Endometrial Cancer in Pre-Menopausal Women and Younger: Risk Factors and Outcome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Instruments
2.2.1. Demographic Data and Clinical Assessment before a Diagnosis
2.2.2. Risk Factors for Endometrial Carcinoma
2.2.3. Histological Examination Finding
2.2.4. Primary Treatment
2.2.5. Outcome Post-Primary Treatment
2.3. Data Analysis
2.4. Ethical Consideration
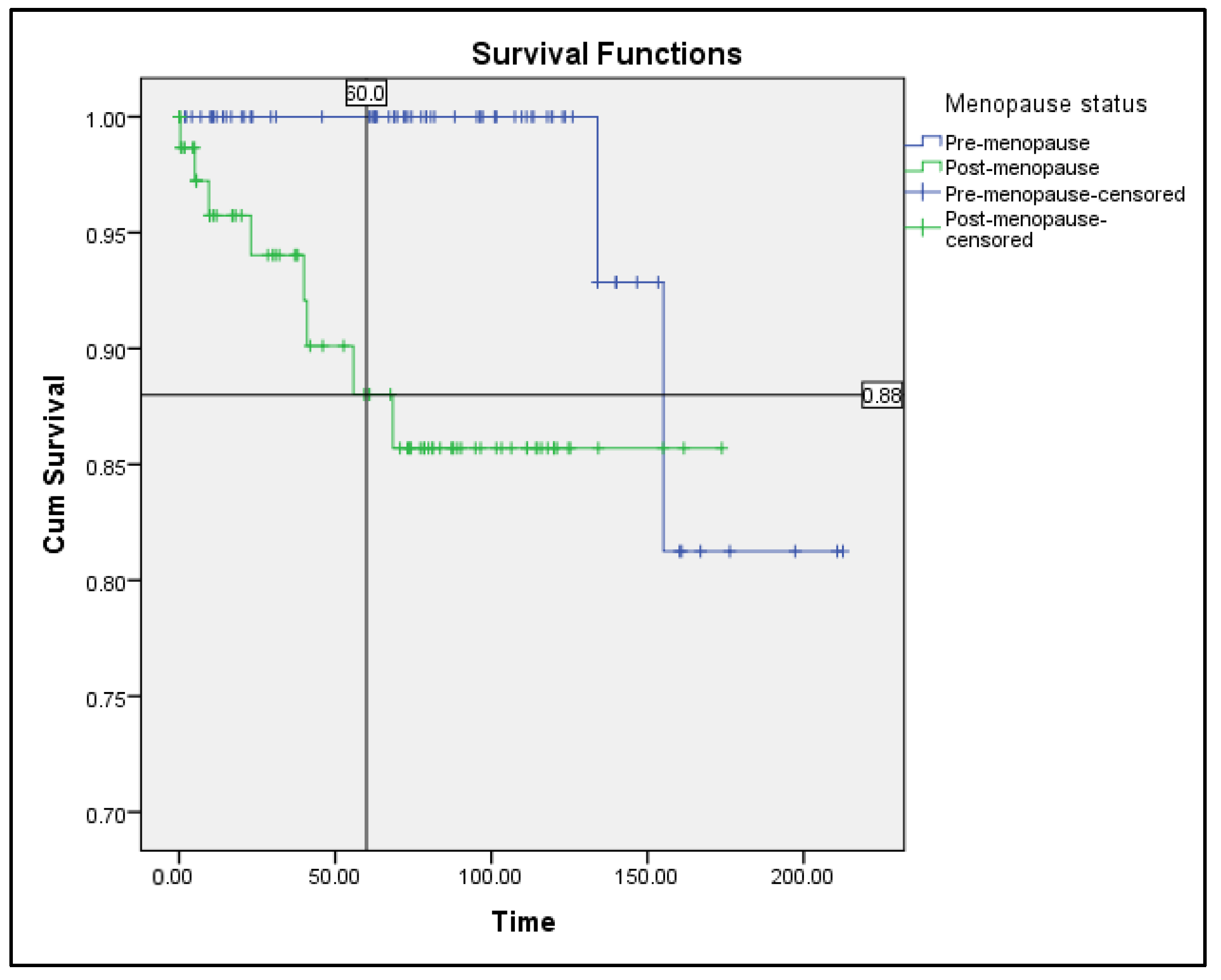
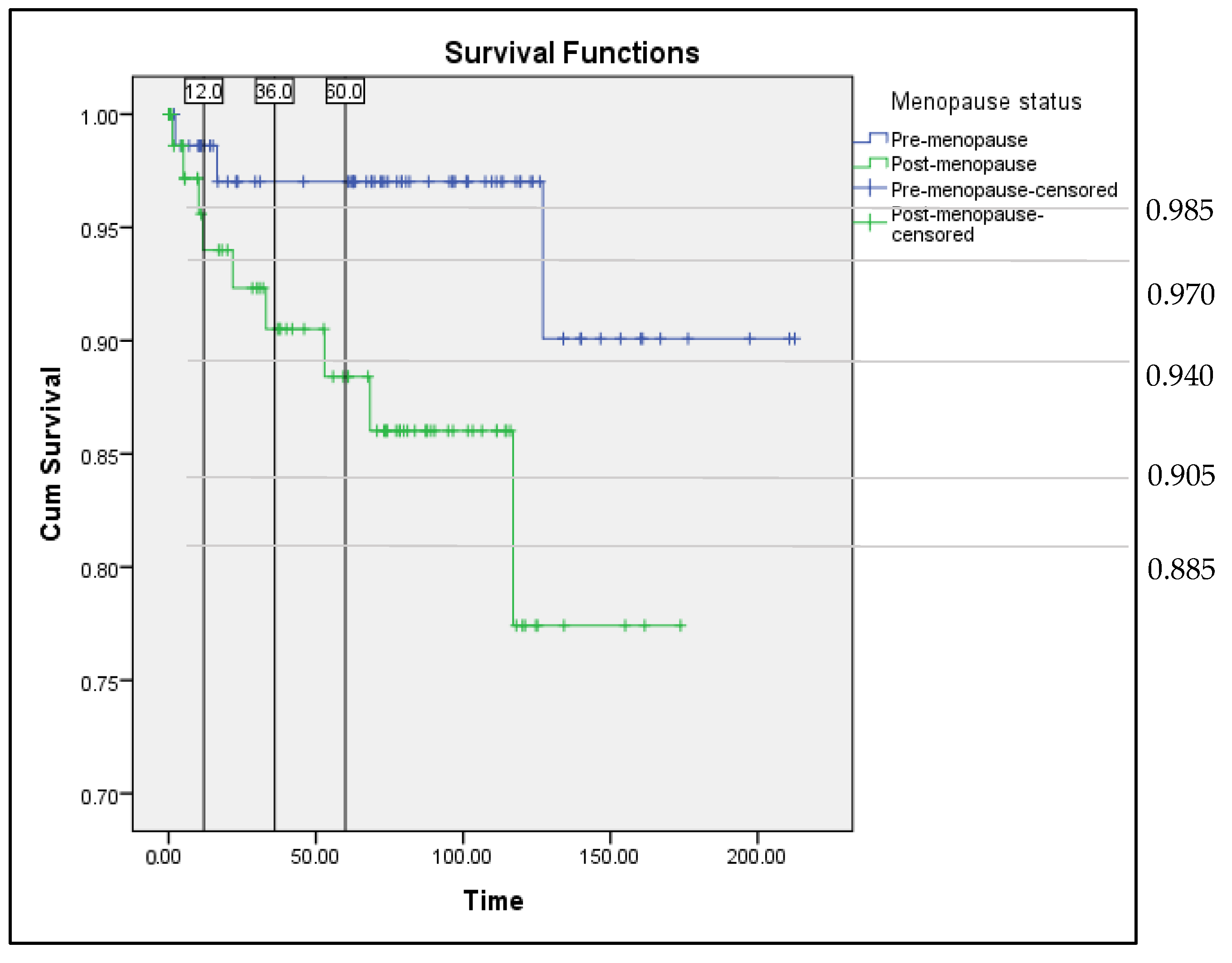
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ministry of Health. The Fifth Report of The National Cancer Registry—Malaysia National Cancer Registry Report (MNCR) 2012–2016; National Cancer Registry; Ministry of Health: Putrajaya, Malaysia, 2019. [Google Scholar]
- Ministry of Health. The Fourth Report of The National Cancer Registry—Malaysia National Cancer Registry Report (MNCR) 2007–2011; National Cancer Registry; Ministry of Health: Putrajaya, Malaysia, 2015. [Google Scholar]
- DiSaia, P.J.; Creasman, W.T. Clinical Gynecologic Oncology, 6th ed.; Mosby: St. Louis, MO, USA, 2002; pp. 137–171. [Google Scholar]
- Burleigh, A.; Talhouk, A.; Blake, H.C.; McAlpine, J.N. Clinical and pathological characterization of endometrial cancer in young women: Identification of a cohort without classical risk factors. Gynecol. Oncol. 2015, 138, 141–146. [Google Scholar] [CrossRef]
- Soliman, P.T.; Oh, J.C.; Schmeler, K.M.; Sun, C.C.; Slomovitz, B.M.; Gerhenson, D.M.; Burke, T.W.; Lu, K.H. Risk factors for young premenopausal women with endometrial cancer. Obstet. Gynecol. 2005, 105, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Pennant, M.E.; Mehta, R.; Moody, P.; Hackett, G.; Prentice, A.; Sharp, S.J.; Lakshman, R. Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG 2017, 124, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Asyikeen, W.A.; Siti-Azrin, A.H.; Che-Jalil, N.A.; Mat-Zin, A.A.; Othman, N.H. Median survival time of endometrial cancer patients with lymphovascular invasion at the Hospital Universiti Sains Malaysia. Malays. J. Med. Sci. 2016, 23, 44–51. [Google Scholar] [PubMed]
- Bharatnur, S.; Kustagi, P.; Krishnamohan, D. Endometrial carcinoma in a young woman: “30 is not immune”. J. Obstet. Gynaecol. India 2011, 61, 686–688. [Google Scholar] [CrossRef][Green Version]
- Biler, A.; Solmaz, U.; Erklinc, S.; Gokcu, M.; Bagci, M.; Temel, O.; Karadeniz, T.; Sanci, M. Analysis of endometrial carcinoma in young women at a high-volume cancer center. Int. J. Surg. 2017, 44, 185–190. [Google Scholar] [CrossRef]
- Ismael, N.N. A study on the menopause in Malaysia. Maturitas 1994, 19, 205–209. [Google Scholar] [CrossRef]
- Pellerin, G.P.; Finan, M.A. Endometrial cancer in women 45 years of age or younger: A clinicopathological analysis. Am. J. Obstet. Gynecol. 2005, 193, 1640–1644. [Google Scholar] [CrossRef]
- Yasumizu, T.; Ogawa, K.; Kato, J. Comparison of the clinicopathological characteristics of premenopausal and postmenopausal endometrial carcinomas: Analysis of endocrinologically evaluated cases”. Jpn. J. Clin. Oncol. 1996, 26, 152–156. [Google Scholar] [CrossRef][Green Version]
- Garg, K.; Soslow, R.A. Endometrial carcinoma in women aged 40 years and younger. Arch. Pathol. Lab. Med. 2014, 138, 335–342. [Google Scholar] [CrossRef]
- Anshika, A.; Rahul, M.; Jain, N.; Chithra, A.; Kausar, H. Endometrial carcinoma in young women: Management options and its review. Int. J. Reprod. Contr. Obstet. Gynecol. 2016, 5, 944–947. [Google Scholar]
- Laure, D.; Allen, N.; Kaaks, R.; Bakken, K.; Lund, E.; Tjonneland, A.; Olsen, A.; Overvad, K.; Clavel-Chapelon, F.; Fournier, A.; et al. Reproductive risk factors and endometrial cancer: The European prospective investigation into cancer and nutrition. Int. J. Cancer 2010, 127, 442–451. [Google Scholar]
- Maryam, G.A.; Delavar, M.A.; Moslemi, D.; Esmaeilzadeh, S. Risk factors for endometrial cancer: Results from a hospital-based case-control study. Asian Pac. J. Cancer Prev. 2016, 17, 4791–4796. [Google Scholar]
- Jie, Z.; Hu, Y.T.; Zhao, Y.; Chen, D.M.; Fang, T.F.; Ding, M. Risk factors of endometrial cancer in patients with endometrial hyperplasia: Implication for clinical treatments. BMC Womens Health 2021, 21, 312. [Google Scholar]
- Wu, Y.J.; Sun, W.J.; Liu, H.; Zhang, D.F. Age at menopause and risk of developing endometrial cancer: A meta-analysis. BioMed. Res. Int. 2019, 2019, 8584130. [Google Scholar] [CrossRef]
- Burbos, N.; Musonda, P.; Giarenis, I.; Shiner, A.M.; Giamougiannis, P.; Morris, E.P.; Nieto, J.J. Predicting the risk of endometrial cancer in postmenopausal women presenting with vaginal bleeding: The Norwich DEFAB risk assessment tool. Br. J. Cancer 2010, 102, 1201–1206. [Google Scholar] [CrossRef]
- Colombo, N.; Preti, E.; Landoni, F.; Carinelli, S.; Colombo, A.; Marini, C.; Sessa, C. Endometrial cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013, 24, vi33–vi38. [Google Scholar] [CrossRef]
- Singh, S.; Raidoo, S.; Pettigrew, G.; Debernardo, R. Management of early stage, high-risk endometrial carcinoma: Preoperative and surgical considerations. Obstet. Gynecol. Int. 2013, 2013, 757249. [Google Scholar] [CrossRef]
- Veena, P.; Amita, M. Diagnosis and pre-management workup of endometrial carcinoma. In Current Concepts in Endometrial Cancer; Springer: Singapore, 2017; pp. 41–53. [Google Scholar]
- Gao, Y.F.; Zhao, M.; Tong, M.; Wei, J.; Chen, Q. The prevalence of endometrial cancer in pre-and postmenopausal Chinese women. Menopause 2016, 23, 884–887. [Google Scholar] [CrossRef]
- Feinberg, J.; Albright, B.; Black, J.; Lu, L.G.; Passarelli, R.; Gysler, S.; Whicker, M.; Altwerger, G.; Menderes, G.; Hui, P.; et al. Ten-year comparison study of type 1 and 2 endometrial cancers: Risk factors and outcomes. Gynecol. Obstet. Investig. 2019, 84, 290–297. [Google Scholar] [CrossRef]
- Wan-Nor-Asyikeen, W.A.; Siti-Azrin, A.H.; Che-Jalil, N.A.; Othman, N.Y.; Mat-Zain, A.A. Endometrial cancer in Hospital Universiti Sains Malaysia. Asian Pac. J. Cancer Prev. 2016, 17, 2867–2870. [Google Scholar] [PubMed]
- Nout, R.A.; Smit, V.T.B.M.; Putter, H.; Jurgenliemk-Schulz, I.M.; Lutgens, L.C.H.W.; van der Steen-Banasik, E.M.; Mens, J.W.M.; Slot, A.; Kroese, M.C.S.; van Bunningen, B.N.F.M.; et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): An open-label, non-inferiority, randomised trial. Lancet 2010, 375, 816–823. [Google Scholar] [CrossRef]
- Kong, T.W.; Chang, S.J.; Paek, J.H.; Lee, Y.H.; Chun, M.S.; Ryu, H.S. Risk group criteria for tailoring adjuvant treatment in patients with endometrial cancer: A validation study of the gynecologic oncology group criteria. J. Gynecol. Oncol. 2015, 26, 32–39. [Google Scholar] [CrossRef] [PubMed]
- ASTEC/EN.5 Study Group.ASTEC. The Adjuvant external beam radiotherapy in the treatment of endometrial cancer (MRC ASTEC and NCIC CTG EN. 5 randomised trials): Pooled trial results, systematic review, and meta-analysis. Lancet 2009, 373, 137–146. [Google Scholar]
- Giustozzi, A.; Salutari, V.; Giudice, E.; Musacchio, L.; Ricci, C.; Landolfo, C.; Perri, M.T.; Scambia, G.; Lorusso, D. Refining adjuvant therapy for endometrial cancer: New standards and perspectives. Biology 2021, 10, 845. [Google Scholar] [CrossRef]
- Van den Heerik, A.S.V.M.; Horeweg, N.; Boer, S.M.D.; Bosse, T.; Creutzberg, C.L. Adjuvant therapy for endometrial cancer in the era of molecular classification: Radiotherapy, chemoradiation and novel targets for therapy. Int. J. Gynecol. Cancer 2021, 31, 594–604. [Google Scholar] [CrossRef]
- Kupets, R.; Le, T.; SOGC-GOC-SCC Policy and Practice Guideline Committee. The role of adjuvant therapy in endometrial cancer. J. Obstet. Gynaecol. Can. 2013, 35, 375–376. [Google Scholar] [CrossRef]
- Maggi, R.; Lissoni, A.; Spina, F.; Melpignano, P.; Zola, P.; Favalli, G.; Colombo, A.; Fossati, R. Adjuvant chemotherapy vs radiotherapy in high-risk endometrial carcinoma: Results of a randomised trial. Br. J. Cancer 2006, 95, 266–271. [Google Scholar] [CrossRef]
- Susumu, N.; Sagae, S.; Udagawa, Y.; Niwa, K.; Kuramoto, H.; Satoh, S.; Kudo, R. Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate-and high-risk endometrial cancer: A Japanese Gynecologic Oncology Group study. Gynecol. Oncol. 2008, 108, 226–233. [Google Scholar] [CrossRef]
- Hogberg, T.; Signorelli, M.; Oliverira, C.F.; Fossati, R.; Lissono, A.A.; Sorbe, B.; Andersson, H.; Grenman, S.; Lundgren, C.; Rosenberg, P.; et al. Sequential adjuvant chemotherapy and radiotherapy in endometrial cancer—Results from two randomised studies. Eur. J. Cancer 2010, 46, 2422–2431. [Google Scholar] [CrossRef] [PubMed]
| Premenopause Subgroup (126) | Postmenopause Subgroup (155) | p-Value | |
|---|---|---|---|
| Age at Diagnosis | 44.9 (7.5) | 62.3 (6.5) | <0.001 |
| Race | 0.622 | ||
| Malay | 89 (70.6%) | 99 (63.9%) | |
| Chinese | 26 (20.6%) | 38 (24.5%) | |
| Indian | 9 (7.1%) | 16 (10.3%) | |
| Others | 2 (1.6%) | 2 (1.3%) | |
| Presentation | 0.117 | ||
| Abnormal uterine bleeding | 114 (90.5%) | 144 (92.9%) | |
| Pelvic mass | 9 (7.1%) | 3 (1.9%) | |
| Abdominal pain | 1 (0.7%) | 2 (1.3%) | |
| Others | 2 (1.5%) | 5 (3.2%) | |
| Duration of symptom (week) | 12 (6–48) | 8 (4–28) | 0.003 |
| Duration to diagnose (week) | 3.7 (1.1–8.4) | 1.8 (0.5–6.0) | 0.003 |
| Endometrial thickness (mm) | 19.8 (10.8) | 18.7 (10.9) | 0.518 |
| BMI (kg/m2) | 30.8 (8.6) | 28.9 (7.1) | 0.040 |
| Age at menarche | 12.7 (1.5) | 13.3 (1.6) | 0.042 |
| Number of children | 1.47 (0–3) | 3.26 (1–5) | <0.001 |
| Nulliparity | 59 (46.8%) | 30 (19.4%) | <0.001 |
| Hypertension | 49 (38.9%) | 96 (61.9%) | <0.001 |
| Diabetes mellitus | 38 (30.2%) | 57 (36.8%) | 0.213 |
| Personal history of malignancy | 4 (3.2%) | 12 (7.8%) | 0.124 |
| Ovarian | 0 | 0 | |
| Breast | 3 (2.4%) | 8 (5.2%) | |
| Colorectal | 1 (0.8%) | 2 (1.3%) | |
| Others (Lymphoma) | 0 | 2 (1.3%) | |
| First-degree relative with malignancy | 17 (13.5%) | 28 (18.0%) | 0.299 |
| Endometrial | 4 (3.2%) | 9 (5.8%) | |
| Ovarian | 0 | 1 (0.6%) | |
| Breast | 10 (7.9%) | 14 (9.0%) | |
| Colorectal | 5 (3.9%) | 7 (4.5%) | |
| COCP user (all < 5 years) | 12 (9.5%) | 14 (9.0%) | NA |
| Smoking | 1 (0.8%) | 2 (1.3%) | NA |
| Tamoxifen | 0 | 6 (3.9%) | NA |
| HRT user | 0 | 3 (1.9%) | NA |
| Premenopause Subgroup (126) | Postmenopause Subgroup (155) | p-Value | ||
|---|---|---|---|---|
| Subtype | Endometrioid | 125 (99.2%) | 138 (89%) | 0.001 |
| Non-endometrioid | 1 (0.8%) | 17 (11%) | ||
| Clear cell | 1 (100%) | 5 (3.2%) | ||
| MMT | 0 | 4 (2.6%) | ||
| Serous | 0 | 3 (1.9%) | ||
| Others | 0 | 5 (3.3%) | ||
| Tumour grading | Well-differentiated | 66 (52.4%) | 47 (30.3%) | 0.001 |
| Moderately differentiated | 49 (38.9%) | 80 (51.6%) | ||
| Poorly differentiated | 6 (4.8%) | 13 (8.4%) | ||
| FIGO staging | Stage 1 | 90 (71.4%) | 113 (72.9%) | 0.470 |
| 1a | 45 (50%) | 48 (42.5%) | ||
| 1b | 45 (50%) | 65 (57.5%) | ||
| Advanced stage | 35 (27.8%) | 36 (23.2%) | ||
| Stage 2 | 18 (14.3%) | 18 (11.6%) | ||
| Stage 3 | 15 (11.9%) | 14 (9.0%) | ||
| Stage 4 | 2 (1.6%) | 4 (2.6%) | ||
| LVSI | Presence | 23 (18.3%) | 29 (18.7%) | 0.960 |
| Synchronous ovarian malignancy | Presence | 7 (5.6%) | 2 (1.3%) | 0.085 |
| Concomitant hyperplasia | Yes | 52 (41.3%) | 43 (27.7%) | 0.017 |
| No Adjuvant | Brachytherapy Alone | EBRT Alone | EBRT + Brachytherapy | CCRT | Chemotherapy Alone | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (50) | Recur n (%) | n (12) | Recur n (%) | n (1) | Recur n (%) | n (21) | Recur n (%) | n (0) | Recur n (%) | n (0) | Recur n (%) | ||
| LR | 34 | 1 (2.9) | 2 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 36 |
| LIR | 12 | 1 (8.3) | 3 | 0 (0) | 1 | 0 (0) | 14 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 30 |
| HIR | 4 | 0 (0) | 7 | 0 (0) | 0 | 0 (0) | 4 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 15 |
| HR | 0 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 3 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 3 |
| No Adjuvant | Brachytherapy Alone | EBRT Alone | EBRT + Brachytherapy | CCRT | Chemotherapy Alone | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (44) | Recur n (%) | n (28) | Recur n (%) | n (6) | Recur n (%) | n (29) | Recur n (%) | n (0) | Recur n (%) | n (3) | Recur n (%) | ||
| LR | 16 | 1 (6.3) | 1 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 0 | 0 (0) | 17 |
| LIR | 15 | 0 (0) | 12 | 0 (0) | 0 | 0 (0) | 6 | 2 (33.3) | 0 | 0 (0) | 0 | 0 (0) | 33 |
| HIR | 9 | 1 (11.1) | 12 | 0 (0) | 5 | 0 (0) | 18 | 2 (11.1) | 0 | 0 (0) | 0 | 0 (0) | 44 |
| HR | 4 | 1 (25) | 3 | 1 (33.3) | 1 | 0 (0) | 5 | 0 (0) | 0 | 0 (0) | 3 | 1 (33.3) | 16 |
| GOG Risk Type | Premenopausal (84) | Postmenopausal (110) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Recurrence (n (%)) | Total Cases (n) | Mean Survival Time (Month) | Log Rankp-Value | Recurrence (n (%)) | Total Cases (n) | Mean Survival Time (Month) | Log Rankp-Value | ||
| LR | No adjuvant | 1 (2.9) | 34 | 155.0 ± 5.8 | 0.758 | 1 (6.3) | 16 | 84.2 ± 4.7 | 0.796 |
| Brachytherapy | 0 | 2 | NA | 0 | 1 | NA | |||
| LIR/HIR | No adjuvant | 1 (6.2%) | 16 | 198.5 ± 13.5 | 0.188 | 1 (4.2) | 24 | 150.8 ± 10.3 | 0.716 |
| Adjuvant | 0 | 29 | NA | 4 (7.5) | 53 | 137.2 ± 9.0 | |||
| Brachy | 0 | 10 | 0 | 24 | |||||
| EBRT | 0 | 1 | 0 | 5 | |||||
| EBRT + Brachy | 0 | 18 | 4 | 24 | |||||
| HR | No adjuvant | 0 | 0 | NA | NA | 1 (25) | 4 | 67.4 ± 40.4 | 0.498 |
| Adjuvant | 0 | 3 | NA | 2 (16.7) | 12 | 138.9 ± 21.6 | |||
| Brachy | - | - | 1 | 3 | |||||
| EBRT | - | - | 0 | 1 | |||||
| EBRT + Brachy | 0 | 3 | 0 | 5 | |||||
| Chemotherapy | - | - | 1 | 3 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdol Manap, N.; Ng, B.K.; Phon, S.E.; Abdul Karim, A.K.; Lim, P.S.; Fadhil, M. Endometrial Cancer in Pre-Menopausal Women and Younger: Risk Factors and Outcome. Int. J. Environ. Res. Public Health 2022, 19, 9059. https://doi.org/10.3390/ijerph19159059
Abdol Manap N, Ng BK, Phon SE, Abdul Karim AK, Lim PS, Fadhil M. Endometrial Cancer in Pre-Menopausal Women and Younger: Risk Factors and Outcome. International Journal of Environmental Research and Public Health. 2022; 19(15):9059. https://doi.org/10.3390/ijerph19159059
Chicago/Turabian StyleAbdol Manap, Nurliza, Beng Kwang Ng, Su Ee Phon, Abdul Kadir Abdul Karim, Pei Shan Lim, and Maimunah Fadhil. 2022. "Endometrial Cancer in Pre-Menopausal Women and Younger: Risk Factors and Outcome" International Journal of Environmental Research and Public Health 19, no. 15: 9059. https://doi.org/10.3390/ijerph19159059
APA StyleAbdol Manap, N., Ng, B. K., Phon, S. E., Abdul Karim, A. K., Lim, P. S., & Fadhil, M. (2022). Endometrial Cancer in Pre-Menopausal Women and Younger: Risk Factors and Outcome. International Journal of Environmental Research and Public Health, 19(15), 9059. https://doi.org/10.3390/ijerph19159059






