Assessing the Dynamic Outcomes of Containment Strategies against COVID-19 under Different Public Health Governance Structures: A Comparison between Pakistan and Bangladesh
Abstract
:1. Introduction
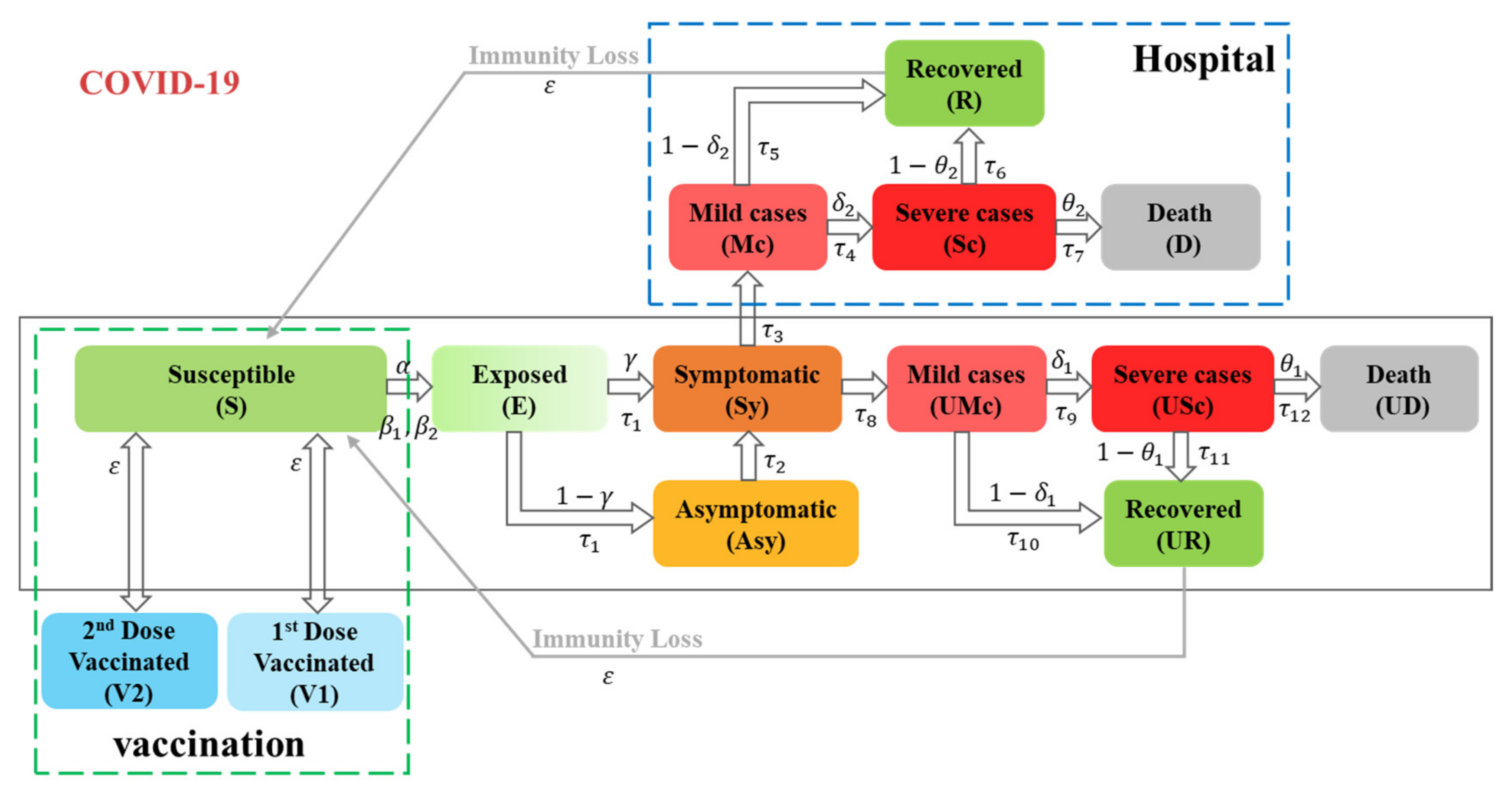
2. Materials and Methods
2.1. Design of the Study
2.2. Data Sources
2.3. Data Analysis and Scenario Simulation
3. Results
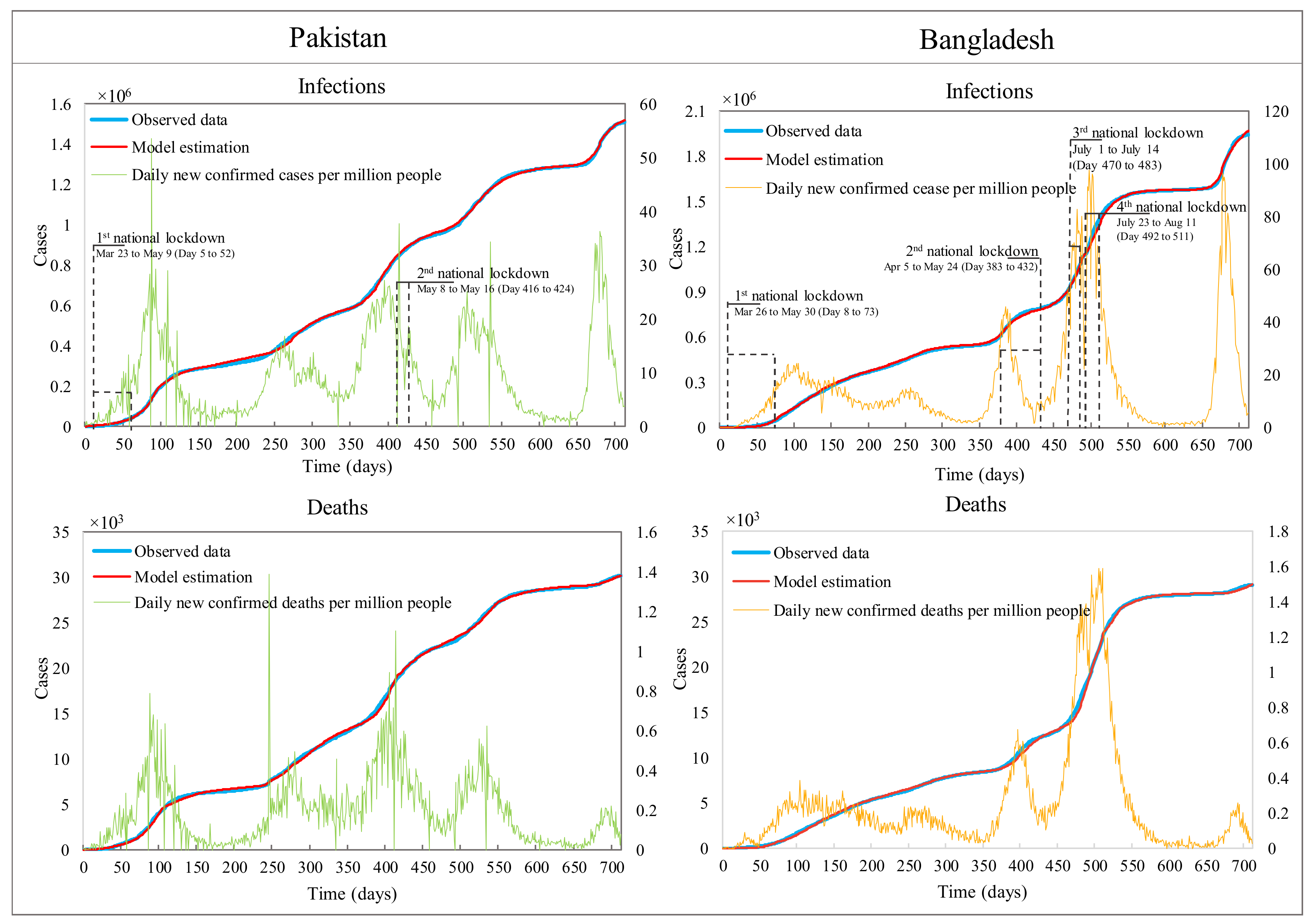
3.1. Fitting Historic Data and Parameter Estimation
3.2. Counterfactual Analysis
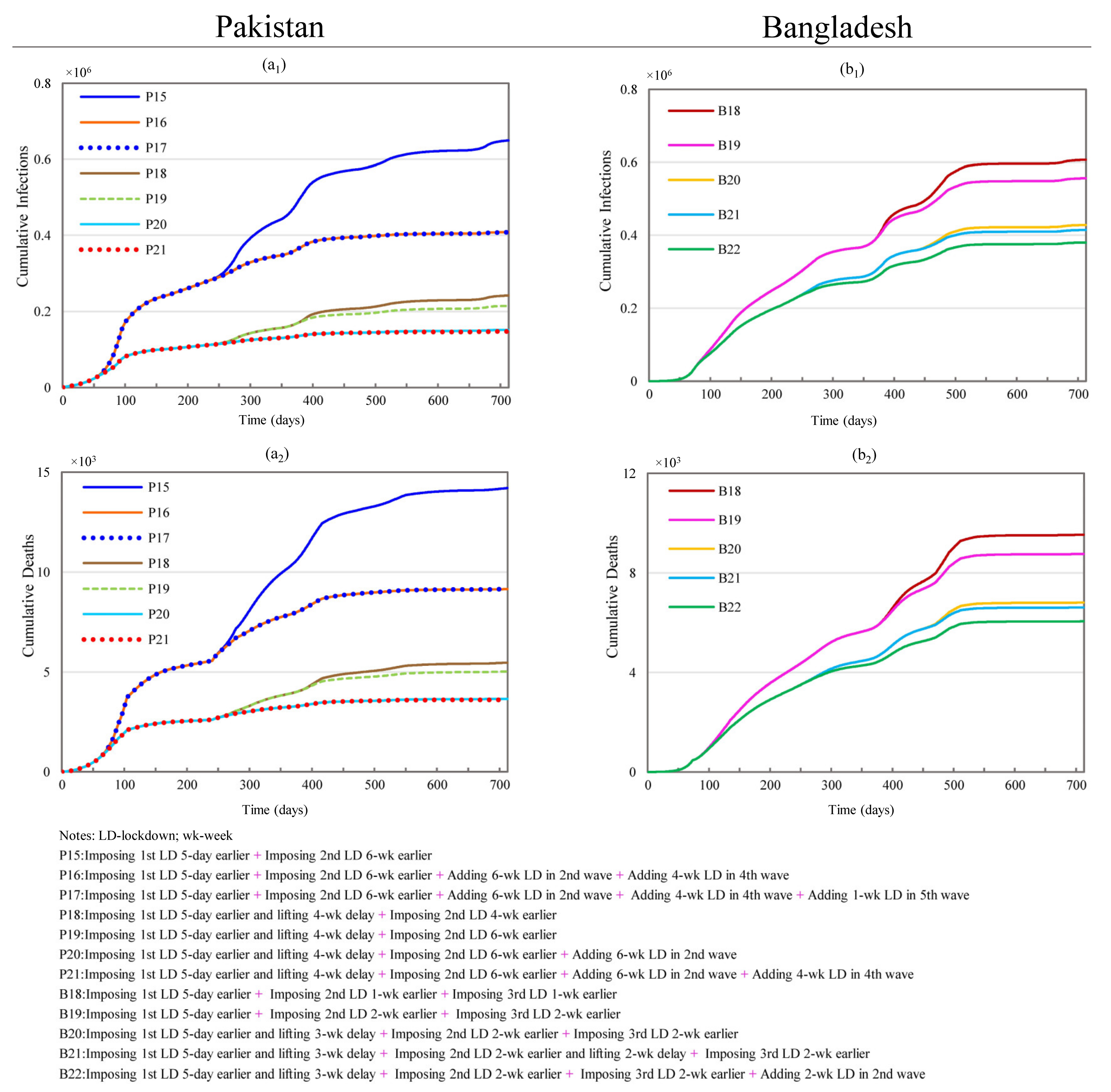
3.2.1. Changing Initial Lockdown Timing and Duration
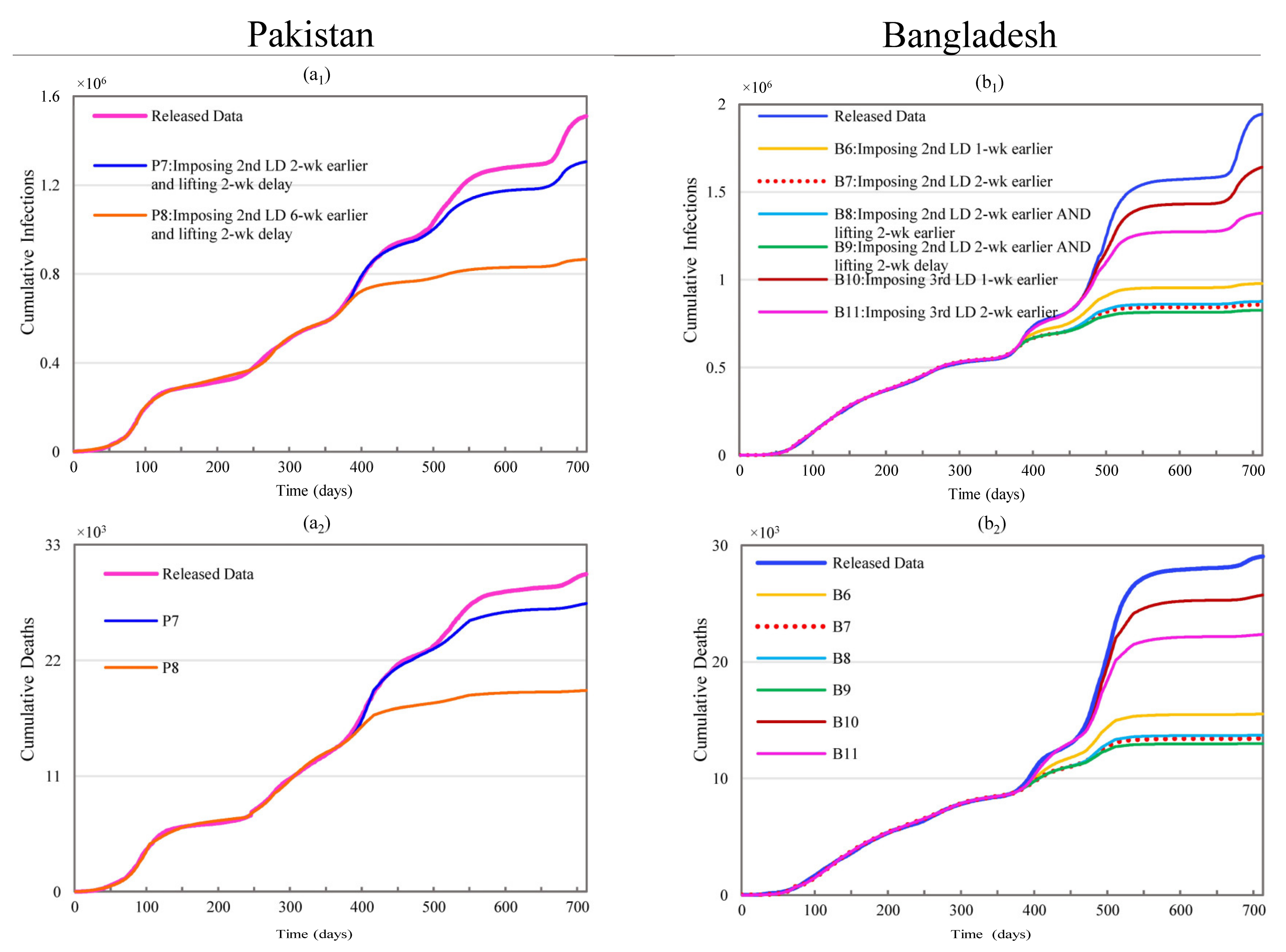
3.2.2. Changing Subsequent Lockdown Timing and Duration
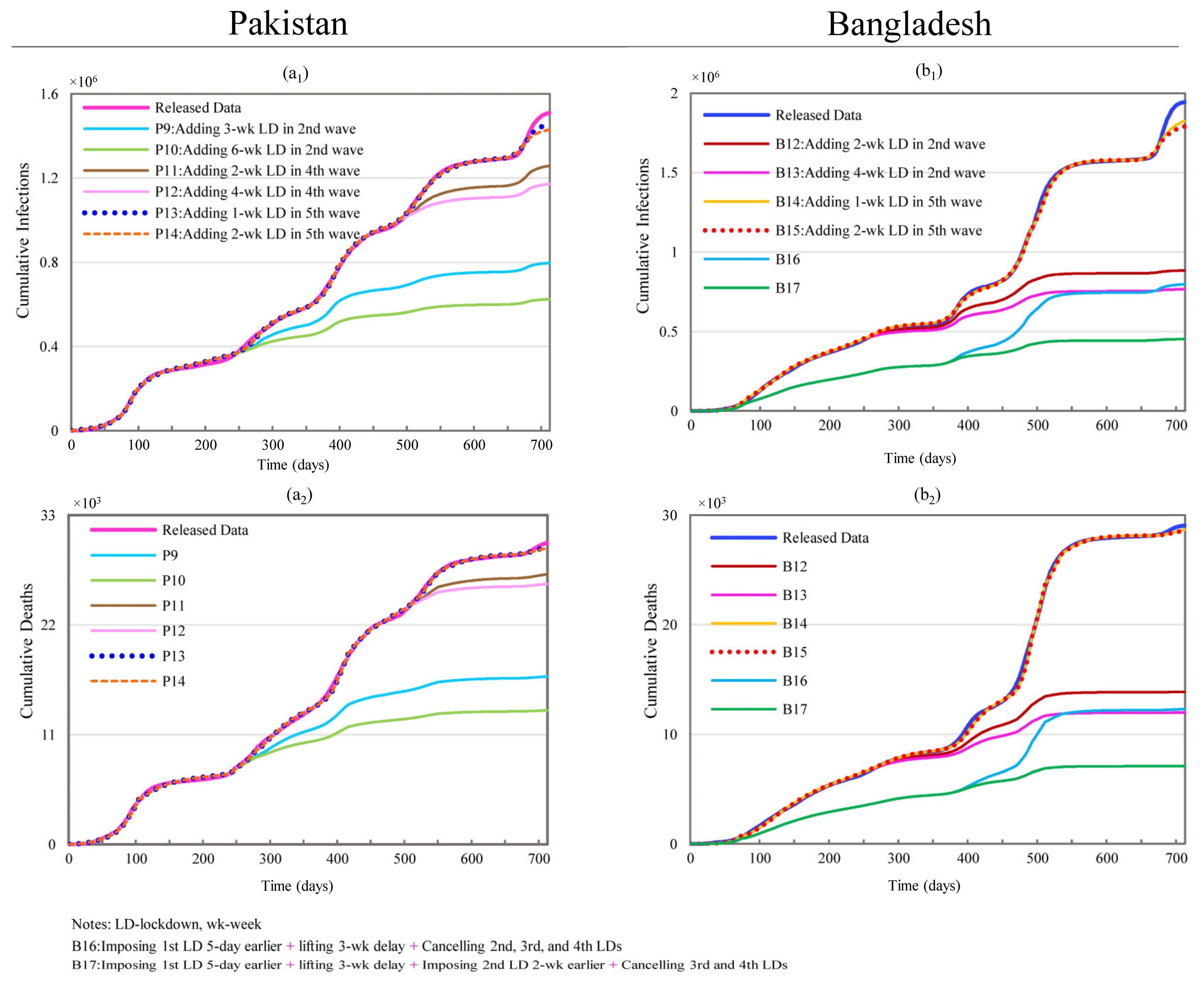
3.2.3. Changing Lockdown Frequency
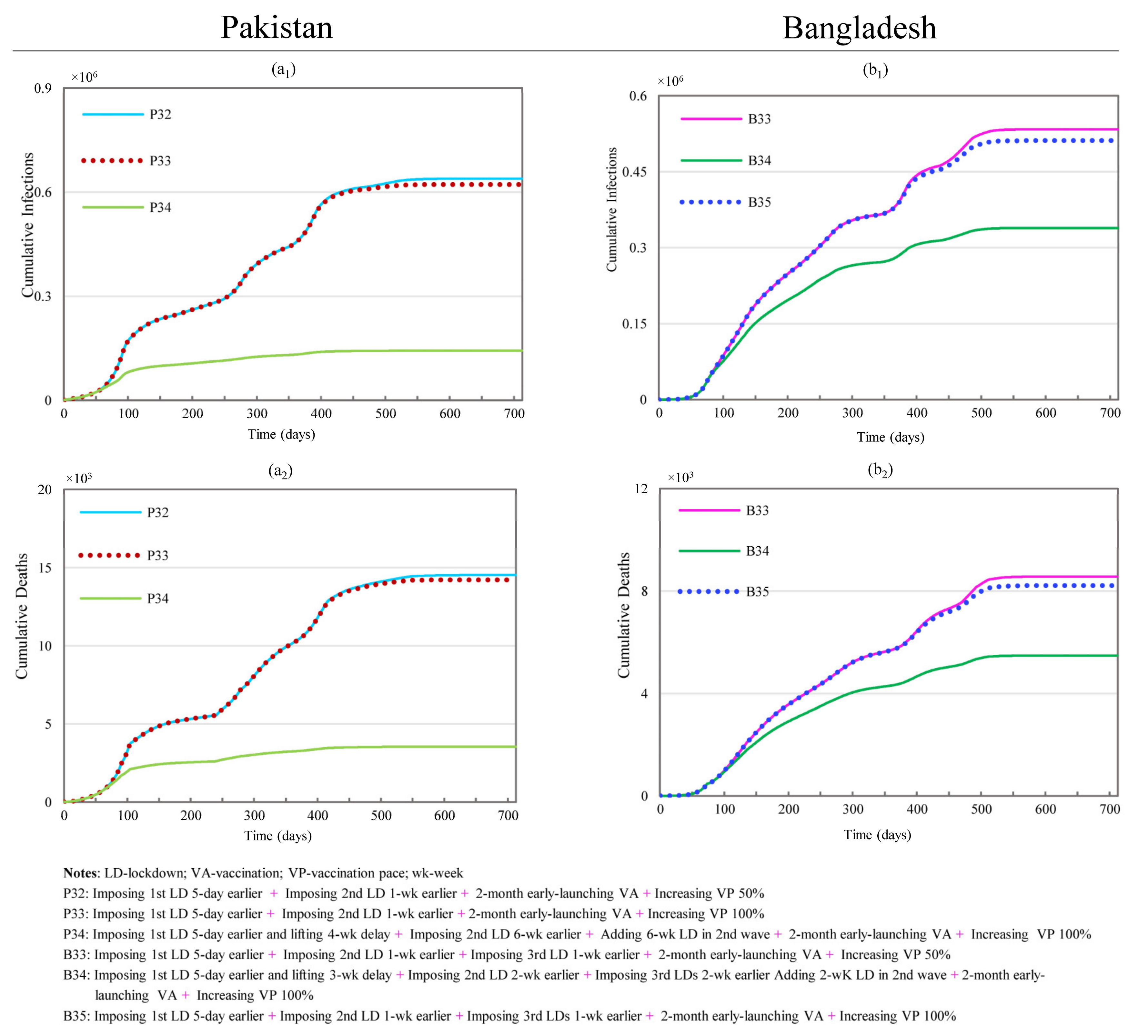
3.2.4. Effects of Changing Multiple Lockdown Conditions
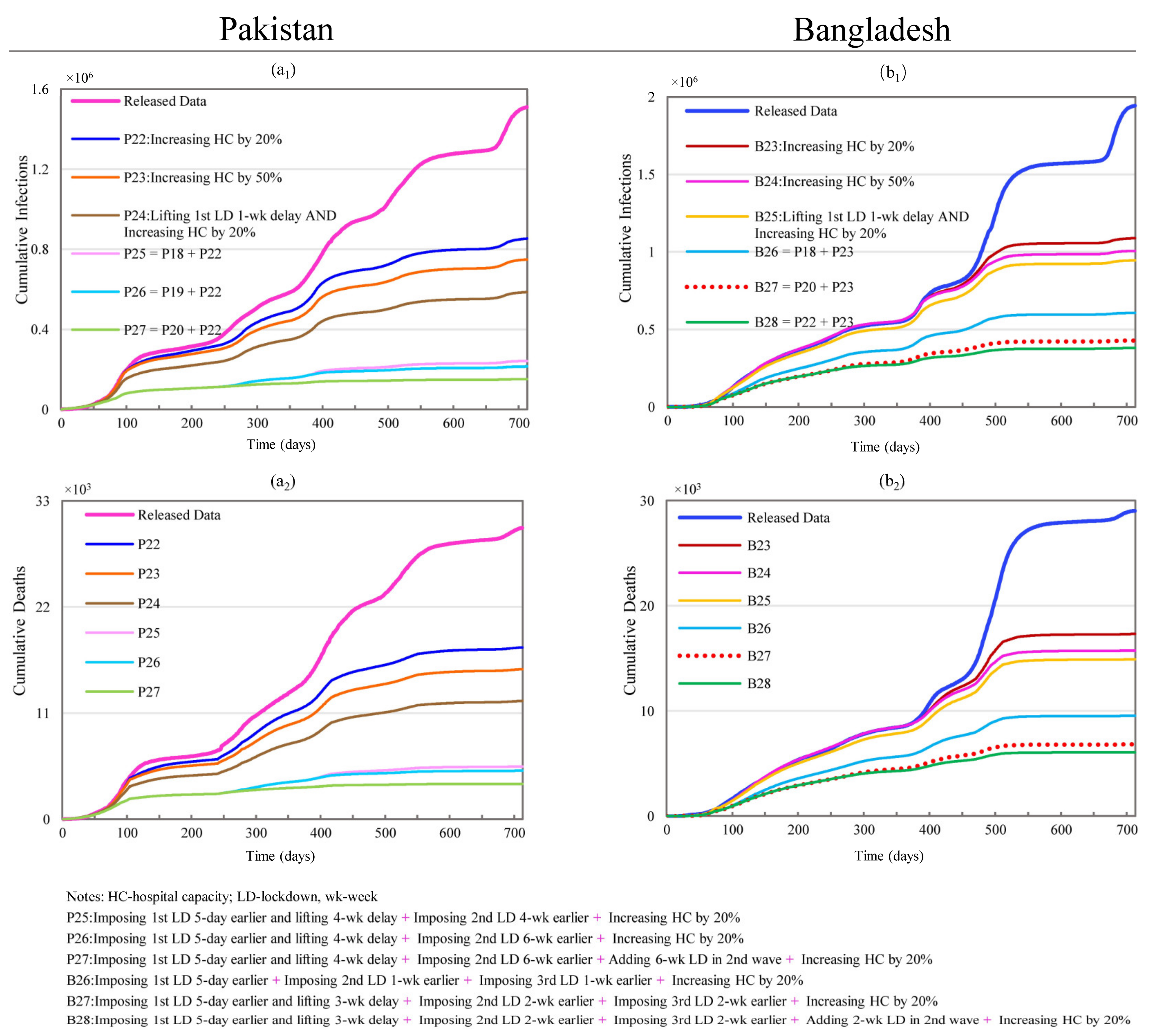
3.2.5. Hospital Capacity and Its Combination with Lockdowns
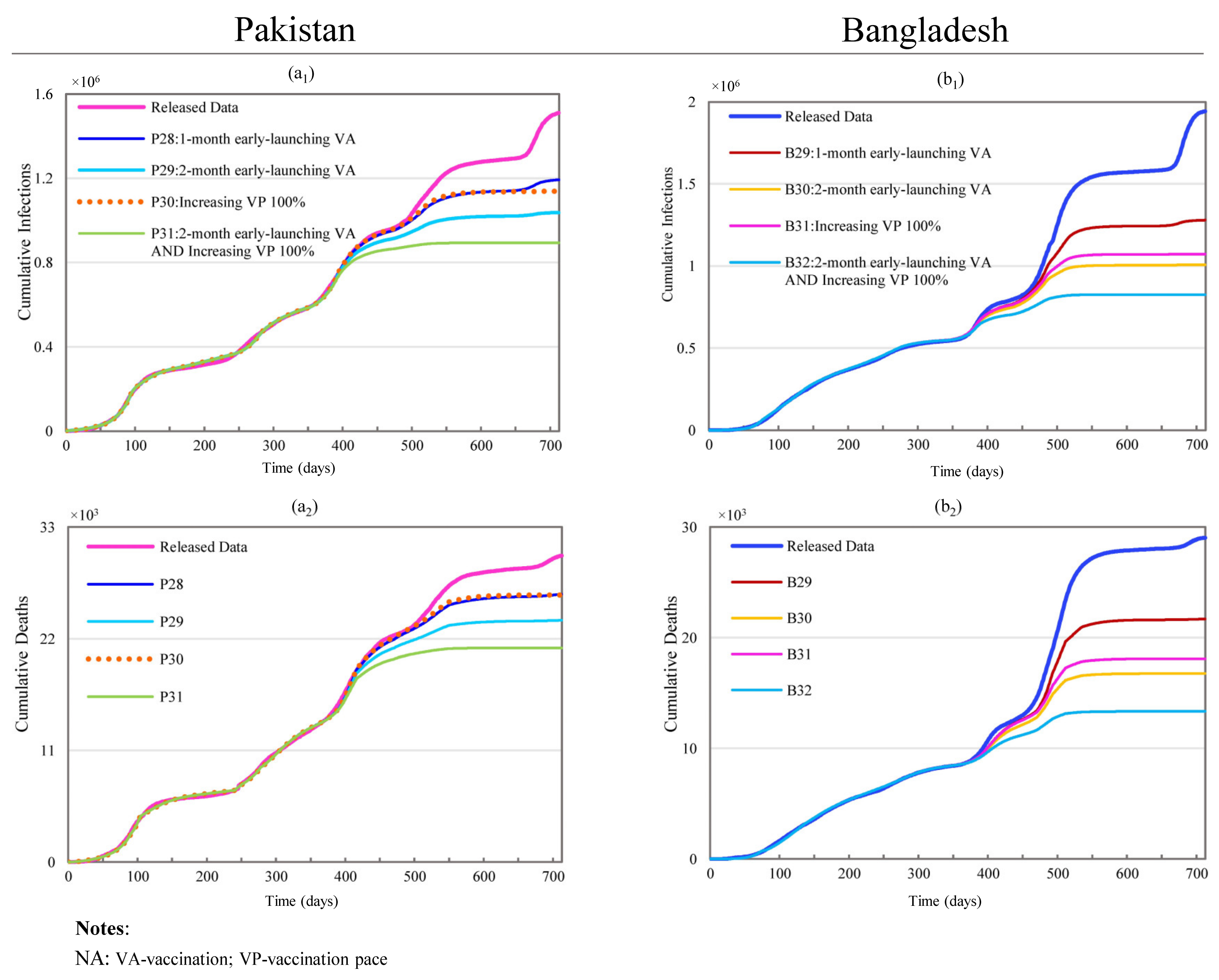
3.2.6. Changing Vaccination Setting and Lockdown Timing
4. Discussion
4.1. Lockdown Adjustments
4.2. Hospital Capacity and Vaccination
4.3. Combined Adjustments
4.4. Strengths and Limitations
4.5. Practical Implications and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gralinski, L.E.; Menachery, V.D. Return of the Coronavirus: 2019-nCoV. Viruses 2020, 12, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 19 April 2022).
- World Health Organization (WHO). Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed on 20 January 2022).
- Ahmed, F. Ethnicity and Politics in Pakistan; Karachi Oxford University Press: Oxford, UK, 1998. [Google Scholar]
- Maddex, R.L. Constitutions of the World; Routledge: London, UK, 2014. [Google Scholar]
- World Bank. Hospital Beds (per 1000 People)-Pakistan. Available online: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?locations=PK (accessed on 25 January 2022).
- World Bank. Physicians (per 1000 People)-Pakistan. Available online: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=PK (accessed on 25 January 2022).
- World Bank. Hospital Beds (per 1000 People)-Bangladesh. Available online: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?locations=BD (accessed on 25 January 2022).
- World Bank. Physicians (per 1000 People)-Bangladesh. Available online: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=BD (accessed on 25 January 2022).
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 28 February 2022).
- World Health Organization (WHO). Update on Omicron. Available online: https://www.who.int/news/item/28-11-2021-update-on-omicron (accessed on 10 December 2021).
- World Health Organization (WHO). COVID-19 Pakistan Situation. Available online: https://covid19.who.int/region/emro/country/pk (accessed on 19 February 2022).
- World Health Organization (WHO). COVID-19 Bangladesh Situation. Available online: https://covid19.who.int/region/searo/country/bd (accessed on 19 February 2022).
- Paremoer, L.; Nandi, S.; Serag, H.; Baum, F. COVID-19 pandemic and the social determinants of health. BMJ 2021, 372, n129. [Google Scholar] [CrossRef]
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, X.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality: Systematic review and meta-analysis. BMJ 2021, 375, e068302. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Xue, H.; Li, Y.; Xu, J.; Wang, Y. Investigating the diffusion of agent-based modelling and system dynamics modelling in population health and healthcare research. Syst. Res. Behav. Sci. 2018, 35, 203–215. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Shahani, A.K.; Roy, R.B.; Sivapalan, S. Simulation modelling for HIV infection and AIDS. Int. J. Biomed. Comput. 1992, 31, 73–88. [Google Scholar] [CrossRef]
- Viana, J.; Brailsford, S.C.; Harindra, V.; Harper, P.R. Combining discrete-event simulation and system dynamics in a healthcare setting: A composite model for Chlamydia infection. Eur. J. Oper. Res. 2014, 237, 196–206. [Google Scholar] [CrossRef]
- Jones, A.P.; Homer, J.B.; Murphy, D.L.; Essien, J.D.; Milstein, B.; Seville, D.A. Understanding diabetes population dynamics through simulation modeling and experimentation. Am. J. Public Health 2006, 96, 488–494. [Google Scholar] [CrossRef]
- Jalali, M.S.; Rahmandad, H.; Bullock, S.L.; Lee-Kwan, S.H.; Gittelsohn, J.; Ammerman, A. Dynamics of intervention adoption, implementation, and maintenance inside organizations: The case of an obesity prevention initiative. Soc. Sci. Med. 2019, 224, 67–76. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Lattimer, V.A.; Tarnaras, P.; Turnbull, J.C. Emergency and on-demand health care: Modeling a large complex system. J. Oper. Res. Soc. 2004, 55, 34–42. [Google Scholar] [CrossRef]
- Lane, D.C.; Husemann, E. System dynamics mapping of acute patient flows. J. Oper. Res. Soc. 2008, 59, 213–224. [Google Scholar] [CrossRef]
- Hunt, J.C.R.; Timoshkina, Y.; Baudains, P.J.; Bishop, S.R. System dynamics applied to operations and policy decisions. Eur. Rev. 2012, 20, 324–342. [Google Scholar] [CrossRef]
- Liu, S.; Triantis, K.P.; Zhao, L.; Wang, Y. Capturing multi-stage fuzzy uncertainties in hybrid system dynamics and agent-based models for enhancing policy implementation in health systems research. PLoS ONE 2018, 13, e0194687. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Osgood, N.; Gao, Q.; Xue, H.; Wang, Y. Systems simulation model for assessing the sustainability and synergistic impacts of sugar-sweetened beverages tax and revenue recycling on childhood obesity prevention. J. Oper. Res. Soc. 2016, 67, 708–721. [Google Scholar] [CrossRef]
- Zhu, N.J.; Ahmad, R.; Holmes, A.; Robotham, J.V.; Lebcir, R.; Atun, R. System dynamics modelling to formulate policy interventions to optimise antibiotic prescribing in hospitals. J. Oper. Res. Soc. 2021, 72, 2490–2502. [Google Scholar] [CrossRef]
- Levy, D.T.; Bauer, J.E.; Lee, H.R. Simulation modeling and tobacco control: Creating more robust public health policies. Am. J. Public Health 2006, 96, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Royston, G.; Dost, A.; Townshend, J.; Turner, H. Using system dynamics to help develop and implement policies and programs in health care in England. Syst. Dyn. Rev. 1999, 15, 293–314. [Google Scholar] [CrossRef]
- Homer, J.B.; Hirsch, G.B. System dynamics modeling for public health: Background and opportunities. Am. J. Public Health 2006, 96, 452–458. [Google Scholar] [CrossRef]
- Mahamoud, A.; Roche, B.; Homer, J. Modelling the social determinants of health and simulating short-term and long-term intervention impacts for the city of Toronto, Canada. Soc. Sci. Med. 2013, 93, 247–255. [Google Scholar] [CrossRef]
- Bugalia, S.; Tripathi, J.P.; Wang, H. Mathematical modeling of intervention and low medical resource availability with delays: Applications to COVID-19 outbreaks in Spain and Italy. Math. Biosci. Eng. 2021, 18, 5865–5920. [Google Scholar] [CrossRef]
- Mokhtari, A.; Mineo, C.; Kriseman, J.; Kremer, P.; Neal, L.; Larson, J. A multi-method approach to modeling COVID-19 disease dynamics in the United States. Sci. Rep. 2021, 11, 12426. [Google Scholar] [CrossRef]
- Mutanga, S.S.; Ngungu, M.; Tshililo, F.P.; Kaggwa, M. Systems dynamics approach for modelling South Africa’s response to COVID-19: A “what if” scenario. J. Public Health Res. 2021, 10, 1897. [Google Scholar] [CrossRef]
- Struben, J. The coronavirus disease (COVID-19) pandemic: Simulation-based assessment of outbreak responses and postpeak strategies. Syst. Dyn. Rev. 2020, 36, 247–293. [Google Scholar] [CrossRef]
- Kakakhel, M.A.; Wu, F.; Khan, T.A.; Feng, H.; Hassan, Z.; Anwar, Z.; Faisal, S.; Ali, I.; Wang, W. The first two months epidimiological study of COVID-19, related public health preparedness, and response to the ongoing epidemic in Pakistan. New Microbes New Infect. 2020, 37, 100734. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Z.; Arif, M.; Ali, F.; Khan, I.; Nisar, K.S. A report on COVID-19 epidemic in Pakistan using SEIR fractional model. Sci. Rep. 2020, 10, 22268. [Google Scholar] [CrossRef]
- Hussain, T.; Ozair, M.; Ali, F.; Rehman, S.U.; Assiri, T.A.; Mahmoud, E.E. Sensitivity analysis and optimal control of COVID-19 dynamics based on SEIQR model. Results Phys. 2021, 22, 103956. [Google Scholar] [CrossRef] [PubMed]
- Hassan, R.; Dosar, A.S.; Mondol, J.K.; Khan, T.H.; Noman, A.A.; Sayem, M.S.; Hasan, M.; Juyena, N.S. Prediction of epidemics trend of COVID-19 in Bangladesh. Front. Public Health 2020, 8, 559437. [Google Scholar] [CrossRef]
- Masud, M.A.; Islam, M.H.; Mamun, K.A.; Kim, B.N.; Kim, S. COVID-19 transmission: Bangladesh perspective. Mathematics 2020, 8, 1793. [Google Scholar] [CrossRef]
- Akanda, A.A.M.; Ahmed, R. How successful Bangladesh is in controlling the coronavirus pandemic? Bull. Natl. Res. Cent. 2020, 44, 196. [Google Scholar] [CrossRef]
- Truelove, S.; Abrahim, O.; Altare, C.; Lauer, S.A.; Grantz, K.H.; Azman, A.S.; Spiegel, P. The potential impact of COVID-19 in refugee camps in Bangladesh and beyond: A modeling study. PLoS Med. 2020, 17, e1003144. [Google Scholar] [CrossRef]
- Kamrujjaman, M.; Mahmud, M.S.; Ahmed, S.; Qayum, M.O.; Alam, M.M.; Hassan, M.N.; Islam, M.R.; Nipa, K.F.; Bulut, U. SARS-CoV-2 and Rohingya refugee camp, Bangladesh: Uncertainty and how the government took over the situation. Biology 2021, 10, 124. [Google Scholar] [CrossRef]
- Khan, I.M.; Haque, U.; Kaisar, S.; Rahman, M.S. A computational modeling study of COVID-19 in Bangladesh. Am. J. Trop. Med. Hyg. 2021, 104, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Brodeur, A.; Gray, D.; Islam, A.; Bhuiyan, S. A literature review of the economics of COVID-19. J. Econ. Surv. 2021, 35, 1007–1044. [Google Scholar] [CrossRef] [PubMed]
- Bartik, A.W.; Bertrand, M.; Cullen, Z.; Glaeser, E.L.; Luca, M.; Stanton, C. The impact of COVID-19 on small business outcomes and expectations. Proc. Natl. Acad. Sci. USA 2020, 117, 17656–17666. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Pierri, F.; Cinelli, M.; Flori, A.; Galeazzi, A.; Porcelli, F.; Schmidt, A.L.; Valensise, C.M.; Scala, A.; Quattrociocchi, W.; et al. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 15530–15535. [Google Scholar] [CrossRef]
- McAloon, C.; Collins, Á.; Hunt, K.; Barber, A.; Byrne, A.W.; Butler, F.; Casey, M.; Griffin, J.; Lane, E.; McEvoy, D.; et al. Incubation period of COVID-19: A rapid systematic review and meta-analysis of observational research. BMJ Open 2020, 10, e039652. [Google Scholar] [CrossRef]
- He, J.; Guo, Y.; Mao, R.; Zhang, J. Proportion of asymptomatic coronavirus disease 2019: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 820–830. [Google Scholar] [CrossRef]
- Hasan, M.J.; Chowdhury, S.M.; Khan, M.A.S.; Rahaman, M.; Fardous, J.; Adit, T.; Rahman, M.; Hossain, M.T.; Yesmin, S.; Raheem, E.; et al. Clinico-epidemiological characteristics of asymptomatic and symptomatic COVID-19-positive patients in Bangladesh. medRxiv, 2020. [Google Scholar] [CrossRef]
- Thompson, M.G.; Burgess, J.L.; Naleway, A.L.; Tyner, H.L.; Yoon, S.K.; Meece, J.; Olsho, L.E.; Caban-Martinez, A.J.; Fowlkes, A.; Lutrick, K.; et al. Interim estimates of vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines in preventing SARS-CoV-2 infection among health care personnel, first responders, and other essential and frontline workers-eight U.S. locations, December 2020–March 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 495–500. [Google Scholar] [CrossRef]
- Thompson, M.G.; Stenehjem, E.; Grannis, S.; Ball, S.W.; Naleway, A.L.; Ong, T.C.; DeSilva, M.B.; Natarajan, K.; Bozio, C.H.; Lewis, N.; et al. Effectiveness of COVID-19 vaccines in ambulatory and inpatient care settings. N. Engl. J. Med. 2021, 385, 1355–1371. [Google Scholar] [CrossRef]
- Pilishvili, T.; Gierke, R.; Fleming-Dutra, K.E.; Farrar, J.L.; Mohr, N.M.; Talan, D.A.; Krishnadasan, A.; Harland, K.K.; Smithline, H.A.; Hou, P.C.; et al. Effectiveness of mRNA COVID-19 vaccine among U.S. health care personnel. N. Engl. J. Med. 2021, 385, e90. [Google Scholar] [CrossRef]
- Khoury, D.S.; Cromer, D.; Reynaldi, A.; Schlub, T.E.; Wheatley, A.K.; Juno, J.A.; Subbarao, K.; Kent, S.J.; Triccas, J.A.; Davenport, M.P. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021, 27, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Tartof, S.Y.; Slezak, J.M.; Fischer, H.; Hong, V.; Ackerson, B.K.; Ranasinghe, O.N.; Frankland, T.B.; Ogun, O.A.; Zamparo, J.M.; Gray, S.; et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 2021, 398, 1407–1416. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Self, W.H.; Naioti, E.A.; Ginde, A.A.; Douin, D.J.; Olson, S.M.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; Zepeski, A.; et al. Sustained effectiveness of Pfizer-BioNTech and Moderna vaccines against COVID-19 associated hospitalizations among adults-United States, March-July 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1156–1162. [Google Scholar] [CrossRef] [PubMed]
- Corona Tracker. Bangladesh Overview. 2022. Available online: https://www.coronatracker.com/country/bangladesh/ (accessed on 3 March 2022).
- Government of Pakistan. COVID-19 Dashboard. 2022. Available online: https://covid.gov.pk/stats/pakistan (accessed on 3 March 2022).
- COVID-19 Vaccination Dashboard for Bangladesh. Vaccination. 2022. Available online: https://dghs-dashboard.com/pages/covid19-vaccination-update.php (accessed on 3 March 2022).
- World Bank. Population, Total-Bangladesh. 2020. Available online: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=BD (accessed on 25 January 2022).
- World Bank. Population, Total-Pakistan. 2020. Available online: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=PK (accessed on 25 January 2022).
- COVID-19 Dynamic Facility Dashboard for Bangladesh. Hospital Information. 2021. Available online: https://dghs-dashboard.com/pages/covid19-bedstatus-display.php (accessed on 20 November 2021).
- Bhutta, Z.A.; Sultan, F.; Ikram, A.; Haider, A.; Hafeez, A.; Islam, M. Balancing science and public policy in Pakistan’s COVID-19 response. East. Mediterr. Health J. 2021, 27, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Wahl, B.; Dudala, S.R.; Gopal, K.; Mohan, B.C.; Neelima, S.; Jawahar Reddy, K.S.; Radhakrishnan, J.; Lewnard, J.A. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 2020, 370, 691–697. [Google Scholar] [CrossRef]
- Mukaddes, A.M.M.; Sannyal, M.; Ali, Q.; Kuhel, M.T. Transmission dynamics of COVID-19 in Bangladesh—A compartmental modeling approach. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Gathungu, D.K.; Ojiambo, V.N.; Kimathi, M.E.M.; Mwalili, S.M. Modeling the Effects of Nonpharmaceutical Interventions on COVID-19 Spread in Kenya. Interdiscip. Perspect. Infect. Dis. 2020, 2020, 6231461. [Google Scholar] [CrossRef] [PubMed]
- Pathak, E.B.; Garcia, R.B.; Menard, J.M.; Salemi, J.L. Out-of-Hospital COVID-19 Deaths: Consequences for Quality of Medical Care and Accuracy of Cause of Death Coding. Am. J. Public Health 2021, 111, S101–S106. [Google Scholar] [CrossRef]
- Piroth, L.; Cottenet, J.; Mariet, A.-S.; Bonniaud, P.; Blot, M.; Tubert-Bitter, P.; Quantin, C. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: A nationwide, population-based retrospective cohort study. Lancet Respir. Med. 2021, 9, 251–259. [Google Scholar] [CrossRef]
- Singh, A.; Bajpai, M.K.; Gupta, S.L. A Time-dependent mathematical model for COVID-19 transmission dynamics and analysis of critical and hospitalized cases with bed requirements. medRxiv, 2020. [Google Scholar] [CrossRef]
- Centers of Disease Control and Prevention. Overview of Testing for SARS-CoV-2, the Virus that Causes COVID-19. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html (accessed on 25 January 2022).
- Bi, Q.; Wu, Y.; Mei, S.; Ye, C.; Zou, X.; Zhang, Z.; Liu, X.; Wei, L.; Truelove, S.A.; Zhang, T.; et al. Epidemiology and Transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1286 of their close contacts. medRxiv, 2020. [Google Scholar] [CrossRef]
- Centers of Disease Control and Prevention. COVID-19 Pandemic Planning Scenarios. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html (accessed on 25 January 2022).
- Kolifarhood, G.; Aghaali, M.; Saadati, H.M.; Taherpour, N.; Rahimi, S.; Izadi, N.; Nazari, S.S.H. Epidemiological and clinical aspects of COVID-19; A narrative review. Arch. Acad. Emerg. Med. 2020, 8, e41. [Google Scholar]
- Campillo-Funollet, E.; Van Yperen, J.; Allman, P.; Bell, M.; Beresford, W.; Clay, J.; Dorey, M.; Evans, G.; Gilchrist, K.; Memon, A.; et al. Predicting and forecasting the impact of local outbreaks of COVID-19: Use of SEIR-D quantitative epidemiological modelling for healthcare demand and capacity. Int. J. Epidemiol. 2021, 50, 1103–1113. [Google Scholar] [CrossRef]
- Crawfurd, L.; Hares, S.; Minardi, A.L. New Data on Learning Loss in Pakistan. 2021. Available online: https://www.cgdev.org/blog/new-data-learning-loss-pakistan (accessed on 25 January 2022).
- Fliegauf, E.; Ayres, A. Coronavirus in South Asia, March 24, 2020: Outbreak in Pakistan and India on Lockdown. 2020. Available online: https://www.cfr.org/blog/coronavirus-south-asia-march-24-2020-outbreak-pakistan-and-india-lockdown (accessed on 25 January 2022).
- Geo News. Ramadan 2020 Pakistan: Sehri Time Gujranwala, Iftar Time Gujranwala, Ramadan Calendar. 2020. Available online: https://www.geo.tv/latest/284292-ramadan-2020-pakistan-sehri-time-gujranwala-iftar-time-gujranwala-ramadan-calendar (accessed on 25 January 2022).
- Ministry of Information and Broadcasting, Government of Pakistan. NCOC through TTQ Identified Top 20 Cities across Pakistan with Potential COVID-19 Hotspots/Clusters. 2020. Available online: http://pid.gov.pk/site/press_detail/13906 (accessed on 25 January 2022).
- Times Now Digital. Muharram Day of Ashura 2020: Date and Everything You Need to Know about It. 2020. Available online: https://www.timesnownews.com/spiritual/religion/article/muharram-day-of-ashura-2020-date-and-everything-you-need-to-know-about-its-significance/643371 (accessed on 25 January 2022).
- Trending, F.P. Eid Milad-un-Nabi 2020: History, Importance and Significance of Event Marking Birth and Death Anniversary of Prophet Muhammad. 2020. Available online: https://www.firstpost.com/india/eid-milad-un-nabi-2020-history-importance-and-significance-of-event-marking-birth-and-death-anniversary-of-prophet-muhammadd-8957751.html (accessed on 25 January 2022).
- Mati, U. Raiwind Tableeghi Ijtema 2020 Will be Held on November 6, 7 & 8. 2020. Available online: https://dnd.com.pk/raiwind-tableeghi-ijtema-2020-will-be-held-on-november-6-7-8/200469 (accessed on 25 January 2022).
- Waseem, F. Pakistan Observes Quaid Day with National Affection on Dec 25, 2020. 2020. Available online: https://pardachaak.pk/?p=863 (accessed on 25 January 2022).
- Noman, M. Ramadan Calendar Pakistan 2021: Sehri and Iftar Timings 2021. 2021. Available online: https://www.bolnews.com/islam/2021/04/ramadan-calendar-pakistan-2021-sehri-and-iftar-timings-2021/ (accessed on 25 January 2022).
- Business Standard. Pak Imposes 10-Day Countrywide Lockdown from May 8 to Control COVID. 2021. Available online: https://www.business-standard.com/article/current-affairs/pak-imposes-10-day-countrywide-lockdown-from-may-8-to-control-covid-121050800752_1.html (accessed on 25 January 2022).
- National Humanitarian Network Pakistan. Sindh Lockdown Notification 14 July 2021. 2021. Available online: http://nhnpakistan.org/wp-content/uploads/2021/07/Sindh-Lockdown-Notification-14-July-2021.pdf (accessed on 25 January 2022).
- National Humanitarian Network Pakistan. Karachi Smart Lockdown Notification 24 July 2021. 2021. Available online: http://nhnpakistan.org/wp-content/uploads/2021/07/Karachi-Smart-Lockdown-Notification-24-July-2021.pdf (accessed on 25 January 2022).
- National Humanitarian Network Pakistan. Balochistan District Kech Lockdown Notification 24 July 2021. 2021. Available online: http://nhnpakistan.org/wp-content/uploads/2021/07/Balochistan-District-Kech-Lockdown-Notification-24-July-2021.pdf (accessed on 25 January 2022).
- The Express Tribune. Eid holidays from July 20 to 22. 2021. Available online: https://tribune.com.pk/story/2310168/eid-holidays-from-july-20-to-22 (accessed on 25 January 2022).
- Shiraz, Z. Muharram 2021: Date of Ashura in India, Saudi Arabia and Other Countries. 2021. Available online: https://www.hindustantimes.com/lifestyle/festivals/muharram-2021-date-of-ashura-in-india-saudi-arabia-and-other-countries-101629272748266.html (accessed on 25 January 2022).
- The Express Tribune. Govt Announces Two-Day Public Holiday on Aug 18–19 for Ashura. 2021. Available online: https://tribune.com.pk/story/2315436/govt-announces-two-day-public-holiday-on-aug-18-19-for-ashura (accessed on 25 January 2022).
- Daily Pakistan. Pakistan Announces Public Holiday on Oct 19 to Mark Eid Milad-un-Nabi. 2021. Available online: https://en.dailypakistan.com.pk/15-Oct-2021/pakistan-announces-public-holiday-on-oct-19-to-mark-eid-milad-un-nabi (accessed on 25 January 2022).
- TheNews. Nation Celebrates Quaid-i-Azam’s Birth Anniversary Today. 2021. Available online: https://www.thenews.com.pk/print/919584-nation-celebrates-quaid-i-azam-s-birth-anniversary-today (accessed on 25 January 2022).
- Latif, A. Pakistan Confirms 1st Case of Omicron Variant. 2021. Available online: https://www.aa.com.tr/en/asia-pacific/pakistan-confirms-1st-case-of-omicron-variant/2446183 (accessed on 25 January 2022).
- National Humanitarian Network Pakistan. Karachi Central Smart Lockdown Notification 22 January 2022. 2022. Available online: http://nhnpakistan.org/wp-content/uploads/2022/01/Karachi-Central-Smart-Lockdown-Notification-22-January-2022.pdf (accessed on 25 January 2022).
- Crisis24. Pakistan: Authorities Relaxing Domestic COVID-19 Restrictions as of Feb. 17/Update 66. 2022. Available online: https://crisis24.garda.com/alerts/2022/02/pakistan-authorities-relaxing-domestic-covid-19-restrictions-as-of-feb-17-update-66 (accessed on 8 March 2022).
- BetterWork. COVID-19 Timeline in Bangladesh. 2021. Available online: https://betterwork.org/portfolio/covid-timeline-in-bangladesh/ (accessed on 25 January 2022).
- Crisis24. Bangladesh: Three-Day Holiday Announced for Eid al-Adha from July 31 to August 2. 2020. Available online: https://crisis24.garda.com/alerts/2020/07/bangladesh-three-day-holiday-announced-for-eid-al-adha-from-july-31-to-august-2 (accessed on 27 January 2022).
- DhakaTribune. National Mourning Day Being Observed. 2020. Available online: https://archive.dhakatribune.com/bangladesh/2020/08/15/national-mourning-day-being-observed-2 (accessed on 27 January 2022).
- DhakaTribune. Lakshmi Puja on Friday. 2020. Available online: https://archive.dhakatribune.com/bangladesh/2020/10/29/lakshmi-puja-on-friday (accessed on 27 January 2022).
- DhakaTribune. Bangladesh Celebrates 50th Victory Day. 2020. Available online: https://archive.dhakatribune.com/bangladesh/2020/12/15/49th-victory-day-on-wednesday (accessed on 27 January 2022).
- Latestly. Language Movement Day 2020 Date: History & Significance of the Day in Bangladesh Also Known as Shohid Dibos. 2020. Available online: https://www.latestly.com/lifestyle/festivals-events/language-movement-day-2020-date-history-significance-of-the-day-in-bangladesh-also-known-as-shohid-dibos-1548649.html (accessed on 27 January 2022).
- XinHuaNet. Bangladesh Kicks off 10-Day Special Events to Mark Founding Father’s Birth Centenary, Golden Jubilee of Independence. 2021. Available online: http://www.xinhuanet.com/english/2021-03/17/c_139817322.htm (accessed on 27 January 2022).
- Colombo Plan Staff College. Bangladesh Celebrates Its Golden Anniversary as an Independent Nation. 2021. Available online: https://www.cpsctech.org/2021/03/bangladesh-celebrates-its-golden.html (accessed on 27 January 2022).
- IndiaToday. Pohela Boishakh 2021: Check Out Bengali New Year Date, Importance and Other Significant Details. 2021. Available online: https://www.indiatoday.in/information/story/pohela-boishakh-2021-check-out-bengali-new-year-date-importance-and-other-significant-details-1790828-2021-04-14 (accessed on 27 January 2022).
- BdNews24. Bangladesh to Celebrate Eid-ul-Fitr on Friday Amid Pandemic Lockdown. 2021. Available online: https://bdnews24.com/bangladesh/2021/05/12/bangladesh-to-celebrate-eid-ul-fitr-on-friday-amid-pandemic-lockdown (accessed on 27 January 2022).
- Time and Date. Buddha Purnima/Vesak in Bangladesh. 2021. Available online: https://www.timeanddate.com/holidays/bangladesh/buddha-purnima (accessed on 27 January 2022).
- Dhaka Tribune. Bangladesh Celebrates Eid-ul-Azha Amid Pandemic. 2021. Available online: https://archive.dhakatribune.com/bangladesh/2021/07/21/bangladesh-celebrates-eid-ul-azha-amid-pandemic (accessed on 27 January 2022).
- Kumar, S. Bangladesh Embassy Observes National Mourning Day 2021. 2021. Available online: http://www.koreaherald.com/view.php?ud=20210816000253 (accessed on 27 January 2022).
- Financial Express. Janmashtami 2021: Here’s How Bangladesh, Other Places Celebrated the Festival. 2021. Available online: https://www.financialexpress.com/lifestyle/janmashtami-2021-heres-how-bangladesh-other-places-celebrated-the-festival/2321954/ (accessed on 27 January 2022).
- Sakib, S.M.N. Bangladesh Reports Sharp Rise in COVID-19 Infections Amid Omicron Fears. 2022. Available online: https://www.aa.com.tr/en/asia-pacific/bangladesh-reports-sharp-rise-in-covid-19-infections-amid-omicron-fears/2463423 (accessed on 8 March 2022).
- Trending, F.P. International Mother Language Day 2022: History, Theme and Significance. 2022. Available online: https://www.firstpost.com/world/international-mother-language-day-2022-history-theme-and-significance-10386841.html (accessed on 8 March 2022).
- Jha, R. Bangladesh Notifies Restrictions on Public Gathering, Transport, Restaurants, COVID Vaccination Certificate Required for Arriving Passengers. 2022. Available online: https://newsonair.com/2022/01/10/bangladesh-notifies-restrictions-on-public-gathering-transport-restaurants-covid-vaccination-certificate-required-for-arriving-passengers/ (accessed on 8 March 2022).
- The Financial Express. Bangladesh Extends Pandemic Restrictions to February 21. 2022. Available online: https://thefinancialexpress.com.bd/national/bangladesh-extends-pandemic-restrictions-to-february-21-1643870769 (accessed on 8 March 2022).

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, W.; Huggins, T.; Zheng, W.; Liu, S.; Du, Z.; Zhu, H.; Raza, A.; Tareq, A.H. Assessing the Dynamic Outcomes of Containment Strategies against COVID-19 under Different Public Health Governance Structures: A Comparison between Pakistan and Bangladesh. Int. J. Environ. Res. Public Health 2022, 19, 9239. https://doi.org/10.3390/ijerph19159239
Zhang W, Huggins T, Zheng W, Liu S, Du Z, Zhu H, Raza A, Tareq AH. Assessing the Dynamic Outcomes of Containment Strategies against COVID-19 under Different Public Health Governance Structures: A Comparison between Pakistan and Bangladesh. International Journal of Environmental Research and Public Health. 2022; 19(15):9239. https://doi.org/10.3390/ijerph19159239
Chicago/Turabian StyleZhang, Weiwei, Thomas Huggins, Wenwen Zheng, Shiyong Liu, Zhanwei Du, Hongli Zhu, Ahmad Raza, and Ahmad Hussen Tareq. 2022. "Assessing the Dynamic Outcomes of Containment Strategies against COVID-19 under Different Public Health Governance Structures: A Comparison between Pakistan and Bangladesh" International Journal of Environmental Research and Public Health 19, no. 15: 9239. https://doi.org/10.3390/ijerph19159239
APA StyleZhang, W., Huggins, T., Zheng, W., Liu, S., Du, Z., Zhu, H., Raza, A., & Tareq, A. H. (2022). Assessing the Dynamic Outcomes of Containment Strategies against COVID-19 under Different Public Health Governance Structures: A Comparison between Pakistan and Bangladesh. International Journal of Environmental Research and Public Health, 19(15), 9239. https://doi.org/10.3390/ijerph19159239





