Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists
Abstract
1. Introduction
Purpose of the Study
- ○
- To explore occupational therapists’ perspectives on clients’ conditions and factors, splint types, and rationale for splinting selection and practice.
- ○
- To find the experience of expert occupational therapists in the nature of clinical instructors determining their clinical reasoning ability and skill in splinting practice.
2. Materials and Methods
2.1. Survey Procedure
2.2. Survey Participants and Recruitment
2.3. Interview Procedure
2.4. Interview Participants and Recruitment
2.5. Data Collection Procedure
2.6. Data Analysis
2.7. Rigor and Trustworthiness
3. Results
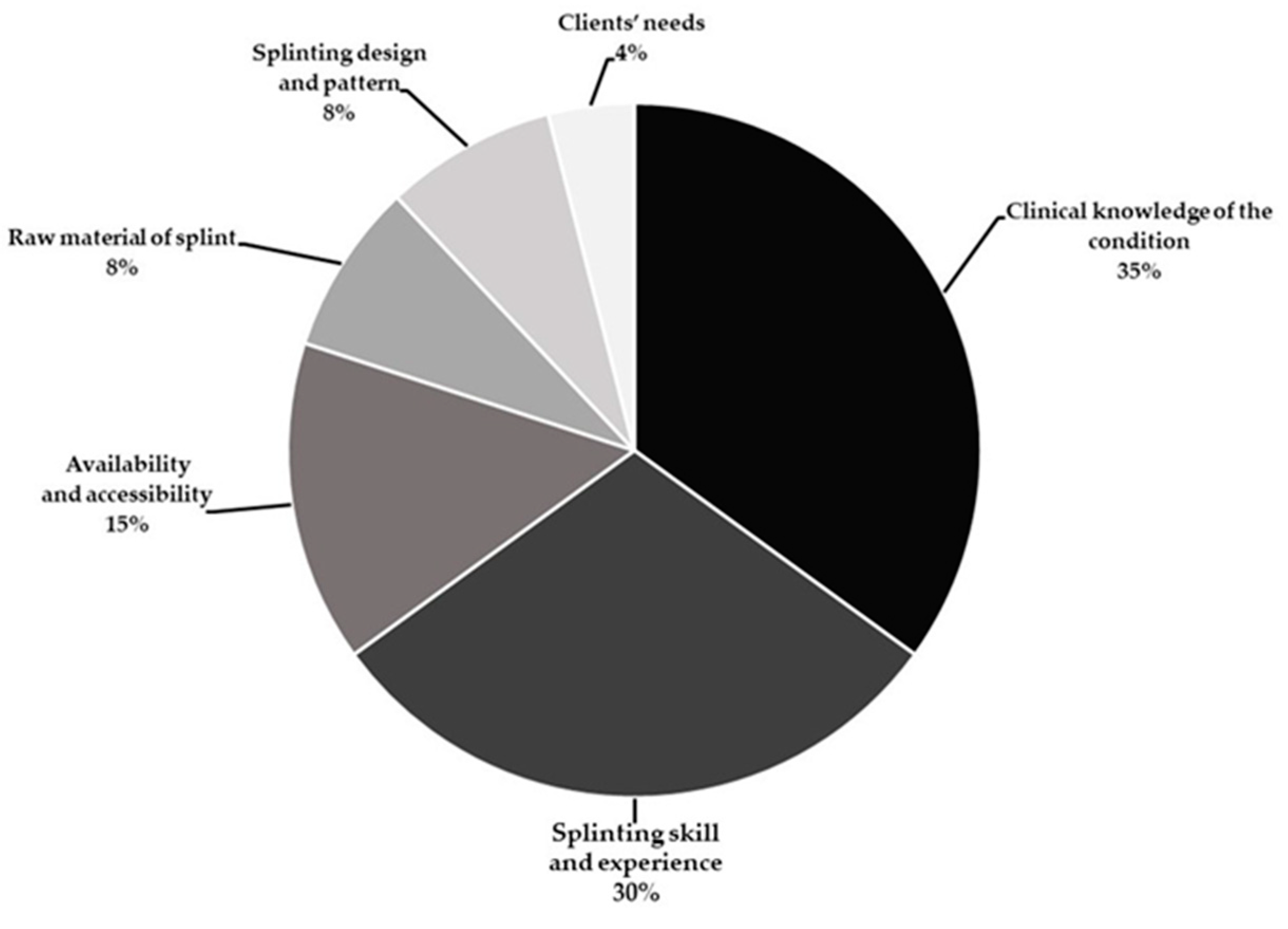
3.1. Survey Outcomes
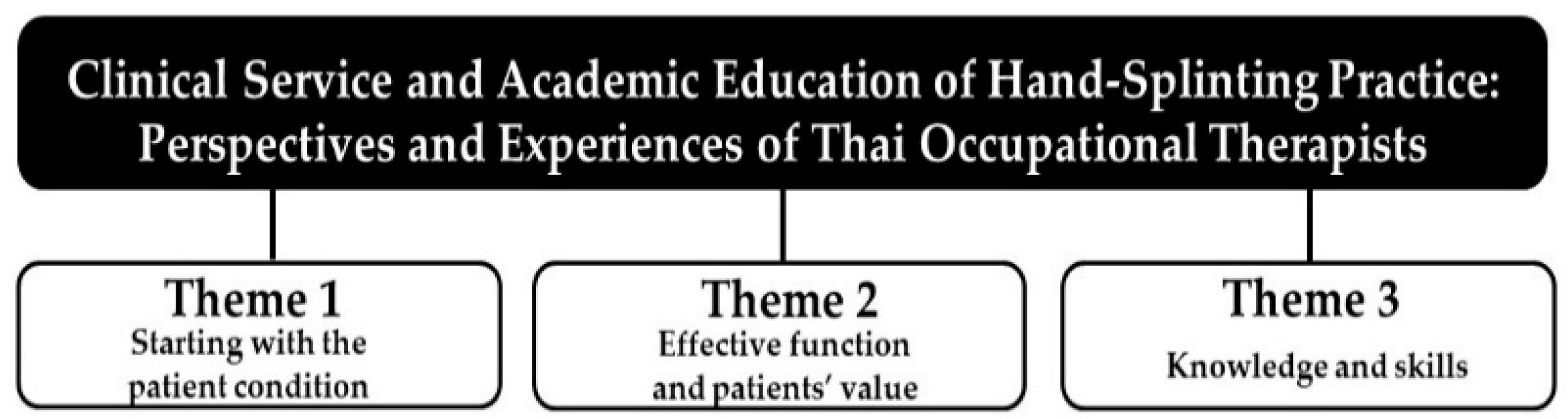
3.2. Qualitative Findings
- Theme 1. Starting with the patients’ condition
“In general, the physician treats a patient based on diagnosis and condition. After a patient recovers, the physician considers consulting occupational therapists for making a splint. So, I need to know a patient’s condition and prognosis of each case. Sometimes, I have found a broken bone and needed to make an evaluation to select a splint type to fit each case.”
“I think that client condition is key to selecting types of splints, and it can help to predict the outcomes after the use of splints. The management of condition needs a specific splint with appropriate duration and time for recovery. Moreover, I need to evaluate current conditions in readiness to use splints. So, I provide splinting for a client through treatment planning and intervention, including maintenance.”
“I found that my patients have sensory problems, especially sensory loss that can affect splint therapy. In those cases, I don’t use splinting for them because the pressure from the splint will affect their bone and skin. It is quite dangerous…it is quite dangerous to hurt them.”
“We think that [it is] just the general knowledge of health providers that we need to find the relevant and effective interventions to match a patient’s condition. We need to consider the types of splints and raw materials to fit a patient. It will help to fix bone alignment and reduce patient deformities.”
- Theme 2. Effective function and patients’ value
“I thoroughly inform my patients regarding what is involved in splint therapy. For example, in one case, a patient wanted to wear an antispastic splint to reduce spasms and pain. He also told me that he needed to wear the splint only at night. In my clinical opinion, I thought that it would not be effective to reduce spasticity and improve hand function when the patient wears a splint and needs to go to sleep. However, I created a splint for him since he actually works at his home during the nighttime.”
“The orthopedic physician then consulted the occupational therapists to make a static splint to prevent ulnar deviation. When the client wore this kind of splint, he felt good, but he could not bend his fingers. He complained that he could not do anything and that the splint negatively affected his abilities to perform everyday activities. I considered his problem and changed his current splint to a dynamic splint. My client was happy because he could perform activities that he wanted.”
“I treat both mature and pediatric patients. The biggest problem is providing splint therapy for children. I have to understand that children are not the same as adults; they have different needs and levels of understanding at different ages. A good way to approach children is to talk to them about their favorite cartoon characters by using stickers that can be stuck on splints or using a vivid splint pattern. Sometimes, I initiated splinting with the child by playing with toys.”
- Theme 3. Knowledge and experiential skills
“I believe that we basically need to understand a patient’s condition. This includes understanding cause and effect relationships as well as preventive measures. As occupational therapists, we need to be confident in gathering a patient’s information in order to select the types of splints that fit a patient’s condition. Overall, we create the pattern and deal with a patient to match the affected hand with the appropriate splint. Moreover, we need to check up on splinting mechanisms and their functions and evaluate a patient’s satisfaction including giving information about splint maintenance.”
“At the beginning, I gained experience in splinting design from senior occupational therapists and by servicing patients. When I intervened with the patients more often, I repeated splinting every day. Therefore, I became more familiar with their situation and also more confident about making sure that I can do it better for my patients. Moreover, I actually learned from the lessons that try to draw and design the pattern on paper before fabricating then splinting sheet.”
“Fifteen years ago, I was nervous when I served my patients in splinting therapy. When I intervened with patients, I had doubts and uncertainty, and did not know whether there would be good outcomes or not. Nevertheless, I did not quit, and kept going forward to improve myself as a therapist. I opened the door to learn from splinting workshops and repeatedly practiced at my clinic over and over again. Now, I have the experience of how to deal with patients who want to be served with splinting. It takes time, but you can make progress.”
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process (4th Edition). Am. J. Occup. Ther. 2020, 74 (Suppl. S2), 7412410010p1–7412410010p87. [Google Scholar]
- Bennett, S.; Rodger, S.; Fitzgerald, C.; Gibson, L.; Sylvia, R.; Gibson, E. Simulation in Occupational Therapy Curricula: A literature review. Aust. Occup. Ther. J. 2017, 64, 314–327. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Beyer, E.; Carter, K. Interprofessional simulation education designed to teach occupational therapy and nursing students complex patient transfers. J. Interprof. Educ. Pract. 2017, 6, 67–70. [Google Scholar] [CrossRef]
- Office of the Higher Education Commission. Thai Qualifications Framework for Higher Education; B.E. 2552; Office of the Higher Education Commission: Bangkok, Thailand, 2009.
- Ministry of Public Health. Professional Standards for the Art of Healing in Occupational Therapy; Ministry of Public Health: Nonthaburi, Thailand, 2011.
- World Federation of Occupational Therapists. Statement Regarding the WFOT Minimum Standards for the Education of Occupational Therapists (Revised 2016) Related to COVID-19 Pandemic. Available online: https://www.wfot.org/resources/covid-19-and-wfot-minimum-education-standards-statement (accessed on 9 March 2022).
- Koski, K.J.; Simon, R.L.; Dooley, N.R. Valuable occupational therapy fieldwork educator behaviors. Work 2013, 44, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Dancza, K.; Warren, A.; Copley, J.; Rodger, S.; Moran, M.; McKay, E.; Taylor, A. Learning experiences on role-emerging placements: An exploration from the students’ perspective. Aust. Occup. Ther. J. 2013, 60, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Tiffen, J.; Corbridge, S.J.; Slimmer, L. Enhancing Clinical Decision Making: Development of a Contiguous Definition and Conceptual Framework. J. Prof. Nurs. 2014, 30, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Simmons, B. Clinical reasoning: Concept analysis. J. Adv. Nurs. 2010, 66, 1151–1158. [Google Scholar] [CrossRef]
- Young, M.; Thomas, A.; Lubarsky, S.; Ballard, T.; Gordon, D.; Gruppen, L.D.; Holmboe, E.; Ratcliffe, T.; Rencic, J.; Schuwirth, L.; et al. Drawing Boundaries: The Difficulty in Defining Clinical Reasoning. Acad. Med. 2018, 93, 990–995. [Google Scholar] [CrossRef]
- Bruggen, H.V. European Network of Occupational Therapy in Higher Education: A five-year review. Occup. Ther. Int. 2001, 8, 132–138. [Google Scholar] [CrossRef]
- Hills, C.; Ryan, S.; Smith, D.R.; Warren-Forward, H. The impact of ‘Generation Y’ occupational therapy students on practice education. Aust. Occup. Ther. J. 2012, 59, 156–163. [Google Scholar] [CrossRef]
- Kondo, T. Cultural Tensions in Occupational Therapy Practice: Considerations from a Japanese Vantage Point. Am. J. Occup. Ther. 2004, 58, 174–184. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johnson, O.C.B. The Impact of ASEAN University Network-Quality Assurance (AUN-QA) Assessment on the Quality of Educational Programmes; Springer: Singapore, 2017. [Google Scholar]
- Spady, W.G. Outcome-Based Education: Critical Issues and Answers; ERIC, 1994. Available online: https://eric.ed.gov/?id=ED380910 (accessed on 9 March 2022).
- Kilbride, C.; Hoffman, K.; Baird, T.; Tuckey, J.; Marston, L.; De Souza, L. Contemporary splinting practice in the UK for adults with neurological dysfunction: A cross-sectional survey. Int. J. Ther. Rehabil. 2013, 20, 559–566. [Google Scholar] [CrossRef][Green Version]
- Boscheinen-Morrin, J.; Conolly, W.B. The Hand: Fundamentals of Therapy, 3rd ed.; Butterworth-Heinemann: Oxford, UK, 2001. [Google Scholar]
- Burns, M.C.; Neumeister, M.W. Orthoses for Overuse Disorders, 4th ed.; MOSBY ELSEVIER: Springfield, IL, USA, 1906. [Google Scholar]
- Kingston, G.A.; Williams, G.; Judd, J.; Gray, M.A. Hand therapy services for rural and remote residents: Results of a survey of Australian occupational therapists and physiotherapists. Aust. J. Rural. Health 2015, 23, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Frye, S.K.; Geigle, P.R. Current U.S. splinting practices for individuals with cervical spinal cord injury. Spinal Cord Ser. Cases 2020, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kumnerddee, W.; Kaewtong, A. Efficacy of acupuncture versus night splinting for carpal tunnel syndrome: A randomized clinical trial. J. Med. Assoc. Thai. 2010, 93, 1463–1469. [Google Scholar] [PubMed]
- Bunyachatakul, S.; Trivittaya, P.; Munkhetvit, P. Effect of low-cost, low-profile dynamic splint on hand function in persons with radial nerve injury. J. Occup. Ther. Assoc. Thail. 2016, 21, 1–13. [Google Scholar]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; SAGE Publications: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Rovinelli, R.J.; Hambleton, R.K. On the use of content specialists in the assessment of criterion-referenced test item validity. Dutch J. Educ. Res. 1977, 2, 49–60. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Twinn, D.S. An analysis of the effectiveness of focus groups as a method of qualitative data collection with Chinese populations in nursing research. J. Adv. Nurs. 1998, 28, 654–661. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice; Sage publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Varagona, L.M.; Hold, J.L. Nursing students’ perceptions of faculty trustworthiness: Thematic analysis of a longitudinal study. Nurse Educ. Today 2018, 72, 27–31. [Google Scholar] [CrossRef]
- Hepworth, L.M.; Govender, P.; Rencken, G. Current trends in splinting the hand in children with neurological impairments. S. Afr. J. Occup. Ther. 2017, 47, 9–15. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Marinaro, C.; Moggio, L.; Pino, I.; Barletta, M.; Petraroli, A.; Ammendolia, A. Comparative Effectiveness of Orthoses for Thumb Osteoarthritis: A Systematic Review and Network Meta-analysis. Arch. Phys. Med. Rehabil 2021, 102, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Suphanchaimat, R.; Sornsrivichai, V.; Limwattananon, S.; Thammawijaya, P. Economic development and road traffic injuries and fatalities in Thailand: An application of spatial panel data analysis, 2012–2016. BMC Public Health 2019, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Chazen, L.-A.; Franzsen, D. Expert opinion on splinting adult patients with neurological injuries. S. Afr. J. Occup. Ther. 2016, 46, 4–9. [Google Scholar] [CrossRef]

| Workplace/Splinting Practice Experience | 2–5 Years | 6–10 Years | 11–15 Years | 16–20 Years | >20 Years | Total |
|---|---|---|---|---|---|---|
| Hospital A | 3 | - | - | 2 | 1 | 6 |
| Hospital B | - | 1 | - | 1 | 1 | 3 |
| Hospital C | 3 | 3 | 1 | - | 1 | 8 |
| Hospital D | 1 | 1 | - | - | 1 | 3 |
| Hospital E | 2 | - | 1 | 1 | - | 4 |
| Hospital F | 1 | - | 1 | 1 | - | 3 |
| Hospital G | 3 | - | - | - | - | 3 |
| Total | 13 | 5 | 3 | 5 | 4 | 30 |
| Participant | Sex | Age | Years of Experience in Splinting | Clinical Field | Clinical Setting |
|---|---|---|---|---|---|
| Somying | Female | 44 | 18 | Physical dysfunction & community | Public hospital |
| Sompong | Male | 40 | 16 | Physical dysfunctions | Private hospital |
| Somsri | Female | 48 | 24 | Physical and pediatrics | Public hospital |
| Somsak | Male | 40 | 17 | Physical and pediatrics | Public hospital |
| Somchai | Male | 47 | 24 | Physical dysfunction | Public hospital |
| Somyod | Male | 49 | 25 | Physical dysfunction | Private hospital |
| Somruidee | Female | 38 | 15 | Physical and elderly | Public hospital |
| Sompon | Female | 45 | 21 | Physical dysfunction | Public hospital |
| Type of Splint | Used (n) | Used (%) | Never Used (n) | Never Used (%) |
|---|---|---|---|---|
| Functional Resting * | 30 | 100 | 0 | 0 |
| Cock-up ** | 28 | 93.3 | 2 | 6.7 |
| Thumb spica *** | 24 | 80 | 6 | 20 |
| Finger *** | 24 | 80 | 6 | 20 |
| De Quervain’s | 15 | 50 | 15 | 15 |
| Anti-spastic | 14 | 46.6 | 16 | 53.4 |
| Dynamic | 9 | 30 | 21 | 70 |
| Supination | 1 | 3.3 | 29 | 96.7 |
| Weight-bearing | 1 | 3.3 | 29 | 96.7 |
| Client Factors in Splinting Practice | Very Frequently (%) | Frequently (%) | Occasionally (%) | Rarely (%) | Never (%) |
|---|---|---|---|---|---|
| Prevention of bone and joint deformities | 43 | 53 | 4 | - | - |
| Prevention of muscle contracture | 40 | 46 | 7 | 7 | - |
| Maintaining/increasing range of motion | 33 | 53 | 14 | - | - |
| Reducing muscle tone | 27 | 50 | 13 | 3 | 7 |
| Improving hand function and prehension | 10 | 47 | 20 | 17 | 6 |
| Patients’ needs | 7 | 13 | 20 | 47 | 13 |
| Pain relief | 6 | 13 | 41 | 27 | 13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaunnil, A.; Sansri, V.; Thongchoomsin, S.; Permpoonputtana, K.; Stanley, M.; Trevittaya, P.; Thawisuk, C.; Thichanpiang, P. Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists. Int. J. Environ. Res. Public Health 2022, 19, 8995. https://doi.org/10.3390/ijerph19158995
Kaunnil A, Sansri V, Thongchoomsin S, Permpoonputtana K, Stanley M, Trevittaya P, Thawisuk C, Thichanpiang P. Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists. International Journal of Environmental Research and Public Health. 2022; 19(15):8995. https://doi.org/10.3390/ijerph19158995
Chicago/Turabian StyleKaunnil, Anuchart, Veerawat Sansri, Surachart Thongchoomsin, Kannika Permpoonputtana, Mandy Stanley, Piyawat Trevittaya, Chirathip Thawisuk, and Peeradech Thichanpiang. 2022. "Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists" International Journal of Environmental Research and Public Health 19, no. 15: 8995. https://doi.org/10.3390/ijerph19158995
APA StyleKaunnil, A., Sansri, V., Thongchoomsin, S., Permpoonputtana, K., Stanley, M., Trevittaya, P., Thawisuk, C., & Thichanpiang, P. (2022). Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists. International Journal of Environmental Research and Public Health, 19(15), 8995. https://doi.org/10.3390/ijerph19158995







