Perspectives of Nursing Students towards Schizophrenia Stigma: A Qualitative Study Protocol
Abstract
:1. Introduction
2. Theoretical Framework
3. Aims
4. Methods and Analysis
4.1. Study Design and Setting
4.2. Participants, and Recruitment
4.3. Sampling
4.4. Sample Size
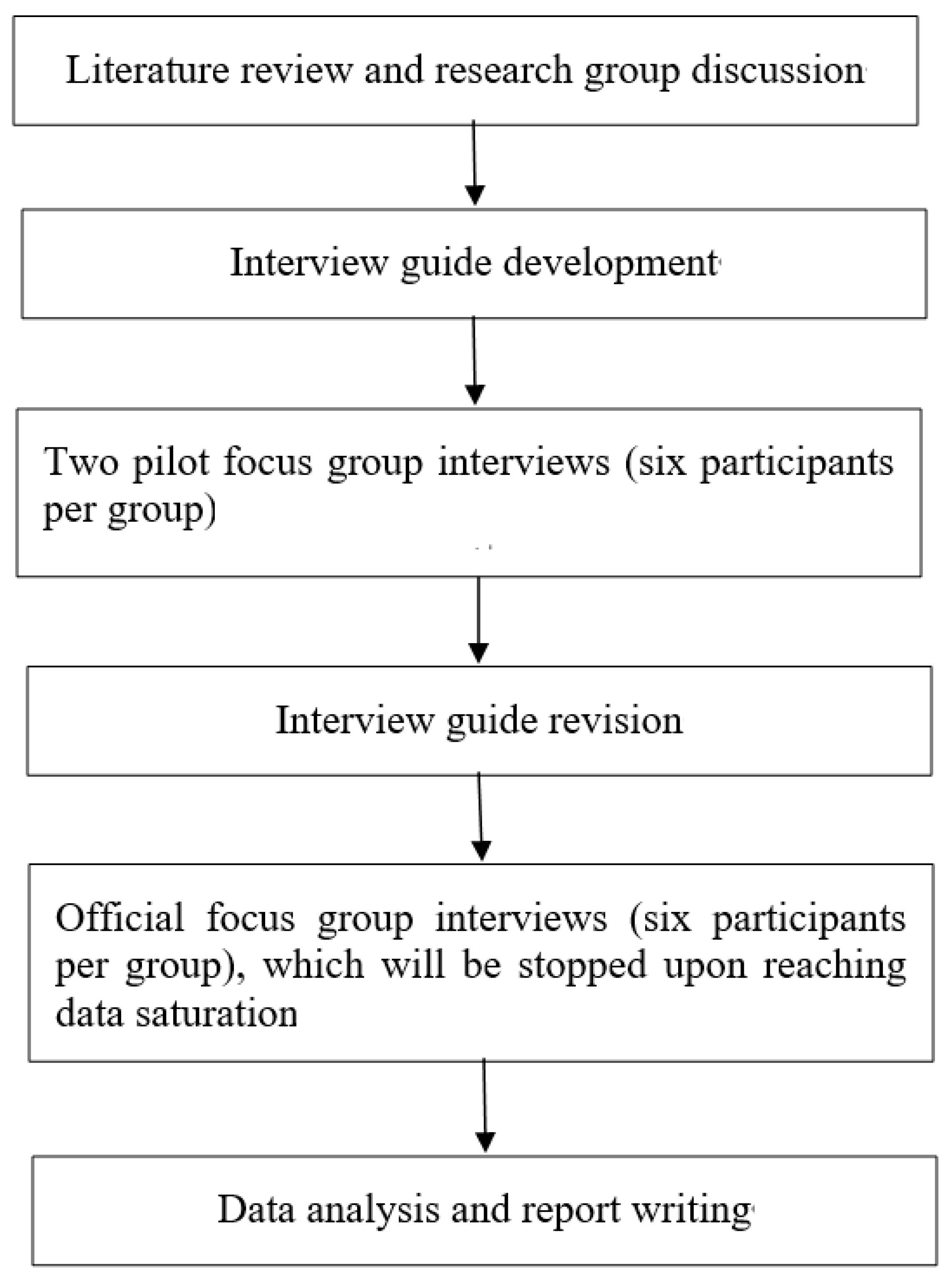
4.5. Data Collection
4.6. Data Analysis
4.6.1. Descriptive Statistics
4.6.2. Qualitative Content Analysis
4.7. Issues of Data Trustworthiness
4.8. Ethical Issues and Data Safety
5. Discussion
6. Limitations and Strengths
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Mental Disorders. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 20 May 2022).
- Corrigan, P.W.; Kerr, A.; Knudsen, L. The stigma of mental illness: Explanatory models and methods for change. Appl. Prev. Psychol. 2005, 11, 179–190. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Medina, T.R.; Martin, J.K.; Long, J.S. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated With Mental Illness. Am. J. Public Health 2013, 103, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, E.P.M. Social stigma is an underestimated contributing factor to unemployment in people with mental illness or mental health issues: Position paper and future directions. BMC Psychol. 2020, 8, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittchen, H.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [Green Version]
- Whitley, R.; Campbell, R.D. Stigma, agency and recovery amongst people with severe mental illness. Soc. Sci. Med. 2014, 107, 1–8. [Google Scholar] [CrossRef]
- WHO. Helping People with Severe Mental Disorders Live Longer and Healthier Lives. 2017. Available online: https://apps.who.int/iris/bitstream/handle/10665/259575/WHO-MSD-MER-17.7-eng.pdf (accessed on 20 May 2022).
- Angermeyer, M.C.; Dietrich, S. Public beliefs about and attitudes towards people with mental illness: A review of population studies. Acta Psychiatr. Scand. 2006, 113, 163–179. [Google Scholar] [CrossRef]
- Jorm, A.F.; Reavley, N.; Ross, A.M. Belief in the dangerousness of people with mental disorders: A review. Aust. N. Z. J. Psychiatry 2012, 46, 1029–1045. [Google Scholar] [CrossRef]
- Valery, K.-M.; Prouteau, A. Schizophrenia stigma in mental health professionals and associated factors: A systematic review. Psychiatry Res. 2020, 290, 113068. [Google Scholar] [CrossRef]
- WHO. Schizophrenia. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/schizophrenia (accessed on 20 May 2022).
- Huang, Y.; Wang, Y.; Wang, H. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry 2019, 6, 211–224. [Google Scholar] [CrossRef]
- Dong, W.; Liu, Y.; Sun, J.; Liu, Y.; Sun, Z.; Bai, R. Temporal Trends in the Incidence and Disability Adjusted Life Years of Schizophrenia in China Over 30 Years. Front. Psychiatry 2022, 13, 831188. [Google Scholar] [CrossRef]
- Zhai, Z. Population Opportunities and Challenges for High-Quality Development in the New Era|Interpretation of the Seventh National Census Communique. Available online: http://www.stats.gov.cn/tjsj/sjjd/202105/t20210512_1817336.html (accessed on 12 May 2021).
- He, H.R.; Liu, Q.Q.; Li, N.; Guo, L.Y.; Gao, F.J.; Bai, L.; Gao, F.; Lyu, J. Trends in the incidence and DALYs of schizophrenia at the global, regional and national levels: Results from the Global Burden of Disease Study 2017. Epidemiol. Psychiatr. Sci. 2021, 30, 30. [Google Scholar] [CrossRef]
- Koschorke, M.; Padmavati, R.; Kumar, S.; Cohen, A.; Weiss, H.A.; Chatterjee, S.; Pereira, J.; Naik, S.; John, S.; Dabholkar, H.; et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc. Sci. Med. 2014, 123, 149–159. [Google Scholar] [CrossRef] [Green Version]
- Sharac, J.; Mccrone, P.; Clement, S.; Thornicroft, G. The economic impact of mental health stigma and discrimination: A systematic review. Epidemiol. E Psichiatr. Soc.-Int. J. Epidemiol. Psychiatr. Sci. 2010, 19, 223–232. [Google Scholar] [CrossRef]
- Lee, S.; Lee, M.T.Y.; Chiu, M.Y.L.; Kleinman, A. Experience of social stigma by people with schizophrenia in Hong Kong. Br. J. Psychiatry 2005, 186, 153–157. [Google Scholar] [CrossRef] [Green Version]
- Leamy, M.; Bird, V.; Le Boutillier, C.; Williams, J.; Slade, M. Conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. Br. J. Psychiatry 2011, 199, 445–452. [Google Scholar] [CrossRef] [Green Version]
- Vass, V.; Sitko, K.; West, S.; Bentall, R.P. How stigma gets under the skin: The role of stigma, self-stigma and self-esteem in subjective recovery from psychosis. Psychosis 2017, 9, 235–244. [Google Scholar] [CrossRef]
- Caqueo-Urízar, A.; Boyer, L.; Urzúa, A.; Williams, D.R. Self-stigma in patients with schizophrenia: A multicentric study from three Latin-America countries. Soc. Psychiatry 2019, 54, 905–909. [Google Scholar] [CrossRef]
- Cai, C.F.; Yu, L.P. Quality of Life in Patients With Schizophrenia in China Relationships Among Demographic Characteristics, Psychosocial Variables, and Symptom Severity. J. Psychosoc. Nurs. Ment. Health Serv. 2017, 55, 48–54. [Google Scholar] [CrossRef]
- Wang, X.Q.; Petrini, M.A.; Morisky, N.E. Predictors of quality of life among Chinese people with schizophrenia. Nurs. Health Sci. 2016, 19, 142–148. [Google Scholar] [CrossRef]
- Maharjan, S.; Panthee, B. Prevalence of self-stigma and its association with self-esteem among psychiatric patients in a Nepalese teaching hospital: A cross-sectional study. BMC Psychiatry 2019, 19, 347. [Google Scholar] [CrossRef] [Green Version]
- Corrigan, P.W.; Druss, B.G.; Perlick, D.A. The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychol. Sci. Public Interes 2014, 15, 37–70. [Google Scholar] [CrossRef] [Green Version]
- Gerlinger, G.; Hauser, M.; De Hert, M.; Lacluyse, K.; Wampers, M.; Correll, C.U. Personal stigma in schizophrenia spectrum disorders: A systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry 2013, 12, 155–164. [Google Scholar] [CrossRef]
- Kleintjes, S.; Lund, C.; Flisher, A. A situational analysis of child and adolescent mental health services in Ghana, Uganda, South Africa and Zambia. Afr. J. Psychiatry 2010, 13, 132–139. [Google Scholar] [CrossRef] [Green Version]
- Lysaker, P.H.; Tsai, J.; Yanos, P.; Roe, D. Associations of multiple domains of self-esteem with four dimensions of stigma in schizophrenia. Schizophr. Res. 2008, 98, 194–200. [Google Scholar] [CrossRef] [Green Version]
- Lysaker, P.H.; Vohs, J.L.; Tsai, J. Negative symptoms and concordant impairments in attention in schizophrenia: Associations with social functioning, hope, self-esteem and internalized stigma. Schizophr. Res. 2009, 110, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Sharaf, A.Y.; Ossman, L.H.; Lachine, O.A. A cross-sectional study of the relationships between illness insight, internalized stigma, and suicide risk in individuals with schizophrenia. Int. J. Nurs. Stud. 2012, 49, 1512–1520. [Google Scholar] [CrossRef] [PubMed]
- Halter, M.J. Perceived Characteristics of Psychiatric Nurses: Stigma by Association. Arch. Psychiatr. Nurs. 2008, 22, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Henderson, C.; Noblett, J.; Parke, H.; Clement, S.; Caffrey, A.; Gale-Grant, O.; Schulze, B.; Druss, B.; Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 2014, 1, 467–482. [Google Scholar] [CrossRef]
- Samari, E.; Seow, E.; Chua, B.Y.; Ong, H.L.; Lau, Y.W.; Mahendran, R.; Verma, S.K.; Xie, H.; Wang, J.; Chong, S.A.; et al. Attitudes towards psychiatry amongst medical and nursing students in Singapore. BMC Med. Educ. 2019, 19, 91. [Google Scholar] [CrossRef]
- Geng, X. Investigation of Mental Health Related Attitude among Nursing Students: Description and Influential Factors. Chin. J. Nurs. 2015, 50, 1217–1221. [Google Scholar]
- Pan, S.M.; Zhou, Y.; Luo, X.J.; Feng, W.S.; Lu, C.J.; Lin, W.Q.; Yan, X.S.; Zhang, H.; Zhang, Y.X. Reliability and Validity of Chinese Version of Mental Illness: Clinician’s Attitudes Scale. Chin. J. Pract. Nurs. 2013, 29, 4–8. [Google Scholar]
- Fei, Y.; Li, F.F.; Geng, L. A Comparative Study on Mental Illness Attitudes between Psychiatric Clinical Nurses and Health School Nurse Students. Chin. J. Mod. Nurs. 2016, 22, 3201–3204. [Google Scholar]
- Liu, W. Recognition of, and beliefs about, causes of mental disorders: A cross-sectional study of US and Chinese undergraduate nursing students. Nurs. Health Sci. 2019, 21, 28–36. [Google Scholar] [CrossRef]
- Sánchez-Martínez, V.; Sales-Orts, R. Design and validation of a brief scale for cognitive evaluation in people with a diagnosis of schizophrenia (BCog-S). J. Psychiatr. Ment. Health Nurs. 2020, 27, 543–552. [Google Scholar] [CrossRef]
- Fekih-Romdhane, F.; Saidi, M.; Chaabane, M.A.; Cheour, M. Knowledge, attitude and behaviours toward people with mental illness among Tunisian nursing students and nonhealth care students: A cross-sectional study. Collegian 2022, 29, 500–509. [Google Scholar] [CrossRef]
- Chang, S.; Ong, H.L.; Seow, E.; Chua, B.Y.; Abdin, E.; Samari, E.; Teh, W.L.; Chong, S.A.; Subramaniam, M. Stigma towards mental illness among medical and nursing students in Singapore: A cross-sectional study. BMJ Open 2017, 7, e018099. [Google Scholar] [CrossRef] [Green Version]
- Palou, R.G.; Vigué, G.P.; Romeu-Labayen, M.; Tort-Nasarre, G. Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students. Int. J. Environ. Res. Public Health 2022, 19, 3213. [Google Scholar] [CrossRef]
- Fernandes, J.B.; Família, C.; Castro, C.; Simões, A. Stigma towards People with Mental Illness among Portuguese Nursing Students. J. Pers. Med. 2022, 12, 326. [Google Scholar] [CrossRef]
- Hawthorne, A.; Fagan, R.; Leaver, E.; Baxter, J.; Logan, P.; Snowden, A. Undergraduate nursing and midwifery student’s attitudes to mental illness. Nurs. Open 2020, 7, 1118–1128. [Google Scholar] [CrossRef] [Green Version]
- Shrivastava, A.; Johnston, M.; Bureau, Y. Stigma of Mental Illness-1: Clinical reflections. Mens Sana Monogr. 2012, 10, 70–84. [Google Scholar] [CrossRef] [Green Version]
- Ran, M.-S.; Hall, B.J.; Su, T.T.; Prawira, B.; Breth-Petersen, M.; Li, X.-H.; Zhang, T.-M. Stigma of mental illness and cultural factors in Pacific Rim region: A systematic review. BMC Psychiatry 2021, 21, 8. [Google Scholar] [CrossRef]
- Sideras, S.; McKenzie, G.; Noone, J.; Dieckmann, N.; Allen, T.L. Impact of a Simulation on Nursing Students’ Attitudes Toward Schizophrenia. Clin. Simul. Nurs. 2015, 11, 134–141. [Google Scholar] [CrossRef]
- Kim, H.; Sefcik, J.; Bradway, C. Characteristics of Qualitative Descriptive Studies: A Systematic Review. Res. Nurs. Health 2017, 40, 23–42. [Google Scholar] [CrossRef] [Green Version]
- Lincoln, Y.S.; Lynham, S.A.; Guba, E.G. Paradigmatic Controversies, Contradictions and Emerging Confluences. In The Sage Handbook of Qualitative Research; Denzin, N.K., Guba, Y.S., Eds.; Sage: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef]
- Ormston, R.; Spencer, L.; Barnard, M.; Snape, D. The foundations of qualitative research. In Qualitative Research Practice. A Guide for Social Science Students and Researchers; Ritchie, J., Lewis, J., McNaughton Nicholls, C., Ormston, R., Eds.; Sage: London, UK, 2014. [Google Scholar]
- Bradshaw, C.; Atkinson, S.; Doody, O. Employing a Qualitative Description Approach in Health Care Research. Glob. Qual. Nurs. Res. 2017, 4, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Riffel, T.; Chen, S.P. Exploring the Knowledge, Attitudes, and Behavioural Responses of Healthcare Students towards Mental Illnesses-A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 25. [Google Scholar] [CrossRef] [Green Version]
- Pederson, A.B.; Fokuo, J.K.; Thornicroft, G.; Bamgbose, O.; Ogunnubi, O.P.; Ogunsola, K.; Oshodi, Y.O. Perspectives of university health care students on mental health stigma in Nigeria: Qualitative analysis. Transcult. Psychiatry 2022, 1–14. [Google Scholar] [CrossRef]
- Samari, E.; Seow, E.; Chua, B.Y.; Ong, H.L.; Abdin, E.; Chong, S.A.; Subramaniam, M. Stigma towards people with mental disorders: Perspectives of nursing students. Arch. Psychiatr. Nurs. 2018, 32, 802–808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fokuo, J.K.; Goldrick, V.; Rossetti, J.; Wahlstrom, C.; Kocurek, C.; Larson, J.; Corrigan, P. Decreasing the Stigma of Mental Illness Through a Student-Nurse Mentoring Program: A Qualitative Study. Community Ment. Health J. 2017, 53, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rivas, M.E. Attitudes towards people with mental illness among medical students: A qualitative research. Psychol. Soc. Educ. 2021, 13, 21–33. [Google Scholar] [CrossRef]
- Yang, L.H.; Chen, F.-P.; Sia, K.J.; Lam, J.; Lam, K.; Ngo, H.; Lee, S.; Kleinman, A.; Good, B. “What matters most”: A cultural mechanism moderating structural vulnerability and moral experience of mental illness stigma. Soc. Sci. Med. 2014, 103, 84–93. [Google Scholar] [CrossRef]
- Yang, L.H.; Kleinman, A. ‘Face’ and the embodiment of stigma in China: The cases of schizophrenia and AIDS. Soc. Sci. Med. 2008, 67, 398–408. [Google Scholar] [CrossRef] [Green Version]
- Thornicroft, G. Tackling discrimination. Ment. Health Today 2006, 26–29. [Google Scholar]
- Thornicroft, G.; Rose, D.; Kassam, A.; Sartorius, N. Stigma: Ignorance, prejudice or discrimination? Br. J. Psychiatry 2007, 190, 192–193. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Penn, D.L. Lessons from social psychology on discrediting psychiatric stigma. Am. Psychol. 1999, 54, 765–776. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Kleinlein, P. The Impact of Mental Illness Stigma. In On the Stigma of Mental Illness: Practical Strategies for Research and Social Change; American Psychological Association: Washington, DC, USA, 2005. [Google Scholar]
- Batson, C.D. These things called empathy: Eight related but distinct phenomena. In The Social Neuroscience of Empathy; Decety, J., Ickes, W., Eds.; MIT Press: Cambridge, MA, USA, 2009. [Google Scholar]
- Pettigrew, T.F.; Tropp, L.R. How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. Eur. J. Soc. Psychol. 2008, 38, 922–934. [Google Scholar] [CrossRef]
- Webb, M.; Peterson, J.; Willis, S.C.; Rodney, H.; Siebert, E.; Carlile, J.A.; Stinar, L. The Role of Empathy and Adult Attachment in Predicting Stigma toward Severe and Persistent Mental Illness and other Psychosocial or Health Conditions. J. Ment. Health Couns. 2016, 38, 62–78. [Google Scholar] [CrossRef]
- Batson, C.D.; Polycarpou, M.P.; Harmon-Jones, E.; Imhoff, H.J.; Mitchener, E.C.; Bednar, L.L.; Klein, T.R.; Highberger, L. Empathy and attitudes: Can feeling for a member of a stigmatized group improve feelings toward the group? J. Personal. Soc. Psychol. 1997, 72, 105–118. [Google Scholar] [CrossRef]
- Naylor, P.B.; Cowie, H.; Walters, S.; Talamelli, L.; Dawkins, J. Impact of a mental health teaching programme on adolescents. Br. J. Psychiatry 2009, 194, 365–370. [Google Scholar] [CrossRef] [Green Version]
- Yang, L.H. Application of mental illness stigma theory to Chinese societies: Synthesis and new directions. Singap. Med. J. 2007, 48, 977–985. [Google Scholar]
- Yang, L.H.; Kleinman, A.; Link, B.G.; Phelan, J.C.; Lee, S.; Good, B. Culture and stigma: Adding moral experience to stigma theory. Soc. Sci. Med. 2007, 64, 1524–1535. [Google Scholar] [CrossRef] [PubMed]
- Ainlay, S.C.; Becker, G.; Coleman, L.M. The Dilemma of Difference: A Multidisciplinary View of Stigma (Perspectives in Social Psychology); Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Chen, S.N.; Zhong, W.; Zhang, J. Stigma and schizophrenia. Lancet 2009, 373, 1335. [Google Scholar] [CrossRef]
- Haddad, M.; Waqas, A.; Qayyum, W.; Shams, M.; Malik, S. The attitudes and beliefs of Pakistani medical practitioners about depression: A cross-sectional study in Lahore using the Revised Depression Attitude Questionnaire (R-DAQ). BMC Psychiatry 2016, 16, 349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haddad, M.; Waqas, A.; Sukhera, A.B.; Tarar, A.Z. The psychometric characteristics of the revised depression attitude questionnaire (R-DAQ) in Pakistani medical practitioners: A cross-sectional study of doctors in Lahore. BMC Res. Notes 2017, 10, 333. [Google Scholar] [CrossRef] [Green Version]
- Waqas, A.; Naveed, S.; Makhmoor, A.; Malik, A.; Hassan, H.; Aedma, K.K. Empathy, Experience and Cultural Beliefs Determine the Attitudes Towards Depression Among Pakistani Medical Students. Community Ment. Health J. 2020, 56, 65–74. [Google Scholar] [CrossRef]
- Waqas, A.; Zubair, M.; Ghulam, H.; Ullah, M.W.; Tariq, M.Z. Public stigma associated with mental illnesses in Pakistani university students: A cross sectional survey. PeerJ 2014, 2, e698. [Google Scholar] [CrossRef] [Green Version]
- Maunder, R.D.; White, F. Intergroup contact and mental health stigma: A comparative effectiveness meta-analysis. Clin. Psychol. Rev. 2019, 72, 101749. [Google Scholar] [CrossRef]
- Rabiee, F. Focus-group interview and data analysis. Proc. Nutr. Soc. 2004, 63, 655–660. [Google Scholar] [CrossRef]
- Campbell, M.; Fitzpatrick, R.; Haines, A.; Kinmonth, A.L.; Sandercock, P.; Spiegelhalter, D.; Tyrer, P. Framework for design and evaluation of complex interventions to improve health. BMJ 2000, 321, 694–696. [Google Scholar] [CrossRef] [Green Version]
- Holloway, I.; Galvin, K. Qualitative Research in Nursing and Healthcare; Wiley-Blackwell: Hoboken, NJ, USA, 2016. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Nyumba, T.O.; Wilson, K.; Derrick, C.J.; Mukherjee, N. The use of focus group discussion methodology: Insights from two decades of application in conservation. Methods Ecol. Evol. 2018, 9, 20–32. [Google Scholar] [CrossRef] [Green Version]
- Marshall, B.; Cardon, P.; Poddar, A.; Fontenot, R. Does Sample Size Matter in Qualitative Research?: A Review of Qualitative Interviews in is Research. J. Comput. Inf. Syst. 2013, 54, 11–22. [Google Scholar] [CrossRef]
- Lincoln, Y.S.; Guba, E. Naturalistic Inquiry; SAGE Publications: London, UK, 1985. [Google Scholar]
- Guest, G.; Namey, E.; Chen, M. A simple method to assess and report thematic saturation in qualitative research. PLoS ONE 2020, 15, e0232076. [Google Scholar] [CrossRef]
- Baker, S.E.; Edwards, R.; How Many Qualitative Interviews Is Enough? Expert Voices and Early Career Reflections on Sampling and Cases in Qualitative Research. National Centre for Research Methods Review Paper. 2012. Available online: http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf (accessed on 20 May 2022).
- Creswell, J.W. Qualitative Inquiry and Research Design: Choosing among Five Approaches; SAGE Publications, Inc.: London, UK, 2013. [Google Scholar]
- Renz, S.M.; Carrington, J.M.; Badger, T.A. Two Strategies for Qualitative Content Analysis: An Intramethod Approach to Triangulation. Qual. Health Res. 2018, 28, 824–831. [Google Scholar] [CrossRef]
- Thomas, D.R. A general inductive approach for analyzing qualitative evaluation data. Am. J. Eval. 2006, 27, 237–246. [Google Scholar] [CrossRef]
- Assarroudi, A.; Heshmati Nabavi, F.; Armat, M.R.; Ebadi, A.; Vaismoradi, M. Directed qualitative content analysis: The description and elaboration of its underpinning methods and data analysis process. J. Res. Nurs. 2018, 23, 42–55. [Google Scholar] [CrossRef] [Green Version]
- Kleinheksel, A.J.; Rockich-Winston, N.; Tawfik, H.; Wyatt, T.R. Demystifying Content Analysis. Am. J. Pharm. Educ. 2020, 84, 127–137. [Google Scholar] [CrossRef]
- Bengtsson, M. How to plan and perform a qualitative study using content analysis. NursingPlus Open 2016, 2, 8–14. [Google Scholar] [CrossRef] [Green Version]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Gibbs, G.R. Analyzing Qualitative Data (Qualitative Research Kit); SAGE Publications Ltd.: London, UK, 2018. [Google Scholar]
- Lincoln, Y.S.; Guba, E.G. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir. Program Eval. 1986, 1986, 73–84. [Google Scholar] [CrossRef]
- Chen, H.-Y.; Boore, J.R. Translation and back-translation in qualitative nursing research: Methodological review. J. Clin. Nurs. 2010, 19, 234–239. [Google Scholar] [CrossRef]
- Anney, V.N. Ensuring the Quality of the Findings of Qualitative Research: Looking at Trustworthiness criteria. J. Emerg. Trends Educ. Res. Policy Stud. 2014, 5, 272–281. [Google Scholar]
- Elo, S.; Kääriäinen, M.; Kanste, O.; Pölkki, T.; Utriainen, K.; Kyngäs, H. Qualitative Content Analysis: A Focus on Trustworthiness. Sage Open 2014, 4, 2158244014522633. [Google Scholar] [CrossRef]
- Sim, J.; Waterfield, J. Focus group methodology: Some ethical challenges. Qual. Quant. 2019, 53, 3003–3022. [Google Scholar] [CrossRef] [Green Version]
- Lo, L.N. Teachers and teaching in China: A critical reflection. Teach. Teach. 2019, 25, 553–573. [Google Scholar] [CrossRef]
| 1. | What is your understanding of schizophrenia (SZ)? (Probe: causal factors, manifestation, prognosis; where did you obtain such information?) |
| 2. | What do you think about the life of people with SZ? (Probe: social support > intimate relationship > education > working) |
| 3. | What are your experiences of interacting with people with SZ or mental illness? (If no personal encounter, any story you have heard?) [When > what happened > who > what did you say > How do you feel]?. |
| 4. | How do you think Chinese people view schizophrenia compared to people from Western countries? |
| 5. | What do you think of the views of traditional Chinese culture and religion on schizophrenia? [How do Confucianism, Taoism, and Buddhism view and deal with schizophrenia > According to the idea of traditional Chinese culture and religion, what are the causes of schizophrenia and how to deal with it?] |
| 6. | How do you perceive the stigma often encountered by people with schizophrenia? |
| 7. | What do you think are the main factors causing the stigma of schizophrenia? |
| 8. | What do you think of caring for people with schizophrenia? |
| 9. | From your view, how could an intervention program be used to decrease the stigma of schizophrenia? |
| 10. | If you need to take part in a contact activity with people recovering from schizophrenia, what kind of activity will you recommend? |
| 11. | What do you think of becoming a mental health nurse? (What are the motivations and barriers?) |
| 12. | What are your suggestions to attract nursing students to work in the psychiatric department? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, X.; Su, J.; Bressington, D.T.; Li, Y.; Leung, S.F. Perspectives of Nursing Students towards Schizophrenia Stigma: A Qualitative Study Protocol. Int. J. Environ. Res. Public Health 2022, 19, 9574. https://doi.org/10.3390/ijerph19159574
Chen X, Su J, Bressington DT, Li Y, Leung SF. Perspectives of Nursing Students towards Schizophrenia Stigma: A Qualitative Study Protocol. International Journal of Environmental Research and Public Health. 2022; 19(15):9574. https://doi.org/10.3390/ijerph19159574
Chicago/Turabian StyleChen, Xi, Jingjing Su, Daniel Thomas Bressington, Yan Li, and Sau Fong Leung. 2022. "Perspectives of Nursing Students towards Schizophrenia Stigma: A Qualitative Study Protocol" International Journal of Environmental Research and Public Health 19, no. 15: 9574. https://doi.org/10.3390/ijerph19159574
APA StyleChen, X., Su, J., Bressington, D. T., Li, Y., & Leung, S. F. (2022). Perspectives of Nursing Students towards Schizophrenia Stigma: A Qualitative Study Protocol. International Journal of Environmental Research and Public Health, 19(15), 9574. https://doi.org/10.3390/ijerph19159574









