The Use of Fluorides in Public Health: 65 Years of History and Challenges from Brazil
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. First Interventions
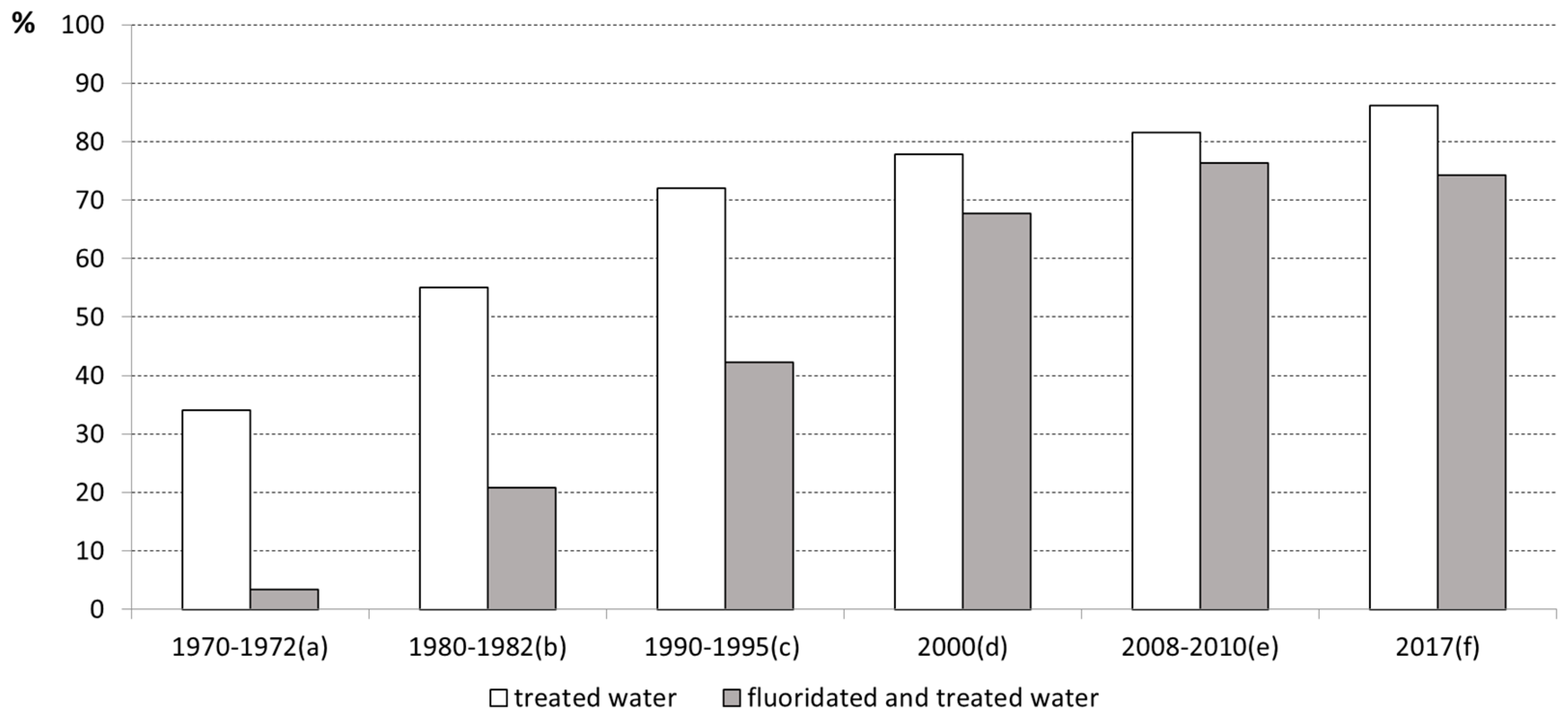
4.2. The Expansion after 1974
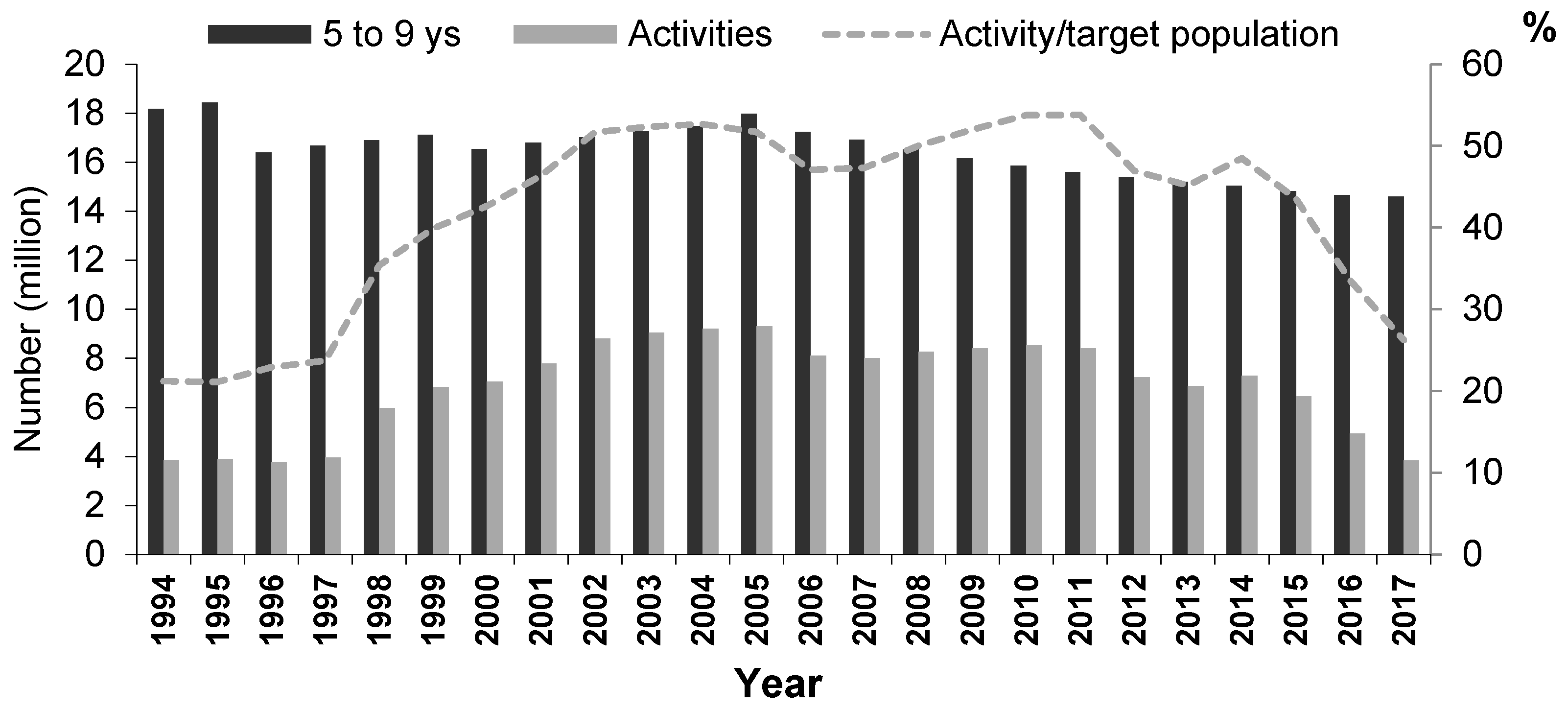
4.3. After the 1988 Constitution
4.4. From 2010 to 2017
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- World Health Organization. World Health Assembly Resolution Paves the Way for Better Oral Health Care; WHO: Geneva, Switzerland, 2021; Available online: https://www.who.int/news/item/27-05-2021-world-health-assembly-resolution-paves-the-way-for-better-oral-health-care (accessed on 17 May 2022).
- Whelton, H.P.; Spencer, A.J.; Do, L.G.; Rugg-Gunn, A.J. Fluoride Revolution and Dental Caries: Evolution of Policies for Global Use. J. Dent. Res. 2019, 98, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Ricomini-Filho, A.P.; Chávez, B.A.; Giacaman, R.A.; Frazão, P.; Cury, J.A. Community interventions and strategies for caries control in Latin American and Caribbean countries. Braz. Oral. Res. 2021, 35, e054. [Google Scholar] [CrossRef] [PubMed]
- O’Mullane, D.M.; Baez, R.J.; Jones, S.; Lennon, M.A.; Petersen, P.E.; Rugg-Gunn, A.J.; Whelton, H.; Whitford, G.M. Fluoride and oral health. Comm. Dental. Health 2016, 33, 69–99. [Google Scholar]
- World Bank. Data and Statistics. 2020. Available online: https://bit.ly/39eANuJ (accessed on 4 July 2022).
- Howlett, M.; Ramesh, M.; Perl, A. Studying Public Policy: Policy Cycles and Policy Subsystems, 3rd ed.; Oxford University Press: Toronto, ON, Canada, 2009. [Google Scholar]
- Wood, E.M. Democracy against Capitalism; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Grinplastch, B.S. Fluoretação de águas no Brasil. Bol. Ofic. Sanit Panam 1974, 76, 321–330. [Google Scholar]
- Pinto, V.G. Saúde bucal no Brasil. Rev. Saude Publ. 1983, 17, 316–327. [Google Scholar] [CrossRef][Green Version]
- Saiani, C.C.S.; Toneto-Junior, R. Evolução do acesso a serviços de saneamento básico no Brasil (1970 a 2004). Econ. Soc. 2010, 19, 79–106. [Google Scholar] [CrossRef]
- Narvai, P.C. Dental caries and fluorine: A twentieth century relation. Cienc. Saude Colet. 2000, 5, 381–392. [Google Scholar] [CrossRef][Green Version]
- Frazão, P.; Narvai, P.C. Water fluoridation in Brazilian cities at the first decade of the 21st century. Rev. Saude Publ. 2017, 51, 47. [Google Scholar] [CrossRef]
- Fundação Instituto Brasileiro de Geografia e Estatística (IBGE). Censo Demográfico-2010: Características da População e dos Domicílios: Resultados do Universo; IBGE: Rio de Janeiro, Brazil, 2011; 270p. [Google Scholar]
- Fundação Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saneamento Básico-2017: Abastecimento de Água e Esgotamento Sanitário; IBGE: Rio de Janeiro, Brazil, 2020; 119p. [Google Scholar]
- Chaves, M.M.; Fraenkel, J.M. Princípios básicos para a organização de um serviço dentário escolar. Rev. Serv. Esp. Saúde Publ. 1952, 5, 469–484. [Google Scholar]
- Gandra, Y.R. Contribution to the knowledge of the fluorine content of waters in the state of São Paulo: Sanitary significance of the problem. Arch. Fac. Hig. Saude Publ. Univ. S. Paulo 1950, 4, 135–184. [Google Scholar]
- Souza, C.F.M.; Lima, J.F.; Adriano, M.S.P.F.; Carvalho, F.G.; Forte, F.D.; Oliveira, R.F.; Silva, A.P.; Sampaio, F.C. Assessment of groundwater quality in a region of endemic fluorosis in the northeast of Brazil. Environ. Monit. Assess 2013, 185, 4735–4743. [Google Scholar] [CrossRef] [PubMed]
- Akuno, M.H.; Nocella, G.; Milia, E.P.; Gutierrez, L. Factors influencing the relationship between fluoride in drinking water and dental fluorosis: A ten-year systematic review and meta-analysis. J. Water Health 2019, 17, 845–862. [Google Scholar] [CrossRef]
- Freire, P.S. Primeiros resultados com a fluoração de água no Brasil. Rev. Serv. Esp. Saúde Públ. 1957, 9, 327–340. [Google Scholar]
- Viegas, Y.; Viegas, A.R. Análise dos dados de prevalência de cárie dental na cidade de Campinas, SP, Brasil, depois de dez anos de fluoração da água de abastecimento público. Rev. Saúde Públ. 1974, 8, 399–409. [Google Scholar] [CrossRef]
- Moreira, B.H.W.; Tumang, A.J.; Guimarães, L.O.C. Incidência de cárie dentária de escolares de Piracicaba-SP, após 6 e 9 anos de fluoretação das águas de abastecimento público. Rev. Bras. Odontol. 1983, 40, 11–14. [Google Scholar]
- De Pretto, P.W.; Dias, O.M.L.; Lopes, E.S.; Bastos, J.R.M. Redução de cárie dentária em escolares de Bauru, após oito anos de fluoretação de água de abastecimento público. Estomatol. Cult. 1985, 15, 20–25. [Google Scholar]
- Arcieri, R.M.; Carvalho, M.L.; Gonçalves, L.M.G.; Almeida, H.A.; Pereira, A.L.C.; Oliveira, E.M. Estudo comparativo da prevalência da cárie dentária após dez anos da adição de flúor nas águas de abastecimento público de Uberlândia, MG. Rev. Paul. Odontol. 1986, 8, 46–55. [Google Scholar]
- Viegas, Y.; Viegas, A.R. Prevalência de cárie dental em Barretos, SP, Brasil, após dezesseis anos de fluoretação da água de abastecimento público. Rev. Saúde Públ. 1988, 22, 25–35. [Google Scholar] [CrossRef]
- Spencer, A.J. Water Fluoridation. In Oral Epidemiology: A Textbook on Oral Health Conditions, Research Topics and Methods; Peres, M.A., Antunes, J.L.F., Watt, R.G., Eds.; Springer Nature: Cham, Switzerland, 2021; Available online: https://doi.org/10.1007/978-3-030-50123-5_29 (accessed on 17 May 2022).
- Bier, A.G.; Paulani, L.M.; Messenberg, R.P. A crise do saneamento no Brasil: Reforma tributária, uma falsa resposta. Pesq. Plan. Econ. 1988, 18, 161–196. [Google Scholar]
- Furtado, C. The Development of Brazil. Sci. Am. 1963, 209, 208–223. [Google Scholar] [CrossRef]
- Turolla, F.A.; Anker, T.; Faria, R.M. Infrastructure Services in Brazil: The Role of Public-Private Partnership in the Water & Sewerage Sector. 5 November 2004. Available online: https://ssrn.com/abstract=616241 (accessed on 17 May 2022). [CrossRef]
- Marinho, M.G.S.M.C.; Oliveira, S.D.P. O Governo Geisel (1974–1979): O Ápice da Disputa pelo Poder entre ‘Duros’ e ‘Moderados’ e sua Expressão Memorialista entre os Militares. Antíteses 2015, 8, 74–100. [Google Scholar] [CrossRef]
- Narvai, P.C.; Frazão, P. Epidemiologia, política, e saúde bucal coletiva. In Epidemiologia da Saúde Bucal; Antunes, J.L.F., Peres, M.A., Eds.; Guanabara Koogan: Rio de Janeiro, Brazil, 2006; pp. 346–362. [Google Scholar]
- Arretche, M. Trajetórias das Desigualdades: Como o Brasil Mudou nos Últimos Cinquenta anos; Editora Unesp CEM: São Paulo, Brazil, 2015. [Google Scholar]
- Jacobi, P.R. Movimentos sociais e Estado: Efeitos político-institucionais da ação coletiva. In Demandas Populares, Políticas Públicas e Saúde; Costa, N.R., Minayo, C.S., Ramos, C.L., Stotz, E.N., Eds.; Vozes: Petrópolis, Brazil, 1989; Volume II. [Google Scholar]
- Fundação Nacional de Saúde (FUNASA). Manual de Orientação para Criação e Organização de Autarquias Municipais de Água e Esgoto; Ministério da Saúde: Brasília, Brazil, 2001.
- Nicolella, A.C.; Dragone, D.S.; Bacha, C.J.C. Determinantes da demanda de fertilizantes no Brasil no período de 1970 a 2002. Rev. Econ. Sociol. Rural 2005, 43, 81–100. [Google Scholar] [CrossRef]
- Chaves, S.C.L. Política de Saúde Bucal no Brasil: Teoria e Prática; EDUFBA: Salvador, Brazil, 2016; 376p. [Google Scholar]
- Sader, E. Quando Novos Personagens Entraram em cena; Paz e Terra: Rio de Janeiro, Brazil, 1988. [Google Scholar]
- Fleury, S. Brazil’s health-care reform: Social movements and civil society. Lancet 2011, 377, 1724–1725. [Google Scholar] [CrossRef]
- Vieira-da-Silva, L.M.; Pinell, P. The genesis of collective health in Brazil. Sociol. Health Illn. 2014, 36, 432–446. [Google Scholar] [CrossRef]
- Rossi, T.R.A.; Moreira, L.G.P.; Barros, S.G. History of fluoridation policies as a strategy by the Brazilian Legislative Branch to fight dental caries, 1963 to 2019. Cad. Saúde Públ. 2020, 36, e00208418. [Google Scholar] [CrossRef]
- Neder, A.C.N.; Manfredini, M.A. Sobre a oportunidade de fluoretar o sal no Brasil: A modernidade do atraso. Saúde Deb. 1991, 32, 73–76. [Google Scholar]
- Newbrun, E. Fluorides and Dental Caries, 2nd ed.; Springfield C C Thomas: Geneseo, IL, USA, 1975. [Google Scholar]
- Haitgejorden, O.; Heloe, L.A. Fluorides for everyone: A review of school-based or community programs. Comm. Dent. Oral. Epidemiol. 1981, 9, 159–169. [Google Scholar] [CrossRef]
- Pinto, V.G. Saúde Bucal: Odontologia Social e Preventiva; Santos: São Paulo, Brazil, 1989. [Google Scholar]
- Valla, V.V.; Hollanda, E. Fracasso escolar, saúde e cidadania. In Demandas Populares, Políticas Públicas e Saúde: Volume II. Movimentos Sociais e Cidadania; Costa, N.R., Minayo, M.C.S., Ramos, C.L., Stotz, E.N., Atiê, E., Hollanda, E., Souza, H.O., Melo, J.A.C., Eds.; Ed. Vozes: Petrópolis, Brazil, 1989; pp. 103–143. [Google Scholar]
- Pinto, I.L. Dental caries prevention with biannual topical administration of acidulated phosphate fluoride. Rev. Saude Publ. 1993, 27, 277–290. [Google Scholar] [CrossRef]
- Cury, J.A.; Tenuta, L.M.A.; Ribeiro, C.C.C.; Paes Leme, A.F. The importance of fluoride dentifrices to the current dental caries prevalence in Brazil. Braz. Dent. J. 2004, 15, 167–174. [Google Scholar] [CrossRef]
- Narvai, P.C. Cárie dentária e flúor: Uma relação do século XX. Ciênc. Saúde Colet. 2000, 5, 381–392. [Google Scholar] [CrossRef][Green Version]
- Centers for Disease Control and Prevention (CDC). Achievements in Public Health, 1900–1999: Fluoridation of drinking water to prevent dental caries. MMW Morb. Mortal. Wkly. Rep. 1999, 48, 933–940. Available online: https://www.cdc.gov/Mmwr/preview/mmwrhtml/mm4841a1.htm (accessed on 17 May 2022).
- Peres, M.A.; Fernandes, L.S.; Peres, K.G. Inequality of water fluoridation in Southern Brazil: The inverse equity hypothesis revisited. Soc. Sci. Med. 2004, 58, 1181–1189. [Google Scholar] [CrossRef]
- Gabardo, M.C.; Silva, W.J.; Olandoski, M.; Moysés, S.T.; Moysés, S.J. Inequalities in public water supply fluoridation in Brazil: An ecological study. BMC Oral. Health 2008, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Najar, A.L.; Fiszon, J.T. Política pública e o modelo de saneamento no Brasil. In Demandas Populares, Políticas Públicas e Saúde; Costa, N.R., Minayo, C.S., Ramos, C.L., Stotz, E.N., Eds.; Ed. Vozes: Petrópolis, Brazil, 1989; Volume I. [Google Scholar]
- Zilbovicius, C.; Ferreira, R.G.L.A.; Narvai, P.C. Water and health: Fluoridation and the repeal of Brazilian Federal Law 6050/74. Rev. Dir. Sanit. 2018, 18, 104–124. [Google Scholar] [CrossRef]
- Souza-Neto, A.C.; Frazão, P. Principles invoked in a population-based health policy: The case of water fluoridation in Brazil. Saúde Soc. 2020, 29, e190048. [Google Scholar]
- Shannon, I.L. The problem of maintaining the fluoride level in fluoridating the water supply. Texas Dent. J. 1980, 98, 6–8. [Google Scholar]
- Kuthy, R.A.; Naleway, C.; Durkee, J. Factors associated with maintenance of proper water fluoride levels. J. Am. Dent. Assoc. 1985, 110, 511–513. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for Drinking-Water Quality, 1st ed.; Volume 1—Recommendations; WHO: Geneva, Switzerland, 1984. [Google Scholar]
- Vasconcellos, M.C.C. Prevalência de cárie dentária em escolares de 7 a 12 anos de idade, na cidade de Araraquara, SP (Brasil), 1979. Rev. Saúde Públ. 1982, 16, 317–328. [Google Scholar] [CrossRef][Green Version]
- Narvai, P.C.; Frazão, P.; Fernandez, R.A. Fluoretação da água e democracia. Saneas 2004, 2, 29–33. [Google Scholar]
- Panizzi, M.; Peres, M.A. Dez anos de heterocontrole da fluoretação de águas em Chapecó, Estado de Santa Catarina, Brasil. Cad. Saúde Publ. 2008, 24, 2021–2031. [Google Scholar] [CrossRef] [PubMed]
- Frazão, P.; Ely, H.C.; Noro, L.R.A.; Pinheiro, H.H.C.; Cury, J.A.; Narvai, P.C. The surveillance framework of water and the reporting of fluoride concentration indicators. Saúde Deb. 2018, 42, 274–286. [Google Scholar] [CrossRef]
- Belotti, L.; Brandão, S.R.; Pacheco, K.T.S.; Frazão, P.; Esposti, C.D.D. Vigilância da qualidade da água para consumo humano: Potencialidades e limitações com relação à fluoretação segundo os trabalhadores. Saúde Deb. 2019, 43, 51–62. [Google Scholar] [CrossRef]
- Frazão, P.; Soares, C.C.S.; Fernandes, G.F.; Marques, R.A.; Narvai, P.C. Fluoretação da água e insuficiências no sistema de informação da política de vigilância à saúde. Rev. Assoc. Paul Cir. Dent. 2013, 67, 94–100. [Google Scholar]
- Frazão, P. 20 years of experience with the Brazilian Unified National Health System: Strides and challenges for oral health. Cad. Saúde Públ. 2009, 25, 712. [Google Scholar] [CrossRef][Green Version]
- Scatena, J.H.G.; Tanaka, O.Y. Os instrumentos normalizadores (NOB) no processo de descentralização da saúde. Saúde Soc. 2001, 10, 47–74. [Google Scholar] [CrossRef]
- Celeste, R.K.; Vital, J.F.; Junger, W.L.; Reichenheim, M.E. Séries de procedimentos odontológicos realizadas nos serviços públicos brasileiros, 1994–2007. Ciênc. Saúde Colet. 2011, 16, 4523–4532. [Google Scholar] [CrossRef]
- Barros, S.G.; Chaves, S.C.L. A utilização do sistema de informações ambulatoriais (SIA-SUS) como instrumento para caracterização das ações de saúde bucal. Epidemiol. Serv. Saúde 2003, 12, 41–51. [Google Scholar] [CrossRef]
- Volpato, L.E.R.; Scatena, J.H. Análise da política de saúde bucal do Município de Cuiabá, Estado de Mato Grosso, Brasil, a partir do banco de dados do Sistema de Informações Ambulatoriais do Sistema Único de Saúde (SIA-SUS). Epidemiol. Serv. Saude 2006, 15, 47–55. [Google Scholar] [CrossRef]
- Carvalho, L.A.C.; Scabar, L.F.; Souza, D.S.; Narvai, P.C. Set of Procedures in Oral Health: Origin, apogee and decline. Saúde Soc. 2009, 18, 490–499. [Google Scholar]
- Fernandes, L.S.; Peres, M.A. Associação entre atenção básica em saúde bucal e indicadores socioeconômicos municipais. Rev. Saúde Públ. 2005, 39, 930–936. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chaves, S.C.L.; Aranha-Rossi, T.R.; Lima, A.M.F.S. Dental service coverage and oral health promotion community actions in primary care in Brazil between 2003 and 2019. Health Policy OPEN 2020, 1, 100022. [Google Scholar] [CrossRef]
- Cury, J.A.; Caldarelli, P.G.; Tenuta, L.M.A. Necessity to review the Brazilian regulation about fluoride toothpastes. Rev. Saúde Públ. 2015, 49, 74. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.B.; Frazão, P. Characteristics of sanitation companies associated to water fluoridation of the supply systems of Brazilian municipalities, 2008. Rev. Bras. Epidemiol. 2020, 23, e200086. [Google Scholar] [CrossRef]
- Narzetti, D.A.; Marques, R.C. Access to Water and Sanitation Services in Brazilian Vulnerable Areas: The Role of Regulation and Recent Institutional Reform. Water 2021, 13, 787. [Google Scholar] [CrossRef]
- Silva, F.B.; Frazão, P. Sanitation utilities and fluoridation of water supply systems: An ecological study in Brazilian municipalities, 2008-2010. Epidemiol. Serv. Saude 2018, 27, e2018015. [Google Scholar]
- Sabbioni, G. Efficiency in the Brazilian sanitation sector. Util. Policy 2008, 16, 11–20. [Google Scholar] [CrossRef]
- Belotti, L.; Frazão, P. Intervening factors in the costs of fluoridation in water supply systems: A case study in seven population sizes. Eng. Sanit. Amb. 2021, 26, 785–791. [Google Scholar] [CrossRef]
- Belotti, L.; Frazão, P. Effectiveness of water fluoridation in an upper-middle-income country: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2022, 32, 503–513. [Google Scholar] [CrossRef]
- Mota, A.G.; Frazão, P. Street-level implementers of population-based oral health policies: The case of water fluoridation supply in Brazil’s small towns. Community Dent. Health 2021, 38, 187–191. [Google Scholar]
- Bomfim, R.A.; Watt, R.G.; Frazão, P. Intersectoral collaboration and coordination mechanisms for implementing water fluoridation: Challenges from a case study in Brazil. J. Public Health Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Collaborating Center of the Ministry of Health in Oral Health Surveillance (CECOL/USP). Consenso Técnico Sobre Classificação de Águas de Abastecimento Público Segundo o teor de Flúor; Faculdade de Saúde Pública da Universidade de São Paulo: São Paulo, Brazil, 2011; Available online: http://www.cecol.fsp.usp.br/dcms/uploads/arquivos/1398177715_CECOL-USP-ClassificacaoAguasSegundoTeorFluor-DocumentoConsensoTecnico-2011.pdf (accessed on 4 July 2022).
- Belotti, L.; Zilbovicius, C.; Soares, C.C.D.S.; Narvai, P.C.; Frazão, P. Municipality-Level Characteristics Associated with Very Low to Good Quality of Water Fluoridation in São Paulo State, Brazil, in 2015. JDR Clin. Trans. Res. 2022, 7, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Paulino, C.M.; Belotti, L.; Azevedo, M.K.Z.; Frazão, P. Coverage of fluoride data in water supply systems using the R software. Rev. Saúde Públ. 2022, 56, 18. [Google Scholar] [CrossRef] [PubMed]
- Chisini, L.A.; Martin, A.S.S.; Pires, A.L.C.; Noronha, T.G.; Demarco, F.F.; Conde, M.C.M.; Correa, M.B. A 19-years study of the dental procedures performed in the Brazilian Unified Health System. Cad. Saude Colet. 2019, 27, 345–353. [Google Scholar] [CrossRef]
- Massuda, A.; Hone, T.; Leles, F.A.G.; Castro, M.C.; Atun, R. The Brazilian health system at crossroads: Progress, crisis and resilience. BMJ Global. Health 2018, 3, e000829. [Google Scholar] [CrossRef]
- Rossi, T.R.A.; Sobrinho, J.E.L.; Chaves, S.C.L.; Martelli, P.J.L. Crise econômica, austeridade e seus efeitos sobre o financiamento e acesso a serviços públicos e privados de saúde bucal. Ciênc. Saúde Colet. 2019, 24, 4427–4436. [Google Scholar] [CrossRef]
- Narvai, P.C. Ocaso do ‘Brasil Sorridente’ e perspectivas da Política Nacional de Saúde Bucal em meados do século XXI. Tempus-Actas Saude Colet. 2020, 14, 175–187. [Google Scholar] [CrossRef]
- Fundação Instituto Brasileiro de Geografia e Estatística (IBGE). National Survey of School Health (PeNSE). Available online: https://www.ibge.gov.br/en/statistics/social/health/16837-national-survey-of-school-health-editions.html?=&t=o-que-e (accessed on 4 July 2022).
- Sousa, M.C.; Esperidião, M.A.; Medina, M.G. Intersectorality in the ‘Health in Schools’ Program: An evaluation of the political-management process and working practices. Ciênc. Saúde Colet. 2017, 22, 1781–1790. [Google Scholar] [CrossRef]
- Petersen, P.E.; Baez, R.J.; Ogawa, H. Global application of oral disease prevention and health promotion as measured 10 years after the 2007 World Health Assembly statement on oral health. Comm. Dent. Oral. Epidemiol. 2020, 48, 338–348. [Google Scholar] [CrossRef]
- Jurgensen, N.; Petersen, P. Promoting oral health of children through schools-results from a WHO global survey 2012. Community Dent. Health 2014, 30, 204–218. [Google Scholar]
- Bin, D. Macroeconomic policies and economic democracy in neoliberal Brazil. Econ. Soc. 2015, 24, 513–539. [Google Scholar] [CrossRef]
- Anderson, P. Brazil Apart: 1964–2019; Verso Books: London, UK, 2019. [Google Scholar]
- Hochman, G.; Faria, C.A.P. Federalismo e Políticas Públicas no Brasil; Ed. Fiocruz: Rio de Janeiro, Brazil, 2013. [Google Scholar]
- Paes-Sousa, R.; Schramm, J.M.A.; Mendes, L.V.P. Fiscal austerity and the health sector: The cost of adjustments. Ciênc. Saúde Colet. 2019, 24, 4375–4384. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.C.; Costa, N.R. Basic sanitation policy in Brazil: Discussion of a path. Hist. Ciênc. Saúde-Manguinhos 2016, 23, 615–634. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frazão, P. The Use of Fluorides in Public Health: 65 Years of History and Challenges from Brazil. Int. J. Environ. Res. Public Health 2022, 19, 9741. https://doi.org/10.3390/ijerph19159741
Frazão P. The Use of Fluorides in Public Health: 65 Years of History and Challenges from Brazil. International Journal of Environmental Research and Public Health. 2022; 19(15):9741. https://doi.org/10.3390/ijerph19159741
Chicago/Turabian StyleFrazão, Paulo. 2022. "The Use of Fluorides in Public Health: 65 Years of History and Challenges from Brazil" International Journal of Environmental Research and Public Health 19, no. 15: 9741. https://doi.org/10.3390/ijerph19159741
APA StyleFrazão, P. (2022). The Use of Fluorides in Public Health: 65 Years of History and Challenges from Brazil. International Journal of Environmental Research and Public Health, 19(15), 9741. https://doi.org/10.3390/ijerph19159741




