Resource-Strengthening Training for Parents of Adolescents with Problematic Gaming (Res@t-P): A Clinical Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
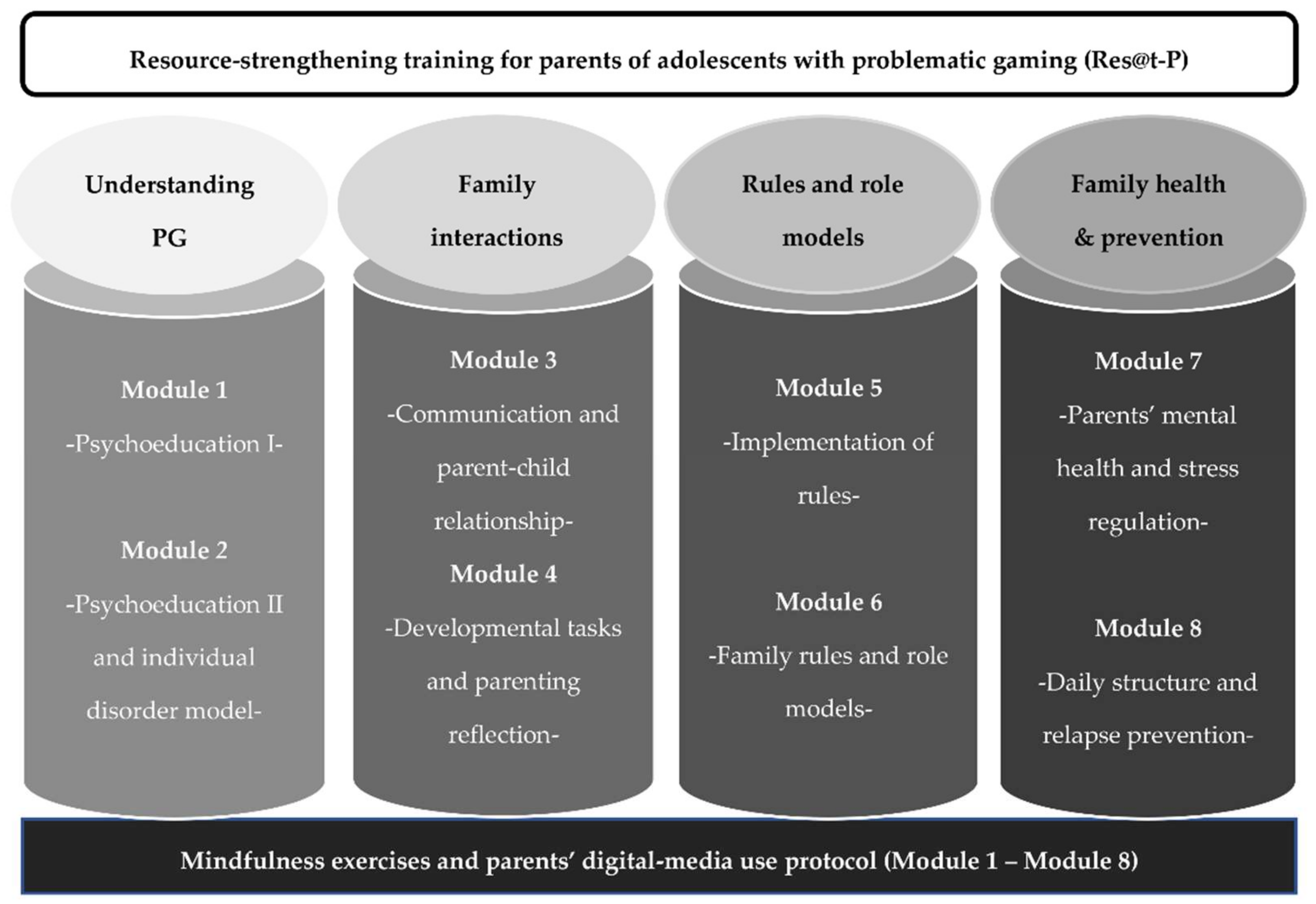
2.1. Res@t-P
2.2. Participants and Procedure
2.3. Measures
2.3.1. Psychological Factors
2.3.2. Parenting Factors
2.3.3. Family Factors
2.3.4. Adolescent PG
2.4. Statistical Analysis
2.4.1. Data Management
2.4.2. Conditional Growth Models
3. Results
3.1. Sample Characteristics
3.2. Psychological Factors
3.3. Parenting Factors
3.4. Family Factors
3.5. Adolescent PG
| Predictors | IRR | CI | p | t(df) | |
|---|---|---|---|---|---|
| Psychological factor | |||||
| (Intercept) | 0.52 | 0.23–1.19 | 0.122 | −1.56 (87) | |
| Week | 0.96 | 0.93–0.99 | 0.009 | −2.66 (87) | |
| PSS-4 | Covariates | ||||
| Attended sessions | 1.15 | 1.01–1.31 | 0.036 | 2.13 (87) | |
| BSI-18 | 1.44 | 1.15–1.81 | 0.002 | 3.25 (87) | |
| R2marg = 0.220 | R2cond = 0.701 | ||||
| Parental factors | |||||
| (Intercept) | 1.13 | 0.48–2.67 | 0.775 | 0.29 (94) | |
| Week | 1.02 | 1.00–1.04 | 0.083 | 1.75 (94) | |
| FSW | Covariates | ||||
| Attended sessions | 0.96 | 0.84–1.10 | 0.575 | −0.56 (94) | |
| BSI-18 | 0.76 | 0.59–0.98 | 0.036 | −2.13 (94) | |
| R2marg = 0.085 | R2cond = 0.633 | ||||
| (Intercept) | 0.41 | 0.16–1.05 | 0.064 | −1.87 (91) | |
| Week | 1.03 | 1.01–1.05 | 0.004 | 2.92 (91) | |
| MR-6 | Covariates | ||||
| Attended sessions | 1.12 | 0.97–1.30 | 0.128 | 1.54 (91) | |
| BSI-18 | 1.12 | 0.85–1.47 | 0.413 | 0.82 (91) | |
| R2marg = 0.094 | R2cond = 0.690 | ||||
| Family factors | |||||
| (Intercept) | 0.79 | 0.33–1.87 | 0.588 | −0.54 (94) | |
| Week | 1.04 | 1.01–1.06 | <0.001 | 3.40 (94) | |
| FCS | Covariates | ||||
| Attended sessions | 1.00 | 0.87–1.14 | 0.983 | −0.02 (94) | |
| BSI-18 | 0.78 | 0.60–1.01 | 0.059 | −1.91 (94) | |
| R2marg = 0.099 | R2cond = 0.722 | ||||
| (Intercept) | 0.76 | 0.33–1.76 | 0.518 | −0.65 (93) | |
| Week | 1.03 | 1.00–1.06 | 0.031 | 2.19 (93) | |
| FB-K | Covariates | ||||
| Attended sessions | 1.00 | 0.88–1.15 | 0.956 | 0.06 (93) | |
| BSI-18 | 0.91 | 0.71–1.17 | 0.473 | −0.72 (93) | |
| R2marg = 0.040 | R2cond = 0.627 | ||||
| Adolescent PG | |||||
| (Intercept) | 4.89 | 2.46–9.71 | <0.001 | 4.60 (89) | |
| Week | 0.97 | 0.95–0.99 | 0.009 | −2.69 (89) | |
| PIGDS | Covariates | ||||
| Attended sessions | 0.81 | 0.73–0.90 | <0.001 | −3.88 (89) | |
| BSI-18 | 1.13 | 0.91–1.40 | 0.273 | 1.10 (89) | |
| R2marg = 0.137 | R2cond = 0.875 | ||||

4. Discussion
4.1. Parental Psychological Stress
4.2. Parenting Factors
4.2.1. Parental Self-Efficacy
4.2.2. Media Rules
4.3. Family Factors
4.4. Adolescent PG Symptoms
4.5. Closing a Gap and Outlook
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feierabend, S.; Rathgeb, T.; Kheredmand, H.; Glöckler, S. JIM-Studie 2021 Medien-Basisstudie zum Medienumgang 12- bis 19-Jähriger in Deutschland; Medienpädagogischer Forschungsverbund Südwest (mpfs), Ed.; Medienpädagogischer Forschungsverbund Südwest: Stuttgart, Germany, 2021. [Google Scholar]
- Paschke, K.; Austermann, M.I.; Simon-Kutscher, K.; Thomasius, R. Adolescent Gaming and Social Media Usage before and during the COVID-19 Pandemic: Interim Results of a Longitudinal Study. SUCHT 2021, 67, 13–22. [Google Scholar] [CrossRef]
- Paschke, K.; Holtmann, M.; Melchers, P.; Klein, M.; Schimansky, G.; Krömer, T.; Reis, O.; Wartberg, L.; Thomasius, R. Media-associated disorders in childhood and adolescence: Evidence paper of the joint addiction commision of the German societies and professional associations of child and adolescent psychiatry and psychotherapy. Z Kinder Jugendpsychiatr. Psychother. 2020, 48, 303–317. [Google Scholar] [CrossRef]
- Paulus, F.W.; Ohmann, S.; von Gontard, A.; Popow, C. Internet Gaming Disorder in Children and Adolescents: A Systematic Review. Dev. Med. Child Neurol. 2018, 60, 645–659. [Google Scholar] [CrossRef]
- Cho, D.J.; Kim, H.T.; Lee, J.; Park, S.H. Economic Cost-Benefit Analysis of the Addictive Digital Game Industry. Appl. Econ. Lett. 2018, 25, 638–642. [Google Scholar] [CrossRef]
- Stevens, M.W.; Dorstyn, D.; Delfabbro, P.H.; King, D.L. Global Prevalence of Gaming Disorder: A Systematic Review and Meta-Analysis. Aust. N. Z. J. Psychiatry 2021, 55, 553–568. [Google Scholar] [CrossRef]
- Kim, H.S.; Son, G.; Roh, E.-B.; Ahn, W.-Y.; Kim, J.; Shin, S.-H.; Chey, J.; Choi, K.-H. Prevalence of Gaming Disorder: A Meta-Analysis. Addict. Behav. 2022, 126, 107183. [Google Scholar] [CrossRef]
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-554-1. [Google Scholar]
- ICD-11 for Mortality and Morbidity Statistics. Available online: https://icd.who.int/browse11/l-m/en (accessed on 13 March 2022).
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A). J. Clin. Med. 2020, 9, 993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montag, C.; Schivinski, B.; Sariyska, R.; Kannen, C.; Demetrovics, Z.; Pontes, H.M. Psychopathological Symptoms and Gaming Motives in Disordered Gaming-A Psychometric Comparison between the WHO and APA Diagnostic Frameworks. J. Clin. Med. 2019, 8, 1691. [Google Scholar] [CrossRef] [Green Version]
- King, D.L.; Chamberlain, S.R.; Carragher, N.; Billieux, J.; Stein, D.; Mueller, K.; Potenza, M.N.; Rumpf, H.J.; Saunders, J.; Starcevic, V.; et al. Screening and Assessment Tools for Gaming Disorder: A Comprehensive Systematic Review. Clin. Psychol. Rev. 2020, 77, 101831. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.-H.; Lin, H.-C.; Lin, P.-C.; Yen, J.-Y. Validity, Functional Impairment and Complications Related to Internet Gaming Disorder in the DSM-5 and Gaming Disorder in the ICD-11. Aust. N. Z. J. Psychiatry 2020, 54, 707–718. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.S.; Bhang, S.Y.; Choi, J.S.; Lee, H.K.; Lee, S.Y.; Kweon, Y.-S. Clinical Characteristics of Diagnosis for Internet Gaming Disorder: Comparison of DSM-5 IGD and ICD-11 GD Diagnosis. J. Clin. Med. 2019, 8, 945. [Google Scholar] [CrossRef] [Green Version]
- Schettler, L.; Thomasius, R.; Paschke, K. Neural Correlates of Problematic Gaming in Adolescents: A Systematic Review of Structural and Functional Magnetic Resonance Imaging Studies. Addict. Biol. 2021, 27, e13093. [Google Scholar] [CrossRef]
- Sugaya, N.; Shirasaka, T.; Takahashi, K.; Kanda, H. Bio-Psychosocial Factors of Children and Adolescents with Internet Gaming Disorder: A Systematic Review. BioPsychoSocial Med. 2019, 13, 3. [Google Scholar] [CrossRef]
- Nielsen, P.; Favez, N.; Rigter, H. Parental and Family Factors Associated with Problematic Gaming and Problematic Internet Use in Adolescents: A Systematic Literature Review. Curr. Addict. Rep. 2020, 7, 365–386. [Google Scholar] [CrossRef]
- Colasante, E.; Pivetta, E.; Canale, N.; Vieno, A.; Marino, C.; Lenzi, M.; Benedetti, E.; King, D.L.; Molinaro, S. Problematic Gaming Risk among European Adolescents: A Cross-national Evaluation of Individual and Socio-economic Factors. Addiction 2022, 117, 2273–2282. [Google Scholar] [CrossRef]
- Taechoyotin, P.; Tongrod, P.; Thaweerungruangkul, T.; Towattananon, N.; Teekapakvisit, P.; Aksornpusitpong, C.; Sathapornpunya, W.; Hempatawee, N.; Rangsin, R.; Mungthin, M.; et al. Prevalence and Associated Factors of Internet Gaming Disorder among Secondary School Students in Rural Community, Thailand: A Cross-Sectional Study. BMC Res. Notes 2020, 13, 11. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Jiang, X.; Mo, P.K.; Cai, Y.; Ma, L.; Lau, J.T. Prevalence and Interpersonal Correlates of Internet Gaming Disorders among Chinese Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 579. [Google Scholar] [CrossRef] [Green Version]
- Wartberg, L.; Kriston, L.; Kramer, M.; Schwedler, A.; Lincoln, T.M.; Kammerl, R. Internet Gaming Disorder in Early Adolescence: Associations with Parental and Adolescent Mental Health. Eur. Psychiatr. 2017, 43, 14–18. [Google Scholar] [CrossRef]
- Koning, I.M.; Peeters, M.; Finkenauer, C.; van den Eijnden, R. Bidirectional Effects of Internet-Specific Parenting Practices and Compulsive Social Media and Internet Game Use. J. Behav. Addict. 2018, 7, 624–632. [Google Scholar] [CrossRef]
- Schneider, L.A.; King, D.L.; Delfabbro, P.H. Family Factors in Adolescent Problematic Internet Gaming: A Systematic Review. J. Behav. Addict. 2017, 6, 321–333. [Google Scholar] [CrossRef] [Green Version]
- Park, S.Y.; Kim, S.M.; Roh, S.; Soh, M.-A.; Lee, S.H.; Kim, H.; Lee, Y.S.; Han, D.H. The Effects of a Virtual Reality Treatment Program for Online Gaming Addiction. Comput. Methods Programs Biomed. 2016, 129, 99–108. [Google Scholar] [CrossRef]
- Stevens, M.W.R.; King, D.L.; Dorstyn, D.; Delfabbro, P.H. Cognitive-Behavioral Therapy for Internet Gaming Disorder: A Systematic Review and Meta-analysis. Clin. Psychol. Psychother. 2019, 26, 191–203. [Google Scholar] [CrossRef]
- Zajac, K.; Ginley, M.K.; Chang, R. Treatments of Internet Gaming Disorder: A Systematic Review of the Evidence. Expert Rev. Neurother. 2020, 20, 85–93. [Google Scholar] [CrossRef]
- Lampropoulou, P.; Siomos, K.; Floros, G.; Christodoulou, N. Effectiveness of Available Treatments for Gaming Disorders in Children and Adolescents: A Systematic Review. Cyberpsychol. Behav. Soc. Netw. 2022, 25, 5–13. [Google Scholar] [CrossRef]
- Torres-Rodríguez, A.; Griffiths, M.D.; Carbonell, X.; Oberst, U. Treatment Efficacy of a Specialized Psychotherapy Program for Internet Gaming Disorder. J. Behav. Addict. 2018, 7, 939–952. [Google Scholar] [CrossRef]
- González-Bueso, V.; Santamaría, J.J.; Fernández, D.; Merino, L.; Montero, E.; Jiménez-Murcia, S.; del Pino-Gutiérrez, A.; Ribas, J. Internet Gaming Disorder in Adolescents: Personality, Psychopathology and Evaluation of a Psychological Intervention Combined with Parent Psychoeducation. Front. Psychol. 2018, 9, 787. [Google Scholar] [CrossRef]
- Nielsen, P.; Christensen, M.; Henderson, C.; Liddle, H.A.; Croquette-Krokar, M.; Favez, N.; Rigter, H. Multidimensional Family Therapy Reduces Problematic Gaming in Adolescents: A Randomised Controlled Trial. J. Behav. Addict. 2021, 10, 234–243. [Google Scholar] [CrossRef]
- Chang, C.-H.; Chang, Y.-C.; Yang, L.; Tzang, R.-F. The Comparative Efficacy of Treatments for Children and Young Adults with Internet Addiction/Internet Gaming Disorder: An Updated Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2612. [Google Scholar] [CrossRef] [PubMed]
- Bonnaire, C.; Phan, O. Relationships between Parental Attitudes, Family Functioning and Internet Gaming Disorder in Adolescents Attending School. Psychiatry Res. 2017, 255, 104–110. [Google Scholar] [CrossRef]
- Wendt, L.M.; Austermann, M.I.; Rumpf, H.-J.; Thomasius, R.; Paschke, K. Requirements of a Group Intervention for Adolescents with Internet Gaming Disorder in a Clinical Setting: A Qualitative Interview Study. Int. J. Environ. Res. Public Health 2021, 18, 7813. [Google Scholar] [CrossRef]
- Geurts, S.M.; Koning, I.M.; Vossen, H.G.M.; van den Eijnden, R.J.J.M. Rules, Role Models or Overall Climate at Home? Relative Associations of Different Family Aspects with Adolescents’ Problematic Social Media Use. Compr. Psychiatry 2022, 116, 152318. [Google Scholar] [CrossRef] [PubMed]
- Donati, M.A.; Guido, C.A.; De Meo, G.; Spalice, A.; Sanson, F.; Beccari, C.; Primi, C. Gaming among Children and Adolescents during the COVID-19 Lockdown: The Role of Parents in Time Spent on Video Games and Gaming Disorder Symptoms. Int. J. Environ. Res. Public Health 2021, 18, 6642. [Google Scholar] [CrossRef] [PubMed]
- Brandhorst, I.; Renner, T.; Barth, G.M. Elternfaktoren Bei Internet- Und Computerspielsucht Im Jugendalter: Eine Übersicht. Z. Für Kinder-Jugendpsychiatr. Psychother. 2022, 50, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Bonnaire, C.; Liddle, H.A.; Har, A.; Nielsen, P.; Phan, O. Why and How to Include Parents in the Treatment of Adolescents Presenting Internet Gaming Disorder? J. Behav. Addict. 2019, 8, 201–212. [Google Scholar] [CrossRef]
- Lee, E.-H. Review of the Psychometric Evidence of the Perceived Stress Scale. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2012, 6, 121–127. [Google Scholar] [CrossRef] [Green Version]
- Vallejo, M.A.; Vallejo-Slocker, L.; Fernández-Abascal, E.G.; Mañanes, G. Determining Factors for Stress Perception Assessed with the Perceived Stress Scale (PSS-4) in Spanish and Other European Samples. Front. Psychol. 2018, 9, 37. [Google Scholar] [CrossRef]
- Harrer, M.; Adam, S.H.; Baumeister, H.; Cuijpers, P.; Karyotaki, E.; Auerbach, R.P.; Kessler, R.C.; Bruffaerts, R.; Berking, M.; Ebert, D.D. Internet Interventions for Mental Health in University Students: A Systematic Review and Meta-Analysis. Int. J. Methods Psychiatr. Res. 2019, 28, e1759. [Google Scholar] [CrossRef] [Green Version]
- Franke, G.H.; Jaeger, S.; Glaesmer, H.; Barkmann, C.; Petrowski, K.; Braehler, E. Psychometric Analysis of the Brief Symptom Inventory 18 (BSI-18) in a Representative German Sample. BMC Med. Res. Methodol. 2017, 17, 14. [Google Scholar] [CrossRef] [Green Version]
- Derogatis, L.R. Brief Symptom Inventory 18 Administration, Scoring, and Procedures Manual; Springer: Berlin/Heidelberg, Germany, 2000. [Google Scholar]
- Kliem, S.; Kessemeier, Y.; Heinrichs, N.; Döpfner, M.; Hahlweg, K. Der Fragebogen Zur Selbstwirksamkeit in Der Erziehung (FSW). Diagnostica 2014, 60, 35–45. [Google Scholar] [CrossRef]
- DAK-Gesundheit. DAK-Studie: Gaming, Social-Media & Corona [DAK Study: Gaming, Social Media & Corona]. Available online: https://www.dak.de/dak/gesundheit/dak-studie-gaming-social-media-und-corona-2295548.html#/ (accessed on 22 January 2021).
- Rivadeneira, J.; López, M.A. Family Communication Scale: Validation in Chilean. Acta Colomb. Psicol. 2017, 20, 127–137. [Google Scholar]
- Olson, D. FACES IV and the Circumplex Model: Validation Study. J. Marital. Fam. Ther. 2011, 37, 64–80. [Google Scholar] [CrossRef]
- Sidor, A.; Cierpka, M. The Family Questionnaire (FB-K)—A Short Version of the General Family Questionnaire and Its Reliability and Validity. Prax. Kinderpsychol. Kinderpsychiatr. 2016, 65, 40–56. [Google Scholar] [CrossRef]
- Wartberg, L.; Zieglmeier, M.; Kammerl, R. Accordance of Adolescent and Parental Ratings of Internet Gaming Disorder and Their Associations with Psychosocial Aspects. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 264–270. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.-Y. Statistical Notes for Clinical Researchers: Assessing Normal Distribution (2) Using Skewness and Kurtosis. Restor. Dent. Endod. 2013, 38, 52. [Google Scholar] [CrossRef]
- Curran, P.J.; Obeidat, K.; Losardo, D. Twelve Frequently Asked Questions About Growth Curve Modeling. J. Cogn. Dev. 2010, 11, 121–136. [Google Scholar] [CrossRef] [Green Version]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Softw. 2015, 67. [Google Scholar] [CrossRef]
- Gjoneska, B.; Potenza, M.N.; Jones, J.; Corazza, O.; Hall, N.; Sales, C.M.D.; Grünblatt, E.; Martinotti, G.; Burkauskas, J.; Werling, A.M.; et al. Problematic Use of the Internet during the COVID-19 Pandemic: Good Practices and Mental Health Recommendations. Compr. Psychiatry 2022, 112, 152279. [Google Scholar] [CrossRef]
- Dahl, V.; Ramakrishnan, A.; Spears, A.P.; Jorge, A.; Lu, J.; Bigio, N.A.; Chacko, A. Psychoeducation Interventions for Parents and Teachers of Children and Adolescents with ADHD: A Systematic Review of the Literature. J. Dev. Phys. Disabil. 2020, 32, 257–292. [Google Scholar] [CrossRef]
- Park, C.; Rosenblat, J.D.; Brietzke, E.; Pan, Z.; Lee, Y.; Cao, B.; Zuckerman, H.; Kalantarova, A.; McIntyre, R.S. Stress, Epigenetics and Depression: A Systematic Review. Neurosci. Biobehav. Rev. 2019, 102, 139–152. [Google Scholar] [CrossRef]
- Vismara, L.; Rollè, L.; Agostini, F.; Sechi, C.; Fenaroli, V.; Molgora, S.; Neri, E.; Prino, L.E.; Odorisio, F.; Trovato, A.; et al. Perinatal Parenting Stress, Anxiety, and Depression Outcomes in First-Time Mothers and Fathers: A 3- to 6-Months Postpartum Follow-Up Study. Front. Psychol. 2016, 7, 938. [Google Scholar] [CrossRef] [PubMed]
- Van Daele, T.; Hermans, D.; Van Audenhove, C.; Van den Bergh, O. Stress Reduction Through Psychoeducation: A Meta- Analytic Review. Health Educ. Behav. 2012, 39, 474–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to Reduce Stress in University Students: A Review and Meta-Analysis. J. Affect. Disord. 2013, 148, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.; Heerkens, Y.; Kuijer, W.; van der Heijden, B.; Engels, J. Effects of Mindfulness-Based Stress Reduction on Employees’ Mental Health: A Systematic Review. PLoS ONE 2018, 13, e0191332. [Google Scholar] [CrossRef]
- Pistrang, N.; Barker, C.; Humphreys, K. Mutual Help Groups for Mental Health Problems: A Review of Effectiveness Studies. Am. J. Community Psychol. 2008, 42, 110–121. [Google Scholar] [CrossRef] [Green Version]
- Ozbay, F.; Johnson, D.C.; Dimoulas, E.; Morgan, C.A.; Charney, D.; Southwick, S. Social Support and Resilience to Stress: From Neurobiology to Clinical Practice. Psychiatry 2007, 4, 35–40. [Google Scholar]
- Wang, M.; Saudino, K.J. Emotion Regulation and Stress. J. Adult Dev. 2011, 18, 95–103. [Google Scholar] [CrossRef]
- Cohen, J.I. Stress and Mental Health: A Behavioral Perspective. Issues Ment. Health Nurs. 2000, 21, 185–202. [Google Scholar] [CrossRef]
- Albanese, A.M.; Russo, G.R.; Geller, P.A. The Role of Parental Self-efficacy in Parent and Child Well-being: A Systematic Review of Associated Outcomes. Child Care Health Dev. 2019, 45, 333–363. [Google Scholar] [CrossRef]
- Hohlfeld, A.S.J.; Harty, M.; Engel, M.E. Parents of Children with Disabilities: A Systematic Review of Parenting Interventions and Self-Efficacy. Afr. J. Disabil. 2018, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Lee, E.J.; Kim, H.S. Gender Differences in Smartphone Addiction Behaviors Associated with Parent-Child Bonding, Parent-Child Communication, and Parental Mediation Among Korean Elementary School Students. J. Addict. Nurs. 2018, 29, 244–254. [Google Scholar] [CrossRef]
- Shin, W.; Huh, J. Parental Mediation of Teenagers’ Video Game Playing: Antecedents and Consequences. N. Media Soc. 2011, 13, 945–962. [Google Scholar] [CrossRef]
- Choo, H.; Sim, T.; Liau, A.; Gentile, D.; Khoo, A. Parental Influences on Pathological Symptoms of Video-Gaming Among Children and Adolescents: A Prospective Study. J. Child Fam. Stud. 2015, 24, 1429–1441. [Google Scholar] [CrossRef]
- McKay, M.; Davis, M.; Fanning, P. Messages: The Communication Skills Book; New Harbinger Publications: Oakland, CA, USA, 2009. [Google Scholar]
- Wiley, A.R. Connecting as a Couple: Communication Skills for Healthy Relationships. Forum Fam. Consum. Issues 2007, 12, 10. [Google Scholar]
- King, D.L.; Delfabbro, P.H. Features of Parent-Child Relationships in Adolescents with Internet Gaming Disorder. Int. J. Ment. Health Addict. 2017, 15, 1270–1283. [Google Scholar] [CrossRef]
- Wissow, L.S.; Gadomski, A.; Roter, D.; Larson, S.; Brown, J.; Zachary, C.; Bartlett, E.; Horn, I.; Luo, X.; Wang, M.-C. Improving Child and Parent Mental Health in Primary Care: A Cluster-Randomized Trial of Communication Skills Training. Pediatrics 2008, 121, 266–275. [Google Scholar] [CrossRef]
- Bender, P.K.; Kim, E.-L.; Gentile, D.A. Gaming Disorder in Children and Adolescents: Risk Factors and Preventive Approaches. Curr. Addict. Rep. 2020, 7, 553–560. [Google Scholar] [CrossRef]
- Zeng, X.; Lu, M.; Chen, M. The Relationship between Family Intimacy and Relapse Tendency among People Who Use Drugs: A Moderated Mediation Model. Subst. Abus. Treat. Prev. Policy 2021, 16, 48. [Google Scholar] [CrossRef]
- Li, W.; Garland, E.L.; Howard, M.O. Family Factors in Internet Addiction among Chinese Youth: A Review of English- and Chinese-Language Studies. Comput. Hum. Behav. 2014, 31, 393–411. [Google Scholar] [CrossRef]
- Lee, P.; Zehgeer, A.; Ginsburg, G.S.; McCracken, J.; Keeton, C.; Kendall, P.C.; Birmaher, B.; Sakolsky, D.; Walkup, J.; Peris, T.; et al. Child and Adolescent Adherence with Cognitive Behavioral Therapy for Anxiety: Predictors and Associations with Outcomes. J. Clin. Child Adolesc. Psychol. 2019, 48, S215–S226. [Google Scholar] [CrossRef]
- Li, A.Y.; Chau, C.; Cheng, C. Development and Validation of a Parent-Based Program for Preventing Gaming Disorder: The Game Over Intervention. Int. J. Environ. Res. Public Health 2019, 16, 1984. [Google Scholar] [CrossRef] [Green Version]
- Torres-Rodríguez, A.; Griffiths, M.D.; Carbonell, X. The Treatment of Internet Gaming Disorder: A Brief Overview of the PIPATIC Program. Int. J. Ment. Health Addict. 2018, 16, 1000–1015. [Google Scholar] [CrossRef] [Green Version]
- Van der Pol, T.M.; Hendriks, V.; Rigter, H.; Cohn, M.D.; Doreleijers, T.A.H.; van Domburgh, L.; Vermeiren, R.R.J.M. Multidimensional Family Therapy in Adolescents with a Cannabis Use Disorder: Long-Term Effects on Delinquency in a Randomized Controlled Trial. Child Adolesc. Psychiatry Ment. Health 2018, 12, 44. [Google Scholar] [CrossRef]
- Liddle, H.A.; Hogue, A. Multidimensional Family Therapy for Adolescent Substance Abuse. In Innovations in Adolescent Substance Abuse Interventions; Pergamon/Elsevier Science Inc.: Amsterdam, The Netherlands, 2001; pp. 229–261. ISBN 978-0-08-043577-0. [Google Scholar]
- Wroe, A.L.; Wise, C. Evaluation of an Adapted Cognitive Behavioural Therapy (CBT) Group Programme for People with Obsessive Compulsive Disorder: A Case Study. Cogn. Behav. Ther. 2012, 5, 112–123. [Google Scholar] [CrossRef]
- Morrison, N. Group Cognitive Therapy: Treatment of Choice or Sub-Optimal Option? Behav. Cogn. Psychother. 2001, 29, 311–332. [Google Scholar] [CrossRef]
- Du, Y.S.; Jiang, W.; Vance, A. Longer Term Effect of Randomized, Controlled Group Cognitive Behavioural Therapy for Internet Addiction in Adolescent Students in Shanghai. Aust. N. Z. J. Psychiatry 2010, 44, 129–134. [Google Scholar] [CrossRef]
- Liu, Q.X.; Fang, X.Y.; Yan, N.; Zhou, Z.K.; Yuan, X.J.; Lan, J.; Liu, C.Y. Multi-Family Group Therapy for Adolescent Internet Addiction: Exploring the Underlying Mechanisms. Addict. Behav. 2015, 42, 1–8. [Google Scholar] [CrossRef]
- Lo, C.K.M.; Yu, L.; Cho, Y.W.; Chan, K.L. A Qualitative Study of Practitioners’ Views on Family Involvement in Treatment Process of Adolescent Internet Addiction. Int. J. Environ. Res. Public Health 2020, 18, 86. [Google Scholar] [CrossRef]
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers by Parental Ratings: Development and Validation of the Gaming Disorder Scale for Parents (GADIS-P). J. Behav. Addict. 2021, 10, 159–168. [Google Scholar] [CrossRef]
- Schneider, L.A.; King, D.L.; Delfabbro, P.H. Maladaptive Coping Styles in Adolescents with Internet Gaming Disorder Symptoms. Int. J. Ment. Health Addict. 2018, 16, 905–916. [Google Scholar] [CrossRef]
- Jeong, H.; Yim, H.W.; Lee, S.-Y.; Lee, H.K.; Potenza, M.N.; Kwon, J.-H.; Koo, H.J.; Kweon, Y.-S.; Bhang, S.; Choi, J.-S. Discordance between Self-Report and Clinical Diagnosis of Internet Gaming Disorder in Adolescents. Sci. Rep. 2018, 8, 10084. [Google Scholar] [CrossRef] [PubMed]
- Burlingame, G.M.; McClendon, D.T.; Yang, C. Cohesion in Group Therapy: A Meta-Analysis. Psychotherapy 2018, 55, 384–398. [Google Scholar] [CrossRef] [PubMed]
- Burlingame, G.M.; Jensen, J.L. Small Group Process and Outcome Research Highlights: A 25-Year Perspective. Int. J. Group Psychother. 2017, 67, S194–S218. [Google Scholar] [CrossRef] [Green Version]
- Gorowska, M.; Tokarska, K.; Zhou, X.; Gola, M.K.; Li, Y. Novel Approaches for Treating Internet Gaming Disorder: A Review of Technology-Based Interventions. Compr. Psychiatry 2022, 115, 152312. [Google Scholar] [CrossRef]
- Wölfling, K.; Beutel, M.E.; Dreier, M.; Müller, K.W. Treatment Outcomes in Patients with Internet Addiction: A Clinical Pilot Study on the Effects of a Cognitive-Behavioral Therapy Program. BioMed Res. Int. 2014, 2014, 425924. [Google Scholar] [CrossRef]
- Wartberg, L.; Thomsen, M.; Moll, B.; Thomasius, R. Pilot Study on the Effectiveness of a Cognitive Behavioural Group Programme for Adolescents with Pathological Internet Use. Prax. Kinderpsychol. Kinderpsychiatr. 2014, 63, 21–35. [Google Scholar]
- Besser, B.; Bischof, G.; Bischof, A.; Brandt, D.; Orlowski, S.; Hoffmann, H.; Rumpf, H.-J. Pilot Study of a Brief Intervention to Treating Internet Use Disorders. SUCHT 2022, 68, 41–49. [Google Scholar] [CrossRef]
- Paschke, K.; Arnaud, N.; Austermann, M.I.; Thomasius, R. Risk Factors for Prospective Increase in Psychological Stress during COVID-19 Lockdown in a Representative Sample of Adolescents and Their Parents. BJPsych Open 2021, 7, e94. [Google Scholar] [CrossRef]
| Variable | Absolute Frequency (Relative Frequency in %) | Mean (SD) | |
|---|---|---|---|
| Sociodemographic measures | |||
| Parent | |||
| Mother | 31 (72.1) | ||
| Father | 12 (27.9) | ||
| Age | |||
| All parents | 48.72 (6.78) | ||
| Mothers | 46.74 (5.92) | ||
| Fathers | 53.83 (6.35) | ||
| Children | |||
| Number of children in a household | 1.86 (0.77) | ||
| Relationship status | |||
| Married/Relationship | 22 (51.2) | ||
| Single | 5 (11.6) | ||
| Separated | 15 (34.9) | ||
| Widowed | 1 (2.3) | ||
| Migration background | |||
| Yes | 14 (32.6) | ||
| No | 29 (67.4) | ||
| Occupational status | |||
| Not working | 7 (16.3) | ||
| Working part-time | 14 (32.6) | ||
| Working fulltime | 22 (51.2) | ||
| School education | |||
| Lower school certificate (Hauptschulabschluss) | 2 (4.7) | ||
| Secondary school certificate (Realschulabschluss) | 11 (25.6) | ||
| University entry qualification (Abitur/Fachhochschulreife) | 29 (67.4) | ||
| Other | 1 (2.3) | ||
| Treatment measures | |||
| Participation | |||
| With the other parent | 18 (41.9) | ||
| Alone | 25 (58.1) | ||
| Completers | Yes No | 34 (79.07) 9 (20.93) | |
| Attended sessions | |||
| All parents | 6.00 (1.95) | ||
| Mothers | 6.39 (1.80) | ||
| Fathers | 5.00 (2.05) | ||
| Psychometric measures Psychological factors | |||
| PSS-4 | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 7.4 (3.1) 6.9 (3.1) 6.0 (3.5) | |
| BSI-18 | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 7.9 (7.0) 8.0 (7.8) 5.9 (6.6) | |
| Parenting factors | |||
| FSW | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 41.2 (4.4) 41.5 (5.4) 42.6 (5.1) | |
| MR-6 | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 7.4 (4.6) 9.4 (5.0) 9.6 (4.5) | |
| Family factors | |||
| FB-K | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 32.7 (6.7) 36.5 (7.0) 35.7 (8.5) | |
| FCS | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 25.3 (6.0) 29.1 (6.4) 28.8 (7.3) | |
| Adolescent PG | |||
| PIGDS | Start of training (baseline) End of training (8 weeks after baseline) Follow-up (14 weeks after baseline) | 8.2 (1.8) 6.9 (2.7) 6.9 (2.9) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hülquist, J.; Fangerau, N.; Thomasius, R.; Paschke, K. Resource-Strengthening Training for Parents of Adolescents with Problematic Gaming (Res@t-P): A Clinical Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 9495. https://doi.org/10.3390/ijerph19159495
Hülquist J, Fangerau N, Thomasius R, Paschke K. Resource-Strengthening Training for Parents of Adolescents with Problematic Gaming (Res@t-P): A Clinical Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(15):9495. https://doi.org/10.3390/ijerph19159495
Chicago/Turabian StyleHülquist, Joel, Nicole Fangerau, Rainer Thomasius, and Kerstin Paschke. 2022. "Resource-Strengthening Training for Parents of Adolescents with Problematic Gaming (Res@t-P): A Clinical Pilot Study" International Journal of Environmental Research and Public Health 19, no. 15: 9495. https://doi.org/10.3390/ijerph19159495
APA StyleHülquist, J., Fangerau, N., Thomasius, R., & Paschke, K. (2022). Resource-Strengthening Training for Parents of Adolescents with Problematic Gaming (Res@t-P): A Clinical Pilot Study. International Journal of Environmental Research and Public Health, 19(15), 9495. https://doi.org/10.3390/ijerph19159495






