Associations of Central Sensitization-Related Symptoms with Low Back Pain-Related Factors and Work Status in Caregivers
Abstract
:1. Introduction
2. Materials and Methods
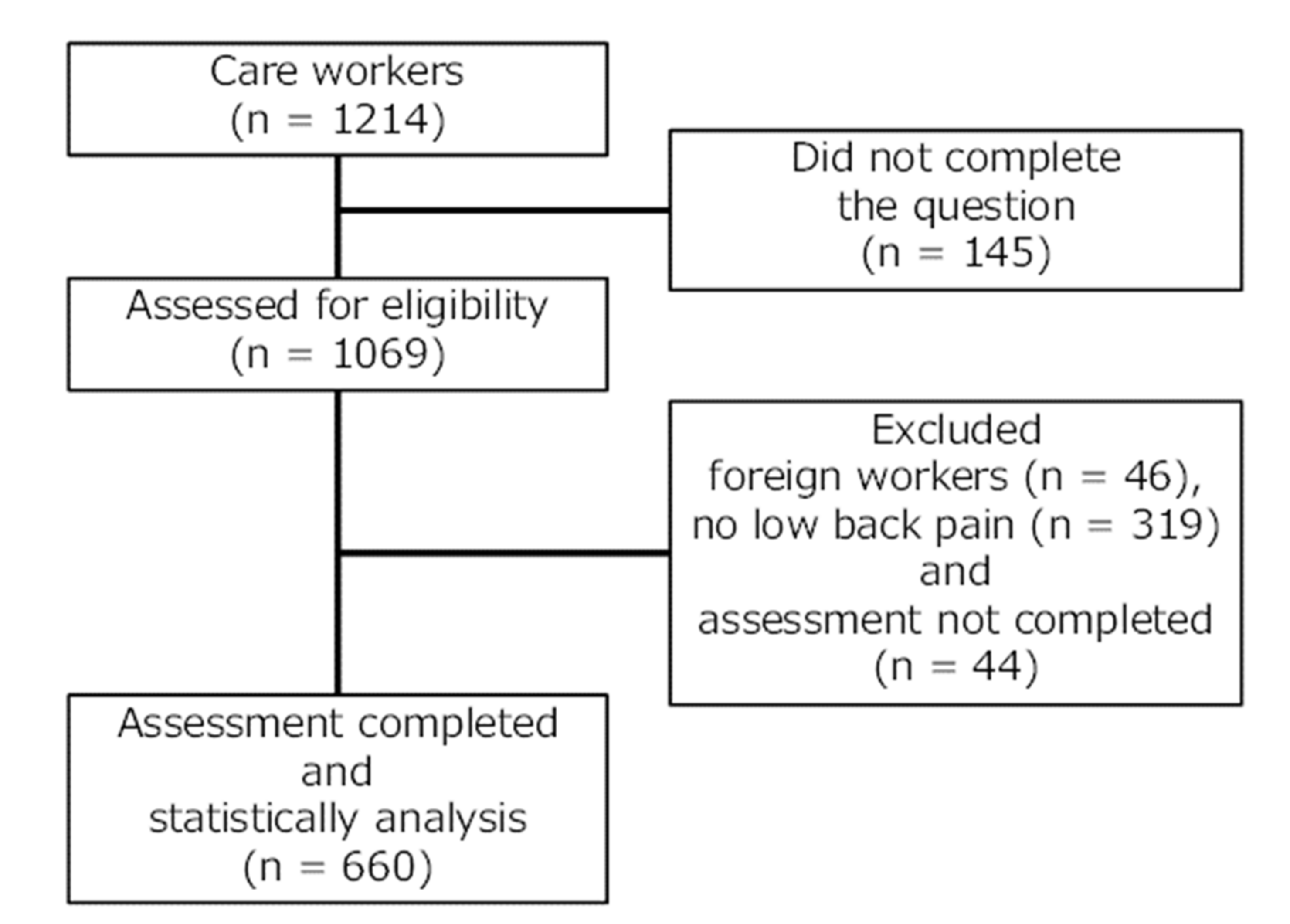
2.1. Participants and Study Design
2.2. Evaluations of the Participants’ Characteristics by Questionnaires
2.3. Statistical Analyses
3. Results
3.1. Participants’ Characteristics
3.2. Comparison of Pain-Related Factors According to CSS Severity Groups
3.3. Comparison of Work Status between CSS Severity Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, E.C.; Burdorf, A.; Kalokerinou, A. A comparative analysis on musculoskeletal disorders between Greek and Dutch nursing personnel. Int. Arch. Occup. Environ. Health 2006, 79, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Clausen, T.; Mortensen, O.S.; Burr, H.; Holtermann, A. A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among health care workers in eldercare. Int. Arch. Occup. Environ. Health 2012, 85, 615–622. [Google Scholar] [CrossRef]
- Faber, A.; Giver, H.; Strøyer, J.; Hannerz, H. Are low back pain and low physical capacity risk indicators for dropout among recently qualified eldercaregivers? A follow-up study. Scand. J. Public Health 2010, 38, 810–816. [Google Scholar] [CrossRef] [PubMed]
- Engkvist, I.L. Evaluation of an intervention comprising a No Lifting Policy in Australian hospitals. Appl. Ergon. 2006, 37, 141–148. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Ferrari, S.; Chiarotto, A.; Pellizzer, M.; Vanti, C.; Monticone, M. Pain Self-Efficacy and Fear of Movement are Similarly Associated with Pain Intensity and Disability in Italian Patients with Chronic Low Back Pain. Pain Pract. 2016, 16, 1040–1047. [Google Scholar] [CrossRef]
- Marshall, P.W.M.; Schabrun, S.; Knox, M.F. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS ONE 2017, 12, e0180788. [Google Scholar] [CrossRef]
- Wertli, M.M.; Eugster, R.; Held, U.; Steurer, J.; Kofmehl, R.; Weiser, S. Catastrophizing-a prognostic factor for outcome in patients with low back pain: A systematic review. Spine J. 2014, 14, 2639–2657. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Oka, H.; Fujii, T.; Kawamata, K.; Kokaze, A.; Koyama, Y.; Matsudaira, K. Survey on chronic disabling low back pain among caregivers at nursing care facilities: A multicenter collaborative cross-sectional study. J. Pain Res. 2019, 12, 1025–1032. [Google Scholar] [CrossRef]
- Kosińska, B.; Tarnacka, B.; Turczyn, P.; Gromadzka, G.; Malec-Milewska, M.; Janikowska-Hołowenko, D.; Neblett, R. Psychometric validation of the Polish version of the Central Sensitization Inventory in subjects with chronic spinal pain. BMC Neurol. 2021, 21, 483. [Google Scholar] [CrossRef] [PubMed]
- Neblett, R.; Hartzell, M.M.; Williams, M.; Bevers, K.R.; Mayer, T.G.; Gatchel, R.J. Use of the Central Sensitization Inventory (CSI) as a treatment outcome measure for patients with chronic spinal pain disorder in a functional restoration program. Spine J. 2017, 17, 1819–1829. [Google Scholar] [CrossRef]
- Shigetoh, H.; Tanaka, Y.; Koga, M.; Osumi, M.; Morioka, S. The Mediating Effect of Central Sensitization on the Relation between Pain Intensity and Psychological Factors: A Cross-Sectional Study with Mediation Analysis. Pain Res. Manag. 2019, 2019, 3916135. [Google Scholar] [CrossRef] [PubMed]
- Shigetoh, H.; Koga, M.; Tanaka, Y.; Morioka, S. Central sensitivity is associated with poor recovery of pain: Prediction, cluster, and decision tree analyses. Pain Res. Manag. 2020, 2020, 8844219. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y. An Examination of the Validity of the Central Sensitization Inventory with Chronic Disabling Occupational Musculoskeletal Disorders; The University of Texas at Arlington: Arlington, TX, USA, 2014. [Google Scholar]
- Nishigami, T.; Tanaka, K.; Mibu, A.; Manfuku, M.; Yono, S.; Tanabe, A. Development and psychometric properties of short form of central sensitization inventory in participants with musculoskeletal pain: A cross-sectional study. PLoS ONE 2018, 13, e0200152. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.; Bishop, S.R.; Pivik, J. The pain catastrophizing scale: Development and validation. Psychol. Assess. 1995, 7, 524. [Google Scholar] [CrossRef]
- Adachi, T.; Nakae, A.; Maruo, T.; Shi, K.; Shibata, M.; Maeda, L.; Saitoh, Y.; Sasaki, J. Validation of the Japanese version of the pain self-efficacy questionnaire in Japanese patients with chronic pain. Pain Med. 2014, 15, 1405–1417. [Google Scholar] [CrossRef]
- van der Noord, R.; Paap, D.; van Wilgen, C.P. Convergent validity and clinically relevant categories for the Dutch Central Sensitization Inventory in patients with chronic pain. J. Appl. Biobehavioral. Res. 2018, 23, e12119. [Google Scholar] [CrossRef]
- van Wilgen, C.P.; Vuijk, P.J.; Kregel, J.; Voogt, L.; Meeus, M.; Descheemaeker, F.; Keizer, D.; Nijs, J. Psychological Distress and Widespread Pain Contribute to the Variance of the Central Sensitization Inventory: A Cross-Sectional Study in Patients with Chronic Pain. Pain Pract. 2018, 18, 239–246. [Google Scholar] [CrossRef]
- Kosek, E.; Cohen, M.; Baron, R.; Gebhart, G.F.; Mico, J.A.; Rice, A.S.C.; Rief, W.; Sluka, A.K. Do we need a third mechanistic descriptor for chronic pain states? Pain 2016, 157, 1382–1386. [Google Scholar] [CrossRef]
- Kosek, E.; Clauw, D.; Nijs, J.; Baron, R.; Gilron, I.; Harris, R.E.; Mico, J.A.; Rice, A.S.C.; Sterling, M. Chronic nociplastic pain affecting the musculoskeletal system: Clinical criteria and grading system. Pain 2021, 162, 2629–2634. [Google Scholar] [CrossRef] [PubMed]
- English, B. Neural and Psychosocial Mechanisms of Pain Sensitivity in Fibromyalgia. Pain Manag. Nurs. 2014, 15, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Muniandy, Y.; Vasanthi, R. Prevalence of musculoskeletal disorders and associated work-related risk factors among pastry chefs in malacca, malaysia. Int. J. Aging Health Mov. 2021, 3, 20–30. [Google Scholar]
- Hodges, P.W.; Smeets, R.J. Interaction between pain, movement, and physical activity: Short-term benefits, long-term consequences, and targets for treatment. Clin. J. Pain 2015, 31, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Galan-Martin, M.A.; Montero-Cuadrado, F.; Lluch-Girbes, E.; Coca-López, M.C.; Mayo-Iscar, A.; Cuesta-Vargas, A. Pain neuroscience education and physical therapeutic exercise for patients with chronic spinal pain in spanish physiotherapy primary care: A pragmatic randomized controlled trial. J. Clin. Med. 2020, 9, 1201. [Google Scholar] [CrossRef] [PubMed]
- Malfliet, A.; Kregel, J.; Coppieters, I.; De Pauw, R.; Meeus, M.; Roussel, N.; Cagnie, B.; Danneels, L.; Nijs, J. Effect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain a randomized clinical trial. JAMA Neurol. 2018, 75, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Leysen, L.; Vanlauwe, J.; Logghe, T.; Ickmans, K.; Polli, A.; Malfliet, A.; Coppieters, I.; Huysmans, E. Treatment of central sensitization in patients with chronic pain: Time for change? Expert Opin. Pharmacother. 2019, 20, 1961–1970. [Google Scholar] [CrossRef]
- Iwakiri, K.; Sotoyama, M.; Takahashi, M.; Liu, X.; Koda, S.; Ichikawa, K. Effectiveness of re-education based on appropriate care methods using welfare equipment on the prevention of low back pain among care workers: A 1.5 year follow-up study. Ind. Health 2018, 56, 419–426. [Google Scholar] [CrossRef]

| Variables | No CSSs (n = 144, 21.8%) | Mild CSSs (n = 380, 57.6%) | Moderate/Severe CSSs (n = 136, 20.6%) | p Value |
|---|---|---|---|---|
| Age (years) | 44.0 (21.0) | 43.0 (18.0) | 44.0 (16.5) | N.S. |
| Sex (male: female) | 57:87 (39.6%:60.4%) | 117:263 (30.8%:69.2%) | 41:95 (30.1%:69.9%) | N.S. |
| Years of employment | 10.0 (11.0) | 11.0 (11.0) | 11.0 (12.0) | N.S. |
| Pain duration (acute/chronic LBP (%)) | 79/65 (54.9%:45.1%) | 132/248 (34.7%:65.3%) | 29/107 (21.3%:78.7%) | p < 0.001 |
| Number of pain sites (including LBP) | 2.0 (2.0) | 3.0 (2.0) | 4.0 (2.0) | p < 0.001 |
| LBP intensity (NRS: 0–10) | 3.0 (3.0) | 4.0 (2.0) | 5.0 (3.3) | p < 0.001 |
| Severity of LBP: mild/moderate/severe (%) | 94/42/8 (65.2%/29.2%/5.6%) | 155/162/63 (40.8%/42.6%/16.6%) | 34/65/37 (25.0%/47.8%/27.2%) | p < 0.001 |
| LBP intensity before becoming caregivers (NRS: 0–10) | 1.0 (2.0) | 1.0 (2.0) | 1.0 (3.0) | p < 0.05 |
| CSI-9 (0–36) | 7.0 (3.0) | 15.0 (5.0) | 23.0 (4.0) | p < 0.001 |
| PCS (0–52) | 15.0 (17.0) | 20.0 (13.3) | 29.5 (14.0) | p < 0.001 |
| PCS ≥ 30 (%) | 13 (9%) | 68 (17.9%) | 68 (50%) | p < 0.001 |
| PSEQ (0–60) | 43.5 (21.3) | 37.0 (15.0) | 30.5 (19.0) | p < 0.001 |
| PSEQ ≤ 40 (%) | 61 (42.4%) | 229 (60.3%) | 96 (70.6%) | p < 0.001 |
| Interference with work due to LBP (no interference vs. interference with work) | 85/59 (59.0%/41.0%) | 168/155/57 (44.2%/40.8%/15.0%) | 51/64/21 (37.5%/47.1%/15.4%) | p < 0.001 |
| Amount of assistance needed for transferring (very little/light assistance/full assistance) (%) | 13/36/95v (9%/25%/66%) | 16/364 (4.2%/95.8%) | 3/133 (2.2%/97.8%) | p < 0.05 |
| Frequency of back-straining movements (often/several/minimal) (%) | 52/58/34 (36.1%/40.3%/23.6%) | 105/178/97 (105%/178%/97%) | 24/61/51 (24%/61%/51%) | p < 0.01 |
| Environment and equipment to prevent LBP (adequate/adequate but insufficient/inadequate) (%) | 32/90/22 (22.2%/62.5%/15.3%) | 65/235/80 (17.1%/61.8%/21.1%) | 15/86/35 (11.0%/63.3%/25.7%) | N.S. |
| Variables | No CSSs (n = 144) | Mild CSSs (n = 380) | Moderate/Severe CSSs (n = 136) |
|---|---|---|---|
| Sex (male/female) | 2.03a/−2.03a | −1.14/1.14 | −0.68/0.68 |
| Acute/chronic LBP | 5.22a/−5.22a | −1.01/1.01 | −4.09a/4.09a |
| Severity of LBP (mild/moderate/severe) | 6.14a/−3.20a/−3.96a | −1.26/1.14/0.17 | −4.73a/1.87/3.84a |
| PCS score (<30/≥30) | 4.40a/−4.40a | 3.35a/−3.35a | −8.59a/8.59a |
| PSEQ score (≥40/<40) | −4.40a/4.40a | 1.08/−1.08 | 3.21a/−3.21a |
| Interference with work due to LBP (no interference/interference with work) | 3.53a/−3.53a | −1.11/1.11 | −2.25a/2.25a |
| Amount of assistance needed for transferring (very little/light assistance/full assistance) (%) | 2.64a/−0.24/−1.01 | −0.89/1.10/−0.63 | −1.61/−1.11/1.80 |
| Frequency of back-straining movements (often/several/minimal) (%) | 2.64a/−1.29/−1.20 | 0.14/1.11/−1.37 | −2.87a/−0.04/2.91a |
| Environment and equipment to prevent LBP (adequate/adequate but insufficient/inadequate) (%) | 1.90/0.06/−1.83 | 0.11/−0.27/0.22 | −2.07a/0.26/1.60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shigetoh, H.; Abiko, T.; Ohyama, M.; Sakata, E.; Murata, S. Associations of Central Sensitization-Related Symptoms with Low Back Pain-Related Factors and Work Status in Caregivers. Int. J. Environ. Res. Public Health 2022, 19, 10135. https://doi.org/10.3390/ijerph191610135
Shigetoh H, Abiko T, Ohyama M, Sakata E, Murata S. Associations of Central Sensitization-Related Symptoms with Low Back Pain-Related Factors and Work Status in Caregivers. International Journal of Environmental Research and Public Health. 2022; 19(16):10135. https://doi.org/10.3390/ijerph191610135
Chicago/Turabian StyleShigetoh, Hayato, Teppei Abiko, Michie Ohyama, Eiji Sakata, and Shin Murata. 2022. "Associations of Central Sensitization-Related Symptoms with Low Back Pain-Related Factors and Work Status in Caregivers" International Journal of Environmental Research and Public Health 19, no. 16: 10135. https://doi.org/10.3390/ijerph191610135
APA StyleShigetoh, H., Abiko, T., Ohyama, M., Sakata, E., & Murata, S. (2022). Associations of Central Sensitization-Related Symptoms with Low Back Pain-Related Factors and Work Status in Caregivers. International Journal of Environmental Research and Public Health, 19(16), 10135. https://doi.org/10.3390/ijerph191610135






