Counseling for Physical Activity in Adults during the COVID-19 Pandemic: A Scope Review
Abstract
:1. Introduction
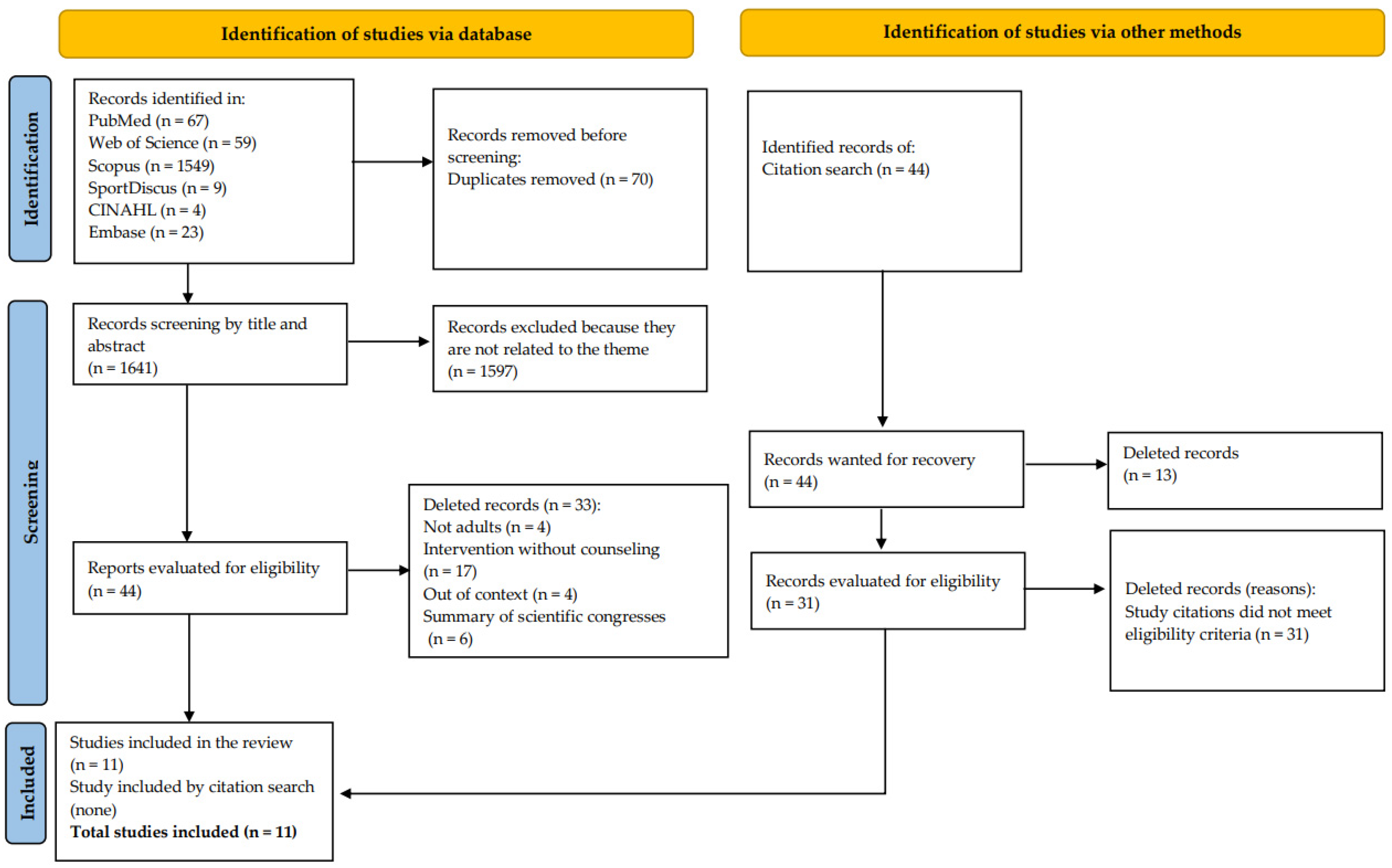
2. Methods
2.1. Study Eligibility Criteria
2.2. Selection of Evidence Sources
2.3. Search Strategies
2.4. Risk of Bias Assessment
3. Results
3.1. Characteristics of Records
3.2. General Sample and Population Characteristics
3.3. Characteristics of PA Counseling during the COVID-19 Pandemic
3.4. Risk of Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- O’Connor, E.A.; Evans, C.V.; Rushkin, M.C.; Redmond, N.; Lin, J.S. Behavioral Counseling Interventions to Promote a Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults with Cardiovascular Risk Factors: Updated Systematic Review for the U.S. Preventive Services Task Force; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2020.
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Lear, S.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The Effect of Physical Activity on Mortality and Cardiovascular Disease in 130,000 People from 17 High-Income, Middle-Income, and Low-Income Countries: The PURE Study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Samitz, G.; Egger, M.; Zwahlen, M. Domains of Physical Activity and All-Cause Mortality: Systematic Review and Dose-Response Meta-Analysis of Cohort Studies. Int. J. Epidemiol. 2011, 40, 1382–1400. [Google Scholar] [CrossRef] [Green Version]
- Kyu, H.H.; Bachman, V.F.; Alexander, L.T.; Mumford, J.E.; Afshin, A.; Estep, K.; Veerman, J.L.; Delwiche, K.; Iannarone, M.L.; Moyer, M.L.; et al. Physical Activity and Risk of Breast Cancer, Colon Cancer, Diabetes, Ischemic Heart Disease, and Ischemic Stroke Events: Systematic Review and Dose-Response Meta-Analysis for the Global Burden of Disease Study 2013. BMJ 2016, 354, i3857. [Google Scholar] [CrossRef] [Green Version]
- Silva, D.A.S.; Tremblay, M.S.; Souza, M.d.F.M.d.; Mooney, M.; Naghavi, M.; Malta, D.C. Mortality and Years of Life Lost by Colorectal Cancer Attributable to Physical Inactivity in Brazil (1990–2015): Findings from the Global Burden of Disease Study. PLoS ONE 2018, 13, e0190943. [Google Scholar] [CrossRef] [Green Version]
- Silva, D.A.S.; Tremblay, M.S.; Souza, M.d.F.M.d.; Guerra, M.R.; Mooney, M.; Naghavi, M.; Malta, D.C. Mortality and Years of Life Lost Due to Breast Cancer Attributable to Physical Inactivity in the Brazilian Female Population (1990–2015). Sci. Rep. 2018, 8, 11141. [Google Scholar] [CrossRef]
- Burtscher, J.; Millet, G.P.; Burtscher, M. Low Cardiorespiratory and Mitochondrial Fitness as Risk Factors in Viral Infections: Implications for COVID-19. Br. J. Sports Med. 2021, 55, 413–415. [Google Scholar] [CrossRef]
- Nieman, D.C.; Wentz, L.M. The Compelling Link between Physical Activity and the Body’s Defense System. J. Sport Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical Inactivity Is Associated with a Higher Risk for Severe COVID-19 Outcomes: A Study in 48,440 Adult Patients. Br. J. Sports Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef]
- Marconcin, P.; Werneck, A.O.; Peralta, M.; Ihle, A.; Gouveia, É.R.; Ferrari, G.; Sarmento, H.; Marques, A. The Association between Physical Activity and Mental Health during the First Year of the COVID-19 Pandemic: A Systematic Review. BMC Public Health 2022, 22, 209. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide Trends in Insufficient Physical Activity from 2001 to 2016: A Pooled Analysis of 358 Population-Based Surveys with 1·9 Million Participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [Green Version]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global Physical Activity Levels: Surveillance Progress, Pitfalls, and Prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, B.; Gan, L.; Ke, L.; Fu, Y.; Di, Q.; Ma, X. Effects of Online Bodyweight High-Intensity Interval Training Intervention and Health Education on the Mental Health and Cognition of Sedentary Young Females. Int. J. Environ. Res. Public Health 2021, 18, 302. [Google Scholar] [CrossRef]
- Burtscher, J.; Burtscher, M.; Millet, G.P. (Indoor) Isolation, Stress, and Physical Inactivity: Vicious Circles Accelerated by COVID-19? Scand. J. Med. Sci. Sports 2020, 30, 1544–1545. [Google Scholar] [CrossRef]
- García Pérez de Sevilla, G.; Barceló Guido, O.; De la Cruz, M.d.l.P.; Blanco Fernández, A.; Alejo, L.B.; Montero Martínez, M.; Pérez-Ruiz, M. Adherence to a Lifestyle Exercise and Nutrition Intervention in University Employees during the COVID-19 Pandemic: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 7510. [Google Scholar] [CrossRef]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A Tale of Two Pandemics: How Will COVID-19 and Global Trends in Physical Inactivity and Sedentary Behavior Affect One Another? Prog. Cardiovasc. Dis. 2021, 64, 108–110. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Sciomer, S.; Cocchi, C.; Maffei, S.; Gallina, S. Quarantine during COVID-19 Outbreak: Changes in Diet and Physical Activity Increase the Risk of Cardiovascular Disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1409–1417. [Google Scholar] [CrossRef]
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B.; Coca, A. Physical Activity Change during COVID-19 Confinement. Int. J. Environ. Resh. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in Physical Activity and Sedentary Behaviours from before to during the COVID-19 Pandemic Lockdown: A Systematic Review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Dwyer, M.J.; Pasini, M.; De Dominicis, S.; Righi, E. Physical Activity: Benefits and Challenges during the COVID-19 Pandemic. Scand. J. Med. Sci. Sports 2020, 30, 1291–1294. [Google Scholar] [CrossRef]
- McKeon, G.; Tiedemann, A.; Sherrington, C.; Teasdale, S.; Mastrogiovanni, C.; Wells, R.; Steel, Z.; Rosenbaum, S. Feasibility of an Online, Mental Health-Informed Lifestyle Program for People Aged 60+ Years during the COVID-19 Pandemic. Health Promot. J. Austr. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, A.R.; Abdallah, F.; Faulkner, G.; Ciliska, D.; Hicks, A. Factors Contributing to the Effectiveness of Physical Activity Counselling in Primary Care: A Realist Systematic Review. Patient Educ. Couns. 2015, 98, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Moraes, S.d.Q.; de Souza, J.H.; de Araújo, P.A.B.; Rech, C.R. Prevalence of physical activity counseling in Primary Health Care: A systematic review. Rev. Bras. Ativ. Fís. Saúde 2019, 24, 1–12. [Google Scholar] [CrossRef]
- Florindo, A.A.; Andrade, D.R. Experiences of Promoting Physical Activity in the Family Health Strategy; SBAFS: Florianópolis, Brazil, 2015. [Google Scholar]
- Artinian, N.T.; Fletcher, G.F.; Mozaffarian, D.; Kris-Etherton, P.; Van Horn, L.; Lichtenstein, A.H.; Kumanyika, S.; Kraus, W.E.; Fleg, J.L.; Redeker, N.S.; et al. Interventions to Promote Physical Activity and Dietary Lifestyle Changes for Cardiovascular Risk Factor Reduction in Adults: A Scientific Statement from the American Heart Association. Circulation 2010, 122, 406–441. [Google Scholar] [CrossRef] [PubMed]
- de Souza Neto, J.M.; de Brito, G.E.G.; Loch, M.R.; da Silva, S.S.; da Costa, F.F. Counseling for physical activity in primary health care: An integrative review. Movimento 2021, 26, e26075. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Peters, M.D.J.; Marnie, C.; Colquhoun, H.; Garritty, C.M.; Hempel, S.; Horsley, T.; Langlois, E.V.; Lillie, E.; O’Brien, K.K.; Tunçalp, Ö.; et al. Scoping Reviews: Reinforcing and Advancing the Methodology and Application. Syst. Rev. 2021, 10, 263. [Google Scholar] [CrossRef]
- NHLBI. Study Quality Assessment Tools; NHLBI: Bethesda, MD, USA, 2014.
- Egan, K.J.; Hodgson, W.; Dunlop, M.D.; Imperatore, G.; Kirk, A.; Maguire, R. A Novel Mobile App (“CareFit”) to Support Informal Caregivers to Undertake Regular Physical Activity From Home During and Beyond COVID-19 Restrictions: Co-Design and Prototype Development Study. JMIR Form. Res. 2021, 5, e27358. [Google Scholar] [CrossRef]
- van de Wiel, H.J.; Stuiver, M.M.; May, A.M.; van Grinsven, S.; Aaronson, N.K.; Oldenburg, H.S.A.; van der Poel, H.G.; Koole, S.N.; Retèl, V.P.; van Harten, W.H.; et al. Effects of and Lessons Learned from an Internet-Based Physical Activity Support Program (with and without Physiotherapist Telephone Counselling) on Physical Activity Levels of Breast and Prostate Cancer Survivors: The PABLO Randomized Controlled Trial. Cancers 2021, 13, 3665. [Google Scholar] [CrossRef]
- Johnson, N.; Bradley, A.; Klawitter, L.; Johnson, J.; Johnson, L.; Tomkinson, G.R.; Hackney, K.J.; Stastny, S.; Ehlers, D.K.; McGrath, R. The Impact of a Telehealth Intervention on Activity Profiles in Older Adults during the COVID-19 Pandemic: A Pilot Study. Geriatrics 2021, 6, 68. [Google Scholar] [CrossRef]
- Robertson, M.C.; Cox-Martin, E.; Liao, Y.; Flores, S.A.; Shegog, R.; Markham, C.M.; Fujimoto, K.; Durand, C.P.; Brewster, A.; Lyons, E.J.; et al. Acceptance- and Mindfulness-Based Techniques for Physical Activity Promotion in Breast Cancer Survivors: A Qualitative Study. Support Care Cancer 2022, 30, 465–473. [Google Scholar] [CrossRef] [PubMed]
- McDonough, D.J.; Helgeson, M.A.; Liu, W.; Gao, Z. Effects of a Remote, YouTube-Delivered Exercise Intervention on Young Adults’ Physical Activity, Sedentary Behavior, and Sleep during the COVID-19 Pandemic: Randomized Controlled Trial. J. Sport Health Sci. 2021, 11, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-L.; Huang, L.-C.; Chang, Y.-T.; Chen, R.-Y.; Yang, S.-H. Under COVID-19 Pandemic: A Quasi-Experimental Trial of Observation on Diabetes Patients’ Health Behavior Affected by the Pandemic From a Coaching Intervention Program. Front. Public Health 2021, 9, 577. [Google Scholar] [CrossRef] [PubMed]
- Jiwani, R.; Dennis, B.; Bess, C.; Monk, S.; Meyer, K.; Wang, J.; Espinoza, S. Assessing Acceptability and Patient Experience of a Behavioral Lifestyle Intervention Using Fitbit Technology in Older Adults to Manage Type 2 Diabetes amid COVID-19 Pandemic: A Focus Group Study. Geriatr. Nurs. 2021, 42, 57–64. [Google Scholar] [CrossRef]
- Sciamanna, C.N.; Ladwig, M.A.; Conroy, D.E.; Schmitz, K.H.; Silvis, M.L.; Ballentine, N.H.; Auer, B.J.; Danilovich, M.K. Feasibility and Impact of a 1-Minute Daily Functional Exercise Regimen Prescribed to Older Adults by Their Primary Care Physician. Prev. Med. Rep. 2021, 21, 101307. [Google Scholar] [CrossRef]
- Brazil National Health Council Resolution. No. 218, of 6 March 1997; Recognizes Social Workers, Biologists, Physical Education Professionals, Nurses, Pharmacists, Physiotherapists, Speech-Language Pathologists, Physicians, Veterinarians, Nutritionists, Psychologists and Occupational Therapists; Official Gazette of the Federative Republic of Brazil: Brasilia, Brazil, 1997.
- Mattos, S.M.; Pereira, D.S.; Moreira, T.M.M.; Cestari, V.R.F.; Gonzalez, R.H. Physical activity and exercise recommendations during the COVID-19 pandemic: Scope review on publications in Brazil. Rev. Bras. Ativ. Fís. Saúde 2020, 25, 1–12. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010; ISBN 92-4-159997-9. [Google Scholar]
- Caputo, E.L.; Reichert, F.F. Studies of Physical Activity and COVID-19 during the Pandemic: A Scoping Review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef]
- Goodyear, V.A.; Boardley, I.; Chiou, S.-Y.; Fenton, S.A.M.; Makopoulou, K.; Stathi, A.; Wallis, G.A.; Veldhuijzen van Zanten, J.J.C.S.; Thompson, J.L. Social Media Use Informing Behaviours Related to Physical Activity, Diet and Quality of Life during COVID-19: A Mixed Methods Study. BMC Public Health 2021, 21, 1333. [Google Scholar] [CrossRef]
- Bezerra, A.C.V.; da Silva, C.E.M.; Soares, F.R.G.; da Silva, J.A.M. Factors Associated with Population Behavior During Social Isolation in the COVID-19 Pandemic. Ciênc. Saúde Coletiva 2020, 25, 2411–2421. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2019; ISBN 92-4-151418-3. [Google Scholar]
- Appleton, R.; Williams, J.; Vera San Juan, N.; Needle, J.J.; Schlief, M.; Jordan, H.; Sheridan Rains, L.; Goulding, L.; Badhan, M.; Roxburgh, E.; et al. Implementation, Adoption, and Perceptions of Telemental Health During the COVID-19 Pandemic: Systematic Review. J. Med. Internet Res. 2021, 23, e31746. [Google Scholar] [CrossRef]
- Kaihlanen, A.-M.; Virtanen, L.; Buchert, U.; Safarov, N.; Valkonen, P.; Hietapakka, L.; Hörhammer, I.; Kujala, S.; Kouvonen, A.; Heponiemi, T. Towards Digital Health Equity—A Qualitative Study of the Challenges Experienced by Vulnerable Groups in Using Digital Health Services in the COVID-19 Era. BMC Health Serv. Res. 2022, 22, 188. [Google Scholar] [CrossRef] [PubMed]
- Seifert, A.; Cotten, S.R.; Xie, B. A Double Burden of Exclusion? Digital and Social Exclusion of Older Adults in Times of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 76, e99–e103. [Google Scholar] [CrossRef] [PubMed]
- Häfele, V.; Siqueira, F. Counseling for physical activity and behavior change in Basic Health Units. Rev. Bras. Ativ. Fís. Saúde 2016, 21, 581–592. [Google Scholar] [CrossRef] [Green Version]
- de Carvalho, F.F.B.; Guerra, P.H.; Loch, M.R. Potential and challenges of body practices and physical activities in health care and promotion. Motrivivência 2020, 32, 1–18. [Google Scholar] [CrossRef]
- Siqueira, F.V.; Nahas, M.V.; Facchini, L.A.; Silveira, D.S.; Piccini, R.X.; Tomasi, E.; Thumé, E.; Hallal, P.C. Counseling for the practice of physical activity as a health education strategy. Cad. Saúde Pública 2009, 25, 203–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gvozdanović, Z.; Farčić, N.; Šimić, H.; Buljanović, V.; Gvozdanović, L.; Katalinić, S.; Pačarić, S.; Gvozdanović, D.; Dujmić, Ž.; Miškić, B.; et al. The Impact of Education, COVID-19 and Risk Factors on the Quality of Life in Patients with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2021, 18, 2332. [Google Scholar] [CrossRef]
- Stonerock, G.L.; Blumenthal, J.A. Role Of Counseling To Promote Adherence In Healthy Lifestyle Medicine: Strategies to Improve Exercise Adherence and Enhance Physical Activity. Prog. Cardiovasc. Dis. 2017, 59, 455–462. [Google Scholar] [CrossRef] [Green Version]
- Lamming, L.; Pears, S.; Mason, D.; Morton, K.; Bijker, M.; Sutton, S.; Hardeman, W. What Do We Know about Brief Interventions for Physical Activity That Could Be Delivered in Primary Care Consultations? A Systematic Review of Reviews. Prev. Med. 2017, 99, 152–163. [Google Scholar] [CrossRef]
- Lopes, S.V.; Jerônimo, J.S.; Borchardt, J.; Häfele, V.; Siqueira, F.V.; da Silva, M.C. Intervention with physical activity counseling for adults without diagnosed diseases: A systematic review. Ciênc. Saúde Coletiva 2022, 27, 2225–2240. [Google Scholar] [CrossRef]
- Hallal, P.C.; Machado, P.T.; Duca, G.F.D.; Silva, I.C.; Amorim, T.C.; Borges, T.T.; Rombaldi, A.J.; Azevedo, M.R.; Knuth, A.G. Physical Activity Advice: Short Report From a Population-Based Study in Brazil. J. Phys. Act. Health 2010, 7, 352–354. [Google Scholar] [CrossRef]
- Campbell, J.P.; Turner, J.E. Debunking the Myth of Exercise-Induced Immune Suppression: Redefining the Impact of Exercise on Immunological Health Across the Lifespan. Front. Immunol. 2018, 9, 648. [Google Scholar] [CrossRef]
- Reyes-Sánchez, F.; Basto-Abreu, A.; Torres-Alvarez, R.; Canto-Osorio, F.; González-Morales, R.; Dyer-Leal, D.D.; López-Ridaura, R.; Zaragoza-Jiménez, C.A.; Rivera, J.A.; Barrientos-Gutiérrez, T. Fraction of COVID-19 Hospitalizations and Deaths Attributable to Chronic Diseases. Prev. Med. 2022, 155, 106917. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.A.S.; Tremblay, M.S.; Marinho, F.; Ribeiro, A.L.P.; Cousin, E.; Nascimento, B.R.; Neto, P.d.F.V.; Naghavi, M.; Malta, D.C. Physical Inactivity as a Risk Factor for All-Cause Mortality in Brazil (1990–2017). Popul. Health Metr. 2020, 18, 13. [Google Scholar] [CrossRef]
- Stein, R.; Börjesson, M. Physical Inactivity in Brazil and Sweden—Different Countries, Similar Problem. Arq. Bras. Cardiol. 2019, 112, 119–120. [Google Scholar] [CrossRef]
- Swift, D.L.; McGee, J.E.; Earnest, C.P.; Carlisle, E.; Nygard, M.; Johannsen, N.M. The Effects of Exercise and Physical Activity on Weight Loss and Maintenance. Prog. Cardiovasc. Dis. 2018, 61, 206–213. [Google Scholar] [CrossRef]
| Author/Year | Local | Sample | Age Range | Sex | Characteristics of the Population | Objective | Study Design | Data Analysis |
|---|---|---|---|---|---|---|---|---|
| (Mckeon et al., 2021) [22] | Australia | 11 | >60 years | F and M | Insufficient levels of physical activity | To determine the feasibility and preliminary effectiveness of delivering an online group lifestyle intervention for older adults during the COVID-19 pandemic. | Intervention | Quantitative |
| (Mcdonough et al., 2021) [35] | United States | 64 | 18 to 35 years | F and M | Insufficient levels of physical activity and Body mass index (BMI) ≥ 18.5 kg/m2 | To examine the effects of a home-based, YouTube-delivered PA intervention grounded in self-determination theory on young adults’ free-living PA, sedentary behavior, and sleep quality. | Controlled and randomized clinical trials | Quantitative |
| (Egan et al., 2021) [31] | United Kingdom (Scotland) | 7 | >18 years | F and M | Health Professionals (Formal and informal caregivers) | To co-design and develop a novel mobile app to educate and support caregivers in the undertaking of regular physical activity at home during and beyond COVID-19 restrictions via integration of the transtheoretical model of behavior change and UK physical activity guidelines. | Longitudinal | Qualitative |
| (Johnson et al., 2021) [33] | United States | 13 | >65 years | F | BMI ≥ 18.5 kg/m2 | To examine how a telehealth intervention changed activity profiles in older adults during the COVID-19 pandemic. | Intervention | Quantitative |
| (Van de Wiel et al., 2021a) [32] | The Netherlands | 137 | >50 years | F and M | Breast and prostate cancer survivors | To develop an Internet-based physical activity (PA) support program (IPAS) and evaluate the effectiveness and costs of IPAS alone (online only) or IPAS combined with physiotherapist telephone counselling (blended care), compared to a control group. | Controlled and randomized clinical trials | Quantitative |
| (García Pérez de Sevilla et al., 2021) [16] | Spain | 24 | >18 years | F and M | Insufficient levels of physical activity | To evaluate the adherence to a lifestyle intervention carried out in university employees during the COVID-19 pandemic and its impact on health-related quality of life (HrQoL). | Controlled and randomized clinical trials | Quantitative |
| (Lin et al., 2021) [36] | Taiwan | 104 | 20 to 75 years | F and M | Type II diabetes patients | To explore the impact of diabetes self-management and HbA1c affected by the COVID-19 pandemic and the epidemic prevention work. | Quasi-experimental | Quantitative |
| (Sciamanna et al., 2021) [38] | United States | 24 | >60 years | F and M | Patients in Primary Health Care | To explore the feasibility and impact of a PCP-prescribed one-minute daily functional exercise program, consisting of 30 s each of bodyweight push-ups and squats, among 24 patients 60 years of age or older. | Intervention | Quantitative |
| (Zhang et al., 2021) [14] | China | 70 | 18 to 30 years | F | Insufficient levels of physical activity | To assess the effectiveness of an online high-intensity interval training (HIIT) intervention and health education on the behaviors, mental health, and cognitive function of sedentary young females. | Controlled and randomized clinical trials | Quantitative |
| (Jiwani et al., 2021) [37] | United States | 18 | >65 years | F and M | Type II diabetes patients, BMI ≥ 25 | To explore participants’ acceptability and experiences following a behavioral lifestyle intervention that integrated Fitbit in overweight/obese older adults with T2D amid the COVID-19 pandemic. | Intervention | Qualitative |
| (Robertson et al., 2022) [34] | United States | 16 | 28 to 82 years | F | Completion of primary cancer treatment. | To develop and characterize the relevance and potential utility of electronically delivered acceptance- and mindfulness-based approaches to physical activity promotion for insufficiently active breast cancer survivors. | Non-randomized trial | Qualitative |
| Author/Year | Means Used for Intervention | Intervention Time | Professionals Involved | Used Tools | Reference Method | Other Strategies | Intervention | Results |
|---|---|---|---|---|---|---|---|---|
| (Mckeon et al., 2021) [22] | Online platform (Facebook) | 6 weeks | Exercise physiologist and nutritionist | Educational contents of physical activity; Recommendations for physical activity or exercise; Negative effects or reduction of sedentary behavior | Transtheoretical model | Did not describe | Distribution of weekly content on physical activity. Facilitators provide education and discussion on goal setting, balance training, reducing sedentary behavior, and diet (posts and video calls in groups); The content was shaped by defined behavior change techniques, such as social support, self-monitoring, identification of barriers, and feedback. | The response rate of the intervention group was 91.0%. The intervention showed evidence of effect for the investigated outcomes (psychological distress, quality of life, sedentary time, function, loneliness, walking time, and moderate and vigorous physical activity). |
| (Mcdonough et al., 2021) [35] | Online platform (YouTube) | 12 weeks | Project manager | Educational contents of physical activity; Recommendations for physical activity or exercise; Physical activity guidelines; Negative effects or reduction of sedentary behavior | Theory of self-determination | Did not describe | Intervention Group: home-based physical activity, with distribution of videos with aerobic exercises, muscle strength, health education videos, and health education related to physical activity; Control group: only weekly health education videos, with physical activity content; The interventions were delivered via an online platform (YouTube), based on the theory of self-determination on the practice of free lifestyle activities by young people, sedentary behavior, and sleep quality. | The intervention showed a significant association for the intervention group, in the variables moderate and vigorous physical activity, sleep efficiency, frequency of physical activity for muscle strengthening, motivation related to physical activity, and coping with barriers to physical activity (p < 0.001–0.002). |
| (Egan et al., 2021) [31] | Online application (CAREFIT) | 6 months | Multidisciplinary team—health professionals, caregivers, and health specialists | Educational contents of physical activity; Physical activity guidelines | Transtheoretical model | Motivation; Communication | Custom application development (CAREFIT) with approaches based on national physical activity guidelines and behavior change models. The application addressed physical activity content, elements of education, communication, tools, or motivation to perform regular physical activity. | Results were based on feedback from participants regarding physical activity orientation, type of physical activity, intensity, educational sections, and others. Thus, it was not possible to identify an effect on the increase in physical activity levels. |
| (Johnson et al., 2021) [33] | Online platform (Google Classroom) and telehealth (telephone contact) | 6 weeks | Trained interviewers | Educational contents of physical activity; General practices of healthy behaviors | Did not use reference method | Definition of goals; Skills; Autonomy | Distribution of teaching materials related to the practice of healthy lifestyle behaviors. Facilitators work individually with participants over the phone to discuss the intervention and develop a personalized physical activity strategy, encouraging participation in light and moderate to vigorous physical activity was emphasized, sense of relationship, and competence. The definition of goals was also used to encourage participants to practice physical activities, autonomy, feelings, and the reinforcement of competence in physical activities. | After completion of the intervention, moderate to vigorous participation in physical activity increased by an estimated 2 min/day (CI: −21, 26) and 12 min/week (CI: −154, 180), but this trend was not statistically significant. |
| (Van de Wiel et al., 2021a) [32] | Online platform (Physical Activity Support Program) and telephone contact | 6 weeks | Doctors, nurses, and physiotherapists | Educational contents of physical activity; Recommendations for physical activity or exercise; Benefits of physical activity; Physical activity guidelines | Transtheoretical model | Definition of goals; Motivation; barriers; self-monitoring | Control group: received a printed leaflet with guidelines and possible benefits of physical activity after cancer treatment. It also introduced physical activity guidelines and provided information on monitoring and intensity of physical activity; Online group: received access to the Online Physical Activity Support Program (IPAS), structured according to the transtheoretical model, using aspects of the theory of planned behavior and social cognitive theory. Participants were separated into stages of behavior change and, according to each stage, received information, images, and interactive attributions and videos of physical activity; Blended group: Received access to IPAS and phone calls for physical activity counseling. Subjects were asked to exercise on a stationary bike or treadmill and to establish goals and targets for intended behavior change. | The intervention showed no significant association with moderate and vigorous physical activity between the online group and the control group (p = 0.39), and between the blended care group and the control group (p = 0.75). Additionally, of the 1242 invited patients, 137 participated in the study (participation rate: 11.0%). |
| (García Pérez de Sevilla et al., 2021) [16] | Online platform and face-to-face service | 18 weeks | Nutritionists and Fitness Trainers | Educational contents of physical activity; Recommendations for physical activity or exercise | Did not use reference method | Motivation; Practical recommendations | Intervention group: Educational intervention on healthy habits, with distribution of 12 weekly videos on motivation for change, exercise recommendations, and exercise strategies. Afterwards, nutritional intervention and physical activity were performed. Carried out recommendations on physical activity and nutrition to maintain acquired habits in the long term; Control group: routine activities without supervision. | The intervention group showed a significant association with quality of life in the time and group interaction, (p = 0.03) health responsibility (p = 0.02), physical activity (p = 0.02), and nutrition (p = 0.02), with a large effect size for these four variables. Sitting time was reduced by 2.5 h per day, with a moderate effect size. |
| (Lin et al., 2021) [36] | Telephone contact and face-to-face service | 6 months | Trainer and Master’s in Public Health | Did not describe | Transtheoretical model | Goal setting | Intervention group: coaching sessions via telephone, all for six months, on top of shared diabetes care, which includes setting goals for behavior change; Control group: a face-to-face coaching and baseline measurement session at the baseline without having any coaching calls; Both intervention and control groups received diabetes health education and usual care. | Positive associations were found between the intervention, setting physical activity goals. and physical activity indicator (p = 0.007). |
| (Sciamanna et al., 2021) [38] | Online platform (email) | 24 weeks | Doctor | Did not describe | Did not use reference method | Brief reminders for physical activity; congratulatory message | Patients were advised to perform squatting and bending exercises, lasting 60 to 90 s. Moreover, brief messages were made available via email to remind participants to perform the exercises, congratulations and memes (humorous images) if the participant entered data about the exercise performed on the day, frequency with which other patients had completed the exercises, the longest daily sequence, and comments that other patients provided. | The intervention response rate was 42.0% over 24 weeks. The intervention showed a significant association with maximal performance in the squat (p < 0.001) and flexion over time (p < 0.0001), suggesting that one-minute counseling was feasible, acceptable, and effective for improving physical fitness. |
| (Zhang et al., 2021) [14] | Online platform (Zoom) | 9 weeks | Professional coaches | Educational contents of physical activity; Negative effects or reduction of sedentary behavior | Did not use reference method | Did not describe | Intervention group: 6-week high-intensity interval training (HIIT) and health education intervention; Control Group: 6-week health education (body self-cognition, exercise, physical inactivity and health, nutrition and diet, fat reduction, muscle gain and shaping, stretching, meditation, relaxation and rehabilitation, and emotion regulation) and risk of sedentary behavior; Both groups received the same lecture content. | The response rate of the intervention group was 100.0% and that of the control group was 78.0%. Positive associations were found between the intervention group and moderate to vigorous physical activity (p < 0.001), while the control group demonstrated a reduction in sedentary time (p = 0.03). In addition, levels of anxiety (p = 0.002) and stress (p = 0.001) were shown to significantly reduce in the intervention group over the six-week period. |
| (Jiwani et al., 2021) [37] | Online platform (WebEx) and online application (FitBit) | 6 months | Researcher | Did not describe | Transtheoretical model | Definition of goals; Motivation; Barriers; Feedback; Self-monitoring; Social support | Behavioral lifestyle intervention (diet and physical activity) with integration of self-monitoring (FitBit app). The facilitator used a publicly available behavioral intervention guide for the study sessions, focusing on adherence to behaviors using motivational strategies. Each participant was given a weight loss and physical activity goal. | The response rate of the intervention group was 90.0%. The results showed good acceptance by the participants of the intervention and with the use of Fitbit technology for self-monitoring of diet and physical activity, high degree of acceptability to the program, and participant motivation to continue to track behavior using program strategies. |
| (Robertson et al., 2022) [34] | Online platform | 4 to 8 weeks | Did not describe | Educational contents of physical activity; General practices of healthy behaviors | Did not use reference method | Did not describe | Acceptance and mindfulness-based intervention (living flexibly) was delivered electronically through survey, and consisted of narrated videos with visual aids, audio files, images, text and accompanying documents, and email and text messages presenting techniques for promoting physical activity. | The results were based on feedback from participants, demonstrating that the content of the intervention was acceptable and relevant to meet needs related to healthy living. |
| Controlled Intervention Studies £ | ||||||
| Criteria | (Mcdonough et al., 2021) [35] | (Van de Wiel et al., 2021a) [32] | (García Pérez de Sevilla et al., 2021) [16] | (Lin et al., 2021) [36] | (Zhang et al., 2021) [14] | (Jiwani et al., 2021) [37] |
| Described as rehearsal | Y | Y | Y | Y | Y | Y |
| Proper randomization | Y | Y | Y | Y | Y | N |
| Hidden treatment | Y | Y | N | Y | Y | N |
| Blinded participants and providers | Y | N | N | Y | Y | N |
| Blinded evaluators | Y | N | N | Y | N | N |
| Similar groups | Y | Y | Y | Y | Y | Y |
| Abandonment rate 20% or lower | Y | N | N | Y | Y | Y |
| Dropout rate by 15 percentage points or lower | Y | N | N | Y | N | Y |
| High adhesion | Y | N | N | N | Y | N |
| Similar interventions were avoided | Y | N | Y | Y | N | N |
| Valid outcome | Y | Y | Y | Y | Y | N |
| Enough sample | Y | N | N | Y | Y | N |
| Outcomes have been reported | Y | Y | Y | Y | Y | N |
| Participants analyzed in the original group | Y | Y | Y | Y | Y | N |
| Total score * | 1.0 | 0.5 | 0.5 | 0.9 | 0.7 | 0.3 |
| Before-After (Pre-Post) Studies with No Control Group £ | ||||||
| Criteria | (Johnson et al., 2021) [33] | (Mckeon et al., 2021) [22] | (Sciamanna et al., 2021) [38] | (Egan et al., 2021) [31] | (Robertson et al., 2022) [34] | |
| Clear objective | Y | Y | Y | Y | Y | |
| Selection eligibility | Y | Y | Y | Y | Y | |
| Eligible participants | Y | Y | Y | Y | Y | |
| Enrollment criteria | Y | Y | Y | Y | Y | |
| Enough sample size | N | Y | N | N | Y | |
| Intervention described to the Population | Y | Y | Y | Y | Y | |
| Valid outcomes | Y | Y | Y | Y | Y | |
| Blinding of evaluators | NR | NR | Y | N | N | |
| Follow loss of 20% or less | Y | N | NR | NR | N | |
| Losses were accounted for in the analysis | N | Y | Y | N | N | |
| Statistics performed before and after the intervention | Y | Y | Y | N | N | |
| P-value and pre-post-post analysis | N | Y | Y | NR | Y | |
| Measures of interest before and after the intervention | - | - | - | - | - | |
| Group-level intervention and individual-level analysis to consider group effects | - | - | - | - | - | |
| Total score * | 0.7 | 0.8 | 0.8 | 0.5 | 0.7 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonçalves, L.; Moraes, M.S.; Silva, D.A.S. Counseling for Physical Activity in Adults during the COVID-19 Pandemic: A Scope Review. Int. J. Environ. Res. Public Health 2022, 19, 8687. https://doi.org/10.3390/ijerph19148687
Gonçalves L, Moraes MS, Silva DAS. Counseling for Physical Activity in Adults during the COVID-19 Pandemic: A Scope Review. International Journal of Environmental Research and Public Health. 2022; 19(14):8687. https://doi.org/10.3390/ijerph19148687
Chicago/Turabian StyleGonçalves, Letícia, Mikael Seabra Moraes, and Diego Augusto Santos Silva. 2022. "Counseling for Physical Activity in Adults during the COVID-19 Pandemic: A Scope Review" International Journal of Environmental Research and Public Health 19, no. 14: 8687. https://doi.org/10.3390/ijerph19148687
APA StyleGonçalves, L., Moraes, M. S., & Silva, D. A. S. (2022). Counseling for Physical Activity in Adults during the COVID-19 Pandemic: A Scope Review. International Journal of Environmental Research and Public Health, 19(14), 8687. https://doi.org/10.3390/ijerph19148687







