Environ. Res. Public Health 2022, 19, 10532. https://doi.org/10.3390/ijerph191710532
Cui P, Dong Z, Yao X, Cao Y, Sun Y, Feng L. What Makes Urban Communities More Resilient to COVID-19? A Systematic Review of Current Evidence. International Journal of Environmental Research and Public Health. 2022; 19(17):10532. https://doi.org/10.3390/ijerph191710532
Chicago/Turabian StyleCui, Peng, Zhiyu Dong, Xin Yao, Yifei Cao, Yifan Sun, and Lan Feng. 2022. "What Makes Urban Communities More Resilient to COVID-19? A Systematic Review of Current Evidence" International Journal of Environmental Research and Public Health 19, no. 17: 10532. https://doi.org/10.3390/ijerph191710532
APA StyleCui, P., Dong, Z., Yao, X., Cao, Y., Sun, Y., & Feng, L. (2022). What Makes Urban Communities More Resilient to COVID-19? A Systematic Review of Current Evidence. International Journal of Environmental Research and Public Health, 19(17), 10532. https://doi.org/10.3390/ijerph191710532







