Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review
Abstract
:1. Introduction
- Individual factors: Bone misalignments with little evidence [7,15,16] and muscle imbalances, increased strength of the hamstrings relative to the quadriceps, as well as anserine paw tendinopathy [15,17,18], as weakness in the quadriceps [19,20] and increased strength in the hip abductor muscles compared to other thigh muscles [12].
- Psychosocial factors: Anxiety and depression may be indirect risk factors for PFPS.
2. Materials and Methods
2.1. Eligibility Criteria
Search Characteristics
2.2. Characteristics of Accepted Studies
2.2.1. Participants
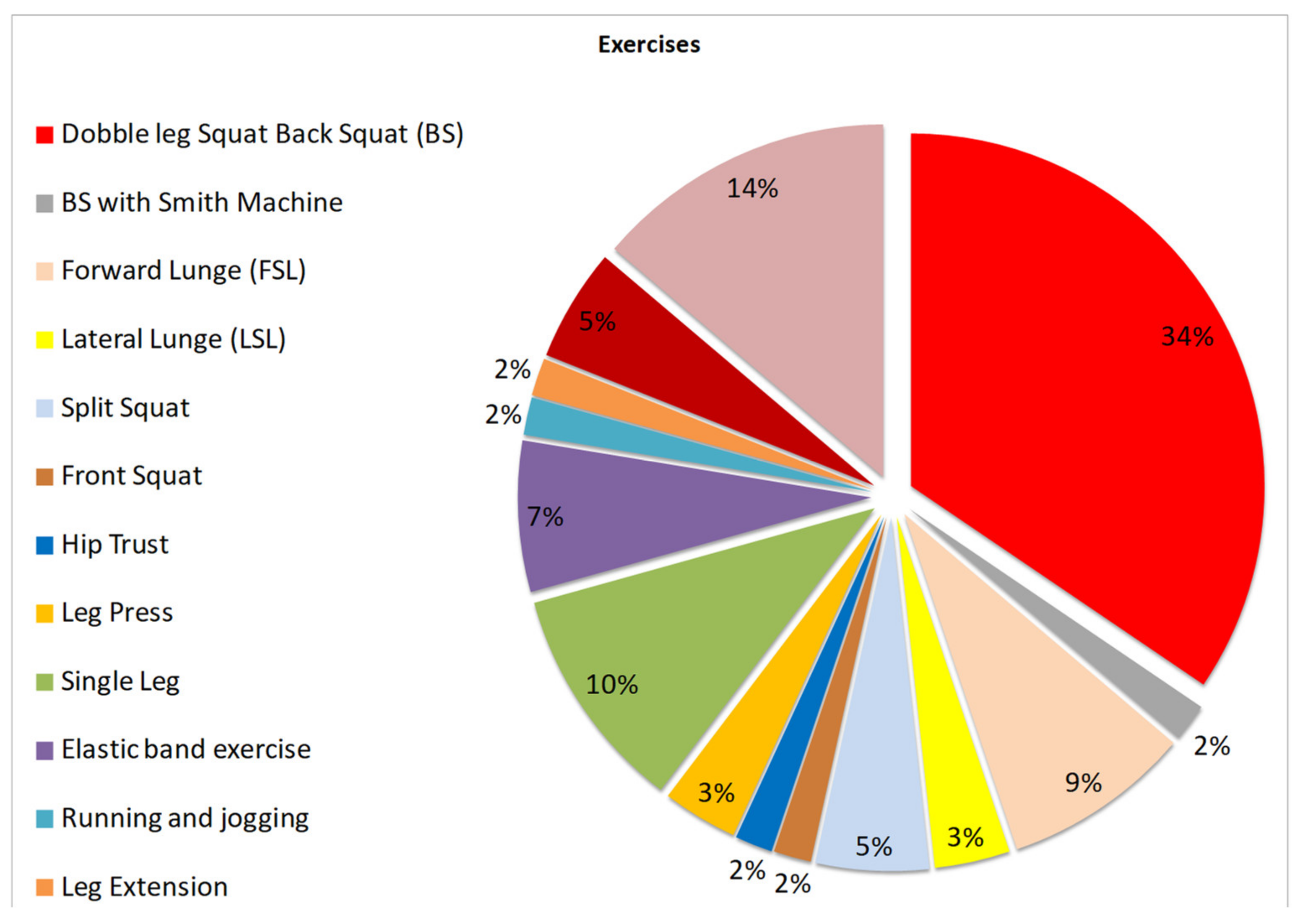
2.2.2. Type of Interventions
- (a)
- Assessment of thigh, leg, and gluteal muscles through electromyography (EMG) and/or video analysis and/or motion kinetics;
- (b)
- Evaluation of knee or hip joints during squatting movements by video and/or kinetic analysis;
- (c)
- The patellofemoral pain syndrome and its relationship with the different movements of squatting or knees bending when evaluated by the methods described in (a) and (b);
- (d)
- Pain assessment in patients with PFPS with the methods defined in (a) and (b);
2.2.3. Design of Accepted Studies
2.3. Information Sources
2.4. Search Strategy
- squat AND (“musculoskeletal disorder” OR “musculoskeletal diseases”) AND worker
- “squat technique”;
- squat AND syndrome AND worker;
- squat AND worker AND Knee AND NOT osteoarthritis;
- squat AND knee AND syndrome AND NOT osteoarthritis AND NOT “low back”;
- “knee pain” AND worker
- (“musculoskeletal disorder” OR “musculoskeletal disease”) AND “patellofemoral pain” AND NOT Osteoarthritis AND NOT “low back” AND NOT ankle;
- squat AND “functional task”;
- “functional task” AND “patellofemoral pain” AND NOT Osteoarthritis AND NOT ankle AND NOT “low back”;
- “patellofemoral pain” AND worker AND NOT Osteoarthritis AND NOT ankle AND NOT “low back”.
2.5. Study Records
2.5.1. Data Management
2.5.2. Selection Process
- Inclusion of healthy humans or those with knee injuries but without prostheses or orthotics.
- Medical evaluation or by another qualified professional.
- Description of the relationship between knee flexion exercises such as squat and PFPS.
- Approach to the musculature of the thigh, leg, and gluteus, evaluated by EMG and/or video analysis and movement kinetics.
- Assessment of knee or hip joints during movement using video analysis and motion kinetics.
- Study of patellofemoral disease and its relationship with any type of physical exercise.
2.6. Data Collection Process
- General information: authors and year of publication.
- Population: athletes/workers and type of activities performed.
- Sample: size, sex distribution, mean age, and BMI.
- Study characteristics: objectives, evaluated parameters, procedures/methods, equipment and software, and conclusions.
- Parameters: type of exercise, muscles and joints involved, tensions in muscle tendons, applied interventions, results, and study characteristics.
- Quality assessment: possible risks of bias (selection, precision, information, researcher), reports (assessment of the overall quality of the study), external validity (assessment of whether the results of the study are generalisable), internal validity (assessment of bias due to study sample selection and/or confounding), and power (assessment of whether study results can be obtained by chance).
- Studies’ results and the direct or indirect relationship with the purpose of the review.
2.7. Prioritisation and Outcomes
- Corresponding to the direct analysis of tensional overload in the patellofemoral joint;
- Tensional overload in the patellofemoral joint through maximum isovolumetric contraction via electroneuromyography.
- Pain reduction and mobility improvement in PFPS patients, after exercise intervention.
2.8. The Risk of Bias and Quality Assessment
3. Results
3.1. Article Selection
3.2. Risk of Bias
4. Discussion, Summary of Evidence
- The anterior translation of the knee with the anterior tibial line in front of the ipsilateral toes line during any squat type [22,24,33,46,49,53,65]. Thus, a difference of strength on the patellar tendon of 18.8% compared to 11.5% was found during the forward lunge squat exercise when the anterior tibial line was translocated from the knee to the front tibial line anterior to the ipsilateral toes line [34].
- Muscle imbalance of the thigh muscles, posteroanterior, and stabilisers such as gluteus medius and vastus medialis oblique muscle (VMO) demonstrated via EMG by the ability to contract. According to some studies, this imbalance was the cause of the most significant pain in patients with PFPS compared to people without the syndrome. It is, therefore, considered one of the main aggravating factors [37,38,60].
5. Conclusions
6. Significance for Practice
7. Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Ref. | Study Characteristics | Population | Study Result | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of Exercise | Assessed Parameters | Athletes/Workers | Characteristics | Gender | Mean Age (Years) | BMI Kg/m2 | Relationship with the Objective of SR | |||||||||
| Sample | Ctr | Direct | Indirect | |||||||||||||
| [22] | 1—Back Squat (Double squat-SQ), Wise squat (WS), narrow squat (NS) 2—Leg Press (LP), Foot different position (high (LPH), Lower (LPL), Wise (WS), Narrow (NS). | Kinetics/Kinematics/Force Muscle/Force on Join/Force Tendon (Anterior cruciate ligament tension: ACL, posterior cruciate ligament: LCL, Tibiofemural tension: TB, Patellofemoral tension: PF) | Physically fit and Healthy subject | Lifters experienced in performing the squat and Legg Press | Male: 10 | NA | Male: 29.6 ± 6.5 | Male: 29.84 | Patellofemoral joint stress at knee flexion— Megapascal Pressure Unit (MPa) 20°—0.92 MPa, 30°—1.98 MPa, 60°—7.00 MPa, 90°—10.21 MPa | NA | ||||||
| [23] | Forward Lunge (FL) Lateral Lunge (LL) | “muscle activation patterns joint moments, powers, impulse mechanical energy expenditure.” | Healthy Subject | NM | Male: 9 Female: 11 | NA | Overall: 75 ± 4.4 | Overall: 28.49 | Knee Peak Power (W·kg−1) | Peak knee power generated during FL was 46.2% greater than during the LL | ||||||
| [24] | Forward lunge (FL) (with and without a stride) Side (Lateral) lunges (LL) (with and without a stride) | Muscle activation patterns Kinematic Force | Healthy Subject | NM | Male: 9 Female: 9 | NA | Male: 29 ± 7 Female: 25 ± 2 | Male: 25.77 Female: 22.22 | Patellofemoral force (N) values approximate/by knee angle for knee flexing phase | NA | ||||||
| angle | Without stride | With stride | ||||||||||||||
| FL | LL | FL | LL | |||||||||||||
| 0° 10° 20° 30° 40° 50° 60° 70° 80° 90° | 69 159 207 356 628 1059 1524 1944 2161 2185 | 46 127 194 332 573 926 1533 2009 2493 2668 | 74 220 301 459 732 1150 1683 2058 2344 2411 | 49 80 120 242 481 856 1378 1896 2267 2419 | ||||||||||||
| [25] | Back Squat (BS) Barbell Hip Thrust | Range of Motion (ROM) to Knee and Hip Joint. Kinematic analyses movement Muscle activation patterns Upper Gluteus Maximus-(UGM) Lower Gluteus—(LG) Biceps Femoris—(BF) Vastus Lateralis—(VL) | Healthy subject | Subject with strength training experience | Female: 13 | NA | Overall: 28.9 ± 5.11 | Overall: 21.97 | Comparison between EMG-verified Thigh Muscles Peak Strength, Back Squat and Barbell Hip Thrust | NA | ||||||
| Back squat | UGM | LG | BF | VL | ||||||||||||
| 84.85 ± 42.91 | 129.60 ± 60.45 | 37.50 ± 18.39 | 243.92 ± 121.63 | |||||||||||||
| Hip Thrust | 171.75 ± 90.99 | 215.85 ± 83.76 | 86.87 ± 38.81 | 215.83 ± 193.89 | ||||||||||||
| [26] | Back Squat with load and without load |
| Healthy Subject | NM | Male: 6 Female: 9 | NA | Overall: 26 ± 5 | Overall: 24.69 | Patellofemoral joint stress at knee flexion—90° | “The results indicate that patellofemoral joint stress increases linearly with increasing knee flexion angle and decreases with decreasing knee flexion angle.” | ||||||
| Concentric phase | Eccentric phase | |||||||||||||||
| load | unload | Load | unload | |||||||||||||
| 13.0 MPa | 9.3 MPa | 13.06 MPa | 9.06 MPa | |||||||||||||
| Descending | Ascending | |||||||||||||||
| FL | LL | FL | LL | |||||||||||||
| 0.71 (0.40) | 0.52 (0.26) | 0.76 (0.35) | 0.48 (0.25) | |||||||||||||
| [33] | ”Split squats with an additional 25% body weight load applied using a barbell.” | Range of Motion (ROM) to Knee and Hip Joint. Kinematic analyses movement. Kinetic movement to split squat | Healthy subject | Students | Male: 5 Female: 6 | NA | Overall: 24.9 ± 2.5 | NI | Front leg relation between tibial angle and knee tension force (N∙m/kg, positive for external flexion) | NA | ||||||
| leg length | 60° | 75° | 90° | 105° | ||||||||||||
| L-1 | 1.46 ± 0.14 | 1.38 ± 0.17 | 1.19 ± 0.22 | NM | ||||||||||||
| L-2 | 1.40 ±.17 | 1.33 ± 0.20 | 1.14 ± 0.19 | NM | ||||||||||||
| L-3 | 1.28 ± 0.12 | 1.19 ± 0.17 | 1.13 ± 0.21 | 0.80 ± 0.16 | ||||||||||||
| Split squat step lengths of l1 = 55% of leg length (ll), l2 = 70% ll, and l3 = 85% ll and four tibia angles (a) were evaluated | ||||||||||||||||
| [34] | “Forward Lunge—with the Knee translated in front of the toes (FSL-FT) Forward Lunge—with the Knee translated behind the toes (FSL-BT).” |
| healthy subject | Volunteers | Female: 25 | NA | Overall: 22.69 ± 0.74 | Overall: 21.55 | The peak patellar tendon stress, stress impulse, quadriceps force, knee moment, knee flexion, and ankle dorsiflexion angle were significantly greater during the FSL-FT than the FSL-BT. The peak patellar tendon stress rate did not differ between the FSL-FT and FSL-BT | NA | ||||||
| [35] | Back Squat with weight | Anthropometric data./3D knee kinematics. (Tibiofemoral joint kinematics.)/“Ground reaction forces (A—Tibiofemoral joint moment, B—Patellofemoral joint reaction force) Patellofemoral joint stress.” | Healthy Subject | Collegiate women athletes | Female: 5 | NA | Female: 19 ± 1.4 | Female: 23.49 | Patellofemoral joint stress at knee Flexion: 72.8° = 4319.2 N 91.5° = 5065.7 N 109.7° = 5097.1 N | NA | ||||||
| [36] | Squatting Running | 1—joint kinematics 2—kinetics 3—muscle forces pPFJS indicates the peak patellofemoral joint stress (MPa); PFJS-TI = patellofemoral joint stress time integral (MPa s); (pQF) indicates the peak quadriceps force (pQF) | Healthy subject | Subject with strength training experience | Female: 11 | NA | Overall: 22 ± 1.8 | Overall: 22.47 | Squat trials | Methods | NA | |||||
| ID—Inverse dynamics | IDO—Inverse dynamics and static optimisation | |||||||||||||||
| PPFJS | 9.81 (sd 3.36) | 17.06 (sd 4.34) | ||||||||||||||
| PFJS-TI | 7.51 (sd 1.98) | 12.87 (sd 2.33) | ||||||||||||||
| pQF | 3.81 (sd 0.72) | 5.16 (sd 0.82) | ||||||||||||||
| [37] | “Squat with three displacements. Displacing the Knee anteriorly (AP malaligned), displacing the Knee medially (ML malaligned). Squats with control alignment (control).” | 1—electromyographic muscle activation during a neutrally aligned squat | healthy subject | Volunteers | Male: 9 Female: 19 | NA | Overall: 21.5 ± 3 | Overall: 22.73 | The misaligned movement, such as the anterior translation of the tibia concerning the foot on the same side, has been shown to be the moment of greatest knee joint overload, requiring excessive activity of the knee's stabilising muscles. It has been shown that the moment of decreased muscle activity in the quadriceps is the moment when the contact forces between the patella are greatest. | NA | ||||||
| [38] | “Exercise 1–3 with an elastic band, hip abductor exercise, hip external rotator exercise. Leg extension, Two-legged Squat (Double Legged).” | 1—muscle activation patterns (EMG). (VL, VMO, and gluteus medius muscles) | Subject with PFPS | Volunteers Students | Female: 30 | NA | Overall: 24.93 ± 4.91 | Overall: 22.95 | NA | VMO muscle activation was induced during the closed kinetic chain knee movements, and the VL/VMO was 1 in Close and Open chain exercise | ||||||
| [39] | (WL)Forward (Walking) lunge (A)Dumbbell = Ipsi-lateral (B)Dumbbell = Contra-lateral (SS)Split Squat | “Range of Motion (ROM) to Knee and Hip Joint, Kinematic analyses movement, Kinetic by movement to split squat, Muscle activation patterns, PT = peak torque obtained during a 5-second isometric contraction at the stated joint angle” VM—Vastos Medialis Muscle, VL—Vastos Lateralis Muscle | Athletes and Healthy subject | Athletes: Powerlifters competing in the Czech championships during | 14 | 14 | InT: 30.02 ± 5.60 C: 28.35 ± 5.71 | InT: 27.22 C: 24.01 | NA | This finding suggests that contralateral WLs may increase the muscle imbalance between the VM and VL, especially in RT individuals. Alternatively, contra-lateral WLs appear to benefit Gmed and VL strengthening if such strengthening is the aim of a training program. | ||||||
| [40] | “Back Squat with 3 different distances to foot and 9 different positions”: “Narrow (NW)—0°, 21°, 42° Hip distance (HS)—0°, 21°, 42° Wide (WS)—0°, 21°, 42°.” | 1—Kinematics 2—range of motion and moments (9 different moments) | Physically fit subject | Volunteers do work out on gym (novice and experienced) | Novice: (Male: 10/Female: 11) Experienced: (Male: 10/Female: 11) | NA | Novice: 25 ± 6 Experienced: 25 ± 5 | Novice: 22.41 Experienced: 22.76 | NA | We would recommend that a moderate foot placement angle (approximately 20°) in combination with a moderate stance width (with feet approximately shoulder-width apart) should be used, and extreme positions would be avoided | ||||||
| [41] | Straight leg raise—freeload (OCK) semi-squat exercises—bodyweight (CKC) |
| Students with PFPS | University students with a diagnosis of patellar chondromalacia | Female: 16 CKC Female: 16 OKC | NA | NI | NI | “The results indicate a significant increase of thigh circumference in the semi-squat group at 5 cm (p = 0.002) and 10 cm (p = 0.01) above the patella compared to the SLR group”. | “The exercise may improve patellofemoral joint performance by improving quadriceps muscle strength and correcting patellar alignment.” | ||||||
| [42] | 1—Sling-Based Open Kinetic Knee Extension Exercise (1) 2—Sling-based closed kinetic knee extension exercise (2) 3—Sling-based hip adduction exercise (3) | Muscle activation patterns (MVC), maximal voluntary contraction | Subject with PFPS | Rehabilitation Center patients | Male: 30 Female: 30 | NA | Male: 21.19 ± 0.68 Female: 21.12 ± 0.74 | Male: 21.16 Female: 20.26 | Electromyography analysis of MVC for open and closed kinetic knee extension and hip adduction exercises | For Chang, “the main factor causing patellofemoral pain is an imbalance of VMO and VL muscle, leading to excessive lateral tracking of the patella.” | ||||||
| Muscle | Exercise | |||||||||||||||
| (1) | (2) | (3) | ||||||||||||||
| VMO | 0.60 ± 0.20 | 0.71 ± 0.20 | 0.54 ± 0.13 | |||||||||||||
| VL | 0.76 ± 0.12 | 0.72 ± 0.13 | 0.56 ± 0.14 | |||||||||||||
| VMO: VL | 0.80 ± 0.31 | 1.00 ± 0.28 | 1.02 ± 0.35 | |||||||||||||
| [43] | “(1) short arc quad with neutral hip position (SAQN), (2) short arc quad with externally rotated hip position (SAQER), (3) medial tibial rotation (MTR) (4) hip adduction (HA)”. | 1—muscle activation patterns (EMG) | Worker with PFPS | Automotive workers | Male: 11 | NA | Overall: 38.45 ± 12.73 | Overall: 22.80 ± 4.69 | NA | Mean iEMG activity of VMO muscle is more than that of VL muscle during all biomechanical rehabilitative exercises. However, one-way ANOVA with repeated measures indicates that mean iEMG activity of VMO muscle is significantly higher than that of VL muscle during SAQER only | ||||||
| [44] | “Single-Leg Squat, Single-Leg Landing, Hip abductor strength Free, Hip Abductors strength with load, This method sequentially challenges the control of the knee position during squatting by gradually progressing from double-leg to single-leg squatting”. | 1—Kinematics to the joint Knee, hip. | Worker | Military volunteers | Male: 11 Female: 4 | Male: 10 Female: 5 | AG: 30.3 (8.8) Control: 29.6 (9.7) | AG:30.3 0 Control: 23.30 | NA | NA | ||||||
| [45] | Squat: Two variation knees before the toes (SBT) knees to go past the toes (SPT). | patellofemoral joint force (PFJF) and quadriceps force (QF) patellofemoral joint reaction force (PFJRF) centre of pressure (COP) knee flexion range of motion (ROM) A/P—anteroposterior | healthy females | Volunteers | Female: 25 | NA | Overall: 22.69 ± 0.74 | Overall: 21.45 | The PFJS, reaction force, and quadriceps force magnitudes were higher (p ˂ 0.001) during SPT than during the SBT technique. | NA | ||||||
| [46] | Forward lunge with a long step (FLF) Forward lunge with a short step(FLS) | Muscle activation patterns Kinematic Force | Healthy Subject | NM | Male: 9 Female: 9 | NA | Male: 29 ± 7 Female: 25 ± 2 | Male: 25.77 Female: 22.22 | Patellofemoral force (N) values approximate/by Knee angle for knee flexing phase | NA | ||||||
| angle | Without stride | With stride | ||||||||||||||
| FLF | FLS | FLF | FLS | |||||||||||||
| 0° 10° 20° 30° 40° 50° 60° 70° 80° 90° | 69 159 207 356 628 1059 1524 1944 2161 2185 | 93 144 233 377 629 1051 1660 2335 2836 3039 | 106 212 306 440 688 1106 1585 2172 2567 2648 | 62 97 147 298 573 1006 1585 2172 2567 2648 | ||||||||||||
| [47] | Back Squat Front Squat | muscle activation patterns (EMG) kinematics of Knee and hip joints (Video) | Athlete | NM | Male: 20 | NA | NM | NM | EMG activities between back squats and front squats during the descending and ascending phases, performed with 1RM loads | “Instead of the load, the level of effort in volunteers’ muscle actions determine the degree of motor unit activity (Carpinelli, 2008); consequently, the level of EMG signalling increases. In addition, higher loads can increase the strain on the patellofemoral joints, increasing the risk of injury during the squat.” | ||||||
| Muscle | descending phases | ascending phases | ||||||||||||||
| Back Squat | Front Squat | Back Squat | Front Squat | |||||||||||||
| Rectus femoris | 37.9 ± 12.1 | 46.4 ± 24.4 | 36.0 ± 13.8 | 46.7 ± 19.4 | ||||||||||||
| Vastus medialis | 48.3 ± 14.3 | 53.1 ± 19.3 | 49.3 ± 13.9 | 58.9 ± 17.1 | ||||||||||||
| Vastus lateralis | 45.9 ± 13.9 | 48.0 ± 15.8 | 48.5 ± 17.2 | 56.2 ± 22.2 | ||||||||||||
| [48] | single-leg squat single-leg stance | 1—muscle activation patterns (EMG) | Subject with/without PFPS | Volunteers | Male: 18 | Male: 18 | with PFP: 24.2 ± 4.4 controls: 213.5 ± 3.8 | PFP: 23.8 Control: 23.9 | Compared to healthy subjects, males with PFP demonstrated altered gluteus medius, VMO, and VL muscle activity during single-leg stance and single-leg squat. | NA | ||||||
| [49] | 1—Muscle activation patterns 3—Kinematic | Healthy Subject | NM | Male: 9 Female: 9 | NA | Male: 29 ± 7 Female: 25 ± 2 | Male: 25.00 Female: 22.20 | Patellofemoral joint stress (MPa) approximate | “The primary cause of the greater patellofemoral force and stress between 90- and 70-knee angles in the wall squat short compared with the one-leg squat was greater quadriceps force during the wall squat short.” | |||||||
| angle | Descending | Ascending | ||||||||||||||
| SL | WSL | WSS | SL | WSL | WSS | |||||||||||
| 60° 70° 80° 90° | 5.3 6.6 7.0 7.2 | 4.5 6.7 7.5 7.3 | 4.5 6.6 7.6 8.0 | 5.8 7.3 7.0 7.5 | 8.0 9.5 8,3 7.5 | 6.3 8.8 9.5 9.2 | ||||||||||
| [50] | “Two-legged (double-legged), Squat (three squat depths (20°, 50° and 80° of knee flexion) while following three knee movement paths (neutral, varus or valgus).” | Kinematic for Squat with three variation muscle activation patterns (EMG) | Healthy subject | NM | Male: 7 Female: 11 | NA | Overall: 22.39 ± 2.25 | Overall: 22.49 | Muscle activation, vastus medialis obliquus (VMO) and vastus lateralis (VL) and VMO: VL ratio (neutral) | NA | ||||||
| Angle | VMO | VL | VMO: VL | |||||||||||||
| 20° | 31.91 | 138.76 | 1.35 | |||||||||||||
| 50° | 74.45 | 267.52 | 1.69 | |||||||||||||
| 80° | 146.16 | 512.68 | 1.84 | |||||||||||||
| [51] | Single-limb squat | Kinematic muscle activation patterns (EMG) Pain | Women not athletes with PFPS and Hip Joint Pain HIP (HJP) | Volunteers | −20 PFPS −14 HJP | −20 knee Control −13 Control Hip | 18–40 years | 17.82–32.30 | Greater external rotation of the knee was correlated with greater knee pain in patellofemoral pain syndrome. All women with dynamic valgus movement had pain when performing single-leg squat exercises. | NA | ||||||
| [52] | DoubleLegged—two variation Free weight squat Smith machine squat. | 1—Muscle activation patterns 3—Kinematic | Healthy Subject | Subject with strength training experience (2–5 years) | Male: 3 Female: 3 | NA | Overall: 22 ± 1.2 | Overall: 24.85 | “The free weight squat elicited a 34% higher EMG MAV from the gastrocnemius, a 26% higher EMG MAV from the biceps femoris, and a 49% higher EMG MAV from the vastus medialis compared to the Smith machine squat.” | “Our finding of a higher biceps femoris and gastrocnemius activity during the free weight squat may be attributed to the increased role that the knee flexors play in stabilising and supporting the ankle, knee, and hip joints in a more unstable.” | ||||||
| [53] | Two-legged Squat (Double legged) 1—Control, two-legged squat 2—Valgus dynamic Squat 3—Knee Anterior Displacement Squat | Kinematic for Squat with three variation Torque to force by knee joint, hip joint, trunk joint, ankle joint | Healthy subject | Volunteers | Male: 11 Females: 19 | NA | Overall: 21.4 ± 3 | Overall: 22.77 | NA | The overload in W/kg on the knee presents greater intensity in the knee flexion movement with anterior malaligned, followed by medial malaligned concerning the control (neutral). | ||||||
| [54] | single-leg squat (SLS) step-down task (SDT) PENS (electrical neuromuscular stimulation) | Kinematic muscle activation patterns (EMG) Pain | Women not athletes with PFPS | Volunteers | 8 | 8 | 23.3 ± 4.9 | 24.1 | Rehabilitation with neuromuscular activation via PENS (electrical neuromuscular stimulation) was beneficial in the patient with PFPS, decreasing the activation of the stabilising muscles in the single-leg squat movement and decreasing pain when performing the movement. | NA | ||||||
| [55] | “1—Semi Squat with hip adduction and internal rotation-CKC 2—Quadriceps isometric in supine position-OKC 3—Terminal knee extension with elastic band—KC 4—Terminal knee extension in supine position OKC 5—Adductor squeeze in crook lying (squeeze the ball) (odd weeks)—CKC 6—Hip adduction in lateral decubitus position (even weeks)–OKC” | 1—Subjective symptoms, 2—functional performance, 3—knee flexion during stair ascent and descent by the patients. 4—VAS—Visual Analog Scale 5—Kujala Questionnaire | Patients | Patients with PFPS | Male: 5 Female: 9 | Male: 5 Female: 9 | Interv.: 25.7 ± 2.6 Control: 26.8 ± 2.3 | Interv: 23.56 Control: 23.19 | Clinical outcomes in the patients with patellofemoral pain syndrome (value). | NA | ||||||
| Assessment | Group Exercise | Control | ||||||||||||||
| Intervencion | Pre | Pós | Pre | Pós | ||||||||||||
| Pain while ascending (VAS) | 49.8 | 19.6 | 51.3 | 54.4 | ||||||||||||
| Pain while descending (VAS) | 51.3 | 19.8 | 50.2 | 54.2 | ||||||||||||
| AKPS (Kujala) | 65.2 | 85.8 | 61.5 | 59.6 | ||||||||||||
| [56] | “1—Squat (until 60° degree) 2—Intervention exercise: table hip abduction with 60°, 15° of hip extension and 30° of external hip rotation with the Knee extended. The subject returned his lower limb to a parallel position.” | Squat range of motion Maximal isometric voluntary contraction (MVIC) | Healthy subject | Volunteers | Female: 11 | NA | Overall: 23.88 ± 2.64 | Overall: 21.75 | NA | During the squat exercise, the average activation ranged from 18.43% to 27.75% MVIC. The ability to activate the gluteus medius increased by 19.99 points after the adaptation exercises. However, the increase in isometric exercise varied with average activation ranging from 24.16% to 25.30% and from 18.43% to 19.70% in the dynamic exercise (squat). Thus, the muscular activity of isometric exercises is greater. | ||||||
| [57] | Knee Flexion 0°–30° | Noninvasive patellar tracking study using a “C”-arm computed tomography (CT) scanner | Women not athletes with PFPS | Volunteers | 12 women 6 men | 8 women 10 men | I: 31 ± 9 Control: 39 ± 15 | NA | “Were observed for patellar proximal-distal shift (PTy) during NWB0°, patella flexion (PF) during WB30°, and anterior-posterior patella shift (PTz) during NWB0°, WB0°, and WB30° on the CT scan.” | NA | ||||||
| [58] | Single–leg squat (SLS) Split–Squat (SS) Squat (Double legged) | Kinematics to exercise movement in water (“included the average angular displacement and speed for each phase) The total range of motion and peak velocities.” | Healthy subject | University students | Male: 14 Female: 11 | NA | Overall: 22.3 ± 2.9 | Male: 24.03 Female: 22.01 | NA | The study showed a lower intensity of exercises in the water and improved mobility. Improvement in movement technique was also demonstrated as a function of immersion concerning land exercise. | ||||||
| [59] | single-leg squat Back Squat Barbell Hip Thrust | Kinematic Pain | Men with PFPS | Volunteers | 1 | 0 | 25 | 23.39 | Maintaining muscle mass is undoubtedly the best path to healthy joints, preventing muscle injuries and increasing the ability to withstand muscle overuse and muscle overload in daily tasks. After one year of training with different physical exercises, the end of pain was evident. | NA | ||||||
| [60] | Squat Jump with Countermoviment with barbell weight −70% 1RM (A—jump squat) Squat Jump with Countermoviment with free loan, and free swing movement by arms (B vertical jump) Hang Lift (Olympic-style lifts—(C) power clean) | Kinetics Kinematics muscle activation patterns of the countermovement jump, the power clean, and the jump squat | Athletes | University student | Male: 10 Female: 10 | NA | Male: 22.7 ± 3.7 Female: 20.4 ± 0.7 | Male: 26.60 Female: 22.60 | Force in Muscle Vastus Medialis (Quadriceps) by exercise. 1—power cleans (17,254 N s−1), 2—jump squat (7920 N s−1) 3—vertical jump (9465 N s−1) | NA | ||||||
| [61] | “1—isometric squat exercises (with) ball” | “muscle activation patterns (EMG) The muscle activity and the ratio of muscle activity were measured”. | Healthy Subject | Students | Male: 24 | NA | Overall: 26.04 ± 2.19 | Overall: 23.71 | “An efficient squat exercise posture for preventing the patellofemoral pain syndrome is to increase the knee joint bending angle on a stable surface. However, it would be efficient for patients with difficulties bending the knee joint to keep a knee joint bending angle of 15 degrees or less on an unstable surface.” | NA | ||||||
| [62] | overhead squat | Electromyography and kinematic | healthy females | Volunteers | 8 (MKD) | 14 | 18–28 | MDK 22.62 ± 1.85 Control: 21.82 ± 1.28 | We observed medial knee displacement (MKD) that exhibit greater muscle activity in the following muscles: adductor magnus, biceps femoris, vastus lateralis, and vastus medialis muscles during the eccentric phase of the overhead squat. Regarding the kinematics, the MKD group showed higher knee internal rotation, knee abduction, and ankle abduction than the controls. | NA | ||||||
| [63] | 1—sling open chain knee extension (SOCKE) exercise 2—sling closed chain knee extension (SCCKE) exercise | Muscle activation patterns (MVC), maximal voluntary contraction | Healthy subject | Students | Female: 7 | NA | Female: 21.3 ± 0.6 | Female: 23.94 | Maximal voluntary contraction MVC | NA | ||||||
| SOCKE exercise | SCCKE exercise | |||||||||||||||
| VMO (%) | VL (%) | VMO (%) | VL (%) | |||||||||||||
| 86.30 ± 14.61 | 86.20 ± 7.25 | 85.67 ± 6.27 | 77.85 ± 11.81 | |||||||||||||
| [64] | “1. Back Squat (Double Legged) stable load on a stable surface, stable load on an unstable surface, unstable load on a stable surface”. | “Kinematics of the Ankle, Knee, Hip, Trunk, and the Bar/Attitude. Muscle activation patterns (EMG)”. | Healthy Subject | University population | Male: 10 | NA | Overall: 21 ± 3 | Overall: 24.1 | During the squat movement, the Gluteus Medius muscle showed greater activity in the squat movement on the stable bar, squat on the tube, and squat in imbalance. The vastus medialis muscle, in turn, showed greater activity in the squat in imbalance, followed by the tube and bar. Represented in Figures 3 and 4 of the article [64] | NA | ||||||
| Ref. | [22] | [23] | [24] | [25] | [26] | [33] | [34] | [35] | [36] | [37] | [38] | [39] | [40] | [41] | [42] | [43] | [44] | [45] | [46] | [47] | [48] | [49] | [50] | [51] | [52] | [53] | [54] | [55] | [56] | [57] | [58] | [59] | [60] | [61] | [62] | [63] | [64] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (a) | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||||
| (b) | X | X | X | ||||||||||||||||||||||||||||||||||
| (c) | X | ||||||||||||||||||||||||||||||||||||
| (d) | X | ||||||||||||||||||||||||||||||||||||
| (e) | X | X | X | X | |||||||||||||||||||||||||||||||||
| Question | |||||||||||||||||||||||||||||||||||||
| 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 3 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | Y | Y | Y |
| 4 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | Y | NR | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | Y | Y | NA | Y | Y | Y | Y | Y |
| 5 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Y | NR | NR | NR | NR | NR | NR | NR | NR | NR | Y | NR | NR | Y | NR | NR | Y | NR | N | NR | NR | Y | NR | NR | Y | NR | NR |
| 6 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 7 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | Y | NA | NA | Y | NA | NA | NA | Y | NA | NA | Y | NA | NA | NA | Y | Y | NA | NA | Y | NA | NA | Y | NA | NA |
| 8 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | Y | NA | Y | Y | Y | Y | Y |
| 9 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 10 | NA | NA | NA | NA | Y | NA | NA | NA | NA | NA | NA | NA | NA | Y | NA | NA | Y | NA | NA | NA | Y | NA | NA | Y | NA | NA | NA | Y | Y | NA | NA | - | NA | NA | Y | NA | NA |
| 11 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NR | Y | Y | NR | Y | Y | Y | Y | Y | Y | Y | - | Y | Y | NR | Y | Y |
| 12 | NA | NA | NR | NA | NA | NR | NA | NA | NA | NA | NA | NA | NA | NR | NA | NA | NR | NA | NR | NA | NR | NR | NA | NR | NR | NA | Y | NR | NR | NA | NA | - | NR | NA | NR | NR | NA |
| 13 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | Y | Y | - | Y | Y | Y | Y | - | Y | Y | - | Y | Y | - | Y | Y |
| 14 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | Y | Y | - | Y | Y | Y | Y | - | Y | Y | - | Y | Y | - | Y | Y |
| TOTAL | 10 | 10 | 10 | 10 | 11 | 10 | 10 | 10 | 10 | 10 | 11 | 10 | 10 | 9 | 10 | 10 | 11 | 10 | 10 | 10 | 10 | 10 | 10 | 9 | 10 | 10 | 12 | 11 | 9 | 10 | 10 | 6 | 10 | 10 | 10 | 10 | 10 |
| Result | G | G | G | G | G | G | G | G | G | G | G | G | G | F | G | G | G | G | G | G | G | G | G | G | G | G | G | G | G | G | G | F | G | G | G | G | G |
References
- Dey, P.; Callaghan, M.; Cook, N.; Sephton, R.; Sutton, C.; Hough, E.; James, J.; Saqib, R.; Selfe, J. A questionnaire to identify patellofemoral pain in the community: An exploration of measurement properties. BMC Musculoskelet. Disord. 2016, 17, 237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarsen, B.; Krosshaug, T.; Bahr, R. Overuse Injuries in Professional Road Cyclists. Am. J. Sports Med. 2010, 38, 2494–2501. [Google Scholar] [CrossRef]
- Sharifian, S.A.; Chinichian, M.; HalimiMilani, A.; Mehrdad, R. Prevalence and risk factors of patellofemoral pain in an automobile manufacturing factory. Malays. J. Med. Health Sci. 2020, 16, 193–197. [Google Scholar]
- Boling, M.; Padua, D.; Marshall, S.; Guskiewicz, K.; Pyne, S.; Beutler, A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand. J. Med. Sci. Sports 2010, 20, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Pereira, P.M.; Amaro, J.; Duarte, J.; Santos Baptista, J.; Torres Costa, J. Prevalence of Patellofemoral Pain Syndrome in Selective Garbage Collection Workers—Cross Sectional Study. In Occupational and Environmental Safety and Health III; Springer: Cham, Switzerland, 2022; pp. 337–343. [Google Scholar]
- Crossley, K.M.; Stefanik, J.J.; Selfe, J.; Collins, N.J.; Davis, I.S.; Powers, C.M.; McConnell, J.; Vicenzino, B.; Bazett-Jones, D.M.; Esculier, J.-F.F.; et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome m. Br. J. Sports Med. 2016, 50, 839–843. [Google Scholar] [CrossRef]
- Willy, R.W.; Hoglund, L.T.; Barton, C.J.; Bolgla, L.A.; Scalzitti, D.A.; Logerstedt, D.S.; Lynch, A.D.; Snyder-Mackler, L.; McDonough, C.M. Patellofemoral Pain. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG95. [Google Scholar] [CrossRef] [Green Version]
- Pereira, P.M.; Amaro, J.; Ribeiro, B.T.; Gomes, A.; De Oliveira, P.; Duarte, J.; Ferraz, J.; Baptista, J.S.; Costa, J.T. Musculoskeletal Disorders’ Classification Proposal for Application in Occupational Medicine. Int. J. Environ. Res. Public Health 2021, 18, 8223. [Google Scholar] [CrossRef]
- Collins, N.J.; Barton, C.J.; Van Middelkoop, M.; Callaghan, M.J.; Rathleff, M.S.; Vicenzino, B.T.; Davis, I.S.; Powers, C.M.; Macri, E.M.; Hart, H.F.; et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: Recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br. J. Sports Med. 2018, 52, 1170–1178. [Google Scholar] [CrossRef]
- Powers, C.M.; Witvrouw, E.; Davis, I.S.; Crossley, K.M. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: Part 3. Br. J. Sports Med. 2017, 51, 1713–1723. [Google Scholar] [CrossRef] [Green Version]
- Lankhorst, N.E.; Bierma-Zeinstra, S.M.A.; Van Middelkoop, M. Risk factors for patellofemoral pain syndrome: A systematic review. J. Orthop. Sports Phys. Ther. 2012, 42, 81–94. [Google Scholar] [CrossRef]
- Neal, B.S.; Lack, S.D.; Lankhorst, N.E.; Raye, A.; Morrissey, D.; Van Middelkoop, M. Risk factors for patellofemoral pain: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 270–281. [Google Scholar] [CrossRef] [Green Version]
- Brechter, J.H.; Powers, C.M. Patellofemoral joint stress during stair ascent and descent in persons with and without patellofemoral pain. Gait Posture 2002, 16, 115–123. [Google Scholar] [CrossRef]
- Crossley, K.M.; Cowan, S.M.; Bennell, K.L.; McConnell, J. Knee flexion during stair ambulation is altered in individuals with patellofemoral pain. J. Orthop. Res. 2004, 22, 267–274. [Google Scholar] [CrossRef]
- Crossley, K.M.; van Middelkoop, M.; Barton, C.J.; Culvenor, A.G. Rethinking patellofemoral pain: Prevention, management and long-term consequences. Best Pract. Res. Clin. Rheumatol. 2019, 33, 48–65. [Google Scholar] [CrossRef]
- Ferràs-Tarragó, J.; Sanchis-Alfonso, V.; Ramírez-Fuentes, C.; Roselló-Añón, A.; Baixauli-García, F. Locating the Origin of Femoral Maltorsion Using 3D Volumetric Technology—The Hockey Stick Theory. J. Clin. Med. 2020, 9, 3835. [Google Scholar] [CrossRef]
- Søgaard, K.; Sjøgaard, G. Physical activity as cause and cure of muscular pain: Evidence of underlying mechanisms. Exerc. Sport Sci. Rev. 2017, 45, 136–145. [Google Scholar] [CrossRef] [Green Version]
- Bolgla, L.A.; Fithian, D.C.; Mace, K.L.; Boling, M.C.; DiStefano, M.J.; Mace, K.L.; DiStefano, M.J.; Fithian, D.C.; Powers, C.M. National Athletic Trainers’ Association Position Statement: Management of Individuals With Patellofemoral Pain. J. Athl. Train. 2018, 53, 820–836. [Google Scholar] [CrossRef] [Green Version]
- Coppack, R.J.; Etherington, J.; Wills, A.K. The effects of exercise for the prevention of overuse anterior knee pain: A randomized controlled trial. Am. J. Sports Med. 2011, 39, 940–948. [Google Scholar] [CrossRef]
- Lovalekar, M.; Perlsweig, K.A.; Keenan, K.A.; Baldwin, T.M.; Caviston, M.; McCarthy, A.E.; Parr, J.J.; Nindl, B.C.; Beals, K. Epidemiology of musculoskeletal injuries sustained by Naval Special Forces Operators and students. J. Sci. Med. Sport 2017, 20, S51–S56. [Google Scholar] [CrossRef]
- Maclachlan, L.R.; Collins, N.J.; Matthews, M.L.G.; Hodges, P.W.; Vicenzino, B. The psychological features of patellofemoral pain: A systematic review. Br. J. Sports Med. 2017, 51, 732–742. [Google Scholar] [CrossRef] [Green Version]
- Escamilla, R.F.; Fleisig, G.S.; Zheng, N.; Lander, J.E.; Barrentine, S.W.; Andrews, J.R.; Bergemann, B.W.; Moorman, C.T. Effects of technique variations on knee biomechanics during the squat and leg press. Med. Sci. Sports Exerc. 2001, 33, 1552–1566. [Google Scholar] [CrossRef]
- Flanagan, S.P.; Wang, M.Y.; Greendale, G.A.; Azen, S.P.; Salem, G.J. Biomechanical attributes of lunging activities for older adults. J. Strength Cond. Res. 2004, 18, 599–605. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Zheng, N.; MacLeod, T.D.; Edwards, W.B.; Hreljac, A.; Fleisig, G.S.; Wilk, K.E.; Moorman, C.T.; Imamura, R. Patellofemoral compressive force and stress during the forward and side lunges with and without a stride. Clin. Biomech. 2008, 23, 1026–1037. [Google Scholar] [CrossRef]
- Contreras, B.; Vigotsky, A.D.; Schoenfeld, B.J.B.J.; Beardsley, C.; Cronin, J. A Comparison of Gluteus Maximus, Biceps Femoris, and Vastus Lateralis Electromyographic Activity in the Back Squat and Barbell Hip Thrust Exercises. J. Appl. Biomech. 2015, 31, 452–458. [Google Scholar] [CrossRef]
- Wallace, D.A.; Salem, G.J.; Salinas, R.; Powers, C.M. Patellofemoral joint kinetics while squatting with and without an external load. J. Orthop. Sports Phys. Ther. 2002, 32, 141–148. [Google Scholar] [CrossRef] [Green Version]
- Dolak, K.L.; Silkman, C.; Mckeon, J.M.; Hosey, R.G.; Lattermann, C.; Uhl, T.L. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2011, 41, 560–570. [Google Scholar] [CrossRef] [Green Version]
- Ferber, R.; Bolgla, L.; Earl-Boehm, J.E.; Emery, C.; Hamstra-Wright, K. Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: A multicenter randomized controlled trial. J. Athl. Train. 2015, 50, 366–377. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamsee, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Pereira, P.M.; Duarte, J.; Ferraz, J.; Torres Costa, J.; Conceição, F. Squat and Patellofemoral Pain Syndrome: Protocol for a systematic review. Int. J. Occup. Environ. Saf. 2019, 3, 1–7. [Google Scholar] [CrossRef]
- Wohlin, C. Guidelines for snowballing in systematic literature studies and a replication in software engineering. In Proceedings of the ACM International Conference Proceeding Series; ACM Press: New York, NY, USA, 2014; pp. 1–10. [Google Scholar]
- National Heart, Lung and Blood Institute Home Page. Available online: http://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 20 June 2022).
- Schütz, P.; List, R.; Zemp, R.; Schellenberg, F.; Taylor, W.R.; Lorenzetti, S. Joint Angles of the Ankle, Knee, and Hip and Loading Conditions During Split Squats. J. Appl. Biomech. 2014, 30, 373–380. [Google Scholar] [CrossRef]
- Zellmer, M.; Kernozek, T.W.; Gheidi, N.; Hove, J.; Torry, M. Patellar tendon stress between two variations of the forward step lunge. J. Sport Health Sci. 2017, 8, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Salem, G.J.; Powers, C.M. Patellofemoral joint kinetics during squatting in collegiate women athletes. Clin. Biomech. 2001, 16, 424–430. [Google Scholar] [CrossRef]
- Kernozek, T.W.; Vannatta, C.N.N.; van den Bogert, A.J.A.J. Comparison of two methods of determining patellofemoral joint stress during dynamic activities. Gait Posture 2015, 42, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Slater, L.V.; Hart, J.M. Muscle Activation Patterns during Different Squat Techniques. J. Strength Cond. Res. 2017, 31, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Chang, W.D.; Wu, J.Y.; Fong, Y.C. Electromyographic analysis of hip and knee muscles during specific exercise movements in females with patellofemoral pain syndrome An observational study. Medicine 2018, 97, e11424. [Google Scholar] [CrossRef] [PubMed]
- Stastny, P.; Lehnert, M.; Zaatar, A.M.Z.; Svoboda, Z.; Xaverova, Z. Does the Dumbbell-Carrying Position Change the Muscle Activity in Split Squats and Walking Lunges? J. Strength Cond. Res. 2015, 29, 3177–3187. [Google Scholar] [CrossRef] [Green Version]
- Lorenzetti, S.; Ostermann, M.; Zeidler, F.; Zimmer, P.; Jentsch, L.; List, R.; Taylor, W.R.; Schellenberg, F.; Lorenzetti, S.; List, R.; et al. How to squat? Effects of various stance widths, foot placement angles and level of experience on knee, hip and trunk motion and loading. BMC Sports Sci. Med. Rehabil. 2018, 10, 14. [Google Scholar] [CrossRef]
- Bakhtiary, A.H.; Fatemi, E. Open versus closed kinetic chain exercises for patellar chondromalacia. Br. J. Sports Med. 2007, 42, 99–102. [Google Scholar] [CrossRef]
- Chang, W.D.; Huang, W.S.; Lai, P.T. Muscle Activation of Vastus Medialis Oblique and Vastus Lateralis in Sling-Based Exercises in Patients with Patellofemoral Pain Syndrome: A Cross-Over Study. Evid. Based Complementary Altern. Med. 2015, 740315, 8. [Google Scholar] [CrossRef] [Green Version]
- Singh, G.K.; Srivastava, S. Preferential strengthening of VMO muscle during selected biomechanical rehabilitative exercises of automotive workers with patellofemoral pain syndrome. Work 2018, 60, 135–141. [Google Scholar] [CrossRef]
- Palmer, K.; Hebron, C.; Williams, J.M. A randomised trial into the effect of an isolated hip abductor strengthening programme and a functional motor control programme on knee kinematics and hip muscle strength. BMC Musculoskelet. Disord. 2015, 16, 105. [Google Scholar] [CrossRef] [Green Version]
- Kernozek, T.W.; Gheidi, N.; Zellmer, M.; Hove, J.; Heinert, B.L.; Torry, M.R. Effects of anterior knee displacement during squatting on patellofemoral joint stress. J. Sport Rehabil. 2018, 27, 237–243. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Zheng, N.; MacLeod, T.D.; Edwards, W.B.; Hreljac, A.; Fleisig, G.S.; Wilk, K.E.; Moorman, C.T.; Imamura, R.; Andrews, J.R. Patellofemoral Joint Force and Stress Between a Short- and Long-Step Forward Lunge. J. Orthop. Sports Phys. Ther. 2008, 38, 681–690. [Google Scholar] [CrossRef]
- Yavuz, H.U.; Erdağ, D.; Amca, A.M.; Aritan, S. Kinematic and EMG activities during front and back squat variations in maximum loads. J. Sports Sci. 2015, 33, 1058–1066. [Google Scholar] [CrossRef]
- Mirzaie, G.H.; Rahimi, A.; Kajbafvala, M.; Manshadi, F.D.; Kalantari, K.K.; Saidee, A. Electromyographic activity of the hip and knee muscles during functional tasks in males with and without patellofemoral pain. J. Bodyw. Mov. Ther. 2019, 23, 54–58. [Google Scholar] [CrossRef] [Green Version]
- Escamilla, R.F.; Zheng, N.; Macleod, T.D.; Brent Edwards, W.; Imamura, R.; Hreljac, A.; Fleisig, G.S.; Wilk, K.E.; Moorman, C.T.; Andrews, J.R. Patellofemoral Joint Force and Stress during the Wall Squat and One-Leg Squat. Med. Sci. Sports Exerc. 2009, 41, 879–888. [Google Scholar] [CrossRef]
- Jaberzadeh, S.; Yeo, D.; Zoghi, M. The Effect of Altering Knee Position and Squat Depth on VMO: VL EMG Ratio During Squat Exercises. Physiother. Res. Int. 2015, 21, 164–173. [Google Scholar] [CrossRef]
- Schmidt, E.; Harris-Hayes, M.; Salsich, G.B. Dynamic knee valgus kinematics and their relationship to pain in women with patellofemoral pain compared to women with chronic hip joint pain. J. Sport Health Sci. 2019, 8, 486–493. [Google Scholar] [CrossRef]
- Schwanbeck, S.; Chilibeck, P.D.; Binsted, G. A comparison of free weight squat to Smith machine squat using electromyography. J. Strength Cond. Res. Natl. Strength Cond. Assoc. 2009, 23, 2588–2591. [Google Scholar] [CrossRef]
- Slater, L.V.; Hart, J.M. The influence of knee alignment on lower extremity kinetics during squats. J. Electromyogr. Kinesiol. 2016, 31, 96–103. [Google Scholar] [CrossRef]
- Glaviano, N.R.; Marshall, A.N.; Colby Mangum, L.; Hart, J.M.; Hertel, J.; Russell, S.; Saliba, S. Improvements in lower-extremity function following a rehabilitation program with patterned electrical neuromuscular stimulation in females with patellofemoral pain: A randomized controlled trial. J. Sport Rehabil. 2020, 29, 1075–1085. [Google Scholar] [CrossRef]
- Minoonejad, H.; Rajabi, R.; Ebrahimi-Takamjani, E.; Alizadeh, M.H.; Jamshidi, A.A.; Azhari, A.; Fatehi, E. Combined Open and Closed Kinetic Chain Exercises for Patellofemoral Pain Syndrome: A Randomized Controlled Trial. World J. Sport Sci. 2012, 6, 278–285. [Google Scholar] [CrossRef]
- Barbosa, A.C.; Carvalho, R.A.N.; Bonifácio, D.N.; Martins, F.L.M.; Barbosa, M.C.S.A. Increased Activation Amplitude Levels of Gluteus Medius in Women During Isometric and Dynamic Conditions Following a 4-week Protocol of Low-load Eccentric Exercises. Physiother. Res. Int. 2016, 21, 257–263. [Google Scholar] [CrossRef]
- Yang, J.S.; Fredericson, M.; Choi, J.H. The effect of patellofemoral pain syndrome on patellofemoral joint kinematics under upright weight-bearing conditions. PLoS ONE 2020, 15, e0239907. [Google Scholar] [CrossRef]
- Severin, A.C.; Burkett, B.J.; McKean, M.R.; Wiegand, A.N.; Sayers, M.G.L.L. Quantifying kinematic differences between land and water during squats, split squats, and single-leg squats in a healthy population. PLoS ONE 2017, 12, e0182320. [Google Scholar] [CrossRef] [Green Version]
- Pereira, P.M.; Reis, J.; Duarte, J.; Santos Baptista, J.; Torres Costa, J.; Conceição, F. Application of bodybuilding for correction of musculoskeletal disease in Patellofemoral Pain Syndrome-A case report. Int. J. Occup. Environ. Saf. 2020, 4, 82–88. [Google Scholar] [CrossRef]
- MacKenzie, S.J.; Lavers, R.J.; Wallace, B.B. A biomechanical comparison of the vertical jump, power clean, and jump squat. J. Sports Sci. 2014, 32, 1576–1585. [Google Scholar] [CrossRef]
- Kang, J.-I.I.; Park, J.-S.S.; Choi, H.; Jeong, D.-K.K.; Kwon, H.-M.M.; Moon, Y.-J.J. A study on muscle activity and ratio of the knee extensor depending on the types of squat exercise. J. Phys. Ther. Sci. 2017, 29, 43–47. [Google Scholar] [CrossRef] [Green Version]
- Dinis, R.; Vaz, J.R.; Silva, L.; Marta, S.; Pezarat-Correia, P. Electromyographic and kinematic analysis of females with excessive medial knee displacement in the overhead squat. J. Electromyogr. Kinesiol. 2021, 57, 102530. [Google Scholar] [CrossRef]
- Chang, W.D.; Huang, W.S.; Lee, C.L.; Lin, H.Y.; Lai, P.T. Effects of open and closed kinetic chains of sling exercise therapy on the muscle activity of the vastus medialis oblique and vastus lateralis. J. Phys. Ther. Sci. 2014, 26, 1363–1366. [Google Scholar] [CrossRef] [Green Version]
- Nairn, B.C.; Sutherland, C.A.; Drake, J.D.M. Motion and Muscle Activity Are Affected by Instability Location during a Squat Exercise. J. Strength Cond. Res. 2017, 31, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Fry, A.C.; Smith, J.C.; Schilling, B.K. Effect of Knee Position on Hip and Knee Torques during the Barbell Squat. J. Strength Cond. Res. 2003, 17, 629–633. [Google Scholar] [PubMed] [Green Version]
- Kaya, D.; Güney, H.; Akseki, D.; Doral, M.N. How can we strengthen the quadriceps femoris in patients with patellofemoral pain syndrome? Sports Inj. Prev. Diagn. Treat. Rehabil. 2012, 2, 1157–1161. [Google Scholar] [CrossRef] [Green Version]

| References | Quality Tool Assessment NHLDI * | Study Authors | Quality Tool Assessment NHLDI * | Study Authors | Quality Tool Assessment NHLDI * |
|---|---|---|---|---|---|
| [22] | G | [23] | G | [24] | G |
| [25] | G | [26] | G | [33] | G |
| [34] | G | [35] | G | [36] | G |
| [37] | G | [38] | G | [39] | G |
| [40] | G | [41] | F | [42] | G |
| [43] | G | [44] | G | [45] | G |
| [46] | G | [47] | G | [48] | G |
| [49] | G | [50] | G | [51] | G |
| [52] | G | [53] | G | [54] | G |
| [55] | G | [56] | G | [57] | G |
| [58] | G | [59] | F | [60] | G |
| [61] | G | [62] | G | [63] | G |
| [64] | G |
| Refs. | [22] | [23] | [24] | [25] | [26] | [33] | [34] | [35] | [36] | [37] | [38] | [39] | [40] | [41] | [42] | [43] | [44] | [45] | [46] | [47] | [48] | [49] | [50] | [51] | [52] | [53] | [54] | [55] | [56] | [57] | [58] | [59] | [60] | [61] | [62] | [63] | [64] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (a) | Y | |||||||||||||||||||||||||||||||||||||
| N | ||||||||||||||||||||||||||||||||||||||
| U | ||||||||||||||||||||||||||||||||||||||
| (b) | Y | |||||||||||||||||||||||||||||||||||||
| N | ||||||||||||||||||||||||||||||||||||||
| (c) | Y | |||||||||||||||||||||||||||||||||||||
| N | ||||||||||||||||||||||||||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira, P.M.; Baptista, J.S.; Conceição, F.; Duarte, J.; Ferraz, J.; Costa, J.T. Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9241. https://doi.org/10.3390/ijerph19159241
Pereira PM, Baptista JS, Conceição F, Duarte J, Ferraz J, Costa JT. Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(15):9241. https://doi.org/10.3390/ijerph19159241
Chicago/Turabian StylePereira, Pablo Monteiro, João Santos Baptista, Filipe Conceição, Joana Duarte, João Ferraz, and José Torres Costa. 2022. "Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 15: 9241. https://doi.org/10.3390/ijerph19159241
APA StylePereira, P. M., Baptista, J. S., Conceição, F., Duarte, J., Ferraz, J., & Costa, J. T. (2022). Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review. International Journal of Environmental Research and Public Health, 19(15), 9241. https://doi.org/10.3390/ijerph19159241







