Association between Loneliness and Depression among Community-Dwelling Older Women Living Alone in South Korea: The Mediating Effects of Subjective Physical Health, Resilience, and Social Support
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Depression
2.2.2. Loneliness
2.2.3. Subjective Physical Health
2.2.4. Resilience
2.2.5. Social Support
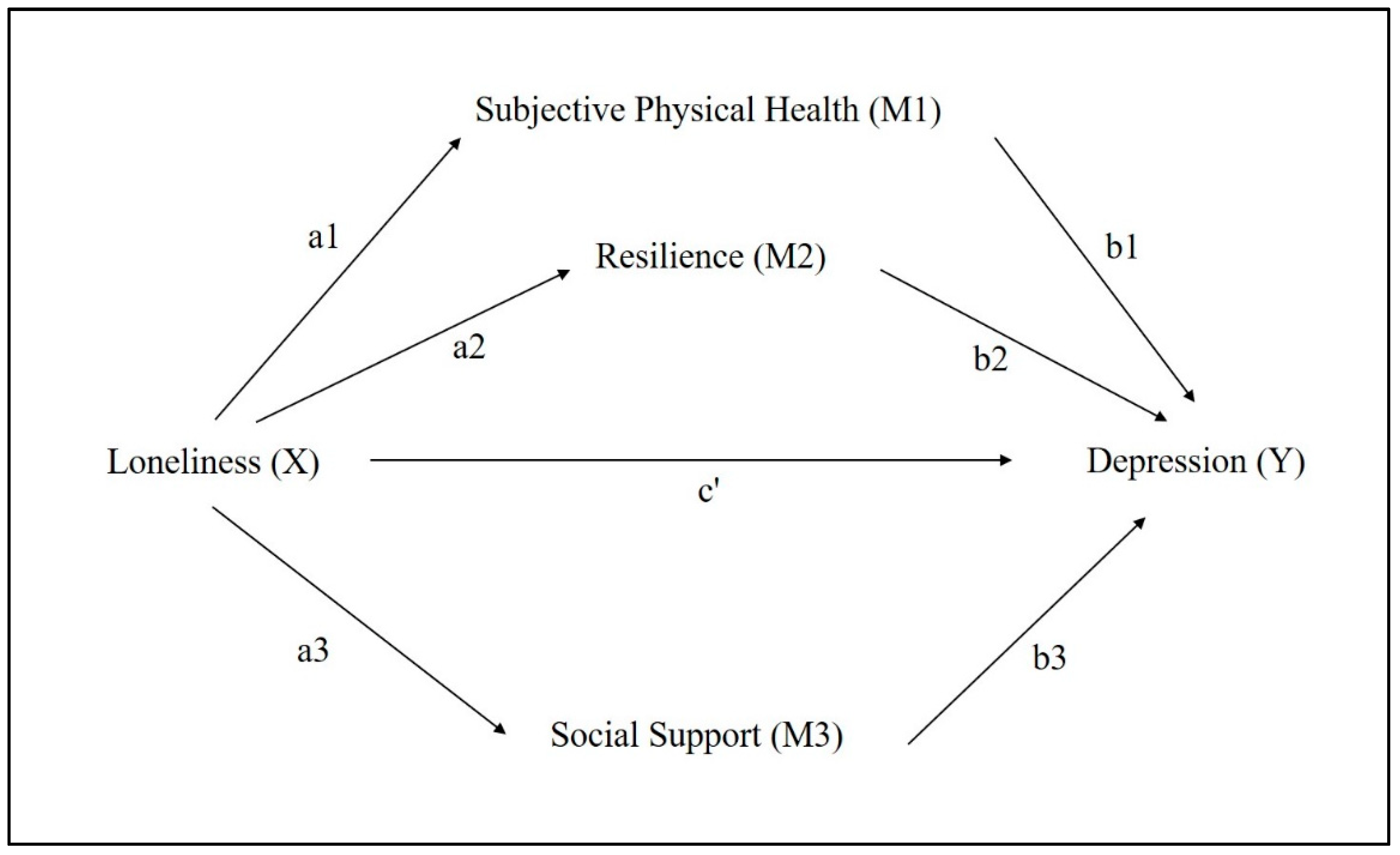
2.3. Statistical Analysis
- M1 on X (a1)
- M2 on X (a2)
- M3 on X (a3)
- Y on M1 (b1)
- Y on M2 (b2)
- Y on M3 (b3)
3. Results
3.1. Description of the Study Population
3.2. Loneliness, Subjective Physical Health, Resilience, Social Support and Depression
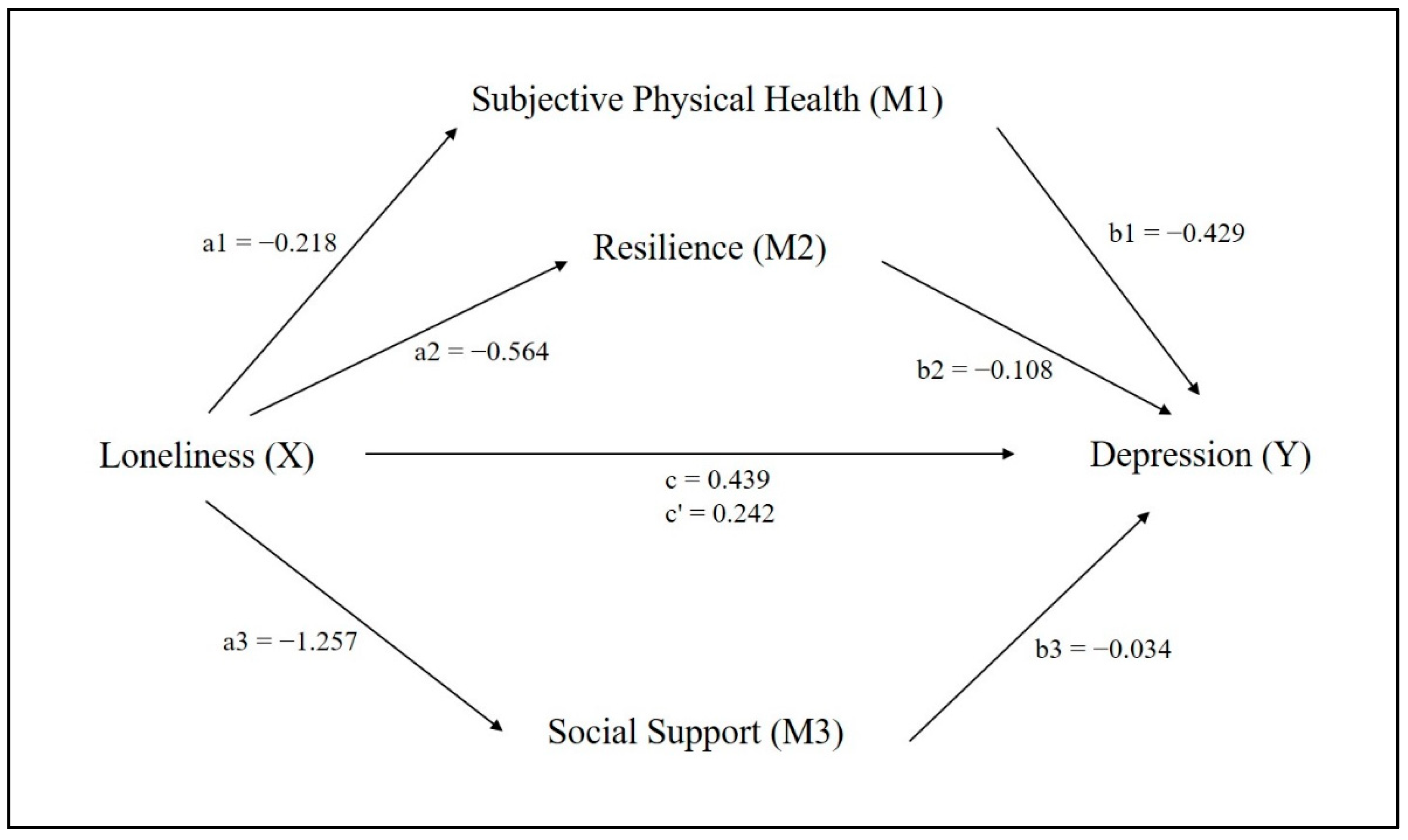
3.3. Results of the Parallel Mediation Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jang, I.-Y.; Lee, H.Y.; Eunju, L. The 50th Anniversary Committee of Korean Geriatrics Society Geriatrics Fact Sheet in Korea 2018 from National Statistics. Ann. Geriatr. Med. Res. 2019, 23, 50–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korean Statistical Information Service. Korean Statistical Information Service National Statistics Portal. Available online: https://kosis.kr/index/index.do (accessed on 17 May 2022).
- Ministry of Health & Welfare & KIHASA. 2020 Older Adults Facts. 16 July 2021. Available online: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&CONT_SEQ=366496&page=1 (accessed on 2 April 2022).
- Shaw, J.; Farid, M.; Noel-Miller, C.; Joseph, N.; Houser, A.; Asch, S.M.; Bhattacharya, J.; Flowers, L. Social Isolation and Medicare Spending: Among Older Adults, Objective Social Isolation Increases Expenditures while Loneliness Does Not. J. Aging Health 2017, 29, 1119–1143. [Google Scholar] [CrossRef] [PubMed]
- Cornwell, E.Y.; Waite, L.J. Social disconnectedness, perceived isolation, and health among older adults. J. Health Soc. Behav. 2009, 50, 31–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stahl, S.T.; Beach, S.R.; Musa, D.; Schulz, R. Living alone and depression: The modifying role of the perceived neighborhood environment. Aging Ment. Health 2017, 21, 1065–1071. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.S.; Song, H.; Kim, B. Association between physical health status, health behaviors and subjective depression among single-person household. Korean J. Health Educ. Promot. 2018, 35, 61–71. [Google Scholar] [CrossRef]
- Bilotta, C.; Bowling, A.; Nicolini, P.; Casè, A.; Vergani, C. Quality of life in older outpatients living alone in the community in Italy. Health Soc. Care Community 2011, 20, 32–41. [Google Scholar] [CrossRef]
- Sakurai, R.; Kawai, H.; Suzuki, H.; Kim, H.; Watanabe, Y.; Hirano, H.; Ihara, K.; Obuchi, S.; Fujiwara, Y. Poor Social Network, Not Living Alone, Is Associated With Incidence of Adverse Health Outcomes in Older Adults. J. Am. Med Dir. Assoc. 2019, 20, 1438–1443. [Google Scholar] [CrossRef]
- Conejero, I.; Olié, E.; Courtet, P.; Calati, R. Suicide in older adults: Current perspectives. Clin. Interv. Aging 2018, 13, 691–699. [Google Scholar] [CrossRef] [Green Version]
- Choi, E.; Han, K.-M.; Chang, J.; Lee, Y.J.; Choi, K.W.; Han, C.; Ham, B.-J. Social participation and depressive symptoms in community-dwelling older adults: Emotional social support as a mediator. J. Psychiatr. Res. 2020, 137, 589–596. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Mundó, J.; Haro, J.M.; Rubio-Valera, M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2018, 246, 82–88. [Google Scholar] [CrossRef] [Green Version]
- Gerst-Emerson, K.; Jayawardhana, J. Loneliness as a Public Health Issue: The Impact of Loneliness on Health Care Utilization among Older Adults. Am. J. Public Health 2015, 105, 1013–1019. [Google Scholar] [CrossRef]
- Kang, H.-J.; Bae, K.-Y.; Kim, S.-W.; Shin, H.-Y.; Shin, I.-S.; Yoon, J.-S.; Kim, J.-M. Impact of Anxiety and Depression on Physical Health Condition and Disability in an Elderly Korean Population. Psychiatry Investig. 2017, 14, 240–248. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.-Y.; Jiang, N.-Z.; Cheung, E.F.; Sun, H.-W.; Chan, R.C. Role of depression severity and impulsivity in the relationship between hopelessness and suicidal ideation in patients with major depressive disorder. J. Affect. Disord. 2015, 183, 83–89. [Google Scholar] [CrossRef]
- Aylaz, R.; Aktürk, U.; Erci, B.; Öztürk, H.; Aslan, H. Relationship between depression and loneliness in elderly and examination of influential factors. Arch. Gerontol. Geriatr. 2012, 55, 548–554. [Google Scholar] [CrossRef]
- Peerenboom, L.; Collard, R.; Naarding, P.; Comijs, H. The association between depression and emotional and social loneliness in older persons and the influence of social support, cognitive functioning and personality: A cross-sectional study. J. Affect. Disord. 2015, 182, 26–31. [Google Scholar] [CrossRef]
- Hsueh, Y.-C.; Chen, C.-Y.; Hsiao, Y.-C.; Lin, C.-C. A longitudinal, cross-lagged panel analysis of loneliness and depression among community-based older adults. J. Elder Abus. Negl. 2019, 31, 281–293. [Google Scholar] [CrossRef]
- Asghar, A.; Iqbal, N. Loneliness matters: A theoretical review of prevalence in adulthood. J. Psychol. 2019, 7, 41–47. [Google Scholar] [CrossRef]
- Luanaigh, C.Ó.; Lawlor, B.A. Loneliness and the health of older people. Int. J. Geriatr. Psychiatry 2008, 23, 1213–1221. [Google Scholar] [CrossRef]
- Alpass, F.M.; Neville, S. Loneliness, health and depression in older males. Aging Ment. Health 2003, 7, 212–216. [Google Scholar] [CrossRef]
- Swami, V.; Chamorro-Premuzic, T.; Sinniah, D.; Maniam, T.; Kannan, K.; Stanistreet, D.; Furnham, A. General health mediates the relationship between loneliness, life satisfaction and depression. Soc. Psychiatry 2006, 42, 161–166. [Google Scholar] [CrossRef]
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerino, E.; Rollè, L.; Sechi, C.; Brustia, P. Loneliness, Resilience, Mental Health, and Quality of Life in Old Age: A Structural Equation Model. Front. Psychol. 2017, 8, 2003. [Google Scholar] [CrossRef] [PubMed]
- Hardy, S.E.; Concato, J.; Gill, T.M. Resilience of Community-Dwelling Older Persons. J. Am. Geriatr. Soc. 2004, 52, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zhang, D.; Wu, M.; Yang, Y.; Xie, H.; Li, Y.; Jia, J.; Su, Y. Loneliness and depression symptoms among the elderly in nursing homes: A moderated mediation model of resilience and social support. Psychiatry Res. 2018, 268, 143–151. [Google Scholar] [CrossRef]
- Liu, J.-C.; Chang, L.-Y.; Wu, S.-Y.; Tsai, P.-S. Resilience mediates the relationship between depression and psychological health status in patients with heart failure: A cross-sectional study. Int. J. Nurs. Stud. 2015, 52, 1846–1853. [Google Scholar] [CrossRef]
- Liu, L.; Gou, Z.; Zuo, J. Social support mediates loneliness and depression in elderly people. J. Health Psychol. 2014, 21, 750–758. [Google Scholar] [CrossRef]
- Arason, B.R.; Sarason, I.G.; Pierce, G.R. Social Support: An Interactional View; John Wiley & Sons: Oxford, UK, 1990. [Google Scholar]
- Wan Mohd Azam, W.M.Y.; Din, N.C.; Ahmad, M.; Ghazali, S.E.; Ibrahim, N.; Said, Z.; Ghazali, A.R.; Shahar, S.; Razali, R.; MPsychMed Famm, T.M. Loneliness and depression among the elderly in an agricultural settlement: Mediating effects of social support. Asia Pac. Psychiatry. 2013, 5, 134–139. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and depression in the elderly: The role of social network. Soc. Psychiatry 2017, 52, 381–390. [Google Scholar] [CrossRef]
- Monthly Population Statistics (Korean). Population Statistics, Yeoju City. 4 April 2022. Available online: https://www.yeoju.go.kr/brd/board/843/L/menu/534?brdType=R&thisPage=1&bbIdx=186957&searchField=&searchText= (accessed on 27 April 2022).
- Luo, F.; Guo, L.; Thapa, A.; Yu, B. Social isolation and depression onset among middle-aged and older adults in China: Moderating effects of education and gender differences. J. Affect. Disord. 2021, 283, 71–76. [Google Scholar] [CrossRef]
- Hoyl, M.T.; Alessi, C.A.; Harker, J.O.; Josephson, K.R.; Pietruszka, F.M.; Koelfgen, M.; Mervis, J.R.; Fitten, L.J.; Rubenstein, L. Development and Testing of a Five-Item Version of the Geriatric Depression Scale. J. Am. Geriatr. Soc. 1999, 47, 873–878. [Google Scholar] [CrossRef]
- Park, H.S.; Deung Jung, Y.J.; Lee, C.I.; Oh, J.E.; Hong, S.H.; Cho, C.Y. Comparing Various Short-Form Geriatric Depression Scales in Elderly Patients. J. Korean Acad. Fam. Med. 2006, 27, 364–369. [Google Scholar]
- Hulin, C.; Netemeyer, R.; Cudeck, R. Can a Reliability Coefficient Be Too High. J. Consum. Psychol. 2001, 10, 55–58. [Google Scholar]
- De Jong Gierveld, J.; van Tilburg, T. A 6-Item Scale for Overall, Emotional, and Social Loneliness. Res. Aging 2006, 28, 582–598. [Google Scholar] [CrossRef]
- National Institute on Aging (NIA). What Do We Know about Healthy Aging? 23 February 2022. Available online: https://www.nia.nih.gov/health/what-do-we-know-about-healthy-aging (accessed on 5 April 2022).
- Vafiadis, D.; How Sleep Affects Your Health. National Council on Aging. 8 March 2021. Available online: https://www.ncoa.org/article/how-sleep-affects-your-health/ (accessed on 5 April 2022).
- Hassani, D.; Arya, L.; Andy, U. Continence: Bowel and Bladder and Physical Function Decline in Women. Curr. Geriatr. Rep. 2020, 9, 64–71. [Google Scholar] [CrossRef]
- Meng, Q.; Xie, Z.; Zhang, T. A signle-item self-rated health measure correlates with objective health status in the elderly: A survey in suburban Beijing. Front. Public Health 2014, 2, 27. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Song, J.; Brytek-Matera, A.; Zhang, H.; He, J. The Relationships between Sleep and Mental and Physical Health of Chinese Elderly: Exploring the Mediating Roles of Diet and Physical Activity. Nutrients 2021, 13, 1316. [Google Scholar] [CrossRef]
- Acar Tek, N.; Karaçil-Ermumcu, M.Ş. Determinants of Health Related Quality of Life in Home Dwelling Elderly Population: Appetite and Nutritional Status. J. Nutr. Health Aging 2018, 22, 996–1002. [Google Scholar] [CrossRef]
- Byles, J.; Millar, C.J.; Sibbritt, D.W.; Chiarelli, P. Living with urinary incontinence: A longitudinal study of older women. Age Ageing 2008, 38, 333–338. [Google Scholar] [CrossRef] [Green Version]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Cosco, T.D.; Kaushal, A.; Richards, M.; Kuh, D.; Stafford, M. Resilience measurement in later life: A systematic review and psychometric analysis. Health Qual. Life Outcomes 2016, 14, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Moser, A.; Stuck, A.E.; Silliman, R.; Ganz, P.A.; Clough-Gorr, K.M. The eight-item modified Medical Outcomes Study Social Support Survey: Psychometric evaluation showed excellent performance. J. Clin. Epidemiol. 2012, 65, 1107–1116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preacher, K.J.; Hayes, A.F. Asymptotic and Resampling Strategies for Assessing and Comparing Indirect Effects in Multiple Mediator Models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Preacher, K.J.; Kelley, K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychol. Methods 2011, 16, 93–115. [Google Scholar] [CrossRef]
- Miocevic, M.; O’Rourke, H.P.; Mackinnon, D.P.; Brown, H.C. Statistical properties of four effect-size measures for mediation models. Behav. Res. Methods 2018, 50, 285–301. [Google Scholar] [CrossRef] [Green Version]
- Zhao, X.; Lynch, J.G., Jr.; Chen, Q. Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis. J. Consum. Res. 2010, 37, 197–206. [Google Scholar] [CrossRef]
- Byeon, H. Relationship between Physical Activity Level and Depression of Elderly People Living Alone. Int. J. Environ. Res. Public Health 2019, 16, 4051. [Google Scholar] [CrossRef] [Green Version]
- Sung, M.-H.; Lim, Y.M.; Joo, K.-S. The Relationship between Social Support and Loneliness in Elderly Women Living Alone. J. Korean Public Health Nurs. 2011, 25, 95–106. [Google Scholar]
- Sonnenberg, C.; Deeg, D.; van Tilburg, T.; Vink, D.; Stek, M.; Beekman, A. Gender differences in the relation between depression and social support in later life. Int. Psychogeriatr. 2012, 25, 61–70. [Google Scholar] [CrossRef]
- Nam, E.J.; Lee, J.-E. Mediating Effects of Social Support on Depression and Suicidal Ideation in Older Korean Adults With Hypertension Who Live Alone. J. Nurs. Res. 2019, 27, e20. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness Matters: A Theoretical and Empirical Review of Consequences and Mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [Green Version]
- Alexander, B.B.; Rubinstein, R.L.; Goodman, M.; Luborsky, M. A Path Not Taken: A Cultural Analysis of Regrets and Childlessness in the Lives of Older Women. Gerontologist 1992, 32, 618–626. [Google Scholar] [CrossRef]
- Bobrowicz-Campos, A. Capacidade de Rastreio da Escala de Depressão Geriátrica com 10 e 5 itens. Rev. Soc. Esp. Farm. Hosp. 2018, 4, 29–39. Available online: https://www.redalyc.org/journal/3882/388256613004/388256613004.pdf (accessed on 2 March 2022).
- Tully, M.A.; McMullan, I.I.; Blackburn, N.E.; Wilson, J.J.; Coll-Planas, L.; Deidda, M.; Caserotti, P.; Rothenbacher, D.; and on behalf of the SITLESS Group. Is Sedentary Behavior or Physical Activity Associated With Loneliness in Older Adults? Results of the European-Wide SITLESS Study. J. Aging Phys. Act. 2019, 28, 549–555. [Google Scholar] [CrossRef]
- Kim, J.; Lee, J.-E. Social Support and Health-Related Quality of Life among Elderly Individuals Living Alone in South Korea: A Cross-Sectional Study. J. Nurs. Res. 2018, 26, 316–323. [Google Scholar] [CrossRef]
- Won, S.; Kim, H. Social participation, health-related behavior, and depression of older adults living alone in Korea. Asian Soc. Work Policy Rev. 2019, 14, 61–71. [Google Scholar] [CrossRef]
- Fullen, M.C.; Gorby, S.R. Reframing resilience: Pilot evaluation of a program to promote resilience in marginalized older adults. Educ. Gerontol. 2016, 42, 660–671. [Google Scholar] [CrossRef]
- Gonyea, J.G.; Curley, A.; Melekis, K.; Levine, N.; Lee, Y. Loneliness and Depression among Older Adults in Urban Subsidized Housing. J. Aging Health 2016, 30, 458–474. [Google Scholar] [CrossRef]
| Variables | n (%) or Mean (SD/Min, Max) | |
|---|---|---|
| Age | Years | 80.02 (5.89/64, 94) |
| Education | None | 194 (63.0%) |
| Primary school | 91 (29.5%) | |
| Middle school | 16 (5.2%) | |
| High school over | 7 (2.3%) | |
| Religion | No | 139 (45.1%) |
| Yes | 169 (54.9%) | |
| Duration of living alone | Years | 13.57 (114.39/0.2, 46) |
| Depression | Values | 2.37 (1.73/0, 5) |
| Loneliness | 3.99 (1.69/0, 6) | |
| Subjective physical health | 3.68 (1.27/0, 5) | |
| Resilience | 12.56 (2.85/5, 20) | |
| Social support | 17.00 (6.67/5, 40) | |
| Loneliness | Physical Health | Resilience | Social Support | Depression | |
|---|---|---|---|---|---|
| Loneliness | 1 | −0.295 * | −0.345 * | −0.315 * | 0.428 * |
| Physical health | - | 1 | 0.237 * | 0.153 * | −0.442 * |
| Resilience | - | - | 1 | - | −0.368 * |
| Social support | - | - | - | 1 | −0.310 * |
| Depression | - | - | - | - | 1 |
| Variable/Effect | b | SE | t | p-Value | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Boot-LLCI | Boot-ULCI | |||||
| loneliness → physical health (a1) | −0.218 | 0.04 | −5.31 | <0.0001 | −0.299 | −0.137 |
| loneliness → resilience (a2) | −0.564 | 0.09 | −6.26 | <0.0001 | −0.742 | −0.387 |
| loneliness → social support (a3) | −1.257 | 0.21 | −5.89 | <0.0001 | −1.676 | −0.838 |
| physical health → depression (b1) | −0.429 | 0.06 | −6.27 | <0.0001 | −0.563 | −0.294 |
| resilience → depression (b2) | −0.108 | 0.03 | −3.36 | 0.001 | −0.171 | −0.045 |
| social support → depression (b3) | −0.034 | 0.01 | −2.55 | 0.011 | −0.061 | −0.008 |
| loneliness → physical health→ depression (a1b1) | 0.094 | 0.02 | - | - | 0.055 | 0.137 |
| loneliness → resilience → depression (a2b2) | 0.059 | 0.02 | - | - | 0.023 | 0.101 |
| loneliness → social support → depression (a3b3) | 0.049 | 0.02 | - | - | 0.016 | 0.085 |
| Effects | ||||||
| Direct Effect (c’) | 0.242 | 0.05 | 4.46 | <0.0001 | 0.135 | 0.349 |
| Total Indirect * | 0.197 | 0.03 | - | - | 0.138 | 0.262 |
| Total Effect (c) | 0.439 | 0.05 | 8.19 | <0.0001 | 0.334 | 0.545 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, Y.M.; Baek, J.; Lee, S.; Kim, J.S. Association between Loneliness and Depression among Community-Dwelling Older Women Living Alone in South Korea: The Mediating Effects of Subjective Physical Health, Resilience, and Social Support. Int. J. Environ. Res. Public Health 2022, 19, 9246. https://doi.org/10.3390/ijerph19159246
Lim YM, Baek J, Lee S, Kim JS. Association between Loneliness and Depression among Community-Dwelling Older Women Living Alone in South Korea: The Mediating Effects of Subjective Physical Health, Resilience, and Social Support. International Journal of Environmental Research and Public Health. 2022; 19(15):9246. https://doi.org/10.3390/ijerph19159246
Chicago/Turabian StyleLim, Young Mi, Juha Baek, Sungmin Lee, and Jung Sug Kim. 2022. "Association between Loneliness and Depression among Community-Dwelling Older Women Living Alone in South Korea: The Mediating Effects of Subjective Physical Health, Resilience, and Social Support" International Journal of Environmental Research and Public Health 19, no. 15: 9246. https://doi.org/10.3390/ijerph19159246
APA StyleLim, Y. M., Baek, J., Lee, S., & Kim, J. S. (2022). Association between Loneliness and Depression among Community-Dwelling Older Women Living Alone in South Korea: The Mediating Effects of Subjective Physical Health, Resilience, and Social Support. International Journal of Environmental Research and Public Health, 19(15), 9246. https://doi.org/10.3390/ijerph19159246







