ePSICONUT: An e-Health Programme to Improve Emotional Health and Lifestyle in University Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
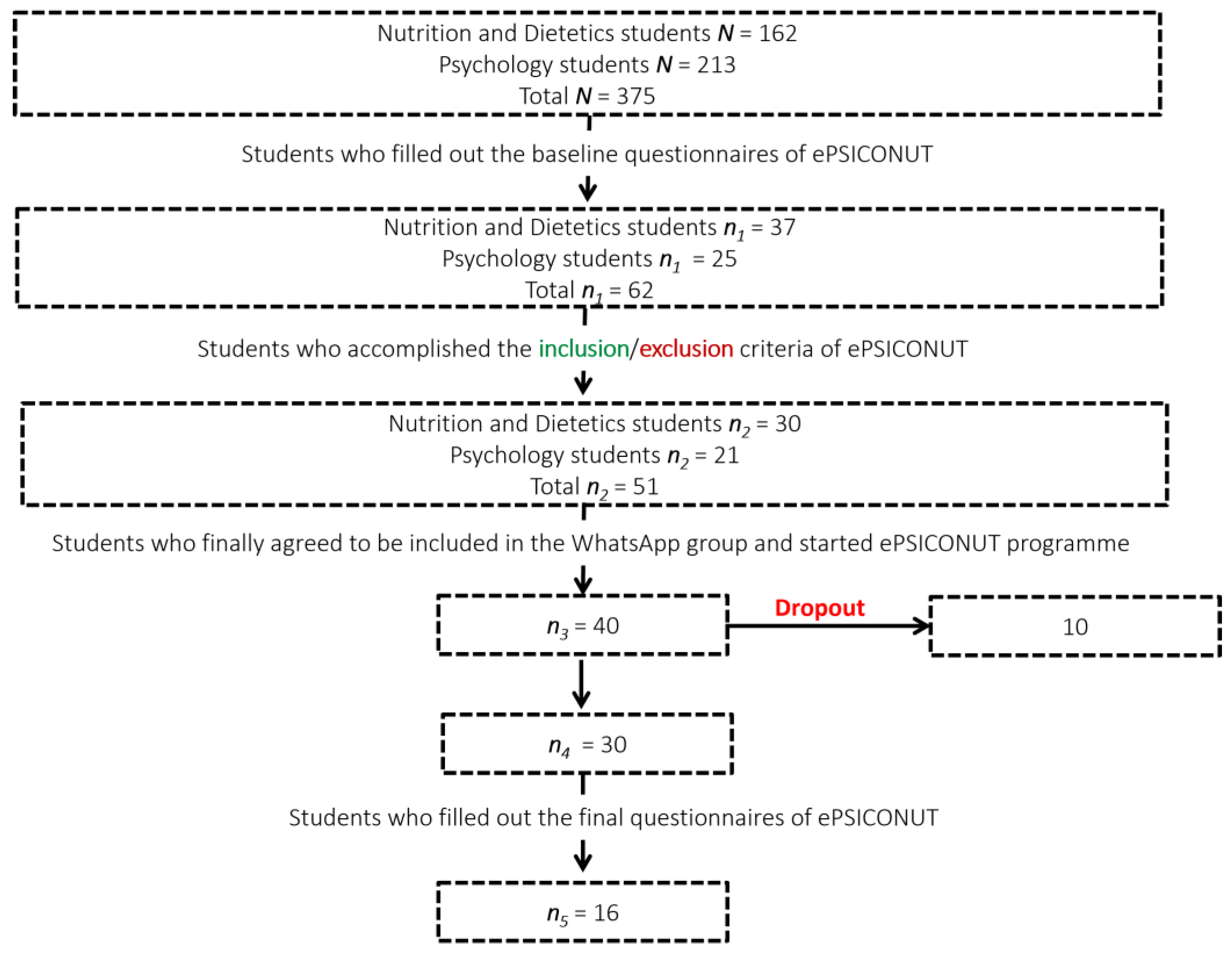
2.2. Participants
2.3. Instruments
2.3.1. Promotion of ePSICONUT Tools
Test Batteries Applied at the Beginning and at the End of ePSICONUT
- A General Health Questionnaire. Consisting of 13 questions, aimed to evaluate the presence/diagnosis of physical and/or mental pathologies, present or past, as well as risk and protective factors for health (such as sleep, smoking, coffee intake, and meditation).
- A Digital Health Questionnaire. It assesses the use and perception of participants about digital tools for the improvement of lifestyle and psychological well-being. Many questions of this instrument were based on a survey called Encuesta de usuarios 2018 sobre sanidad digital de España [2018 Spanish eHealth User survey] [27]. In the initial questionnaires’ battery, this section had just 11 questions to evaluate these topics in general. In the final questionnaires’ battery, this part consisted of 24 questions: on the one hand, the same questions that included the initial test; on the other hand, questions that were focused on evaluating the subjects’ perception about the digital tools specifically used in ePSICONUT (Headspace, Insight Timer, Fabulous, YouTube channel, WhatsApp group, e-mail, and Excel sheets to perform some of the programme’s tasks/activities). Furthermore, this last questionnaire included an ad hoc Satisfaction Survey to evaluate the participants’ appreciation about the following aspects of the programme: organisation, quality of the follow-up offered, quality of the information provided, self-perception of the ePSICONUT impact on the improvement of their eating habits, physical exercise, and psychological well-being.
Instruments Used to Evaluate the Psychological State and Lifestyle of the Participants
2.4. Procedure and Design of the Intervention
2.5. Data Analysis
3. Results
3.1. Impact of ePSICONUT on Global Diet Quality Index
3.2. Impact of ePSICONUT on Physical Exercise
3.3. Impact of ePSICONUT on Overall Lifestyle
3.4. Impact of ePSICONUT on Subjective Well-Being and Motivation to Change
3.5. Program Impact
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rehman, H.; Ahmad, M.I. COVID-19: Quarantine, Isolation, and Lifestyle Diseases. Arch. Physiol. Biochem. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Idrovo Carlier, S.; Leon Llorente, C.; Grau Grau, M. Comparing Work—Life Balance in Spanish and Latin—American Countries. Eur. J. Train. Dev. 2012, 36, 286–307. [Google Scholar] [CrossRef]
- Global Diffusion of EHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on EHealth. Available online: https://apps.who.int/iris/handle/10665/252529 (accessed on 3 June 2022).
- Ratheeswari, K. Information Communication Technology in Education. J. Appl. Adv. Res. 2018, 3, 45–47. [Google Scholar] [CrossRef]
- Yang, X.; Song, B.; Wu, A.; Mo, P.K.H.; Di, J.; Wang, Q.; Lau, J.T.F.; Wang, L. Social, Cognitive, and eHealth Mechanisms of COVID-19-Related Lockdown and Mandatory Quarantine That Potentially Affect the Mental Health of Pregnant Women in China: Cross-Sectional Survey Study. J. Med. Internet Res. 2021, 23, e24495. [Google Scholar] [CrossRef]
- Cantisano, L.M.; Belando Pedreño, N.; Ballester Sánchez, Á.; Blanco Fernández, A.; González Soltero, R. Changes in lifestyle and emotions during the COVID-19 lockdown. Int. J. Dev. Educ. Psychol. 2021, 1, 413–424. [Google Scholar] [CrossRef]
- Téllez-Carvajal, E. Reflexiones En Torno a La “Ciudadanía Digital”. Rev. Doxa Dig. 2017, 7, 47–65. [Google Scholar] [CrossRef]
- Bhardwaj, N.N.; Wodajo, B.; Gochipathala, K.; Paul, D.P.; Coustasse, A. Can mHealth Revolutionize the Way We Manage Adult Obesity? Perspect. Health Inf. Manag. 2017, 14, 1a. [Google Scholar] [PubMed]
- Burke, L.E.; Styn, M.A.; Sereika, S.M.; Conroy, M.B.; Ye, L.; Glanz, K.; Sevick, M.A.; Ewing, L.J. Using MHealth Technology to Enhance Self-Monitoring for Weight Loss: A Randomized Trial. Am. J. Prev. Medic. 2012, 43, 20–26. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Manzoni, G.M.; Pietrabissa, G.; Corti, S.; Giusti, E.M.; Molinari, E.; Simpson, S. Obesity and Outpatient Rehabilitation Using Mobile Technologies: The Potential MHealth Approach. Front. Psych. 2014, 5, 559. [Google Scholar] [CrossRef]
- Gilliland, J.; Sadler, R.; Clark, A.; O’Connor, C.; Milczarek, M.; Doherty, S. Using a Smartphone Application to Promote Healthy Dietary Behaviours and Local Food Consumption. Biomed. Res. Int. 2015, 2015, 841368. [Google Scholar] [CrossRef]
- San Mauro Martín, I.; González Fernández, M.; Collado Yurrita, L. Aplicaciones móviles en nutrición, dietética y hábitos saludables: Análisis y consecuencia de una tendencia al alza. Nutr. Hosp. 2014, 30, 15–24. [Google Scholar] [CrossRef]
- Santos-Miranda, E.; Rico-Díaz, J.; Carballo-Fazanes, A.; Abelairas-Gómez, C. Cambios En Hábitos Saludables Relacionados Con Actividad Física y Sedentarismo Durante Un Confinamiento Nacional Por COVID-19 (Changes in Healthy Habits Regarding Physical Activity and Sedentary Lifestyle during a National Lockdown Due to COVID-19). Retos 2021, 43, 415–421. [Google Scholar] [CrossRef]
- Kanstrup, A.M.; Bertelsen, P.S.; Knudsen, C. Changing Health Behavior with Social Technology? A Pilot Test of a Mobile App Designed for Social Support of Physical Activity. Int. J. Environ. Res. Public Health 2020, 17, 8383. [Google Scholar] [CrossRef]
- Sucala, M.; Cuijpers, P.; Muench, F.; Cardoș, R.; Soflau, R.; Dobrean, A.; Achimas-Cadariu, P.; David, D. Anxiety: There Is an App for That. A Systematic Review of Anxiety Apps. Depress. Anxiety 2017, 34, 518–525. [Google Scholar] [CrossRef]
- Turner, T.; Hingle, M. Evaluation of a Mindfulness-Based Mobile App Aimed at Promoting Awareness of Weight-Related Behaviors in Adolescents: A Pilot Study. JMIR Res. Protoc. 2017, 6, e6695. [Google Scholar] [CrossRef]
- Muñoz, A.O.; Camacho, E.; Torous, J. Marketplace and Literature Review of Spanish Language Mental Health Apps. Front. Digit. Health 2021, 3, 615366. [Google Scholar] [CrossRef]
- Feldman, D.I.; Theodore Robison, W.; Pacor, J.M.; Caddell, L.C.; Feldman, E.B.; Deitz, R.L.; Feldman, T.; Martin, S.S.; Nasir, K.; Blaha, M.J. Harnessing MHealth Technologies to Increase Physical Activity and Prevent Cardiovascular Disease. Clin. Cardiol. 2018, 41, 985–991. [Google Scholar] [CrossRef]
- Sarwar, C.M.S.; Vaduganathan, M.; Butler, J. Impact of Site Selection and Study Conduct on Outcomes in Global Clinical Trials. Curr. Heart Fail. Rep. 2017, 14, 203–209. [Google Scholar] [CrossRef]
- Alyami, M.; Melyani, Z.; Johani, A.A.; Ullah, E.; Alyami, H.; Sundram, F.; Hill, A.; Henning, M. The Impact of Self-Esteem, Academic Self-Efficacy and Perceived Stress on Academic Performance: A Cross-Sectional Study of Saudi Psychology Students. Eur. J. Educ. Sci. 2017, 4, 51–63. [Google Scholar] [CrossRef]
- Manterola, C.; Otzen, T. Estudios Experimentales 2 Parte. Estudios cuasi-experimentales. Int. J. Morphol. 2015, 33, 382–387. [Google Scholar] [CrossRef]
- Caroll, J.; Moorhead, A.; Bond, R.; LeBlanc, W.; Petrella, R.; Fiscella, K. Who Uses Mobile Phone Health Apps and Does Use Matter? A Secondary Data Analytics Approach. J. Med. Internet Res. 2017, 19, e125. [Google Scholar] [CrossRef]
- Younes, N.; Chollet, A.; Menard, E.; Melchior, M. E-Mental Health Care among Young Adults and Help-Seeking Behaviors: A Transversal Study in a Community Sample. J. Med. Internet Res. 2015, 17, e123. [Google Scholar] [CrossRef] [PubMed]
- Otzen, T.; Manterola, C. Técnicas de Muestreo Sobre Una Población a Estudio. Int. J. Morphol. 2017, 35, 227–232. [Google Scholar] [CrossRef]
- Belmont, I. Principios Éticos & Directrices Para La Protección de Sujetos Humanos de Investigación. Estados Unidos de Norteamérica: Reporte de la Comisión Nacional para la Protección de Sujetos Humanos de Investigación Biomédica y de Comportamiento. In Informe Belmont; National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research: Berkeley, CA, USA, 1978. [Google Scholar]
- Gilder, S. World Medical Association Meets in Helsinki. Br. Med. J. 1964, 2, 299–300. [Google Scholar] [CrossRef]
- Accenture Consulting. Encuesta de Usuarios 2018 Sobre Sanidad Digital-España. 2018. Available online: https://www.accenture.com/_acnmedia/pdf-83/accenture-health-meet-todays-healthcare-spain.pdf (accessed on 1 October 2020).
- Beck, A.; Steer, R.; Brown, G. Beck Depression Inventory, 2nd ed.; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- García-Batista, Z.E.; Guerra-Peña, K.; Cano-Vindel, A.; Herrera-Martínez, S.X.; Medrano, L.A. Validity and Reliability of the Beck Depression Inventory (BDI-II) in General and Hospital Population of Dominican Republic. PLoS ONE 2018, 13, e0199750. [Google Scholar] [CrossRef]
- García-Batista, Z.E.; Guerra-Peña, K.; Cano-Vindel, A.; Cantisano-Guzmán, L.M.; Flores-Kanter, P.E.; Medrano, L.A. Medición de la comorbilidad depresiva en drogodependientes: Validez y eficacia diagnóstica del Inventario de Depresión de Beck (BDI-II) en dominicanos con múltiple consumo de sustancias. Rev. Psicop. Y Psic. Clín. 2019, 24, 163–171. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.; Lushene, R. Manual for the State-Trait Anxiety Inventory; Consulting Psychologist: Palo Alto, CA, USA, 1970. [Google Scholar]
- García-Batista, Z.E.; Guerra-Peña, K.; Cano-Vindel, A.; Herrera-Martínez, S.X.; Flores-Kanter, P.E.; Medrano, L.A. Propiedades psicométricas del Inventario de Ansiedad Estado-Rasgo en población general y hospitalaria de República Dominicana. Ansiedad Estré S 2017, 23, 53–58. [Google Scholar] [CrossRef]
- Cánovas-Sánchez, J. EBP: Escala de Bienestar Psicológico. TEA Ediciones. 2013. Available online: https://pdfcoffee.com/escala-de-bienestar-psicologico-ebp-jose-sanchez-canovas-2-pdf-free.html (accessed on 1 September 2020).
- McConnaughy, E.A.; Prochaska, J.O.; Velicer, W.F. Stages of Change in Psychotherapy: Measurement and Sample Profiles. Psychother. Theory Res. Pract. 1983, 20, 368–375. [Google Scholar] [CrossRef]
- Gómez-Peña, M.; Penelo, E.; Granero, R.; Fernández-Aranda, F.; Álvarez-Moya, E.; Santamaría, J.J.; Moragas, L.; Aymamí, M.-N.; Bueno, B.; Gunnard, K.; et al. Motivation to Change and Pathological Gambling: Analysis of the Relationship with Clinical and Psychopathological Variables. Br. J. Clin. Psych. 2011, 50, 196–210. [Google Scholar] [CrossRef]
- Wang, D.; Xing, X.-H.; Wu, X.-B. The Healthy Lifestyle Scale for University Students: Development and Psychometric Testing. Aust. J. Prim. Health 2012, 18, 339–345. [Google Scholar] [CrossRef]
- Domínguez Lara, S.; Martín-Díaz, A.; Ramírez-Colina, S.; Campos-Uscanga, Y. Análisis Estructural de Una Escala de Estilos de Vida Saludables en Estudiantes Universitarias Mexicanas. Rev. Cub. Enfer. 2019, 35. Available online: http://www.revenfermeria.sld.cu/index.php/enf/article/view/2221 (accessed on 1 October 2020).
- Mantilla Toloza, S.C.; Gómez-Conesa, A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iber. Fisiot. Y Kines. 2007, 10, 48–52. [Google Scholar] [CrossRef]
- Ghasemi, A.; Zahediasl, S. Normality Tests for Statistical Analysis: A Guide for Non-Statisticians. Int. J. End. Y Metab. 2012, 10, 486–489. [Google Scholar] [CrossRef]
- Caycho-Rodríguez, T.; Ventura-León, J.L. El coeficiente Omega: Un método alternativo para la estimación de la confiabilidad. Rev. A Lat. Cien. Soc. Niñ. Y Juv. 2017, 15, 625–627. [Google Scholar]
- Molina, J.G.; Rodrigo, M.F. T.5—Pruebas no Paramétricas; Universitat de València: Valencia, Spain, 2014. [Google Scholar]
- Sánchez Turcios, R.A. t-Student: Usos y abusos. Rev. Mex. Card. 2015, 26, 59–61. [Google Scholar]
- Cohen, J. The Effect Size Index: D. Statistical Power Analysis for the Behavioral Sciences; Routhledge Academic: Abingdon-on-Thames, UK, 1988. [Google Scholar]
- Ellis, J.G. Cognitive Behavioral Therapy for Insomnia and Acute Insomnia: Considerations and Controversies. Sleep Med. Clin. 2019, 14, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Lara, S. Magnitud del Efecto, una Guía Rápida. Educ. Méd. 2018, 19, 251–254. [Google Scholar] [CrossRef]
- Economides, M.; Martman, J.; Bell, M.J.; Sanderson, B. Improvements in Stress, Affect, and Irritability Following Brief Use of a Mindfulness-Based Smartphone App: A Randomized Controlled Trial. Mindfulness 2018, 9, 1584–1593. [Google Scholar] [CrossRef] [PubMed]
- Mani, M.; Kavanagh, D.J.; Hides, L.; Stoyanov, S.R. Review and Evaluation of Mindfulness-Based IPhone Apps. JMIR Mhealth Uhealth 2015, 3, e82. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.P.A.; Heuvel, W.A.C.V.D.; Jonker, C.M. EHealth WhatsApp for Social Support: Design Lessons. Int. J. Netw. Virtual Organ. 2020, 23, 112–127. [Google Scholar] [CrossRef]
- Pot, G.K.; Battjes-Fries, M.C.; Patijn, O.N.; Pijl, H.; Witkamp, R.F.; de Visser, M.; van der Zijl, N.; de Vries, M.; Voshol, P.J. Nutrition and Lifestyle Intervention in Type 2 Diabetes: Pilot Study in the Netherlands Showing Improved Glucose Control and Reduction in Glucose Lowering Medication. BMJ Nutr. Prev. Health 2019, 2, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Borrega-Mouquinho, Y.; Sánchez-Gómez, J.; Fuentes-García, J.P.; Collado-Mateo, D.; Villafaina, S. Effects of High-Intensity Interval Training and Moderate-Intensity Training on Stress, Depression, Anxiety, and Resilience in Healthy Adults During Coronavirus Disease 2019 Confinement: A Randomized Controlled Trial. Front. Psychol. 2021, 12, 643069. [Google Scholar] [CrossRef] [PubMed]
- Rajgopal, A.; Li, C.R.; Shah, S.; Budhathoki, S.S. The use of telehealth to overcome barriers to mental health services faced by young people from Afro-Caribbean back-grounds in England during the COVID-19 pandemic. J. Glob. Health 2021, 11, 03040. [Google Scholar] [CrossRef] [PubMed]
- Termes Escalé, M.; Martínez Chicano, D.; Egea Castillo, N.; Gutiérrez Sánchez, A.; García Arenas, D.; Llata Vidal, N.; Martín de Carpi, J. Educación nutricional en niños en edad escolar a través del Programa Nutriplato(r). Nutr. Hosp. 2020, 37, 47–51. [Google Scholar] [CrossRef]
- Pedersen, S.; Grønhøj, A.; Thøgersen, J. Following Family or Friends. Social Norms in Adolescent Healthy Eating. Appetite 2015, 86, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Torniainen-Holm, M.; Pankakoski, M.; Lehto, T.; Saarelma, O.; Mustonen, P.; Joutsenniemi, K.; Suvisaari, J. The Effectiveness of Email-Based Exercises in Promoting Psychological Wellbeing and Healthy Lifestyle: A Two-Year Follow-up Study. BMC Psychol. 2016, 4, 21. [Google Scholar] [CrossRef]
- Tang, Y.H.; Chong, M.C.; Chua, Y.P.; Chui, P.L.; Tang, L.Y.; Rahmat, N. The Effect of Mobile Messaging Apps on Cardiac Patient Knowledge of Coronary Artery Disease Risk Factors and Adherence to a Healthy Lifestyle. J. Clin. Nurs. 2018, 27, 4311–4320. [Google Scholar] [CrossRef]
- Breuer, L.; Barker, C. Online Support Groups for Depression: Benefits and Barriers. SAGE Open 2015, 5. [Google Scholar] [CrossRef]
- Swancutt, D.; Tarrant, M.; Pinkney, J. How Group-Based Interventions Can Improve Services for People with Severe Obesity. Curr. Obes. Rep. 2019, 8, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Lie, S.S.; Karlsen, B.; Graue, M.; Oftedal, B. The Influence of an EHealth Intervention for Adults with Type 2 Diabetes on the Patient-Nurse Relationship: A Qualitative Study. Scand. J. Caring Sci. 2019, 33, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Brandt, C.J.; Søgaard, G.I.; Clemensen, J.; Søndergaard, J.; Nielsen, J.B. Determinants of Successful EHealth Coaching for Consumer Lifestyle Changes: Qualitative Interview Study Among Health Care Professionals. J. Med. Internet Res. 2018, 20, e237. [Google Scholar] [CrossRef] [PubMed]
- Fuller-Tyszkiewicz, M.; Richardson, B.; Lewis, V.; Linardon, J.; Mills, J.; Juknaitis, K.; Lewis, C.; Coulson, K.; O’Donnell, R.; Arulkadacham, L.; et al. A Randomized Trial Exploring Mindfulness and Gratitude Exercises as EHealth-Based Micro-Interventions for Improving Body Satisfaction. Comp. Hum. Behav. 2019, 95, 58–65. [Google Scholar] [CrossRef]
- Lahtinen, O.; Aaltonen, J.; Kaakinen, J.; Franklin, L.; Hyönä, J. The Effects of App-Based Mindfulness Practice on the Well-Being of University Students and Staff. Curr. Psychol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Reyes, A.T. A Mindfulness Mobile App for Traumatized COVID-19 Healthcare Workers and Recovered Patients: A Response to “The Use of Digital Applications and COVID-19”. Community Ment. Health J. 2020, 56, 1204–1205. [Google Scholar] [CrossRef] [PubMed]
- Sort, A. The Role of MHealth in Mental Health. Mhealth 2017, 3, 1. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Villani, D.; Cognetta, C.; Repetto, C.; Serino, S.; Toniolo, D.; Scanzi, F.; Riva, G. Promoting Emotional Well-Being in Older Breast Cancer Patients: Results from an EHealth Intervention. Front. Psych. 2018, 9, 2279. [Google Scholar] [CrossRef]
- Nayak, M.S.D.P.; Narayan, K.A. Strengths and weakness of online surveys. J. Hum. Soc. Sci. 2019, 24, 31–38. [Google Scholar] [CrossRef]
- Hernández Sampieri, R.; Fernández Collado, C.; Baptista Lucio, M.d.P. Metodología de la Investigación, 6th ed.; McGraw-Hill/Interamericana Editores, S.A. de C.V: México, Mexico, 2014. [Google Scholar]
- Levy, Y.; Ellis, T.J. A guide for novice researchers on experimental and quasi-experimental studies in information systems research. Interdiscip. J. Inf. Knowl. Manag. 2011, 6, 151. [Google Scholar] [CrossRef]
- García-Solano, M.; Gutiérrez-González, E.; Santos-Sanz, S.; Yusta-Boyo, M.J.; Villar-Villalba, C.; Dal Re-Saavedra, M.A. Intervención grupal de promoción de hábitos saludables en el ámbito laboral: Programa IPHASAL. Med. Y Seg. Trab. 2021, 67, 24–36. [Google Scholar] [CrossRef]
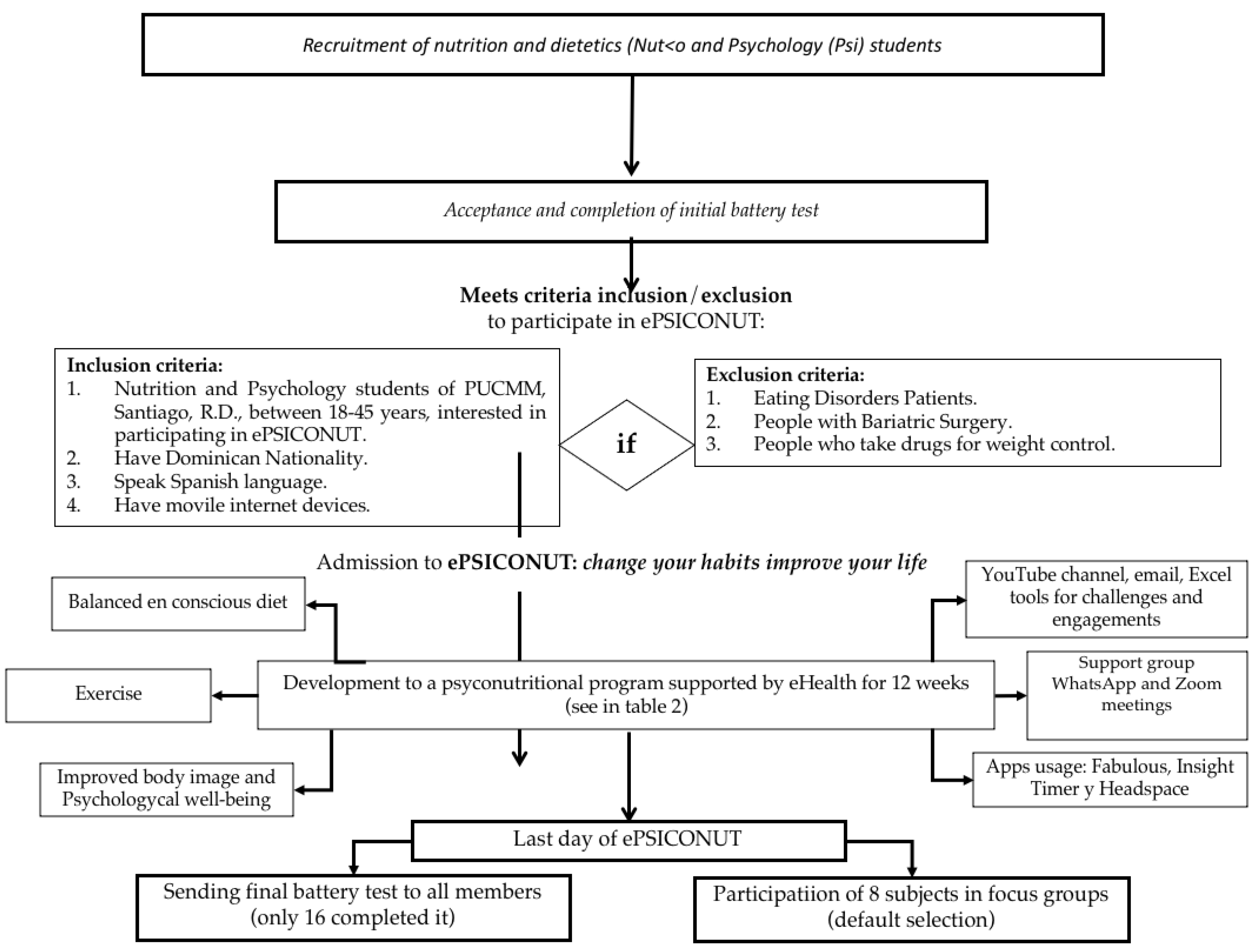
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Students of Nutrition and Dietetics or Psychology from PUCMM, Santiago, D.R., between 18 and 45 years old, who agree to participate in ePSICONUT. | Dropout from the psychonutritional intervention programme. |
| Have Dominican nationality. | People with an eating disorder. |
| Speak Spanish. | People undergoing bariatric surgery. |
| Have mobile devices with Internet services. | People taking drugs related to weight control. |
| Weeks | Activities |
|---|---|
| Week 1 | Creation of WhatsApp group and welcome and sending mail with video on YouTube channel. |
| Week 2 | Reminders of commitments and clarification of doubts by mail and WhatsApp. |
| Week 3 | Reminders of commitments and challenges via WhatsApp. |
| Week 4 | Continuation of messages by WhatsApp to take care of food and follow the exercise to strengthen the psychological well-being. |
| Week 5 | Meeting via Zoom to address the balance between self-care and study habits. Fabulous was introduced as the mobile application to create, strengthen, and track healthy habits. |
| Week 6 | Informative capsule posted on the YouTube channel to promote the organisation and optimisation of food quality; provide recipes/options for healthy breakfasts, lunches, dinners, and snacks; introduce the Nestlé Nutriplato. |
| Week 7 | Videos posted on YouTube channel to promote physical exercise at home and in nature (according to the limitations by COVID-19 pandemia situation). |
| Week 8 | Meeting via Zoom to introduce mindfulness practice (led by the principal investigator and a certified mindfulness practitioner). The use of Headspace was encouraged to practice mindfulness on a daily basis thereafter. |
| Week 9 | Video via YouTube channel to introduce mindful eating. Insight Timer is presented as a mobile application to support the practice of mindful eating. |
| Week 10 | Sending an informative document: what it is, how to exercise, and optimising acceptance. |
| Week 11 | Constant communication via WhatsApp, stimulating: conscious eating, physical exercise, body image acceptance. Meeting via Zoom to practice conscious eating at lunchtime. |
| Week 12 | Sending of final test battery. Closing meeting via Zoom with a focus group of eight people, in order to make a qualitative analysis of the effectiveness, limitations, and areas for improvement of the ePSICONUT programme. |
| Variables | 2 | Sig. t Student | d | 1 − ß | |
|---|---|---|---|---|---|
| Healthy food | |||||
| Dairy products | 5.44 | 6.31 | 0.371 | ||
| Total ICGD score | 74.31 | 87.38 | 0.002 * | −0.92 | 0.93 |
| Variables | 1 | 2 | Sig. Wilcoxon | rbis | 1 − ß |
|---|---|---|---|---|---|
| Healthy foods | |||||
| Vegetables | 3.75 | 7.50 | 0.005 * | −0.91 | 0.96 |
| Fruits | 1.75 | 7.50 | 0.063 | ||
| Legumes | 10.00 | 10.00 | 0.317 | ||
| Fish | 4.25 | 7.50 | 0.114 | ||
| “Unhealthy” foods | |||||
| Cakes, cookies, and sweets | 5.00 | 6.25 | 0.258 | ||
| Sugary drinks | 3.75 | 7.50 | 0.042 * | −0.64 | 0.58 |
| Sugar | 7.50 | 1.00 | 0.064 | ||
| Fried foods | 7.50 | 7.50 | 0.885 | ||
| Meals | |||||
| Breakfasts | 10.00 | 10.00 | 1.000 | ||
| Lunches | 10.00 | 10.00 | 0.317 | ||
| Dinners | 10.00 | 10.00 | 0.655 |
| Variables | 1 | 2 | Sig. Wilcoxon |
|---|---|---|---|
| MET | 214.50 | 394.50 | 0.221 |
| Weekly physical activity time | 65.00 | 80.00 | 0.363 |
| Variables | 1 | 2 | Sig. Wilcoxon | rbis | 1 − ß |
|---|---|---|---|---|---|
| BDI-II | 13.00 | 3.50 | 0.001 * | 0.97 | 0.99 |
| EBPS | 104.50 | 120.00 | 0.021 * | 0.65 | 0.73 |
| Variables | 1 | 2 | Sig. t Student | d | 1 − ß |
|---|---|---|---|---|---|
| STAI-S | 24.63 | 15.56 | 0.002 * | 0.94 | 0.93 |
| STAI-T | 25.00 | 18.44 | 0.017 * | 0.67 | 0.71 |
| Criteria for Satisfaction with ePSICONUT | s | ||
|---|---|---|---|
| Quality criteria | |||
| Quality of the follow-up provided | 4.88 | 5.00 | 0.34 |
| Level of organisation | 4.94 | 5.00 | 0.25 |
| Quality of information provided | 5.00 | 5.00 | 0.00 |
| Evaluation of subjective impact | |||
| Impact on physical exercise | 3.94 | 4.00 | 1.24 |
| Impact on psychological well-being | 4.38 | 4.50 | 0.72 |
| Impact on diet | 4.50 | 5.00 | 0.73 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cantisano, L.M.; Gonzalez-Soltero, R.; Blanco-Fernández, A.; Belando-Pedreño, N. ePSICONUT: An e-Health Programme to Improve Emotional Health and Lifestyle in University Students. Int. J. Environ. Res. Public Health 2022, 19, 9253. https://doi.org/10.3390/ijerph19159253
Cantisano LM, Gonzalez-Soltero R, Blanco-Fernández A, Belando-Pedreño N. ePSICONUT: An e-Health Programme to Improve Emotional Health and Lifestyle in University Students. International Journal of Environmental Research and Public Health. 2022; 19(15):9253. https://doi.org/10.3390/ijerph19159253
Chicago/Turabian StyleCantisano, Luisa Marilia, Rocio Gonzalez-Soltero, Ascensión Blanco-Fernández, and Noelia Belando-Pedreño. 2022. "ePSICONUT: An e-Health Programme to Improve Emotional Health and Lifestyle in University Students" International Journal of Environmental Research and Public Health 19, no. 15: 9253. https://doi.org/10.3390/ijerph19159253
APA StyleCantisano, L. M., Gonzalez-Soltero, R., Blanco-Fernández, A., & Belando-Pedreño, N. (2022). ePSICONUT: An e-Health Programme to Improve Emotional Health and Lifestyle in University Students. International Journal of Environmental Research and Public Health, 19(15), 9253. https://doi.org/10.3390/ijerph19159253








