Latent Class Analysis of Polysubstance Use and Sexual Risk Behaviors among Men Who Have Sex with Men Attending Sexual Health Clinics in Mexico City
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Measures
2.2.1. Demographic Characteristics
2.2.2. Cigarette Smoking
2.2.3. Alcohol Use and Binge Drinking
2.2.4. Drug Use
2.2.5. Sexual Behavior
2.3. Data Analysis
3. Results
3.1. Descriptive Statistics of the Study Population
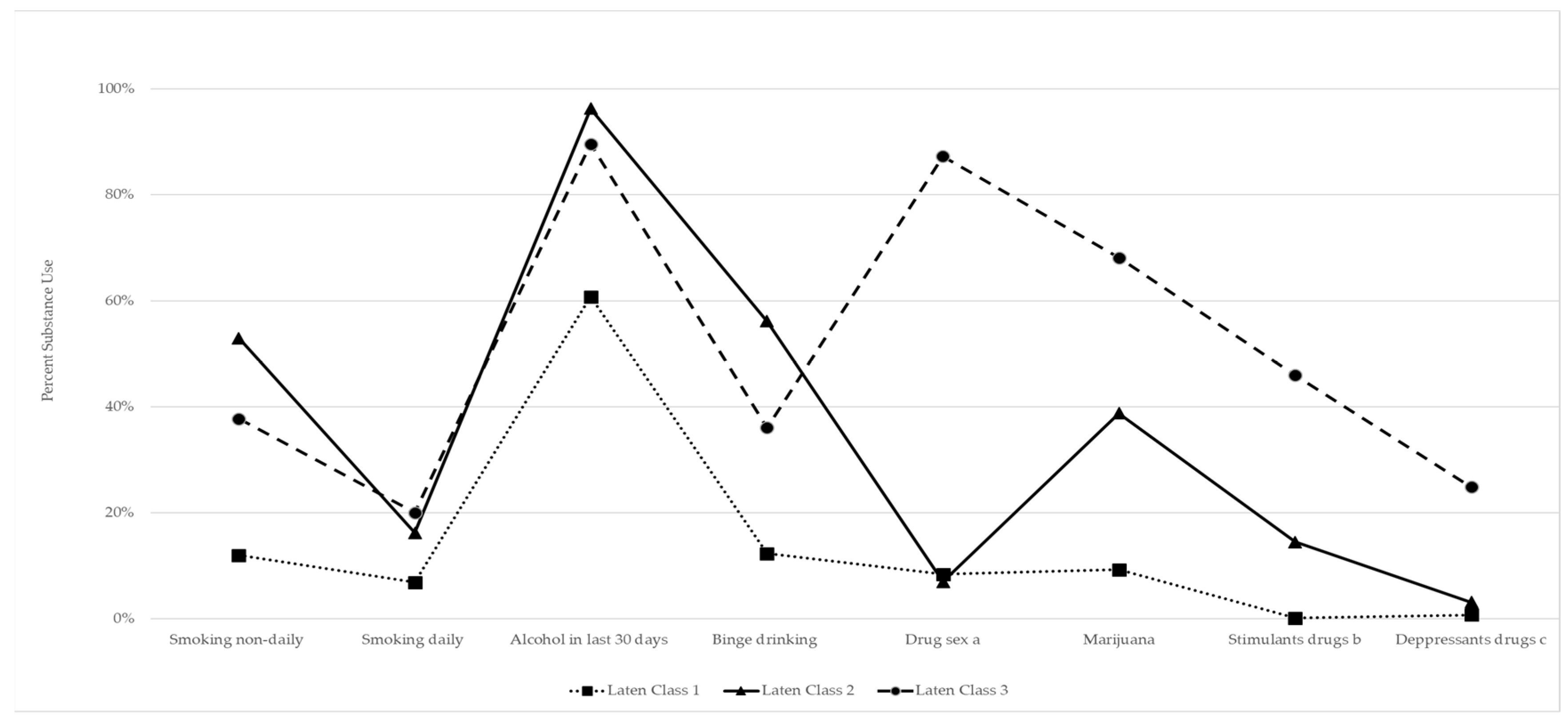
3.2. Latent Class Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- UNAIDS. Fact Sheet-Latest Global and Regional Statistics on the Status of the AIDS Epidemic; UNAIDS: Geneva, Switzerland, 2020. [Google Scholar]
- PAHO. Plan of Action for the Prevention and Control of HIV and Sexually Transmitted Infections 2016–2021; Pan American Health Organization: Washington, DC, USA, 2016. [Google Scholar]
- Censida, Secretaria de Salud. Día Mundial del Sida. Country Mexico. 2017. Available online: https://www.gob.mx/cms/uploads/attachment/file/275582/Boletin_D_aMundial2017.pdf (accessed on 11 July 2022).
- Espolea, Interculturalidad Salud y Derechos AC. Encuesta sobre uso de drogas en poblacion LGBT en Mexico. 2015. Available online: https://idpc.net/es/publications/2015/10/reporte-de-resultados-de-la-encuesta-sobre-uso-de-drogas-en-poblacion-lgbtien-mexico-2015 (accessed on 11 July 2022).
- Schuler, M.S.; Stein, B.D.; Collins, R.L. Differences in Substance Use Disparities Across Age Groups in a National Cross-Sectional Survey of Lesbian, Gay, and Bisexual Adults. LGBT Health 2019, 6, 68–76. [Google Scholar] [CrossRef] [PubMed]
- D’Avanzo, P.A.; Halkitis, P.N.; Yu, K.; Kapadia, F. Demographic, Mental Health, Behavioral, and Psychosocial Factors Associated with Cigarette Smoking Status among Young Men Who Have Sex with Men: The P18 Cohort Study. LGBT Health 2016, 3, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Newcomb, M.E.; Ryan, D.T.; Greene, G.J.; Garofalo, R.; Mustanski, B. Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug Alcohol Depend. 2014, 141, 65–71. [Google Scholar] [CrossRef] [PubMed]
- PAHO. Regional Status Report on Alcohol and Health and Health 2020; Pan American Health Organization: Washington, DC, USA, 2020. [Google Scholar]
- Bourey, C.; Stephenson, R.; Bautista-Arredondo, S. Syndemic Vulnerability and Condomless Sex among Incarcerated Men in Mexico City: A Latent Class Analysis. AIDS Behav. 2018, 22, 4019–4033. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.; Khanna, A.S.; Skaathun, B.; Michaels, S.; Young, L.; Duvoisin, R.; Chang, M.; Voisin, D.; Cornwell, B.; Coombs, R.W.; et al. Marijuana Use among Young Black Men Who Have Sex with Men and the HIV Care Continuum: Findings from the uConnect Cohort. Subst. Use Misuse 2016, 51, 1751–1759. [Google Scholar] [CrossRef]
- Drumright, L.; Gorbach, P.M.; Little, S.J.; Strathdee, S. Associations Between Substance Use, Erectile Dysfunction Medication and Recent HIV Infection among Men Who have Sex with Men. AIDS Behav. 2009, 13, 328–336. [Google Scholar] [CrossRef]
- Drumright, L.N.; Little, S.J.; Strathdee, S.A.; Slymen, D.J.; Araneta, M.R.G.; Malcarne, V.L.; Daar, E.S.; Gorbach, P.M. Unprotected Anal Intercourse and Substance Use among Men Who Have Sex with Men with Recent HIV Infection. JAIDS J. Acquir. Immune Defic. Syndr. 2006, 43, 344–350. [Google Scholar] [CrossRef]
- McCarty-Caplan, D.; Jantz, I.; Swartz, J. MSM and Drug Use: A Latent Class Analysis of Drug Use and Related Sexual Risk Behaviors. AIDS Behav. 2014, 18, 1339–1351. [Google Scholar] [CrossRef]
- Ostrow, D.G.; Plankey, M.W.; Cox, C.; Li, X.; Shoptaw, S.; Jacobson, L.P.; Stall, R.C. Specific Sex Drug Combinations Contribute to the Majority of Recent HIV Seroconversions among MSM in the MACS. JAIDS J. Acquir. Immune Defic. Syndr. 2009, 51, 349–355. [Google Scholar] [CrossRef]
- Bourne, A.; Weatherburn, P. Substance use among men who have sex with men: Patterns, motivations, impacts and intervention development need. Sex. Transm. Infect. 2017, 93, 342–346. [Google Scholar] [CrossRef]
- Daskalopoulou, M.; Rodger, A.; Phillips, A.N.; Sherr, L.; Speakman, A.; Collins, S.; Elford, J.; Johnson, M.A.; Gilson, R.; Fisher, M.; et al. Recreational drug use, polydrug use, and sexual behaviour in HIV-diagnosed men who have sex with men in the UK: Results from the cross-sectional ASTRA study. Lancet HIV 2014, 1, e22–e31. [Google Scholar] [CrossRef]
- Marshall, B.D.L.; Wood, E.; Shoveller, J.A.; Patterson, T.L.; Montaner, J.S.G.; Kerr, T. Pathways to HIV risk and vulnerability among lesbian, gay, bisexual, and transgendered methamphetamine users: A multi-cohort gender-based analysis. BMC Public Health 2011, 11, 20. [Google Scholar] [CrossRef] [PubMed]
- Pappas, M.K.; Halkitis, P.N. Sexual risk taking and club drug use across three age cohorts of HIV-positive gay and bisexual men in New York City. AIDS Care 2011, 23, 1410–1416. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Vallabhaneni, S.; Raymond, H.F.; McFarland, W. Predictors of Serosorting and Intention to Serosort among Men Who Have Sex with Men, San Francisco. AIDS Educ. Prev. 2012, 24, 564–573. [Google Scholar] [CrossRef] [PubMed]
- Mexican National Statistics Institute (INEGI). Population Census; INEGI: Mexico City, Mexico, 2015; Available online: https://www.inegi.org.mx/temas/estructura/ (accessed on 11 July 2022).
- Consejo Nacional para Prevenir la Discriminación. Encuesta Nacional Contra la Discriminación. 2017. Available online: http://sindis.conapred.org.mx/estadisticas/enadis/ (accessed on 11 July 2022).
- Achterbergh, R.C.A.; de Vries, H.J.C.; Boyd, A.; Davidovich, U.; Drückler, S.; Hoornenborg, E.; Prins, M.; Matser, A. Identification and characterization of latent classes based on drug use among men who have sex with men at risk of sexually transmitted infections in Amsterdam, the Netherlands. Addiction 2020, 115, 121–133. [Google Scholar] [CrossRef]
- Tobin, K.E.; Yang, C.; King, K.; Latkin, C.A.; Curriero, F.C. Associations Between Drug and Alcohol Use Patterns and Sexual Risk in a Sample of African American Men Who Have Sex with Men. AIDS Behav. 2016, 20, 590–599. [Google Scholar] [CrossRef]
- Achterbergh, R.; Drückler, S.; van Rooijen, M.; van Aar, F.; Slurink, I.; de Vries, H.; Boyd, A. Sex, drugs, and sexually transmitted infections: A latent class analysis among men who have sex with men in Amsterdam and surrounding urban regions, the Netherlands. Drug Alcohol Depend. 2020, 206, 107526. [Google Scholar] [CrossRef]
- Card, K.G.; Lachowsky, N.J.; Cui, Z.; Carter, A.; Armstrong, H.; Shurgold, S.; Moore, D.; Hogg, R.S.; Roth, E.A. A Latent Class Analysis of Seroadaptation among Gay and Bisexual Men. Arch. Sex. Behav. 2018, 47, 95–106. [Google Scholar] [CrossRef]
- Lim, S.H.; Cheung, D.H.; Guadamuz, T.E.; Wei, C.; Koe, S.; Altice, F. Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug Alcohol Depend. 2015, 151, 31–37. [Google Scholar] [CrossRef]
- Dangerfield, D.T.; Carmack, C.C.; Gilreath, T.D.; Duncan, D.T. Latent Classes of Sexual Positioning Practices and Sexual Risk among Men Who Have Sex with Men in Paris, France. AIDS Behav. 2018, 22, 4001–4008. [Google Scholar] [CrossRef]
- Lazcano-Ponce, E.; Salmerón, J.; González, A.; Allen-Leigh, B.; León-Maldonado, L.; Magis-Rodriguez, C.; Aranda-Flores, C.; Conde-González, C.; Romero, A.J.P.; Yunes-Díaz, E.; et al. Prevention and control of neoplasms associated with HPV in high-risk groups in Mexico City: The Condesa Study. Salud Publica Mex. 2018, 60, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Reséndiz Escobar, E.; Bustos Gamino, M.N.; Mujica Salazar, R.; Soto Hernández, I.S.; Cañas Martínez, V.; Fleiz Bautista, C.; Villatoro Velázquez, J.A. National trends in alcohol consumption in Mexico: Results of the National Survey on Drug, Alcohol and Tobacco Consumption 2016–2017. Salud Ment. 2018, 41, 7–16. [Google Scholar] [CrossRef]
- Suarez, T. Negotiating risks in context: A perspective on unprotected anal intercourse and barebacking among men who have sex with men-where do we go from here? Arch. Sex. Behav. 2001, 30, 287–300. [Google Scholar] [CrossRef]
- Suarez, T.P.; Kelly, J.A.; Pinkerton, S.D.; Stevenson, Y.L.; Hayat, M.; Smith, M.D.; Ertl, T. Influence of a partner’s HIV serostatus, use of highly active antiretroviral therapy, and viral load on perceptions of sexual risk behavior in a community sample of men who have sex with men. J. Acquir. Immune Defic. Syndr. 2001, 28, 471–477. [Google Scholar] [CrossRef]
- McCutcheon, A.L. Basic concepts and procedures in single and multiple-group latent class analysis. In Applied Latent Class Models; Hagenaars, J., McCutcheon, A., Eds.; Cambridge University Press: Cambridge, UK, 2002; pp. 89–95. [Google Scholar]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Stata Statistical Software, Release 16; StataCorp LP: College Station, TX, USA, 2017.
- Feinstein, B.A.; Newcomb, M.E. Event-Level Associations among Drinking Motives, Alcohol Consumption, and Condomless Anal Sex in a Sample of Young Men Who Have Sex with Men. AIDS Behav. 2017, 21, 1904–1913. [Google Scholar] [CrossRef]
- Przybyla, S.M.; Krawiec, G.; Godleski, S.A.; Crane, C.A. Meta-Analysis of Alcohol and Serodiscordant Condomless Sex among People Living with HIV. Arch. Sex. Behav. 2018, 47, 1351–1366. [Google Scholar] [CrossRef]
- NIAAA. Alcohol Alert Alcohol and HIV/AIDS: Intertwining Stories. Available online: https://pubs.niaaa.nih.gov/publications/AA80/AA80.pdf (accessed on 11 July 2022).
- Vosburgh, H.W.; Mansergh, G.; Sullivan, P.; Purcell, D. A Review of the Literature on Event-Level Substance Use and Sexual Risk Behavior among Men Who Have Sex with Men. AIDS Behav. 2012, 16, 1394–1410. [Google Scholar] [CrossRef]
- Wray, T.B.; Celio, M.A.; Pérez, A.E.; DiGuiseppi, G.T.; Carr, D.J.; Woods, L.A.; Monti, P.M. Causal Effects of Alcohol Intoxication on Sexual Risk Intentions and Condom Negotiation Skills among High-Risk Men Who Have Sex with Men (MSM). AIDS Behav. 2018, 23, 161–174. [Google Scholar] [CrossRef]
- Chan, P.A.; Rose, J.; Maher, J.; Benben, S.; Pfeiffer, K.; Almonte, A.; Poceta, J.; Oldenburg, C.E.; Parker, S.; Marshall, B.D.; et al. A Latent Class Analysis of Risk Factors for Acquiring HIV among Men Who Have Sex with Men: Implications for Implementing Pre-Exposure Prophylaxis Programs. AIDS Patient Care STDs 2015, 11, 597–605. [Google Scholar] [CrossRef]
- Card, K.G.; Lachowsky, N.J.; Armstrong, H.L.; Cui, Z.; Wang, L.; Sereda, P.; Jollimore, J.; Patterson, T.L.; Corneil, T.; Hogg, R.S.; et al. The additive effects of depressive symptoms and polysubstance use on HIV risk among gay, bisexual, and other men who have sex with men. Addict. Behav. 2018, 82, 158–165. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco use and Prevention Policies; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Conde Gutiérrez Del Álamo, F.; Santoro Domingo, P. Tipología, valores y preferencias de las personas con VIH e imaginarios de la infección: Resultados de un estudio cualitativo. Rev. Esp. Salud Publica 2012, 86, 139–152. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jacques Aviñó, C.; García de Olalla, P.; Díez, E.; Martín, S.; Caylà, J.A. Explicaciones de las prácticas sexuales de riesgo en hombres que tienen sexo con hombres. Gac. Sanit. 2015, 4, 252–257. [Google Scholar] [CrossRef]
- Berg, R.C. Barebacking: A Review of the Literature. Arch. Sex. Behav. 2009, 38, 754–764. [Google Scholar] [CrossRef] [PubMed]
- Halkitis, P.N. Behavioral Patterns, Identity, and Health Characteristics of Self-Identified Barebackers: Implications for HIV Prevention and Intervention. J. LGBT Health Res. 2007, 3, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Infante, C.; Cuadra-Hernández, S.M.; Baruch-Domínguez, R.; Granados-Cosme, J.A. “Dame una pastilla”: Los significados del VIH/sida en la práctica del bareback en la ciudad de México e implicaciones para la prevención. Salud Publica Mex. 2015, 57, 113–118. [Google Scholar] [CrossRef]
- Baruch-Dominguez, R. El Uso de Cristal-Meth, ¿Una Crisis de Salud Pública en México? 2021. Available online: https://www.animalpolitico.com/blog-invitado/el-uso-de-cristal-meth-una-crisis-de-salud-publica-en-mexico/ (accessed on 11 July 2022).
- Baruch-Dominguez, R.; Cuadra-Hernández, S.M. Los productos biomédicos para la prevención del VIH: Un cambio de paradigma limitado por condiciones sociales y políticas. In Perspectivas Multidimensionales del VIH. Primera; Robles-Aguirre., B.A., Granados-Cosme, J.A., Eds.; Universidad Autónoma Metropolitana: Ciudad de México, Mexico, 2020; pp. 55–68. [Google Scholar]
- González Portillo, A.; Robles Soto, N. Guía Breve Para la Implementación del Enfoque de Reducción de Riesgos y Daños Con Usuarios de Drogas; Secretaría de Salud: Cuidad de México, México, 2020. [Google Scholar]
- Comisión Nacional de los Derechos Humanos en México. Programa Especial de Sexualidad, Salud y VIH. Available online: https://www.cndh.org.mx/programa/36/programa-especial-de-sexualidad-salud-y-vih (accessed on 11 July 2022).
| Model | df | AIC | BIC |
|---|---|---|---|
| One class | 8 | 13,543.42 | 13,587.21 |
| Two classes | 25 | 12,735.85 | 12,872.71 |
| Three classes | 42 | 12,569.68 | 12,799.60 |
| Four classes | 59 | 12,526.34 | 12,849.31 |
| Characteristics | n | % |
|---|---|---|
| Age in Years | (M = 29.1, SD = 7.37) | (Range = 15–59) |
| 18–22 | 561 | 30.3 |
| 23–28 | 446 | 24.1 |
| 29–33 | 392 | 21.2 |
| 34 or more | 451 | 24.4 |
| Marital status | ||
| Single | 1480 | 80.0 |
| Married/common-law | 366 | 19.8 |
| Missing | 4 | 0.2 |
| Educational attainment | ||
| High school graduates | 545 | 29.9 |
| Four-year college graduates | 677 | 37.1 |
| Completed postgraduate studies | 604 | 33.1 |
| HIV status | ||
| Negative | 1054 | 57.0 |
| Positive | 751 | 40.6 |
| Unknown | 45 | 2.4 |
| Condomless anal sex (CAS) | ||
| No | 810 | 44.1 |
| Yes | 1028 | 55.9 |
| Serosorting | ||
| No | 1592 | 86.5 |
| Yes | 248 | 13.5 |
| Smoking pattern (last 30 days) | ||
| Non-smoker | 1068 | 57.7 |
| Non-daily | 541 | 29.2 |
| Daily | 234 | 12.6 |
| Missing | 7 | 0.4 |
| Alcohol use (last 30 days) | ||
| No | 428 | 23.1 |
| Yes | 1410 | 76.2 |
| Missing | 12 | 0.6 |
| Binge drinking (last 30 days) | ||
| No | 1245 | 67.3 |
| Yes | 541 | 29.2 |
| Missing | 64 | 3.5 |
| Drug use (last 3 months) a | ||
| No | 803 | 43.4 |
| Yes | 1021 | 55.2 |
| Missing | 26 | 1.4 |
| Sex-drugs b | 434 | 23.9 |
| Marijuana | 544 | 29.4 |
| Stimulants c | 249 | 13.7 |
| Depressants d | 114 | 6.3 |
| Class 1–Reference | Class 2 | Class 3 | ||
|---|---|---|---|---|
| aOR | CI 95% | aOR | CI 95% | |
| Age in Years | ||||
| 18–22 | 1.00 | 1.00 | ||
| 23–28 | 1.36 | (0.90–2.05) | 1.86 * | (1.16–3.00) |
| 29–33 | 0.95 | (0.59–1.52) | 1.86 * | (1.14–3.03) |
| 34 or more | 0.48 * | (0.29–0.80) | 1.54 | (0.95–2.47) |
| Marital status | ||||
| Single | 1.00 | 1.00 | ||
| Married/common-law | 0.86 | (0.56–1.29) | 0.79 | (0.53–1.16) |
| Educational attainment | ||||
| High school graduates | 1.00 | 1.00 | ||
| Four-year college graduates | 1.15 | (0.77–1.71) | 1.22 | (0.80–1.86) |
| Completed postgraduate studies | 0.67 | (0.43–1.06) | 1.60 * | (1.05–2.43) |
| HIV status | ||||
| Negative | 1.00 | 1.00 | ||
| Positive | 0.82 | (0.5–1.15) | 1.26 | (0.90–1.75) |
| Condomless anal sex (CAS) | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.28 | (0.89–1.84) | 2.92 ** | (1.30–3.12) |
| Serosorting | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.09 | (0.62–1.89) | 2.02 ** | (2.02–4.22) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Bolaños, R.; Baruch-Dominguez, R.; Arillo-Santillán, E.; Yunes-Díaz, E.; Rivera-Rivera, L.; Cruz-Jiménez, L.; Thrasher, J.F.; Nyitray, A.G.; Lazcano-Ponce, E. Latent Class Analysis of Polysubstance Use and Sexual Risk Behaviors among Men Who Have Sex with Men Attending Sexual Health Clinics in Mexico City. Int. J. Environ. Res. Public Health 2022, 19, 8847. https://doi.org/10.3390/ijerph19148847
Rodríguez-Bolaños R, Baruch-Dominguez R, Arillo-Santillán E, Yunes-Díaz E, Rivera-Rivera L, Cruz-Jiménez L, Thrasher JF, Nyitray AG, Lazcano-Ponce E. Latent Class Analysis of Polysubstance Use and Sexual Risk Behaviors among Men Who Have Sex with Men Attending Sexual Health Clinics in Mexico City. International Journal of Environmental Research and Public Health. 2022; 19(14):8847. https://doi.org/10.3390/ijerph19148847
Chicago/Turabian StyleRodríguez-Bolaños, Rosibel, Ricardo Baruch-Dominguez, Edna Arillo-Santillán, Elsa Yunes-Díaz, Leonor Rivera-Rivera, Lizeth Cruz-Jiménez, James F. Thrasher, Alan G. Nyitray, and Eduardo Lazcano-Ponce. 2022. "Latent Class Analysis of Polysubstance Use and Sexual Risk Behaviors among Men Who Have Sex with Men Attending Sexual Health Clinics in Mexico City" International Journal of Environmental Research and Public Health 19, no. 14: 8847. https://doi.org/10.3390/ijerph19148847
APA StyleRodríguez-Bolaños, R., Baruch-Dominguez, R., Arillo-Santillán, E., Yunes-Díaz, E., Rivera-Rivera, L., Cruz-Jiménez, L., Thrasher, J. F., Nyitray, A. G., & Lazcano-Ponce, E. (2022). Latent Class Analysis of Polysubstance Use and Sexual Risk Behaviors among Men Who Have Sex with Men Attending Sexual Health Clinics in Mexico City. International Journal of Environmental Research and Public Health, 19(14), 8847. https://doi.org/10.3390/ijerph19148847






