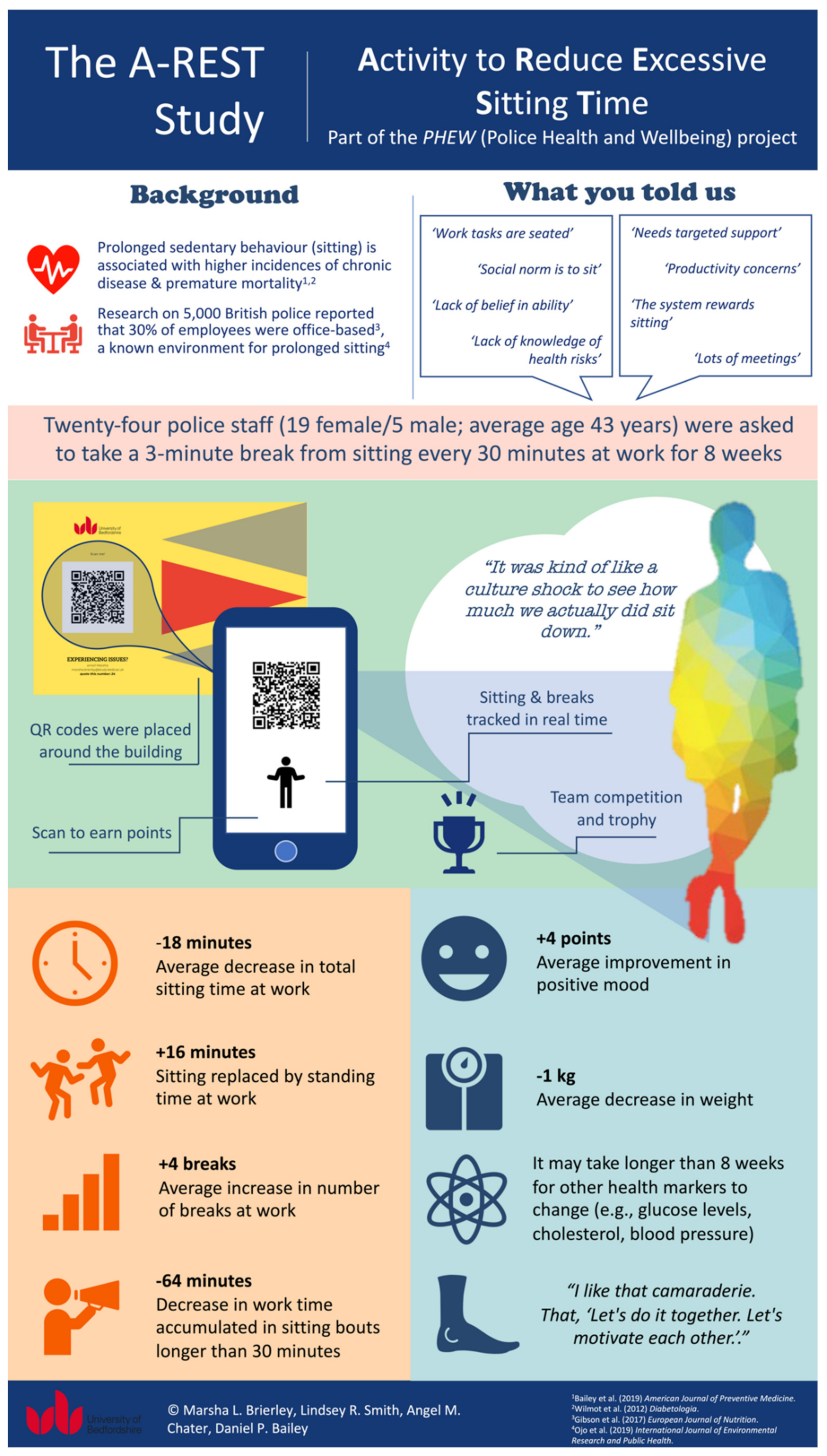
A-REST (Activity to Reduce Excessive Sitting Time): A Feasibility Trial to Reduce Prolonged Sitting in Police Staff
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Overview
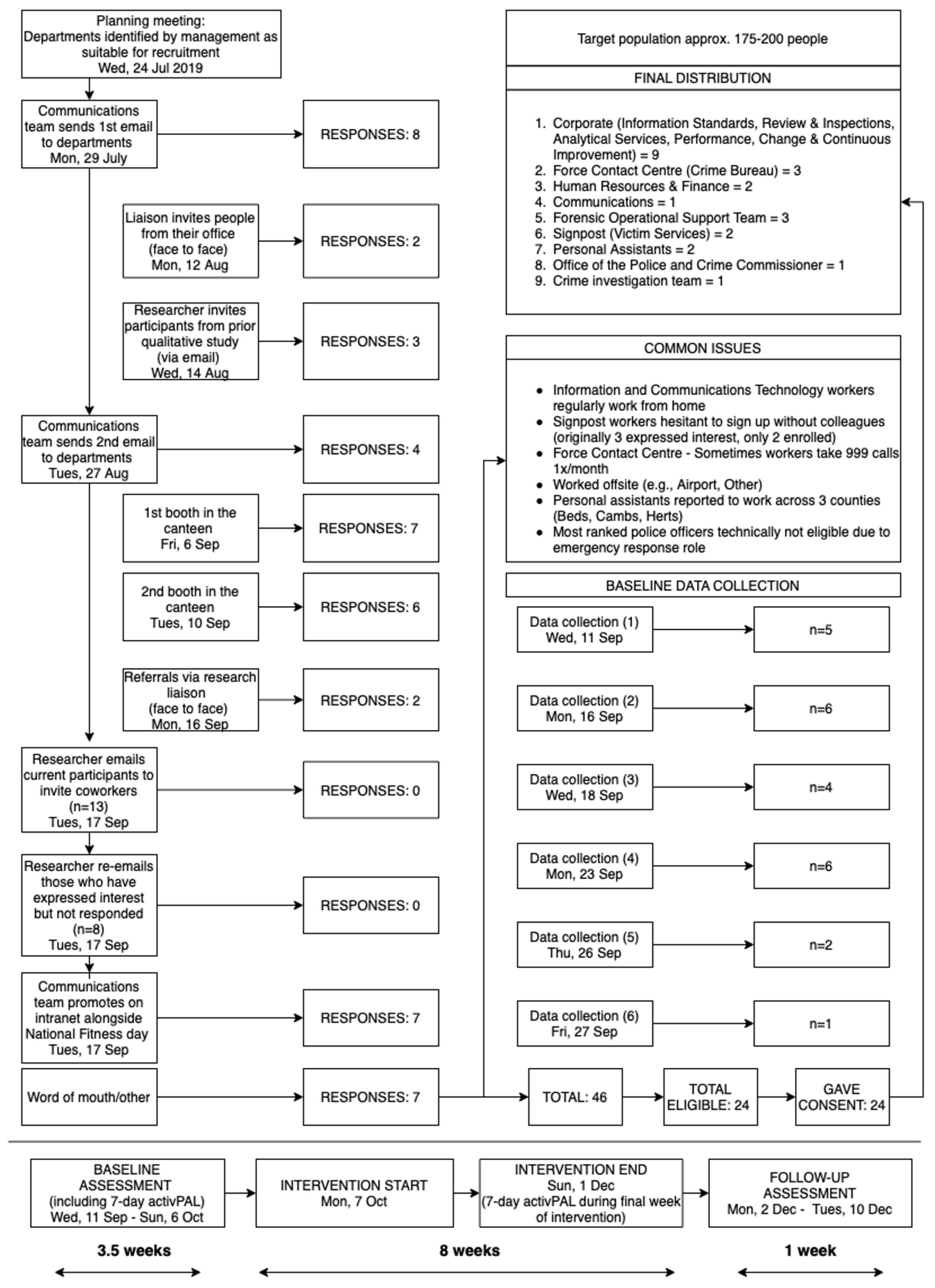
2.1.1. Study Setting and Recruitment
2.1.2. Sample Size
2.1.3. Eligibility Criteria
2.1.4. The A-REST Intervention
2.1.5. Demographic Measurements
2.2. Outcome Measurements
2.2.1. Primary Outcome—Feasibility and Acceptability
2.2.2. Secondary Outcome—Potential Effects
- Sitting, standing, and stepping
- Anthropometric, cardiometabolic risk marker, and psychometric measures
- Post-intervention interviews
2.3. Data Analysis
2.3.1. Primary Outcome—Feasibility and Acceptability
2.3.2. Secondary Outcome—Potential Effects
3. Results
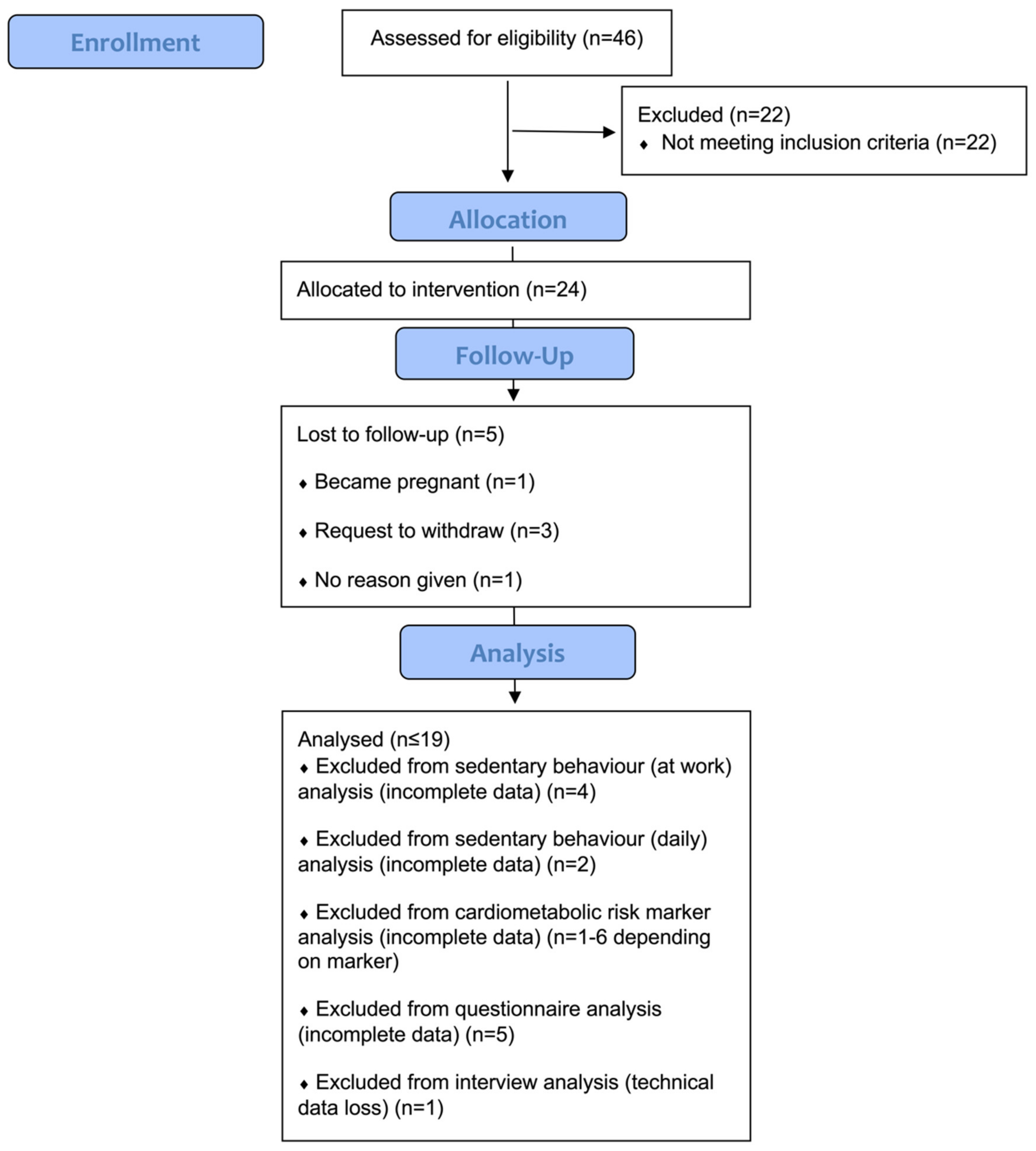
- Participation rates and sample description
3.1. Primary Outcome—Feasibility and Acceptability
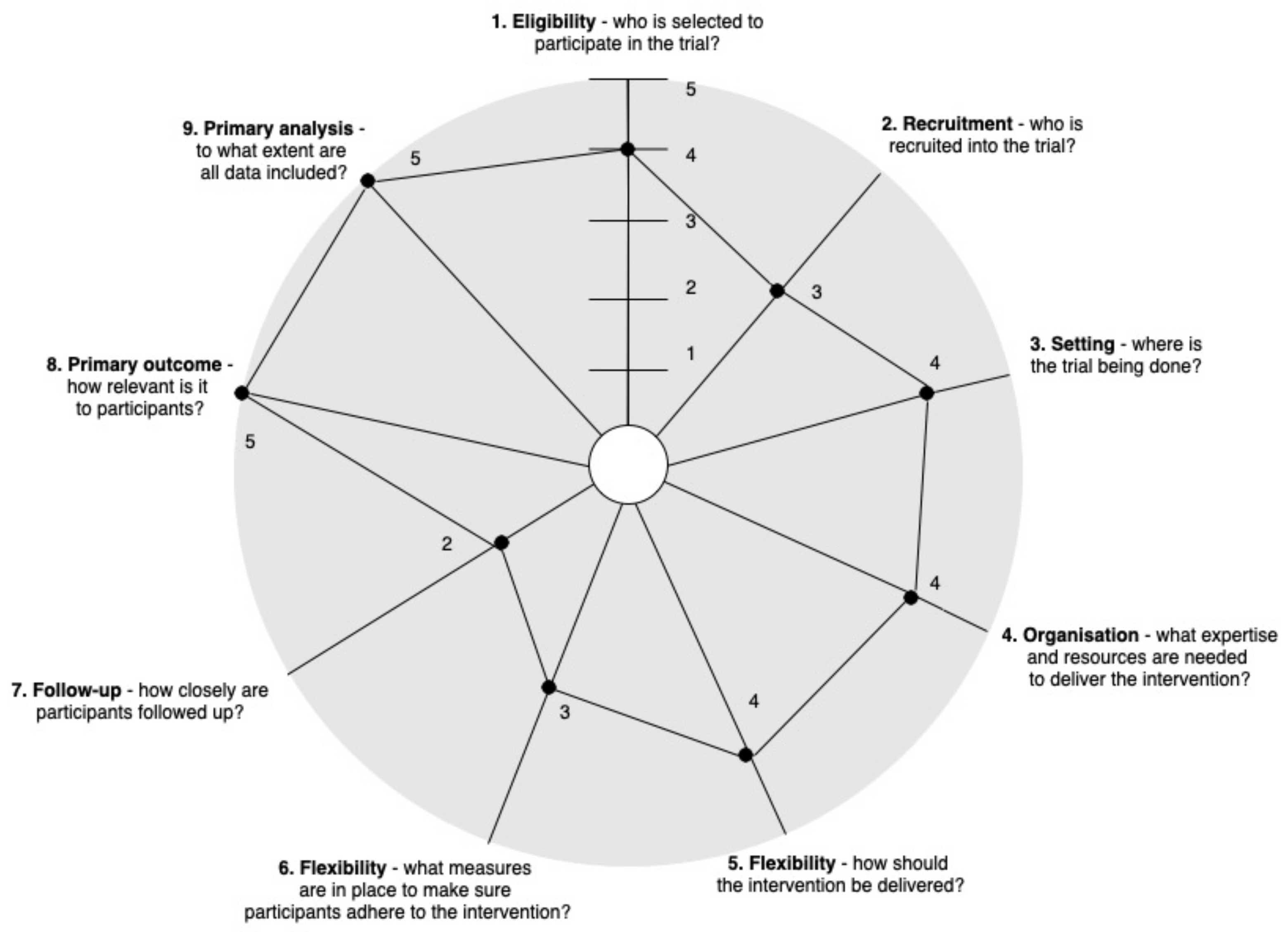
3.1.1. PRECIS-2: How Pragmatic Was the A-REST Intervention?
- 1.
- Eligibility—Rated 4
- 2.
- Recruitment—Rated 3
- 3.
- Setting—Rated 4
- 4.
- Organisation—Rated 4
- 5.
- Flexibility of delivery—Rated 4
- 6.
- Flexibility of adherence—Rated 3
- 7.
- Follow-up—Rated 2
- 8.
- Primary outcome—Rated 5
- 9.
- Primary analysis—Rated 5
3.1.2. Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM)
- Reach
- Effectiveness
- Adoption (by people who deliver the programme)
- Adoption (by settings)
- Implementation (by people who deliver the programme)
- Implementation (individual)
- Education sessionTo accommodate varying work shift patterns and availability, the education session was offered at four different times over four days during week one of the intervention. Five participants were unable to attend any education sessions and were thus hand-delivered the A-REST booklet and education session materials (a handout with suggestions for electronic prompt tools) by the research liaison. For those who attended, the educational lecture was delivered as intended and appeared useful for providing information about health consequences:“I was surprised by the basis for it. How detrimental the sitting, excessive sitting is. I hadn’t really thought about it”.(P5)
- A-REST bookletThe booklet was completed by participants as intended during the education session, but it was not particularly memorable as indicated during the interviews; the education session itself was remembered better. Participants generally found the booklet useful, but most did not use it beyond the education session:“It was probably more useful going through it in a big group. I thought that was quite good in that but honestly, I didn’t refer to it afterwards”.(P1)Participants who did not attend an education session most likely did not complete the booklet. Managers stated that they participated in the study to demonstrate solidarity with employees:“To be honest, it [the booklet] wasn’t overly relevant. Just because of what I’ve said earlier I was mostly more focused on the health bit and making sure the organisation are taking part rather than myself”.(P17)
- Electronic promptsTo begin with, implementation of some intervention components had to be adapted due to security permissions. For example, because free computer prompt software options were open source, it was not possible to use these in a high security setting, and there was neither the time nor the resources to procure closed source software. The intervention was adapted by instructing individuals to choose from a selection of electronic prompts available on their phone or computer (e.g., phone app, recurring calendar appointment, or alarm). It was hypothesised that if the participant chose their preferred mode of prompting, they would be more likely to engage with it. Engagement with the prompts varied based on the individual but according to the interviews, the majority of participants used a prompt tool or were prompted to break up their sitting by their colleague’s prompt tool or behaviour:“I think having several people in the office did, it really helped because as I said, especially those that are more regimented and sat at their desk, they would have an alarm set. They would get up every, so, literally one person would get up and all of us would go, ‘It’s time!’ and follow each other up”.(P14)Over time, participants began to anticipate the prompt showing improved awareness of time spent sitting:“As time went on, I kind of got used to it and then I was looking for it, even before it pinged, if you know what I mean. But, and I think the QR code really helped in like giving you a reason to get up”.(P8)
- QR codesParticipants indicated that the most frequently used QR codes were those located within their respective offices:“Just it [the office QR code] was the closest by. I did use the one in the canteen a few times. And I used the one that I had on the card as well for like the meetings”.(P9)Evidence of behaviour patterns emerged; for example, a couple of participants regularly walked during their breaks and would scan the same QR codes in the order that they passed them. Participants still found it challenging to take breaks and/or stand during meetings:“Yeah, I’ll have a meeting and, well, we said this before about maybe standing up, but yeah in practice it doesn’t work so much”.(P4)
- CompetitionThe competition helped make the taking of breaks acceptable because of the team-based nature of it:“I like that camaraderie that, ‘Let’s do it together. Let’s motivate each other”.(P15)A complaint of cheating made in a joking manner over email was explored by the research team in the second week:“They cheated!
”.
(P9)QR code break logs checked by the researcher (MLB) confirmed that two participants were repeatedly logging breaks less than 30 min apart. Once the pattern was detected, the decision was made to cap the number of breaks a participant could claim based on their working hours that day (i.e., 16 breaks in an 8 h workday). The competition also had to be altered due to the very high and very low engagement of certain teams. It was felt that large discrepancies in points between these teams would lead to amotivation among low engagers and therefore the decision was made to average the team points based on participating individuals within the team each week. Interviews revealed that there were occasional issues around internet connectivity and specific devices that affected their ability to log their sitting breaks:“Sometimes mine didn’t register. Because I was going to scan it and I thought I couldn’t connect, particularly downstairs. Or sometimes, my phone’s not brilliant, it wasn’t connecting to wherever it should connect, so it’d scan but then it gets stuck”.(P4) - EmailsParticipants reported looking forward to the emails each week in large part due to finding out the leaderboard standings:“Yeah I liked that. I think that was good and everybody was like, ‘Oh, [colleague’s name] you’ve won again on that team. ((laughs)) Something like that that’s fine, you know, a little bit of fun isn’t it? And a little trophy. ‘Oh yes, we’ve got the trophy’. Yeah so that was good”.(P18)No adaptations were made to the intervention apart from the research liaison adding a personalised message in weeks one and five. Participants did not feel the presence or absence of management’s involvement with the emails impacted how they perceived the message, nor did it affect their engagement with the rest of the intervention. It was generally remarked that they felt supported by the organisation:“I think it’s always good to see little messages and things. That little extra inspiration or something”.(P18)
- Rise and recharge® appMost participants reported downloading and engaging with this sitting break tracking smartphone app:“I quite like the way it laid out like the colours and the circles and things. Quite visual it was easy to see how you’ve done in the day”.(P13)Importantly, the app only gave feedback on break behaviour. The optional prompting function was not operational throughout the entirety of the study and thus was not used by participants. An issue that was sometimes reported was accuracy, but it was unclear if this was due to app performance or participants taking breaks without their phone:“I did wonder whether it was that accurate because there were some times where I swear I’d got up and it hadn’t registered. And I think in that sense, the biggest problem that I had, ‘cos I don’t really have pockets in my trousers, so I’ll just have my phone on my desk so if I do just nip to the toilet or something, I’d often forget to take the phone with me”.(P13)
- Study measurementsReferral letters were provided after baseline measures to participants with cardiometabolic risk marker readings outside of NICE health guidelines (n = 13). A couple of participants remarked on receiving the letters, stating that they impacted their other health behaviours such as nutrition and health seeking behaviour:“My cholesterol was better [at the end] which I was a little bit worried about. And so I did make some dietary changes as well. […] probably, after I received my letter about my cholesterol. So then I decided to just make a few changes”.(P10)”It’s [my cholesterol’s] gone down. So I did have some blood tests last week. So I did show that letter, that is the email that you sent me, I printed it out about my cholesterol. […] Then they were doing like a full body MOT [health] check”.(P12)
- Maintenance (by individuals)
“I don’t think I will do half an hour. I would definitely try and do it in within an hour to be able to get up and go do something. Yeah, I think that would work better for me”.(P12)
“That’s something I’ve been doing with the up and down-y desks. A lot more is standing up and doing the shift”.(P1)
“Generally, I’ll make sure, as I say, I’m making coffee every hour and a half, at least. I’ll be up doing that and obviously taking breaks in between then, so yeah, that is definitely more of a habit”.(P1)
“I mean I would like to [continue] however, in reality, I probably should have bought into the kind of psychological techniques that you suggested early on… largely because of the kinda the extra strain that I was under”.(P12)
- Maintenance (by the organisation)
3.2. Secondary Outcomes
3.2.1. Changes in Workplace Sitting, Standing and Stepping
3.2.2. Changes in Daily Sitting, Standing, and Stepping
3.2.3. Changes in Anthropmetric and Cardiometabolic Risk Markers
3.2.4. Changes in Affect, Wellbeing, Stress, Job Satisfaction and Job Performance
| Variable | Baseline Mean (n = 15) | 95% CI | Post Intervention Mean (n = 15) | 95% CI | Mean Difference | 95% CI | p | Effect Size |
|---|---|---|---|---|---|---|---|---|
| Sitting time (minutes) | 399.21 | 379.29, 419.14 | 381.56 | 358.78, 404.34 | −17.65 | −34.17, −1.13 | 0.04 | 0.46 |
| Sitting time (%) | 83.17 | 79.02, 87.32 | 79.49 | 74.75, 84.24 | −3.68 | −7.12, −0.24 | 0.04 | 0.46 |
| Standing time (minutes) | 52.86 | 36.84, 68.89 | 68.36 | 48.15, 88.56 | 15.49 | 1.87, 29.12 | 0.03 | 0.47 |
| Standing time (%) | 11.01 | 7.67, 14.35 | 14.24 | 10.03, 18.45 | 3.23 | 0.39, 6.07 | 0.03 | 0.47 |
| Time in sitting bouts ≥ 30 min | 249.85 | 218.99, 280.71 | 185.89 | 135.72, 236.07 | −63.95 | −98.59, −29.31 | <0.01 | 0.85 |
| Time in sitting bouts ≥ 30 min (%) | 52.05 | 45.62, 58.48 | 38.73 | 28.27, 49.18 | −13.32 | −20.54, −6.11 | <0.01 | 0.85 |
| Number of sitting bouts ≥ 30 min | 4.70 | 4.25, 5.14 | 3.73 | 2.78, 4.69 | −0.96 | −1.80, −0.12 | 0.03 | 0.72 |
| Number of sit-upright transitions | 22.81 | 19.55, 26.08 | 26.51 | 23.27, 29.76 | 3.70 | 1.39, 6.02 | <0.01 | 0.63 |
| Stepping time (minutes) | 27.92 | 19.52, 36.33 | 30.08 | 22.45, 37.71 | 2.16 | −6.64, 10.96 | 0.61 | 0.15 |
| Number of steps | 2592 | 1689, 3495 | 2711 | 1848, 3574 | 119 | −831, 1069 | 0.79 | 0.07 |
| Variable (Units) | n | Baseline Mean | 95% CI | Post-Intervention Mean | 95% CI | Mean Difference | 95% CI | p | Effect Size |
|---|---|---|---|---|---|---|---|---|---|
| Waist circumference (cm) | 19 | 88.21 | 82.44, 93.98 | 87.77 | 76.12, 99.42 | −0.44 | −2.05, 1.17 | 0.57 | 0.04 |
| Weight (kg) | 19 | 78.47 | 69.98, 86.95 | 77.61 | 57.82, 97.40 | −0.86 | −1.68, −0.03 | 0.04 | 0.05 |
| Body Mass Index (kg/m2) | 19 | 27.59 | 25.15, 30.03 | 27.34 | 20.44, 34.25 | −0.25 | −0.75, 0.25 | 0.32 | 0.05 |
| Body Fat (%) | 19 | 34.24 | 29.83, 38.65 | 33.77 | 19.24, 48.30 | −0.47 | −2.35, 1.41 | 0.60 | 0.05 |
| Fat Free Mass (kg) | 19 | 51.17 | 45.34, 57.01 | 50.97 | 29.67, 72.27 | −0.20 | −1.53, 1.13 | 0.76 | 0.02 |
| Systolic Blood Pressure (mmHg) | 19 | 125.42 | 117.39, 133.45 | 124.81 | 89.27, 160.34 | −0.61 | −5.70, 4.47 | 0.80 | 0.04 |
| Diastolic Blood Pressure (mmHg) | 19 | 83.44 | 77.77, 89.11 | 82.93 | 57.95, 107.91 | −0.51 | −4.74, 3.72 | 0.80 | 0.05 |
| Resting Heart Rate (bpm) | 19 | 65.12 | 58.46, 71.78 | 63.46 | 35.41, 91.50 | −1.67 | −7.54, 4.21 | 0.56 | 0.13 |
| Total Cholesterol (mmol/L) | 18 | 4.94 | 4.43, 5.45 | 4.90 | 2.95, 6.86 | −0.03 | −0.41, 0.34 | 0.86 | 0.04 |
| HDL cholesterol (mmol/L) | 19 | 1.51 | 1.21, 1.80 | 1.52 | −0.20, 3.24 | 0.01 | −0.14, 0.16 | 0.86 | 0.02 |
| Triglycerides (mmol/L) | 19 | 1.13 | 0.77, 1.49 | 1.18 | −1.13, 3.49 | 0.05 | −0.19, 0.29 | 0.65 | 0.07 |
| LDL cholesterol (mmol/L) | 13 | 3.00 | 2.39, 3.62 | 2.74 | −0.14, 5.63 | −0.26 | −0.67, 0.16 | 0.20 | 0.30 |
| Non-HDL cholesterol (mmol/L) | 16 | 3.56 | 3.03, 4.09 | 3.45 | 0.27, 6.62 | −0.11 | −0.48, 0.25 | 0.52 | 0.12 |
| Glucose (mmol/L) | 19 | 4.95 | 4.69, 5.22 | 4.75 | 2.91, 6.59 | −0.20 | −0.45, 0.04 | 0.10 | 0.41 |
| Mean Arterial Pressure (mmHg) | 18 | 97.42 | 91.22, 103.61 | 96.89 | 42.11, 151.66 | −0.53 | −4.77, 3.71 | 0.80 | 0.04 |
| Variable | Baseline Mean | 95% CI | Post-Intervention Mean | 95% CI | Mean Difference | 95% CI | p | Effect Size |
|---|---|---|---|---|---|---|---|---|
| Positive affect | 28.84 | 25.14, 32.55 | 32.47 | 29.69, 35.25 | 3.63 | 0.89, 6.37 | 0.01 | 0.87 |
| Negative affect | 14.32 | 11.66, 16.97 | 14.47 | 11.98, 16.96 | 0.16 | −1.74, 2.06 | 0.86 | 0.04 |
| Wellbeing | 48.58 | 45.58, 51.58 | 49.89 | 47.31, 52.47 | 1.32 | −1.39, 4.02 | 0.32 | 0.20 |
| Occupational stress | 34.37 | 26.70, 42.04 | 34.47 | 28.51, 40.43 | 0.11 | −8.11, 8.32 | 0.98 | 0.01 |
| Organisational stress | 41.53 | 30.25, 52.81 | 44.74 | 32.04, 57.44 | 3.21 | −7.44, 13.86 | 0.54 | 0.17 |
| Job Satisfaction | 5.05 | 4.48, 5.62 | 5.16 | 4.65, 5.67 | 0.11 | −0.32, 0.53 | 0.61 | 0.10 |
| Job Performance | 5.47 | 5.01, 5.93 | 5.63 | 5.23, 6.03 | 0.16 | −0.13, 0.45 | 0.27 | 0.18 |
4. Discussion
4.1. Feasibility and Acceptability of the Intervention
- Pragmatism
- Reach and adoption
- Implementation
- Unintended effects
- Maintenance
4.2. Potential Effects of the Intervention
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parry, S.; Straker, L. The Contribution of Office Work to Sedentary Behaviour Associated Risk. BMC Public Health 2013, 13, 296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorp, A.A.; Healy, G.N.; Winkler, E.; Clark, B.K.; Gardiner, P.A.; Owen, N.; Dunstan, D.W. Prolonged Sedentary Time and Physical Activity in Workplace and Non-Work Contexts: A Cross-Sectional Study of Office, Customer Service and Call Centre Employees. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Khunti, K.; Yates, T.; Biddle, S.J.H. Sedentary Time in Adults and the Association with Diabetes, Cardiovascular Disease and Death: Systematic Review and Meta-Analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef] [PubMed]
- De Rezende, L.F.M.; Lopes, M.R.; Rey-Loṕez, J.P.; Matsudo, V.K.R.; Luiz, O.D.C. Sedentary Behavior and Health Outcomes: An Overview of Systematic Reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef]
- Bailey, D.P.; Hewson, D.J.; Champion, R.B.; Sayegh, S.M. Sitting Time and Risk of Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. Am. J. Prev. Med. 2019, 57, 408–416. [Google Scholar] [CrossRef]
- Dunstan, D.W.; Healy, G.N.; Sugiyama, T.; Owen, N. “Too Much Sitting” and Metabolic Risk—Has Modern Technology Caught up with Us? Eur. Endocrinol. 2010, 6, 19–23. [Google Scholar] [CrossRef] [Green Version]
- Frey, C.B.; Osborne, M.A. The Future of Employment: How Susceptible Are Jobs to Computerisation? Technol. Forecast. Soc. Chang. 2017, 114, 254–280. [Google Scholar] [CrossRef]
- Chau, J.Y.; van der Ploeg, H.P.; van Uffelen, J.G.Z.; Wong, J.; Riphagen, I.; Healy, G.N.; Gilson, N.D.; Dunstan, D.W.; Bauman, A.E.; Owen, N.; et al. Are Workplace Interventions to Reduce Sitting Effective? A Systematic Review. Prev. Med. 2010, 51, 352–356. [Google Scholar] [CrossRef]
- Shrestha, N.; Kukkonen-Harjula, K.T.; Verbeek, J.H.; Ijaz, S.; Hermans, V.; Bhaumik, S. Workplace Interventions for Reducing Sitting at Work. Cochrane Database Syst. Rev. 2016, 43, 136–298. [Google Scholar] [CrossRef] [Green Version]
- Brierley, M.L.; Chater, A.M.; Smith, L.R.; Bailey, D.P. The Effectiveness of Sedentary Behaviour Reduction Workplace Interventions on Cardiometabolic Risk Markers: A Systematic Review. Sports Med. 2019, 49, 1739–1767. [Google Scholar] [CrossRef]
- Buckley, J.P.; Hedge, A.; Yates, T.; Copeland, R.J.; Loosemore, M.; Hamer, M.; Bradley, G.; Dunstan, D.W. The Sedentary Office: An Expert Statement on the Growing Case for Change towards Better Health and Productivity. Br. J. Sports Med. 2015, 49, 1357–1362. [Google Scholar] [CrossRef]
- Gibson, R.; Eriksen, R.; Singh, D.; Vergnaud, A.-C.; Heard, A.; Chan, Q.; Elliott, P.; Frost, G. A Cross-Sectional Investigation into the Occupational and Socio-Demographic Characteristics of British Police Force Employees Reporting a Dietary Pattern Associated with Cardiometabolic Risk: Findings from the Airwave Health Monitoring Study. Eur. J. Nutr. 2017, 57, 2913–2926. [Google Scholar] [CrossRef] [Green Version]
- Elliott, P.; Vergnaud, A.C.; Singh, D.; Neasham, D.; Spear, J.; Heard, A. The Airwave Health Monitoring Study of Police Officers and Staff in Great Britain: Rationale, Design and Methods. Environ. Res. 2014, 134, 280–285. [Google Scholar] [CrossRef] [Green Version]
- Evans, R.E.; Fawole, H.O.; Sheriff, S.A.; Dall, P.M.; Grant, P.M.; Ryan, C.G. Point-of-Choice Prompts to Reduce Sitting Time at Work: A Randomized Trial. Am. J. Prev. Med. 2012, 43, 293–297. [Google Scholar] [CrossRef]
- Kozey-Keadle, S.; Libertine, A.; Staudenmayer, J.; Freedson, P. The Feasibility of Reducing and Measuring Sedentary Time among Overweight, Non-Exercising Office Workers. J. Obes. 2012, 2012, 282303. [Google Scholar] [CrossRef] [Green Version]
- Biddle, S.J.H. Sedentary Behaviour at the Individual Level: Correlates, Theories, and Interventions. In Sedentary Behaviour Epidemiology; Leitzmann, M., Jochem, C., Schmid, D., Eds.; Springer: Cham, Switzerland, 2018; pp. 405–429. [Google Scholar]
- Dutta, N.; Koepp, G.; Stovitz, S.; Levine, J.; Pereira, M. Using Sit-Stand Workstations to Decrease Sedentary Time in Office Workers: A Randomized Crossover Trial. Int. J. Environ. Res. Public Health 2014, 11, 6653–6665. [Google Scholar] [CrossRef] [Green Version]
- Gorman, E.; Ashe, M.C.; Dunstan, D.W.; Hanson, H.M.; Madden, K.; Winkler, E.A.H.; McKay, H.A.; Healy, G.N. Does an ‘Activity-Permissive’ Workplace Change Office Workers’ Sitting and Activity Time? PLoS ONE 2013, 8, e76723-6. [Google Scholar] [CrossRef] [Green Version]
- Graves, L.; Murphy, R.; Shepherd, S.; Cabot, J.; Hopkins, N. Evaluation of Sit-Stand Workstations in an Office Setting: A Randomised Controlled Trial. BMC Public Health 2015, 15, 1145. [Google Scholar] [CrossRef] [Green Version]
- John, D.; Thompson, D.L.; Raynor, H.; Bielak, K.; Rider, B.; Bassett, D.R. Treadmill Workstations: A Worksite Physical Activity Intervention in Overweight and Obese Office Workers. J. Phys. Act. Health 2011, 8, 1034–1043. [Google Scholar] [CrossRef]
- Carr, L.J.; Karvinen, K.; Peavler, M.; Smith, R.; Cangelosi, K. Multicomponent Intervention to Reduce Daily Sedentary Time: A Randomised Controlled Trial. BMJ Open 2013, 3, e003261. [Google Scholar] [CrossRef] [Green Version]
- Danquah, I.H.; Kloster, S.; Holtermann, A.; Aadahl, M.; Bauman, A.; Ersboll, A.K.; Tolstrup, J.S.; Ersbøll, A.K.; Tolstrup, J.S. Take a Stand!—A Multi-Component Intervention Aimed at Reducing Sitting Time among Office Workers-a Cluster Randomized Trial. Int. J. Epidemiol. 2017, 46, 128–140. [Google Scholar] [CrossRef]
- Healy, G.N.; Winkler, E.A.H.H.; Eakin, E.G.; Owen, N.; LaMontagne, A.D.; Moodie, M.; Dunstan, D.W. A Cluster RCT to Reduce Workers’ Sitting Time. Med. Sci. Sports Exerc. 2017, 49, 2032–2039. [Google Scholar] [CrossRef]
- Healy, G.N.; Eakin, E.G.; LaMontagne, A.D.; Owen, N.; Winkler, E.A.H.; Wiesner, G.; Gunning, L.; Neuhaus, M.; Lawler, S.; Fjeldsoe, B.S.; et al. Reducing Sitting Time in Office Workers: Short-Term Efficacy of a Multicomponent Intervention. Prev. Med. 2013, 57, 43–48. [Google Scholar] [CrossRef] [Green Version]
- Neuhaus, M.; Healy, G.N.; Fjeldsoe, B.S.; Lawler, S.; Owen, N.; Dunstan, D.W.; LaMontagne, A.D.; Eakin, E.G. Iterative Development of Stand Up Australia: A Multi-Component Intervention to Reduce Workplace Sitting. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 21. [Google Scholar] [CrossRef] [Green Version]
- Shrestha, N.; Kukkonen-Harjula, K.T.; Verbeek, J.H.; Ijaz, S.; Hermans, V.; Pedisic, Z. Workplace Interventions for Reducing Sitting at Work. Cochrane Database Syst. Rev. 2018, 6, CD010912. [Google Scholar] [CrossRef] [Green Version]
- Neuhaus, M.; Healy, G.N.; Dunstan, D.W.; Owen, N.; Eakin, E.G. Workplace Sitting and Height-Adjustable Workstations: A Randomized Controlled Trial. Am. J. Prev. Med. 2014, 46, 30–40. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Healthy Workplaces: A Model for Action: For Employers, Workers, Policy-Makers and Practitioners. Available online: https://www.who.int/occupational_health/publications/healthy_workplaces_model_action.pdf (accessed on 15 March 2022).
- Medical Research Council A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health. Int. J. Pharm. Pract. 2000, 14, 233–234.
- Macmillan, F.; Karamacoska, D.; El Masri, A.; McBride, K.A.; Steiner, G.Z.; Cook, A.; Kolt, G.S.; Klupp, N.; George, E.S. A Systematic Review of Health Promotion Intervention Studies in the Police Force: Study Characteristics, Intervention Design and Impacts on Health. Occup. Environ. Med. 2017, 74, 913–923. [Google Scholar] [CrossRef]
- Macdonald, B.; Janssen, X.; Kirk, A.; Patience, M.; Gibson, A.M. An Integrative, Systematic Review Exploring the Research, Effectiveness, Adoption, Implementation, and Maintenance of Interventions to Reduce Sedentary Behaviour in Office Workers. Int. J. Environ. Res. Public Health 2018, 15, 2876. [Google Scholar] [CrossRef] [Green Version]
- Loudon, K.; Treweek, S.; Sullivan, F.; Donnan, P.; Thorpe, K.E.; Zwarenstein, M. The PRECIS-2 Tool: Designing Trials That Are Fit for Purpose. BMJ 2015, 350, h2147. [Google Scholar] [CrossRef] [Green Version]
- Thorpe, K.E.; Zwarenstein, M.; Oxman, A.D.; Treweek, S.; Furberg, C.D.; Altman, D.G.; Tunis, S.; Bergel, E.; Harvey, I.; Magid, D.J.; et al. A Pragmatic-Explanatory Continuum Indicator Summary (PRECIS): A Tool to Help Trial Designers. J. Clin. Epidemiol. 2009, 62, 464–475. [Google Scholar] [CrossRef] [PubMed]
- Gaglio, B.; Shoup, J.A.; Glasgow, R.E. The RE-AIM Framework: A Systematic Review of Use over Time. Am. J. Public Health 2013, 103, 9. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the Public Health Impact of Health Promotion Interventions: The RE-AIM Framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauman, A.; Nutbeam, D. Theory in a Nutshell: A Practical Guide to the Evaluation of Health Promotion Programs, 2nd ed.; McGraw-Hill: Sydney, Australia, 2013; ISBN 978-0074713327. [Google Scholar]
- Gaglio, B.; Phillips, S.M.; Heurtin-Roberts, S.; Sanchez, M.A.; Glasgow, R.E. How Pragmatic Is It? Lessons Learned Using PRECIS and RE-AIM for Determining Pragmatic Characteristics of Research. Implement. Sci. 2014, 9, 96. [Google Scholar] [CrossRef] [Green Version]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; Altman, D.; Bretz, F.; Campbell, M.; et al. CONSORT 2010 Statement: Extension to Randomised Pilot and Feasibility Trials. BMJ 2016, 2, 64. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Hooper, R. Justifying Sample Size for a Feasibility Study. Available online: https://www.rds-london.nihr.ac.uk/resources/justify-sample-size-for-a-feasibility-study/ (accessed on 15 March 2022).
- Sim, J.; Lewis, M. The Size of a Pilot Study for a Clinical Trial Should Be Calculated in Relation to Considerations of Precision and Efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef]
- Julious, S.A. Sample Size of 12 per Group Rule of Thumb for a Pilot Study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions, 1st ed.; Silverback Publishing: Sutton, UK, 2014; ISBN 978-1291846058. [Google Scholar]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Brierley, M.L.; Smith, L.S.; Bailey, D.P.; Every, S.A.; Staines, T.A.; Chater, A.M. Perceived Influences on Reducing Prolonged Sitting in Police Staff: A Qualitative Investigation Using the Theoretical Domains Framework and COM-B Model. BMC Public Health 2021, 21, 2126. [Google Scholar] [CrossRef]
- Ojo, S.O.; Bailey, D.P.; Brierley, M.L.; Hewson, D.J.; Chater, A.M. Breaking Barriers: Using the Behavior Change Wheel to Develop a Tailored Intervention to Overcome Workplace Inhibitors to Breaking up Sitting Time. BMC Public Health 2019, 19, 1126. [Google Scholar] [CrossRef] [Green Version]
- Brierley, M.L.; Smith, L.R.; Bailey, D.P.; Ojo, S.O.; Hewson, D.J.; Every, S.A.; Staines, T.A.; Chater, A.M. Evaluating a Multi-Component Intervention to Reduce and Break up Office Workers’ Sitting with Sit-Stand Desks Using the APEASE Criteria. BMC Public Health 2022, 22, 458. [Google Scholar] [CrossRef]
- Marshall, A.L.; Miller, Y.D.; Burton, N.W.; Brown, W.J. Measuring Total and Domain-Specific Sitting: A Study of Reliability and Validity. Med. Sci. Sports Exerc. 2010, 42, 1094–1102. [Google Scholar] [CrossRef]
- The IPAQ Group. IPAQ: International Physical Activity Questionnaire. Available online: https://sites.google.com/site/theipaq/home (accessed on 6 March 2020).
- Crawford, J.O. The Nordic Musculoskeletal Questionnaire. Occup. Med. 2007, 57, 300–301. [Google Scholar] [CrossRef] [Green Version]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic Questionnaires for the Analysis of Musculoskeletal Symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- World Health Organization. Tobacco Questions for Surveys: A Subset of Key Questions from the Global Adult Tobacco Survey (GATS), 2nd ed.; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). Recommended Alcohol Questions. Available online: https://www.niaaa.nih.gov/research/guidelines-and-resources/recommended-alcohol-questions (accessed on 26 February 2021).
- Weiner, B.J.; Lewis, C.C.; Stanick, C.; Powell, B.J.; Dorsey, C.N.; Clary, A.S.; Boynton, M.H.; Halko, H. Psychometric Assessment of Three Newly Developed Implementation Outcome Measures. Implement. Sci. 2017, 12, 108. [Google Scholar] [CrossRef]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 65–76. [Google Scholar] [CrossRef] [Green Version]
- Loudon, K.; Zwarenstein, M.; Sullivan, F.; Donnan, P.; Treweek, S. Making Clinical Trials More Relevant: Improving and Validating the PRECIS Tool for Matching Trial Design Decisions to Trial Purpose. Trials 2013, 14, 115. [Google Scholar] [CrossRef] [Green Version]
- Matei, R.; Thuné-Boyle, I.; Hamer, M.; Iliffe, S.; Fox, K.R.; Jefferis, B.J.; Gardner, B. Acceptability of a Theory-Based Sedentary Behaviour Reduction Intervention for Older Adults (‘On Your Feet to Earn Your Seat’). BMC Public Health 2015, 15, 606. [Google Scholar] [CrossRef] [Green Version]
- Bellg, A.J.; Resnick, B.; Minicucci, D.S.; Ogedegbe, G.; Ernst, D.; Borrelli, B.; Hecht, J.; Ory, M.; Orwig, D.; Czajkowski, S. Enhancing Treatment Fidelity in Health Behavior Change Studies: Best Practices and Recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004, 23, 443–451. [Google Scholar] [CrossRef]
- Macdonald, B.; Gibson, A.M.; Janssen, X.; Hutchinson, J.; Headley, S.; Matthews, T.; Kirk, A. Should We Scale-up? A Mixed Methods Process Evaluation of an Intervention Targeting Sedentary Office Workers Using the RE-AIM QuEST Framework. Int. J. Environ. Res. Public Health 2020, 17, 239. [Google Scholar] [CrossRef] [Green Version]
- Healy, G.N.; Winkler, E.A.H.; Goode, A.D. A RE-AIM Evaluation in Early Adopters to Iteratively Improve the Online BeUpstanding™ Program Supporting Workers to Sit Less and Move More. BMC Public Health 2021, 21, 1916. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and Evaluating Complex Interventions: The New Medical Research Council Guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [Green Version]
- Lyden, K.; Kozey-Keadle, S.L.; Staudenmayer, J.W.; Freedson, P.S. Validity of Two Wearable Monitors to Estimate Breaks from Sedentary Time. Med. Sci. Sports Exerc. 2012, 44, 2243. [Google Scholar] [CrossRef] [Green Version]
- Grant, P.M.; Ryan, C.G.; Tigbe, W.W.; Granat, M.H. The Validation of a Novel Activity Monitor in the Measurement of Posture and Motion during Everyday Activities. Br. J. Sports Med. 2006, 40, 992–997. [Google Scholar] [CrossRef] [Green Version]
- Ryan, C.G.; Grant, P.M.; Tigbe, W.W.; Granat, M.H. The Validity and Reliability of a Novel Activity Monitor as a Measure of Walking. Br. J. Sports Med. 2006, 40, 779–784. [Google Scholar] [CrossRef] [Green Version]
- Hart, T.L.; Ainsworth, B.E.; Tudor-Locke, C. Objective and Subjective Measures of Sedentary Behavior and Physical Activity. Med. Sci. Sports Exerc. 2011, 43, 449–456. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Rowlands, A.V.; Bunnewell, S.; Sanders, J.; Esliger, D.W.; Gorely, T.; O’Connell, S.; Davies, M.J.; Khunti, K.; Yates, T. Accuracy of Posture Allocation Algorithms for Thigh- and Waist-Worn Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 1085–1090. [Google Scholar] [CrossRef] [Green Version]
- Edwardson, C.L.; Winkler, E.A.H.; Bodicoat, D.H.; Yates, T.; Davies, M.J.; Dunstan, D.W.; Healy, G.N. Considerations When Using the ActivPAL Monitor in Field-Based Research with Adult Populations. J. Sport Health Sci. 2017, 6, 162–178. [Google Scholar] [CrossRef] [Green Version]
- Winkler, E.A.H.; Bodicoat, D.H.; Healy, G.N.; Bakrania, K.; Yates, T.; Owen, N.; Dunstan, D.W.; Edwardson, C.L. Identifying Adults’ Valid Waking Wear Time by Automated Estimation in ActivPAL Data Collected with a 24 h Wear Protocol. Physiol. Meas. 2016, 37, 1653. [Google Scholar] [CrossRef] [Green Version]
- Meaney, E.; Alva, F.; Moguel, R.; Meaney, A.; Alva, J.; Webel, R. Formula and Nomogram for the Sphygmomanometric Calculation of the Mean Arterial Pressure. Heart 2000, 84, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCreary, D.R.; Thompson, M.M. Development of Two Reliable and Valid Measures of Stressors in Policing: The Operational and Organizational Police Stress Questionnaires. Int. J. Stress Manag. 2006, 13, 494. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-Being Scale. Health Qual Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and Validation of Brief Measures of Positive and Negative Affect: The PANAS Scales. EPJ Web Conf. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Maylor, B.D.; Edwardson, C.L.; Zakrzewski-Fruer, J.K.; Champion, R.B.; Bailey, D.P. Efficacy of a Multicomponent Intervention to Reduce Workplace Sitting Time in Office Workers: A Cluster Randomized Controlled Trial. J. Occup. Environ. Med. 2018, 60, 787–795. [Google Scholar] [CrossRef] [Green Version]
- Edwardson, C.L.; Yates, T.; Biddle, S.J.H.; Davies, M.J.; Dunstan, D.W.; Esliger, D.W.; Gray, L.J.; Jackson, B.; O’Connell, S.E.; Waheed, G.; et al. Effectiveness of the Stand More AT (SMArT) Work Intervention: Cluster Randomised Controlled Trial. BMJ 2018, 363, k3870. [Google Scholar] [CrossRef] [Green Version]
- Ojo, S.O.; Bailey, D.P.; Hewson, D.J.; Chater, A.M. Perceived Barriers and Facilitators to Breaking up Sitting Time among Desk-Based Office Workers: A Qualitative Investigation Using the TDF and COM-B. Int. J. Environ. Res. Public Health 2019, 16, 2903. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the Framework Method for the Analysis of Qualitative Data in Multi-Disciplinary Health Research. BMC Med. Res. Methodol. 2013, 13, 1. [Google Scholar] [CrossRef] [Green Version]
- Norris, E.; Dunsmuir, S.; Duke-Williams, O.; Stamatakis, E.; Shelton, N. Mixed Method Evaluation of the Virtual Traveller Physically Active Lesson Intervention: An Analysis Using the RE-AIM Framework. Eval. Program Plan. 2018, 70, 107–114. [Google Scholar] [CrossRef]
- Wasserstein, R.L.; Lazar, N.A. The ASA’s Statement on p-Values: Context, Process, and Purpose. Am. Stat. 2016, 70, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–160. [Google Scholar] [CrossRef]
- Bullock, S. An Independent Review into the Strategic Factors Impacting Bedfordshire Police; (Internal Report); Police: London, UK, 2017; pp. 1–118.
- Bedfordshire Police. Employee Rank, Role, and Disposition within the Force; Bedfordshire Police: Kempston, UK, 2018.
- Hadgraft, N.T.; Willenberg, L.; LaMontagne, A.D.; Malkoski, K.; Dunstan, D.W.; Healy, G.N.; Moodie, M.; Eakin, E.G.; Owen, N.; Lawler, S.P. Reducing Occupational Sitting: Workers’ Perspectives on Participation in a Multi- Component Intervention. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 73. [Google Scholar] [CrossRef] [Green Version]
- Dewitt, S.; Hall, J.; Smith, L.; Buckley, J.P.; Biddle, S.J.H.; Mansfield, L.; Gardner, B. Office Workers’ Experiences of Attempts to Reduce Sitting-Time: An Exploratory, Mixed-Methods Uncontrolled Intervention Pilot Study. BMC Public Health 2019, 19, 819. [Google Scholar] [CrossRef] [Green Version]
- Buckingham, S.A.; Morrissey, K.; Williams, A.J.; Price, L.; Harrison, J. The Physical Activity Wearables in the Police Force (PAW-Force) Study: Acceptability and Impact. BMC Public Health 2020, 20, 1645. [Google Scholar] [CrossRef]
- Carr, L.J.; Leonhard, C.; Tucker, S.; Fethke, N.; Benzo, R.; Gerr, F. Total Worker Health Intervention Increases Activity of Sedentary Workers. Am. J. Prev. Med. 2016, 50, 9–17. [Google Scholar] [CrossRef]
- Puig-Ribera, A.; Bort-Roig, J.; González-Suárez, A.M.; Martínez-Lemos, I.; Giné-Garriga, M.; Fortuño, J.; Martori, J.C.; Muñoz-Ortiz, L.; Milà, R.; McKenna, J.; et al. Patterns of Impact Resulting from a ‘Sit Less, Move More’ Web-Based Program in Sedentary Office Employees. PLoS ONE 2015, 10, e0122474-15. [Google Scholar] [CrossRef]
- Schuna, J.M.; Swift, D.L.; Hendrick, C.A.; Duet, M.T.; Johnson, W.D.; Martin, C.K.; Church, T.S.; Tudor-Locke, C. Evaluation of a Workplace Treadmill Desk Intervention: A Randomized Controlled Trial. J. Occup. Environ. Med. 2014, 56, 1266–1276. [Google Scholar] [CrossRef] [Green Version]
- Tudor-Locke, C.; Schuna, J.M.; Frensham, L.J.; Proenca, M. Changing the Way We Work: Elevating Energy Expenditure with Workstation Alternatives. Int. J. Obes. 2013, 38, 755–765. [Google Scholar] [CrossRef]
- Munir, F.; Biddle, S.J.H.; Davies, M.J.; Dunstan, D.; Esliger, D.; Gray, L.J.; Jackson, B.R.; O’Connell, S.E.; Yates, T.; Edwardson, C.L. Stand More at Work (SMArT Work): Using the Behaviour Change Wheel to Develop an Intervention to Reduce Sitting Time in the Workplace. BMC Public Health 2018, 18, 319. [Google Scholar] [CrossRef] [Green Version]
- Bailey, D.P.; Edwardson, C.L.; Pappas, Y.; Dong, F.; Hewson, D.J.; Biddle, S.J.H.; Brierley, M.L.; Chater, A.M. A Randomised-Controlled Feasibility Study of the REgulate Your SItting Time (RESIT) Intervention for Reducing Sitting Time in Individuals with Type 2 Diabetes: Study Protocol. Pilot Feasibility Stud. 2021, 7, 76. [Google Scholar] [CrossRef]
- Bond, D.S.; Thomas, J.G.; Raynor, H.A.; Moon, J.; Sieling, J.; Trautvetter, J.; Leblond, T.; Wing, R.R. B-MOBILE—A Smartphone-Based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A within-Subjects Experimental Trial. PLoS ONE 2014, 9, e100821-8. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Edwardson, C.L.; Gorely, T.; Wilmot, E.G.; Yates, T.; Nimmo, M.A.; Khunti, K.; Davies, M.J. Reducing Sedentary Time in Adults at Risk of Type 2 Diabetes: Process Evaluation of the STAND (Sedentary Time ANd Diabetes) RCT. BMC Public Health 2017, 17, 80. [Google Scholar] [CrossRef] [Green Version]
- Voigt, L.; Baumann, S.; Ullrich, A.; Weymar, F.; John, U.; Ulbricht, S. The Effect of Mere Measurement from a Cardiovascular Examination Program on Physical Activity and Sedentary Time in an Adult Population. BMC Sports Sci. 2018, 10, 1. [Google Scholar] [CrossRef] [Green Version]
- Healy, G.N.; Eakin, E.G.; Owen, N.; LaMontagne, A.D.; Moodie, M.; Winkler, E.A.H.; Fjeldsoe, B.S.; Wiesner, G.; Willenberg, L.; Dunstan, D.W. A Cluster Randomized Controlled Trial to Reduce Office Workers’ Sitting Time: Effect on Activity Outcomes. Med. Sci. Sports Exerc. 2016, 48, 1787–1797. [Google Scholar] [CrossRef]
- Lin, Y.-P.; Lin, C.-C.; Chen, M.-M.; Lee, K.-C. Short-Term Efficacy of a “Sit Less, Walk More” Workplace Intervention on Improving Cardiometabolic Health and Work Productivity in Office Workers. J. Occup. Environ. Med. 2017, 59, 327–334. [Google Scholar] [CrossRef]
- Mailey, E.L.; Rosenkranz, S.K.; Casey, K.; Swank, A. Comparing the Effects of Two Different Break Strategies on Occupational Sedentary Behavior in a Real World Setting: A Randomized Trial. Prev. Med. Rep. 2016, 4, 423–428. [Google Scholar] [CrossRef] [Green Version]
- Dunning, J.R.; McVeigh, J.A.; Goble, D.; Meiring, R.M. The Effect of Interrupting Sedentary Behavior on the Cardiometabolic Health of Adults With Sedentary Occupations: A Pilot Study. J. Occup. Environ. Med. 2018, 60, 760–767. [Google Scholar] [CrossRef]
- Mansoubi, M.; Pearson, N.; Biddle, S.J.H.; Clemes, S.A. Using Sit-to-Stand Workstations in Offices: Is There a Compensation Effect? Med. Sci. Sports Exerc. 2016, 48, 720–725. [Google Scholar] [CrossRef] [Green Version]
- Gay, J.L.; Buchner, D.M.; Smith, J.; He, C. An Examination of Compensation Effects in Accelerometer-Measured Occupational and Non-Occupational Physical Activity. Prev. Med. Rep. 2017, 8, 55–59. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; De Craemer, M.; Lien, N.; Bernaards, C.; Buck, C.; Oppert, J.M.; Nazare, J.A.; Lakerveld, J.; O’Donoghue, G.; Holdsworth, M.; et al. The SOS-Framework (Systems of Sedentary Behaviours): An International Transdisciplinary Consensus Framework for the Study of Determinants, Research Priorities and Policy on Sedentary Behaviour across the Life Course: A DEDIPAC-Study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Donoghue, G.; Perchoux, C.; Mensah, K.; Lakerveld, J.; van Der Ploeg, H.; Bernaards, C.; Chastin, S.F.M.; Simon, C.; O’Gorman, D.; Nazare, J.A. A Systematic Review of Correlates of Sedentary Behaviour in Adults Aged 18-65 Years: A Socio-Ecological Approach. BMC Public Health 2016, 16, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutter, H.; Cavill, N.; Bauman, A.; Bull, F. Systems Approaches to Global and National Physical Activity Plans. Bull. World Health Organ. 2019, 97, 162. [Google Scholar] [CrossRef] [PubMed]
- Brakenridge, C.L.; Fjeldsoe, B.S.; Young, D.C.; Winkler, E.A.H.; Dunstan, D.W.; Straker, L.M.; Healy, G.N. Evaluating the Effectiveness of Organisational-Level Strategies with or without an Activity Tracker to Reduce Office Workers’ Sitting Time: A Cluster-Randomised Trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 115. [Google Scholar] [CrossRef] [Green Version]
- Carter, S.E.; Draijer, R.; Maxwell, J.D.; Morris, A.S.; Pedersen, S.J.; Graves, L.E.F.; Thijssen, D.H.J.; Hopkins, N.D. Using an E-Health Intervention to Reduce Prolonged Sitting in UK Office Workers: A Randomised Acceptability and Feasibility Study. Int. J. Env. Res. Public Health 2020, 17, 8942. [Google Scholar] [CrossRef]
- Home Office. Police Workforce, England and Wales: 30 September 2021. Available online: https://www.gov.uk/government/statistics/police-workforce-england-and-wales-30-september-2021/police-workforce-england-and-wales-30-september-2021 (accessed on 8 June 2022).
- Reilly, J.J.; Penpraze, V.; Hislop, J.; Davies, G.; Grant, S.; Paton, J.Y. Objective Measurement of Physical Activity and Sedentary Behaviour: Review with New Data. Arch. Dis. Child. 2008, 93, 614–619. [Google Scholar] [CrossRef]
- Krumpal, I. Determinants of Social Desirability Bias in Sensitive Surveys: A Literature Review. Qual. Quant. 2013, 47, 2025–2047. [Google Scholar] [CrossRef]
- Van Nassau, F.; Chau, J.Y.; Lakerveld, J.; Bauman, A.E.; van der Ploeg, H.P. Validity and Responsiveness of Four Measures of Occupational Sitting and Standing. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 144. [Google Scholar] [CrossRef] [Green Version]
| RE-AIM Dimension Guiding Question(s) | Data Type | Indicator | Measure |
|---|---|---|---|
| Reach Is the intervention reaching the target population? Those most in need? | Quantitative | Absolute number, proportion, and representativeness of eligible individuals who participate | Participation rate = #participating/#eligible Overall retention rate = #completed the study/#enrolled Demographic data frequencies and percentages Number (n) and percentage (%) of participants providing all and/or partial data |
| Qualitative | What explains variation in Reach, number of participants enrolled, and the dropout rate? Questions specific to A-REST: What were the motivations for participating in the intervention? | Semi-structured interviews with participants | |
| Effectiveness Does the intervention accomplish its goals? | Quantitative | Intervention effects on outcomes | Potential effects on sedentary behaviour, physical activity, health and wellbeing |
| Qualitative | What are the conditions and mechanisms that lead to effectiveness? What are the potential adverse side-effects? | Semi-structured interviews with participants | |
| Adoption To what extent are those targeted to deliver the intervention participating? | Quantitative | Number, percentage, and representativeness of participating settings and providers | Uptake = #departments participating/#invited |
| Qualitative | What affects provider participation? | Semi-structured interviews with participants | |
| Implementation To what extent was the intervention consistently implemented? | Quantitative | The extent to which the intervention was consistently implemented (and delivered as intended) | Device-measured sitting and activity #emails sent |
| Qualitative | What were the modifications to the intervention and why did they occur? What are the contextual factors and processes underlying alterations to implementation and how to address them? Questions specific to A-REST: Experience of: education session, team competition, Rise & Recharge® app, electronic prompts, other resources not suggested by the intervention, and weekly emails? | Semi-structured interviews with participants Descriptions of fidelity to protocol (actual versus intended) [58] | |
| Maintenance To what extent did the intervention become part of routine organisational practices and maintain effectiveness? | Quantitative | The extent to which a programme becomes part of routine organisational practices/policies and maintains effectiveness | Not assessed quantitatively |
| Qualitative | In what form are the components of the intervention or behaviour sustained? Questions specific to A-REST: How, and to what extent, do participants intend to maintain behaviour change? | Semi-structured interviews with participants Worksite board meeting report on sustainability |
| Characteristic | All Participants (n = 24) |
|---|---|
| Female, n (%) | 19 (79) |
| Age (years), M (SD) | 43 (11) |
| People from ethnic minority backgrounds, n (%) | 3 (13) |
| Body mass index (kg/m2), M (SD) | 27.6 (5.2) |
| Marriage status, n (%) | |
| Cohabiting | 4 (17) |
| Married or civil status | 13 (54) |
| Single | 7 (29) |
| Education, n (%) | |
| GCSE or equivalent | 9 (38) |
| Vocational qualifications | 2 (8) |
| A levels/Highers or equivalent | 7 (29) |
| Bachelor’s degree or equivalent | 5 (21) |
| Postgraduate qualifications | 1 (4) |
| Job role (manager), n (%) | 8 (33) |
| Years in service, M (SD) | 11.7 (10.8) |
| Hours worked per week, M (SD) | 38.2 (1.9) |
| Shift length (hours), M (SD) | 8.3 (1.4) |
| Self-rated heath, n (%) | |
| Fair | 5 (21) |
| Good | 13 (54) |
| Very good | 6 (25) |
| Tobacco use, n (%) | |
| Current smoker | 3 (13) |
| Previous smoker | 8 (33) |
| Smoked daily in the past | 7 (29) |
| Alcohol use score (AUDIT-C), M (SD) | |
| Women | 3.5 (1.7) |
| Men | 6.6 (1.3) |
| IPAQ weekly METs, M (SD) | 1457 (829) |
| Self-reported sitting time, M (SD) | |
| Weekdays (hours) | 15.5 (6.8) |
| Weekend (hours) | 12.8 (8) |
| Office size, n (%) | |
| Cell office (one person per room) | 2 (8) |
| Shared room (2–3 people per room) | 2 (8) |
| Small landscape (4–9 people per room) | 3 (13) |
| Medium-size landscape (10–24 people per room) | 7 (29) |
| Large-size landscape (24+ people per room) | 10 (42) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brierley, M.L.; Smith, L.R.; Chater, A.M.; Bailey, D.P. A-REST (Activity to Reduce Excessive Sitting Time): A Feasibility Trial to Reduce Prolonged Sitting in Police Staff. Int. J. Environ. Res. Public Health 2022, 19, 9186. https://doi.org/10.3390/ijerph19159186
Brierley ML, Smith LR, Chater AM, Bailey DP. A-REST (Activity to Reduce Excessive Sitting Time): A Feasibility Trial to Reduce Prolonged Sitting in Police Staff. International Journal of Environmental Research and Public Health. 2022; 19(15):9186. https://doi.org/10.3390/ijerph19159186
Chicago/Turabian StyleBrierley, Marsha L., Lindsey R. Smith, Angel M. Chater, and Daniel P. Bailey. 2022. "A-REST (Activity to Reduce Excessive Sitting Time): A Feasibility Trial to Reduce Prolonged Sitting in Police Staff" International Journal of Environmental Research and Public Health 19, no. 15: 9186. https://doi.org/10.3390/ijerph19159186
APA StyleBrierley, M. L., Smith, L. R., Chater, A. M., & Bailey, D. P. (2022). A-REST (Activity to Reduce Excessive Sitting Time): A Feasibility Trial to Reduce Prolonged Sitting in Police Staff. International Journal of Environmental Research and Public Health, 19(15), 9186. https://doi.org/10.3390/ijerph19159186