Coping with Stress in Neoplastic Diseases
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
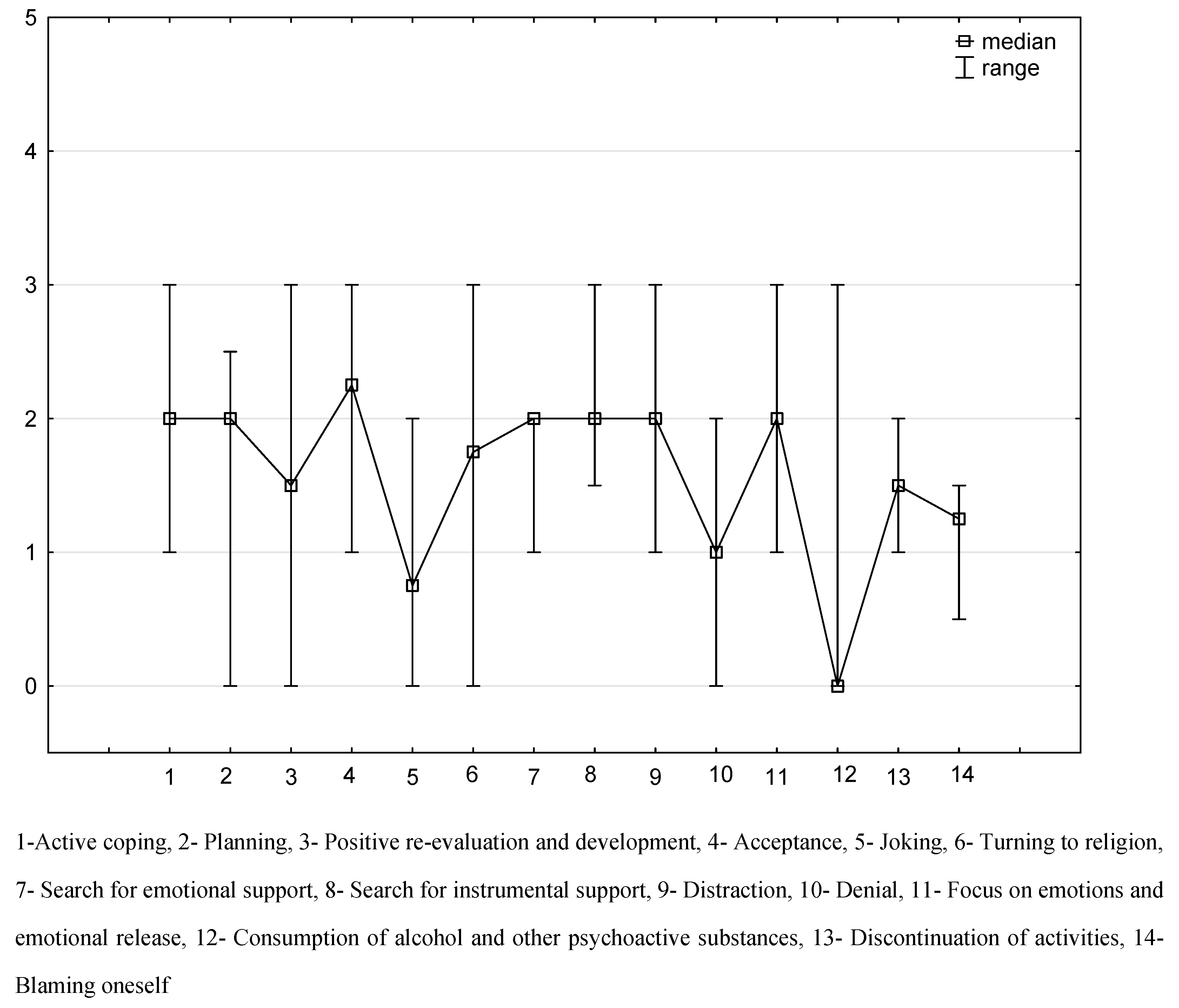
3. Results
Limitation of the Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sklar, L.S.; Anisman, H. Stress and cancer. Psychol. Bull. 1981, 89, 369–406. [Google Scholar] [CrossRef]
- Lissoni, P.; Cangemi, P.; Pirato, D.; Roselli, M.G.; Rovelli, F.; Brivio, F.; Malugani, F.; Maestroni, G.J.M.; Conti, A.; Laudon, M.; et al. A review on cancer-psychospiritual status interactions. Neuro Endocrinol. Lett. 2001, 22, 175–180. [Google Scholar]
- Moussas, G.I.; Papadopoulou, A.G.; Christodoulaki, A.G.; Karkanias, A.P. Psychological and psychiatric problems in cancer patients: Relationship to the localization of the disease. Psychiatriki 2012, 23, 46–60. [Google Scholar]
- Juczyński, Z.; Ogińska-Bulik, N. NPSR—Narzędzia Pomiaru Stresu i Radzenia Sobie ze Stresem, 1st ed.; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszaw, Poland, 2009; pp. 5–20. [Google Scholar]
- Sabanciogullari, S.; Yilmaz, F.T. The Effect of Religious Coping on Hope Level of Cancer Patients Receiving Chemotherapy. J. Relig. Health 2021, 60, 2756–2769. [Google Scholar] [CrossRef]
- Bonomo, A.A.; Gragefe, C.K.; Gerbasi, A.R.V.; Carvalho, M.D.B.; Fontes, K.B. Religious/spiritual coping in cancer patients under treatment. J. Nurs. UFPE Line Recife 2015, 9, 7539–7546. [Google Scholar]
- Karekla, M.; Constantinou, M. Religious coping and cancer: Proposing an acceptance and commitment therapy approach. Cogn. Behav. Pract. 2010, 17, 371–381. [Google Scholar] [CrossRef]
- de Paiva Ribeiro Dantas Sousa, F.F.; Freitas, S.M.F.M.; Farias, A.G.S.; Cunha, M.C.S.O.; Araújo, M.F.M.; Veras, V.S. Religious/spiritual coping by people with cancer undergoing chemotherapy: Integrative literature review. SMAD Rev. Eletrônica Saúde Ment. Álcool E Drog. 2017, 13, 45–51. [Google Scholar]
- Osowiecka, K.; Sroda, R.; Saied, A.; Szwiec, M.; Mangold, S.; Osuch, D.; Nawrocki, S.; Rucinska, M. Patients’ Non-Medical and Organizational Needs during Cancer Diagnosis and Treatment. Int. J. Environ. Res. Public Health 2020, 17, 5841. [Google Scholar] [CrossRef]
- Esterbauer, E.; Anders, I.; Ladurner, G.; Huemer, M.; Wranek, U. Stress management in heart diseases, obesity, nicotine and alcohol use. Wien. Klin. Wochenschr. 2001, 17, 947–953. [Google Scholar]
- Alter, C.L. Palliative and supportive care of patients with pancreatic cancer. Semin. Oncol. 1996, 23, 229–240. [Google Scholar]
- Ohaeri, B.M.; Ofi, A.B.; Campbell, O.B. Relationship of knowledge of psychosocial issues about cancer with psychic distress and adjustment among breast cancer clinic attendees in a Nigerian teaching hospital. Psycho-Oncology 2012, 21, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.L.; Mayer, D.K.; Chou, F.H.; Hsiao, K.Y. The Experience of Cancer Stigma in Taiwan: A Qualitative Study of Female Cancer Patients. Arch. Psychiattic Nurs. 2016, 30, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Martins-Klein, B.; Bamonti, P.M.; Owsiany, M.; Naik, A.; Moye, J. Age differences in cancer-related stress, spontaneous emotion regulation, and emotional distress. Aging Ment. Health 2021, 25, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Calderon, C.; Gomez, D.; Carmona-Bayonas, A.; Hernandez, R.; Ghanem, I.; Gil Raga, M.; Garcia, L.O.; Carrasco, M.G.; de Ceballos, M.H.L.; Ferreira, E.; et al. Social support, coping strategies and sociodemographic factors in women with breast cancer. Clin. Transl. Oncol. 2012, 23, 1955–1960. [Google Scholar] [CrossRef]
- Amini-Tehrani, M.; Zamanian, H.; Daryaafzoon, M.; Andikolaei, S.; Mohebbi, M.; Imani, A.; Tahmasbi, B.; Foroozanfar, S.; Jalali, Z. Body image, internalized stigma and enacted stigma predict psychological distress in women with breast cancer: A serial mediation model. J. Adv. Nurs. 2012, 77, 3412–3423. [Google Scholar] [CrossRef]
- Brandberg, Y.; Sandelin, K.; Erikson, S.; Jurell, G.; Liljegren, A.; Lindblom, A.; Lindén, A.; Von Wachenfeldt, A.; Wickman, M.; Arver, B. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: A prospective one year follow up study. J. Clin. Oncol. 2008, 26, 3943–3949. [Google Scholar] [CrossRef]
- Schmid-Buchi, S.; Halfens, R.J.C.; Dassen, T.; Borne, B. Psychosocial problems and needs of post treatment patients with breast cancer and their relatives. Eur. J. Oncol. Nurs. 2009, 15, 260–266. [Google Scholar] [CrossRef]
- Tsaras, K.; Papathanasiou, I.V.; Mitsi, D.; Veneti, A.; Kelesi, M.; Zyga, S.; Fradelos, E.C. Assessment of Depression and Anxiety in Breast Cancer Patients: Prevalence and Associated Factors. Asian Pac. J. Cancer Prev. 2018, 19, 1661–1669. [Google Scholar]
- Onyedibe, M.C.; Ifeagwazi, M.C. Group Psychoeducation to Improve Cognitive Emotion Regulation in Nigerian Women with Breast Cancer. Int. J. Group Psychother. 2021, 71, 509–538. [Google Scholar] [CrossRef]
- Herdman, H.M.; Holland, J.R.; Hewitt, M. Meeting Psychosocial Needs of Women with Breast Cancer; National Academic Press: Washington, DC, USA, 2004. [Google Scholar]
- Taino, G.; Giroletti, E.; Delogu, A.; Malagò, G.; Corona, G.; Businaro, J.; Imbriani, M. Judgment of fitness for work in employees with a history of malignant neoplastic disease and exposed to ionizing radiations: Evaluation criteria and their application in a case-series study. La Med. Lav. 2014, 105, 445–472. [Google Scholar]
- Pluta, M. Professional work in the lives of people with cancer. Stud. Hum. AGH 2020, 3, 15–32. [Google Scholar]
- Pilevarzadeh, M.; Amirshahi, M.; Afsargharehbagh, R.; Rafiemanesh, H.; Hashemi, S.M.; Balouchi, A. Global prevalence of depression among breast cancer patients: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2019, 176, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, S.M.; Rafiemanesh, H.; Aghamohammadi, T.; Badakhsh, M.; Amirshahi, M.; Sari, M.; Behnamfar, N.; Roudini, K. Prevalence of anxiety among breast cancer patients: A systematic review and meta-analysis. Breast Cancer 2020, 27, 166–178. [Google Scholar] [CrossRef] [PubMed]
- Rieke, K.; Schmid, K.K.; Lydiatt, W.; Houfek, J.; Boilesen, E.; Galloway, W.S. Depression and survival in head and neck cancer patients. Oral Oncol. 2017, 65, 76–82. [Google Scholar] [CrossRef]
- Sullivan, D.R.; Forsberg, C.W.; Ganzini, L.; Au, D.H.; Gould, M.K.; Provenzale, D.; Slatore, C.G. Longitudinal changes in depression symptoms and survival among patients with lung cancer: A national cohort assessment. J. Clin. Oncol. 2016, 34, 3984–3991. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Wang, N.; Zhong, L.; Wang, S.; Zheng, Y.; Yang, B.; Zhang, J.; Lin, Y.; Wang, Z. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: A systematic review and meta-analysis of 282, 203 patients. Mol. Psychiatry 2020, 25, 3186–3197. [Google Scholar] [CrossRef]
- Becker, H. Psychodynamic Aspects of Breast Cancer. Psychother. Psychosom. 1979, 32, 287–296. [Google Scholar] [CrossRef]
- Popoola, A.O.; Adewuya, A.O. Prevalence and correlates of depressive disorders in outpatients with breast cancer in Lagos, Nigeria. Psycho-Oncology 2011, 21, 675–679. [Google Scholar] [CrossRef]
| All | n = 306 | ||
|---|---|---|---|
| Sex | |||
| woman | 255 | 83.3 | |
| man | 51 | 16.7 | |
| Age [years] | mean± | 39 ± 8.3 | |
| Place of residence | |||
| city with less than 100.000 residents | 153 | 50.0 | |
| city with more than 100.000 residents | 153 | 50.0 | |
| Education | |||
| secondary, vocational | 102 | 33.3 | |
| higher | 204 | 66.7 | |
| Marital status | |||
| married, in a registered partnership | 255 | 83.3 | |
| divorced, separated | 51 | 16.7 | |
| Employment | |||
| full-time worker | 204 | 66.7 | |
| unemployed | 102 | 33.3 |
| Women | Men | ||||
|---|---|---|---|---|---|
| Stress Management Strategies | Median | 25–75% IQR | Median | 25–75% IQR | p-Value |
| Active coping | 2.00 | (2–2) | 1.00 | (1–1) | <0.001 |
| Planning | 2.00 | (2–2) | 0.00 | (0–0) | <0.001 |
| Positive re-evaluation and development | 2.00 | (2–2.5) | 0.00 | (0–0) | <0.001 |
| Acceptance | 2.00 | (2–2.5) | 3.00 | (3–3) | <0.001 |
| Joking | 0.50 | (0.5–2) | 1.00 | (1–1) | 0.02 |
| Turning to religion | 2.00 | (1.5–2) | 0.00 | (0–0) | <0.001 |
| Search for emotional support | 2.00 | (1.5–2) | 2.00 | (2–2) | <0.001 |
| Search for instrumental support | 2.00 | (2–2) | 3.00 | (3–3) | <0.001 |
| Distraction | 2.00 | (1.5–2) | 3.00 | (3–3) | <0.001 |
| Denial | 1.00 | (0.5–1.5) | 1.00 | (1–1) | 1.0 |
| Focus on emotions and emotional release | 2.00 | (1.5–2) | 3.00 | (3–3) | <0.001 |
| Consumption of alcohol or other psychoactive substances | 0.00 | (0–0) | 0,00 | (0–0) | 0.02 |
| Discontinuation of activity | 1.50 | (1–1.5) | 1.50 | (2–2) | 0.02 |
| Blaming oneself | 1.00 | (1.0–1.5) | 1.50 | (2–2) | <0.001 |
| Stress Management Strategies | r | p-Value |
|---|---|---|
| Active coping | 0.21 | <0.05 |
| Planning | 0.17 | <0.05 |
| Positive re-evaluation and development | 0.09 | >0.05 |
| Acceptance | −0.8 | <0.05 |
| Joking | −0.6 | <0.05 |
| Turning to religion | 0.64 | <0.05 |
| Search for emotional support | 0.44 | <0.05 |
| Search for instrumental support | −0.34 | <0.05 |
| Distraction | −0.77 | <0.05 |
| Denial | −0.06 | >0.05 |
| Focus on emotions and emotional release | −0.77 | <0.05 |
| Consumption of alcohol or other psychoactive substances | −0.39 | <0.05 |
| Discontinuation of activity | −0.49 | <0.05 |
| Blaming oneself | 0.37 | <0.05 |
| City with Less than 100,000 Residents | City with More than 100,000 Residents | ||||
|---|---|---|---|---|---|
| Stress Management Strategies | Median | 25–75% IQR | Median | 25–75% IQR | p-Value |
| Active coping | 2.00 | (1–2) | 2.00 | (1.5–3) | <0.001 |
| Planning | 2.00 | (0–2) | 2.00 | (2–2.5) | <0.001 |
| Positive re-evaluation and development | 1.00 | (0–2) | 2.00 | (0.5–3) | <0.001 |
| Acceptance | 2.00 | (2–3) | 2.50 | (1–3) | 1.00 |
| Joking | 0.50 | (0.5–1) | 2.00 | (0–2) | <0.001 |
| Turning to religion | 1.50 | (0–2) | 2.00 | (1–3) | <0.001 |
| Search for emotional support | 2.00 | (2–2) | 1.50 | (1–2) | <0.001 |
| Search for instrumental support | 2.00 | (2–3) | 2.00 | (1.5–2) | <0.001 |
| Distraction | 2.00 | (1.5–3) | 2.00 | (1–3) | 0.09 |
| Denial | 1.00 | (1–1.5) | 0.50 | (0–2) | <0.001 |
| Focus on emotions and emotional release | 2.00 | (1.5–3) | 2.00 | (1–3) | 0.09 |
| Consumption of alcohol or other psychoactive substances | 0.00 | (0–0) | 0.00 | (0–3) | <0.001 |
| Discontinuation of activity | 1.50 | (1–1.5) | 1.50 | (1–2) | <0.001 |
| Blaming oneself | 1.50 | (1.5–1.5) | 1.00 | (0.5–1) | <0.001 |
| Secondary, Vocational | Higher | ||||
|---|---|---|---|---|---|
| Stress Management Strategies | Median | 25–75% IQR | Median | 25–75% IQR | p-Value |
| Active coping | 1.50 | (1–2) | 2.00 | (1.75–2.5) | <0.001 |
| Planning | 1.00 | (0–2) | 2.00 | (2–2.25) | <0.001 |
| Positive re-evaluation and development | 1.00 | (0–2) | 1.50 | (0.75–2.5) | <0.001 |
| Acceptance | 2.50 | (2–3) | 2.25 | (1.5–2.75) | <0.001 |
| Joking | 0.75 | (0.5–1) | 1.25 | (0.25–2) | 0.07 |
| Turning to religion | 0.75 | (0–1.5) | 2.00 | (1.5–2.5) | <0.001 |
| Search for emotional support | 2.00 | (2–2) | 1.75 | (1.25–2) | <0.001 |
| Search for instrumental support | 2.50 | (2–3) | 2.00 | (1.75–2) | <0.001 |
| Distraction | 2.50 | (2–3) | 1.75 | (1.25–2.5) | <0.001 |
| Denial | 1.25 | (1–1.5) | 0.75 | (0.25–1.5) | <0.001 |
| Focus on emotions and emotional release | 2.50 | (2–3) | 1.75 | (1.25–2.5) | <0.001 |
| Consumption of alcohol or other psychoactive substances | 0.00 | (0–0) | 0.00 | (0–1.5) | <0.001 |
| Discontinuation of activity | 1.50 | (1.5–1.5) | 1.25 | (1–1.75) | <0.001 |
| Blaming oneself | 1.50 | (1.5–1.5) | 1.00 | (0.75–1.25) | <0.001 |
| Full-Time Worker | Unemployed | ||||
|---|---|---|---|---|---|
| Stress Management Strategies | Median | 25–75% IQR | Median | 25–75% IQR | p-Value |
| Active coping | 2.00 | (1.75–2.5) | 1.50 | (1–2) | <0.001 |
| Planning | 2.00 | (2–2.25) | 1.00 | (0–2) | <0.001 |
| Positive re-evaluation and development | 2.00 | (1.25–2.50) | 0.50 | (0–1) | <0.001 |
| Acceptance | 2.25 | (1.5–2.75) | 2.50 | (2–3) | <0.001 |
| Joking | 1.25 | (0.25–2) | 0.75 | (0.5–1) | 0.07 |
| Turning to religion | 1.75 | (1.25–2.5) | 1.00 | (0–2) | <0.001 |
| Search for emotional support | 1.75 | (1.25–2) | 2.00 | (2–2) | <0.001 |
| Search for instrumental support | 2.00 | (1.75–2) | 2.50 | (2–3) | <0.001 |
| Distraction | 2.00 | (1.5–2.5) | 2.25 | (1.5–3) | 0.07 |
| Denial | 1.00 | (0.25–1.75) | 1.00 | (1–1) | 1.0 |
| Focus on emotions and emotional release | 2.00 | (1.5–2.5) | 2.25 | (1.5–3) | 0.07 |
| Consumption of alcohol or other psychoactive substances | 0.00 | (0–15) | 0.00 | (0–0) | <0.001 |
| Discontinuation of activity | 1.50 | (1.25–1.75) | 1.25 | (1–1.5) | <0.001 |
| Blaming oneself | 1.00 | (0.75–1.25) | 1.50 | (1.5–1.5) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olejniczak, D.; Mularczyk-Tomczewska, P.; Klimiuk, K.; Olearczyk, A.; Kielan, A.; Staniszewska, A.; Osowiecka, K. Coping with Stress in Neoplastic Diseases. Int. J. Environ. Res. Public Health 2022, 19, 9675. https://doi.org/10.3390/ijerph19159675
Olejniczak D, Mularczyk-Tomczewska P, Klimiuk K, Olearczyk A, Kielan A, Staniszewska A, Osowiecka K. Coping with Stress in Neoplastic Diseases. International Journal of Environmental Research and Public Health. 2022; 19(15):9675. https://doi.org/10.3390/ijerph19159675
Chicago/Turabian StyleOlejniczak, Dominik, Paulina Mularczyk-Tomczewska, Krzysztof Klimiuk, Agata Olearczyk, Aleksandra Kielan, Anna Staniszewska, and Karolina Osowiecka. 2022. "Coping with Stress in Neoplastic Diseases" International Journal of Environmental Research and Public Health 19, no. 15: 9675. https://doi.org/10.3390/ijerph19159675
APA StyleOlejniczak, D., Mularczyk-Tomczewska, P., Klimiuk, K., Olearczyk, A., Kielan, A., Staniszewska, A., & Osowiecka, K. (2022). Coping with Stress in Neoplastic Diseases. International Journal of Environmental Research and Public Health, 19(15), 9675. https://doi.org/10.3390/ijerph19159675






