1. Introduction
In low- and middle-income countries (LMICs), formal emergency medical services (EMSs) rarely exist and, when present, are often hampered by structural inefficiencies, such as poor transportation and infrastructure, the shortage of skilled medical staff and resources, and a lack of comprehensive referral protocols [
1,
2]. To address the transportation gap, many nongovernmental organisations (NGOs) working in LMICs have implemented EMSs at the local or regional level using different means of transport, including even motorbike and bicycle ambulances [
3,
4,
5]. Nonetheless, the absence of well-established protocols for patient transfer frequently leads to the inappropriate transport of uncomplicated cases to referral hospitals, overwhelming their personnel and impacting already scarce available resources [
6,
7]. In this scenario, the implementation of patient prioritisation strategies is pivotal in managing the challenges associated with the existing mismatch between the demand for emergency care and the available resources, thus avoiding the inappropriate use of national referral hospitals and all the consequences associated with it. While prehospital triage criteria for patient transport are frequently adopted in upper-middle- and high-income countries [
8], there is a lack of the scientific literature on the implementation of triage systems in LMICs’ prehospital settings, and no consensus on which triage tool works better in these contexts exists [
9,
10]. More broadly, only recently have LMICs started incorporating triage tools into emergency department practice by either adapting existing protocols or implementing new tools such as the South African Triage Scale (SATS) [
11,
12,
13].
SATS, a triage protocol expressly designed for LMICs, is a four-level triage algorithm based on a list of emergency conditions and on the evaluation of seven different vital signs (mobility, respiratory rate, heart rate, systolic blood pressure, temperature, neurologic status, and history of trauma). Using three different tables (for adults, younger, and older children) containing reference values, the so-called Triage Early Warning Score (TEWS) is calculated. Patients who present one of the predetermined emergency conditions listed in the SATS protocol (obstructed airway, facial burns and inhalation, severe hypoglycaemia, and cardiac arrest) are immediately classified within the maximal priority category (red), while others have codes assigned according to the TEWS [
11]. The use of objective vital-sign data renders the SATS a robust, simple, and rapid tool to be taught to inexperienced staff [
14,
15]. While the use of SATS has been extensively validated in different emergency departments located in resource-constrained settings, effectively reducing patient waiting time, hospital length of stay, and mortality [
15,
16,
17,
18,
19,
20,
21], its performance in the prehospital field and in the assessment of nontrauma cases has not been thoroughly evaluated. Indeed, the formal assessment of the SATS utilisation by prehospital providers has been performed only through indirect methodologies, such as written clinical vignettes or focus-group discussions [
22,
23,
24].
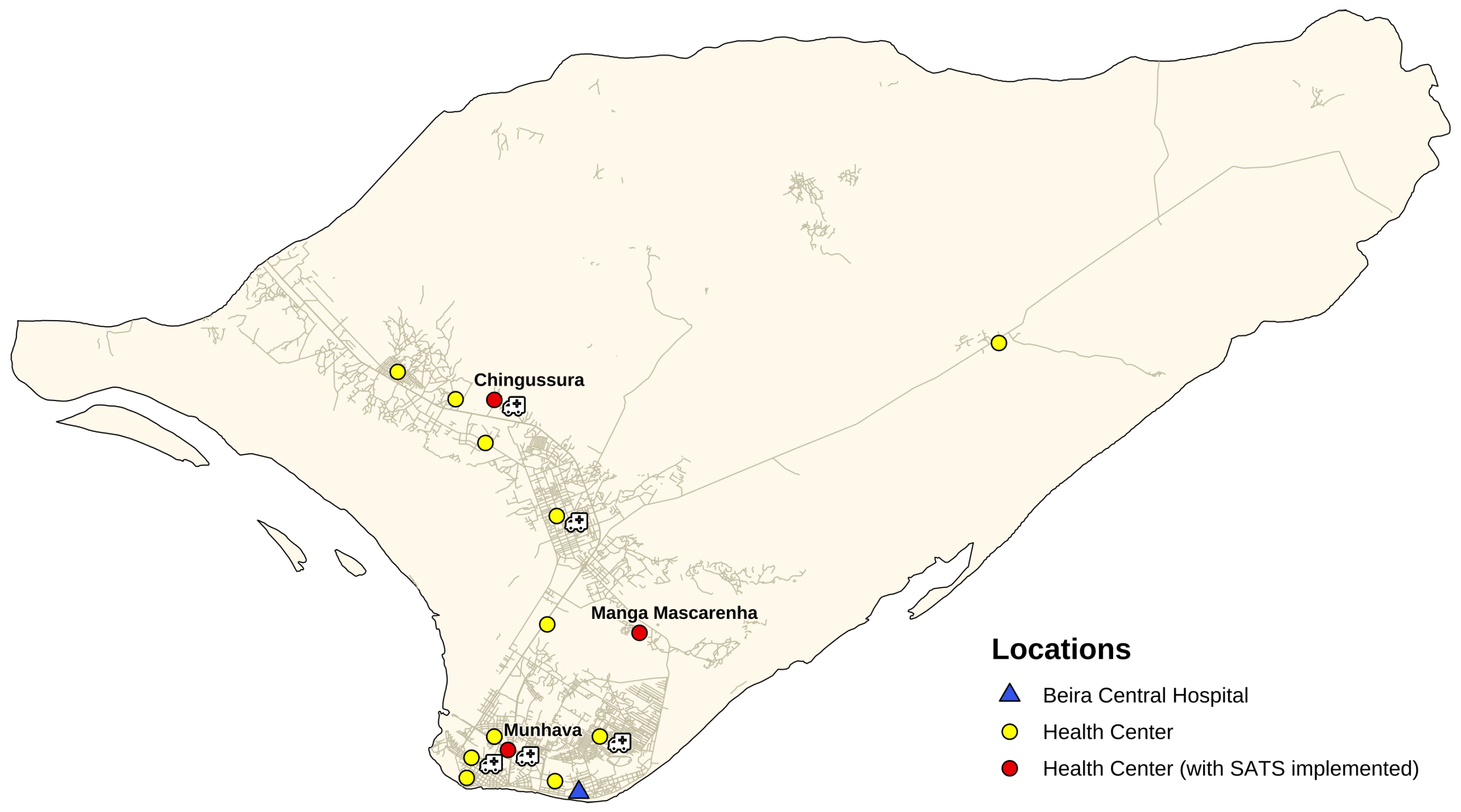
SATS has been recently integrated in the urban ambulance system of Beira, the second largest city of Mozambique with more than 530,000 inhabitants. The ambulance system was established immediately after the 2019 Cyclone Idai by NGO doctors with Africa CUAMM (Padova, Italy) in collaboration with the Centre for Research and Training in Disaster Medicine, Humanitarian Aid, and Global Health (CRIMEDIM, Università del Piemonte Orientale, Novara, Italy), with the aim of reducing hospital care referral time. The 24/7 free-of-charge referral service started its activities on 1 June 2019, linking Beira Central Hospital (HCB) with 15 peripheral health centres (HCs) through a fleet of five ambulances stationed in five different HCs, selected according to their geographical position and to the number of patients treated per day (
Figure 1).
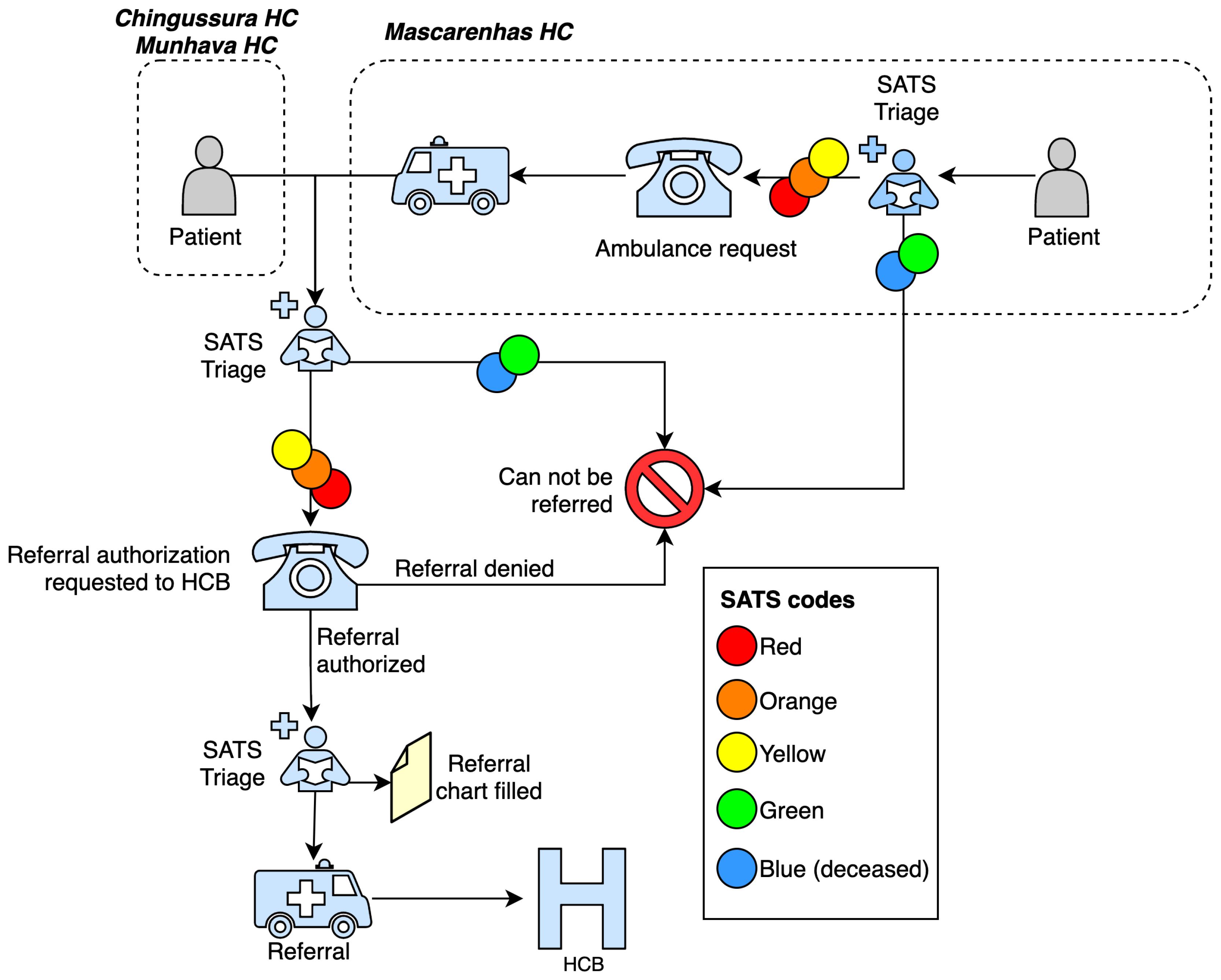
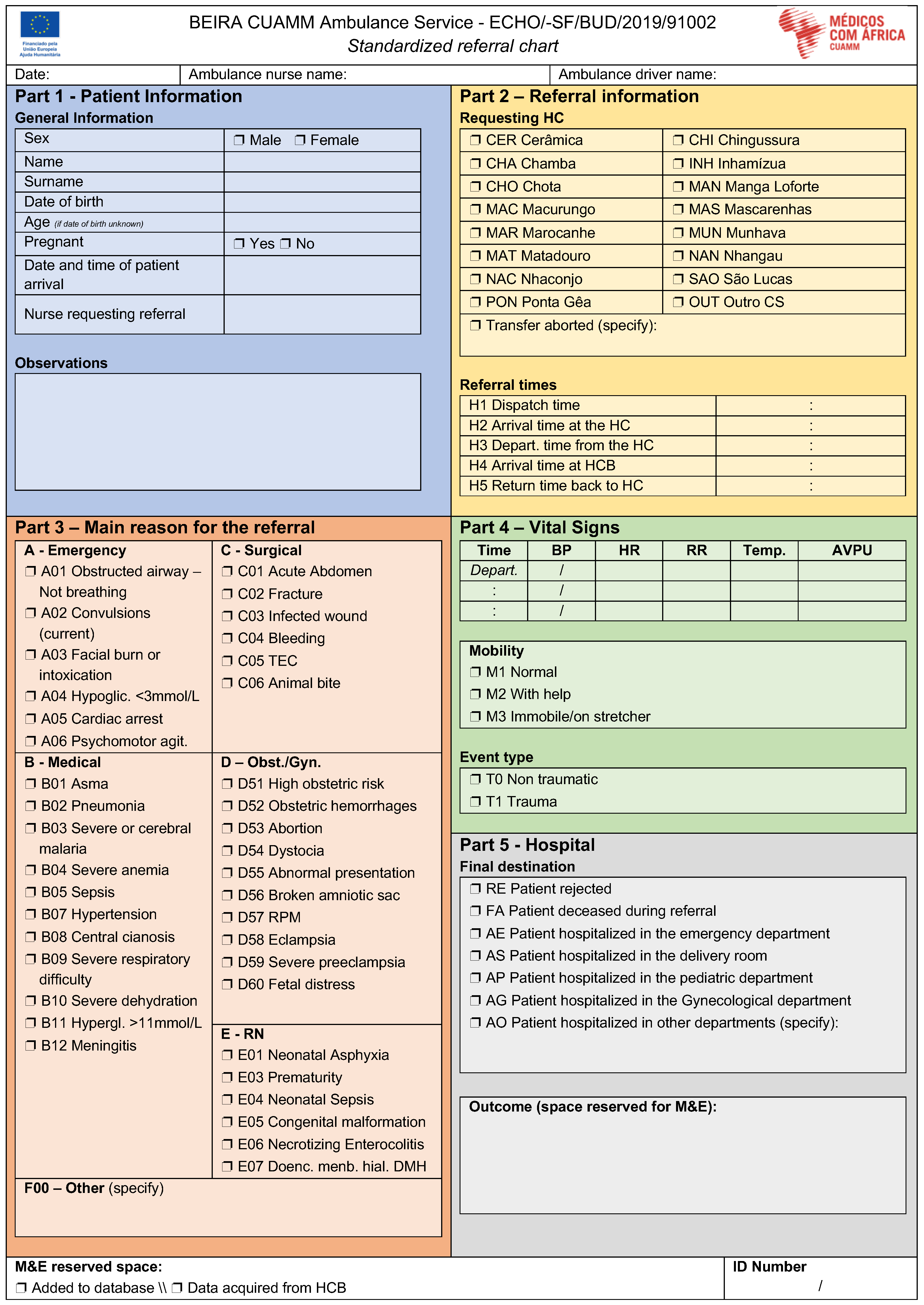
Upon its inception, the service did not contemplate a standardised prioritisation protocol for patient referral, but rather followed a first-in–first-out approach, thus often leading to a saturation of the service’s referral capacity. Therefore, SATS has been incorporated to improve referrals and regulate the number of severe cases accessing HCB from the three HCs of Chingussura, Munhava, and Manga Mascarenhas. From 27 to 30 November 2019, 75 nurses working in the above-mentioned HCs were trained on the use of SATS, and instructed to refer patients when deemed necessary according to the priority codes. Specifically, nurses underwent a single two-day course (
Table A1) and were instructed to follow a specific protocol for patient transport from the three HCs to HCB (
Figure A1). This is the first example of SATS integration and assessment within the referral protocol of an urban ambulance system in a low-income country. The purpose of this study was to assess whether the implementation of the SATS varied the pattern of acute patients referred from HCs to HCB. In addition, we evaluated the correct use of the SATS performed by nurses in the HCs, defined as the accuracy related to the application of the tool.
3. Results
During the observation period, a total of 2636 referral charts were collected, and 159 and 317 records (from the pre- and postimplementation phases, respectively) were excluded.
Table 1 summarises the demographic information of the considered patients. Our analysis comprised a total of 552 and 1608 referral charts for the pre- and postimplementation phases, respectively. Referral rate did not change appreciably over time. In both phases, referred patients were mainly women, and most of the referrals regarded obstetric or gynaecological and paediatric complaints (
Table 1).
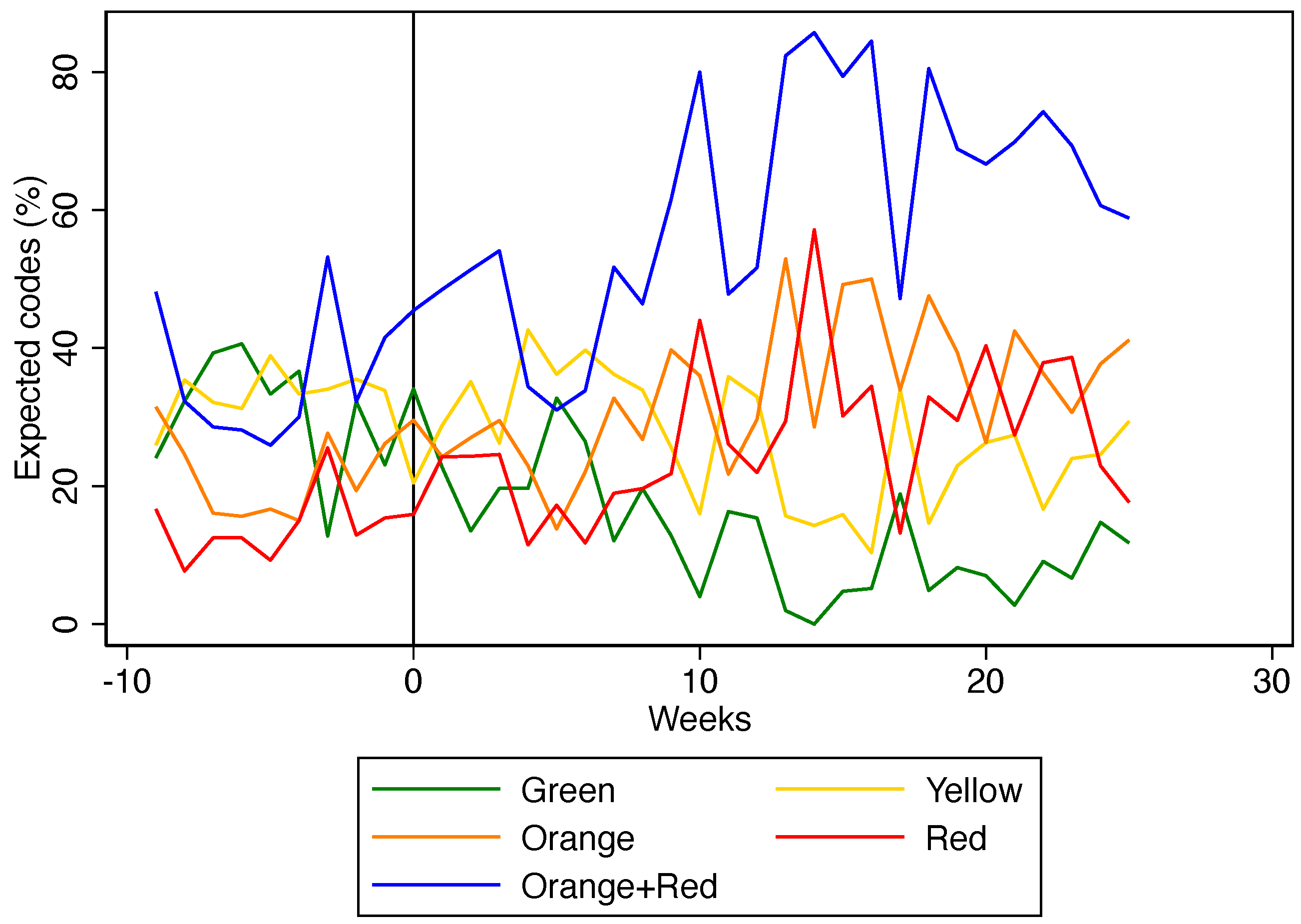
After the implementation of SATS, there was an increase in orange and red codes (+12.2%; +12.9%, respectively), and a reduction in green and yellow codes (−18.7%; −5.8%, respectively) referred to the HCB (
Table 2).
Figure 2 shows how this phenomenon took place gradually and lasted for the whole study period.
Table 3 shows the accuracy of SATS codes assigned by nurses during the postimplementation phase. The overall rate of nurses’ accuracy, and under- and over-triage were 34.2%, 36.3% and 29.5% respectively.
Table A2 and
Table A3 report the accuracy for obstetric or gynaecological and paediatric cases subgroups. The overall inter-rater agreement was 0.25 (95% confidence interval (CI) 0.21–0.29); in obstetric or gynaecological and paediatric cases, it was 0.17 (95% CI 0.10–0.25) and 0.16 (95% CI 0.06–0.25), respectively.
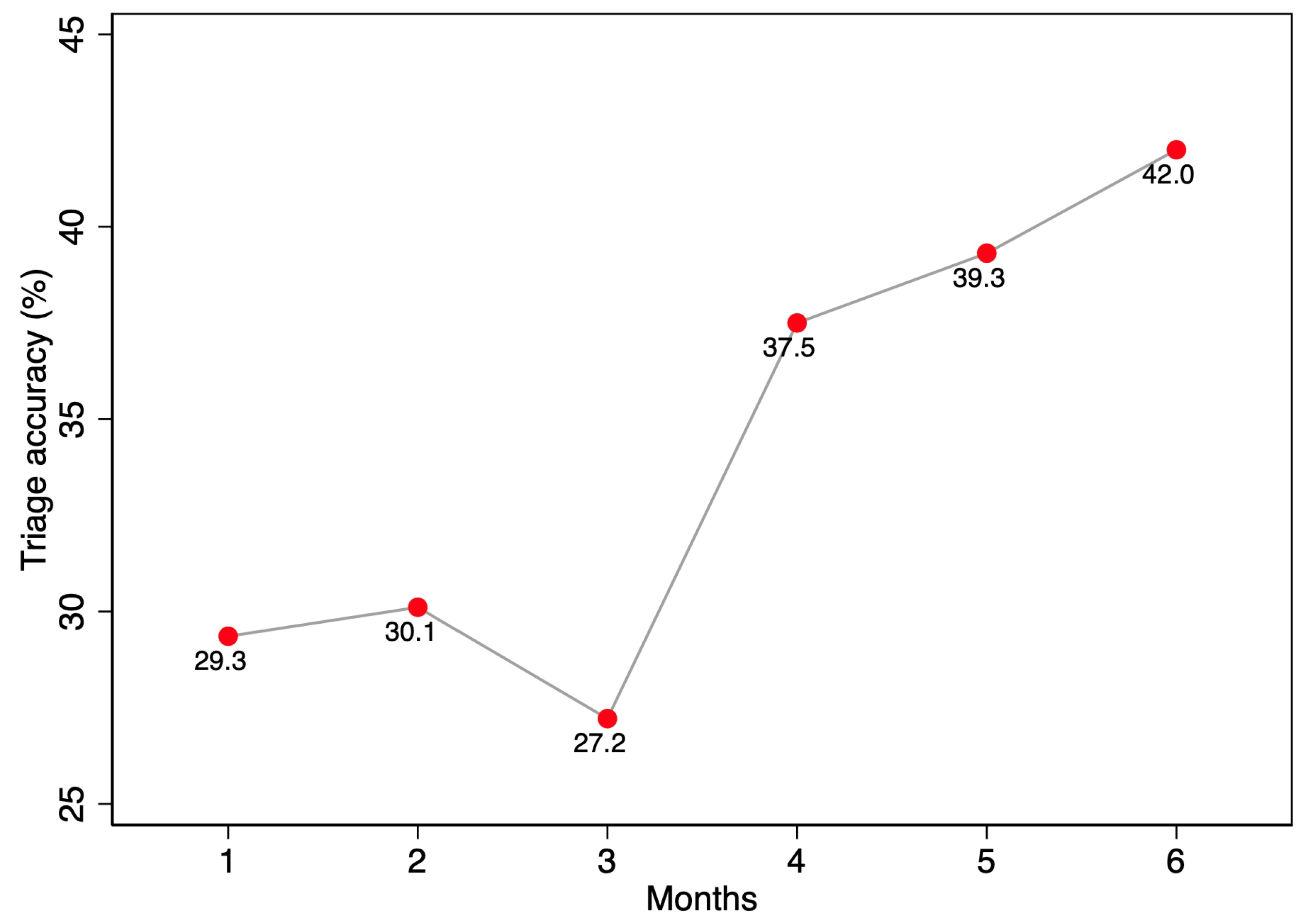
Figure 3 reports the association between time and accuracy, displaying an increasing trend from December 2019 (29.4%) to May 2020 (42.0%). This result was confirmed in the logistic regression, showing a statistically significant association between time since implementation and accuracy in the application of the tool (
p-value < 0.0005). In contrast, the gender and age of patients did not influence nurses’ accuracy in applying the SATS protocol.
4. Discussion
The integration of SATS in the urban ambulance system of Beira modified the pattern of transported patients, improving the selection process and enabling local staff to become acquainted with the notions of triage and referral protocols, concepts that are still uncommon in Mozambique [
23].
The increase in the proportion of severe transported cases followed a continuous progressive trend, suggesting that the concept of patient prioritisation and the SATS protocol might need time to be fully mastered by local professionals. Gradually, the first-in–first-out approach that aimed purely at reducing the pressure on constantly overcrowded HCs was replaced by a more coordinated system that has the utmost goal of addressing the limited resources available in postcyclone Mozambique to the most severe cases, optimising the use of the few ambulances, healthcare staff, and hospital assets [
26]. The daily transport rates were similar before and after the SATS implementation, suggesting that the service worked from the beginning at its maximal capacity, and highlighting the importance of regulating the referral process through a standardised and rational approach.
To the best of our knowledge, this is the first formal assessment of the integration of SATS in the referral protocol of a low-income country. The decision to introduce the SATS to improve the existing referral service stemmed from its proven suitability for a low-resource context, evidenced by its algorithm-based approach, the availability of ready-to-use charts and training manuals, and the inclusion of easy-to-record vital signs [
18,
27,
28].
Nevertheless, the use of SATS in this prehospital setting was associated with high rates of incorrect triage compared to the thresholds of 15% and 10% for over- and undertriage, respectively, which are usually deemed to be acceptable in hospital settings [
24]. Our results are consistent with those of Mould-Millman and colleagues reporting high rates of undertriage among prehospital providers asked to assess clinical vignettes and assign a final SATS triage colour [
24]. The authors suggested that the degree of miscalculation of TEWS, identified as one the most frequent causes of error in assigning the final triage colour could be further exacerbated under stressful real-life circumstances, such as the management of acute patients. The incorrect identification of predetermined emergency conditions and the incorrect selection of clinical discriminators are other common errors reported in the literature [
24,
29].
Furthermore, our analysis focused exclusively on under- and overtriage rates without investigating the root causes behind the decisions by nurses. The low inter-rater agreement and overall high rates of incorrect triage could have been amplified by the specific context. Indeed, the triage process is a complex activity, often performed in a stressful, distracting environment [
30] that can influence the triage code assigned by nurses independently from the intrinsic reliability of the protocol [
31]. This could, at least partially, justify the poorer SATS performance when compared to that in vignette-based studies [
24].
This suggests the need for further studies to better assess the practical limitations for the implementation of SATS in a prehospital setting.
On the other hand, the main aim of the referral protocol implemented in the urban ambulance system of Beira was to avoid the transportation of green codes to HCB. The misclassification of yellow, orange, and red codes did not affect the referral indication. Among the 126 green-code patients erroneously referred to HCB, the vast majority were undertriaged (
Table 3). This could mean that nurses could have recognised the mismatch between the assigned green code and the actual clinical condition, subsequently deciding to refer patients to HCB anyway, a frequent phenomenon already described in the literature [
22,
24,
29]. Despite this procedure being contemplated in the SATS [
32], it could have led to an apparent incorrect triage due to the contrast between recorded clinical parameters and triage codes assigned retrospectively.
Furthermore, the delivered training course might not have been sufficient in terms of content, duration, and teaching methodologies to provide sufficient skills and knowledge to the nurses. On the other hand, the available literature highlights a great heterogeneity among SATS training, thus indicating that no standardisation currently exists; for example, the duration of courses varies from 1-h [
19,
20] to 2-day courses [
21]. In addition, the official SATS training manual [
32] does not provide a suggested duration nor a specific teaching approach.
Moreover, this referral service represents, especially for the vulnerable strata of population, one of the few chances to reach HCB. Subsequently, nurses could have decided to refer patients with specific health needs even if not presenting an urgent condition recognised by SATS. Despite this approach overtaking the initial design and objectives of the referral system, it is very common and could be considered acceptable in the specific low-resource context [
33]. In the same vein, the SATS has been implemented without any specific adaptation. Despite this approach being deemed necessary to provide a reliable and evidence-based tool, it does not take in consideration the specific needs and peculiarities of Beira’s prehospital context.
Hence, whether SATS represents the best available option to regulate acute patients’ referral in the prehospital setting is still under debate. Studies that assess the practical implications, benefits, and limitations of SATS implementation are needed to better understand its use in this context, and whether any adaptation is required to adjust the algorithm according to prehospital and local particularities.
Our findings should be interpreted considering some limitations. First, the study was performed immediately after the introduction of SATS, thus intercepting the learning curve of local nurses, and not investigating the long-term effects of the implementation. In addition, data used for this study were gathered from patients’ referral charts, thus only including information on transported patients. Therefore, we are unaware of the actual number of patients assessed and treated at each HC in the selected timeframe, and we could not estimate the proportion of the different codes assigned to patients who have not been referred to the HCB. Additionally, as available data do not provide the outcome after hospitalisation, we were unable to establish whether the prioritisation of severe cases in the referral system effectively translated into improved health outcomes.