1. Introduction
The mosquito is the world’s deadliest creature. They caused around 750,000 deaths worldwide through the transmission of mosquito-borne diseases (MBDs) in 2018 [
1,
2]. An MBD occurs when mosquitoes infected with parasites or viruses transmit the pathogens to their host while feeding on the host’s blood. The most common MBD is malaria, with the highest fatality rate and the highest (65,493.1) disability-adjusted life years (DALYs), followed by lymphatic filariasis (DALYs 2022.1) and dengue (DALYs 1142.7) [
3]. Around 2400 million people worldwide are at risk of developing malaria, whereas dengue can cause 100–400 million estimated infections each year [
4,
5]. In addition to health suffering and death, economic losses due to MBDs are underrated. The direct cost of MBDs for treatment and prevention purposes spent by the government and individuals, as well as indirect costs due to productive labor time lost, is not accumulated and thus overlooked. A study estimated that the annual cost of dengue illness in the Americas is USD 2.1 billion, without the cost of preventive measures [
6]. However, this can create a huge economic burden for developing countries such as Bangladesh. A recent study showed that the aggregate economic expenditure for dengue treatment in Bangladesh is around USD 15.27 million a year [
7].
Bangladesh is prone to MBDs due to the combination of several factors such as climate change, rapid urbanization, increased human mobility, improper drainage systems, illiteracy, and lack of awareness [
8,
9]. About 33.6% of the population of Bangladesh is at risk of contracting malaria, while it is estimated that around 70 million people are at risk of developing lymphatic filariasis [
10]. Bangladesh saw a massive outbreak of dengue fever in 2019, where 100,000 people were infected with 197 confirmed deaths, and an outbreak of chikungunya fever in 2017, where more than 13,000 were infected [
11,
12]. A recent study reported the high prevalence of Japanese encephalitis in Bangladesh, as around 8% of patients with meningitis-encephalitis syndrome were diagnosed with it [
13]. However, due to a lack of proper surveillance and reporting, we can assume the number to be higher than reported. The increase in global movement and presence of appropriate vectors has made the introduction of other MBDs such as Zika, West Nile fever, and yellow fever into Bangladesh a matter of time. Remarkably, different regions of Bangladesh showed variations in the endemicity of different MBDs. The southern hill region is malaria-endemic, while most lymphatic filariasis cases are reported in the northern part of the country [
14]. Though dengue and chikungunya cases were documented all around the country, the highest prevalence was present in the central part of the country due to urbanization and dense population, which favors the breeding of its vector,
Aedes spp.
Current control strategies of MBDs largely rely on vector control through the use of synthetic pesticides against mosquito larva or their mature form. However, it has negative impacts on the environment, high operational costs, and there is a chance of developing resistant mosquito populations [
15,
16]. Microbial controls of mosquitoes through the application of entomopathogenic fungus and symbiotic bacteria, genetic modification, and plant-derived, eco-friendly, insecticidal nanoparticles are gaining much attention [
15,
17]. Enormous efforts have been made toward the development of vaccines against some of these MBD pathogens, but with limited success [
18,
19].
The increase in mosquito-borne diseases is highly anthropogenic and connected to global climate change, involving high temperatures or rainfall that affects mosquito bionomics [
20]. However, simple human intervention and behavioral changes can reduce the mosquito load significantly [
21]. On the other hand, education and knowledge regarding MBD and mosquito control can lead to improved attitudes of citizens and help them to adopt protective practices [
22]. Previous knowledge, attitude, and practice (KAP) studies conducted in different regions of Bangladesh on malaria and dengue have demonstrated a knowledge gap among community dwellers regarding the transmission, prevention, or treatment of MBDs and their reluctance to perform preventive measures [
23,
24]. Another study conducted among university students in Dhaka City, Bangladesh, showed good knowledge (66.72%), attitude (89.28%), and practices (68.32%) scores, though the authors emphasized the inclusion of infectious disease-related subjects into the university curriculum [
25]. However, most of these studies were focused on a specific MBD or carried out in communities of a specific zone, such as hilly tracts or city areas. The aim of this study was to conduct a KAP survey on common MBDs (malaria, lymphatic filariasis, dengue, and chikungunya) in Bangladesh, involving people of all walks of life to understand different socio-economic predictors of improved knowledge, attitude, and practices (KAP) regarding MBDs.
4. Discussion
Mosquito-borne diseases are considered a major health threat in Southeast Asian countries such as Bangladesh because of unplanned and impromptu urbanization and overpopulation, which serves as a suitable environment for rapid dissemination of MBDs such as dengue, malaria, filariasis, and chikungunya [
29]. To prevent and control such life-threatening diseases, socio-demographical factors as well as the KAP among the population play critical roles [
30]. The study was conducted to assess the KAPs regarding MBDs and their prevention in different regions of Bangladesh.
Results obtained from the investigation showed evidence of rather good knowledge about major MBDs in the urban population of Bangladesh. The majority of the respondents were familiar with mosquito-borne diseases (98%), and among the diseases, dengue was the more commonly known (97%). Only half of the respondents were familiar with filariasis (53%), while malaria (85%) and chikungunya (81%) were relatively well-known. These findings can be compared with another study conducted by Saha et al. [
31], where it was found that 89% of respondents were aware of malaria, while a recent study by Farzana et al. [
32] reported that 97% of the population was familiar with dengue fever, supporting our data. The data can also be compared with similar studies conducted in Nepal [
33], India [
34], and Jamaica [
35].
Knowledge regarding the nature of mosquitoes among the respondents revealed that the majority of the participants were familiar with the name
Aedes spp. (91%), while half of them knew about
Anopheles spp. (52%). The maximum number of respondents that were aware of the fact that dengue and chikungunya-carrying mosquitoes bite during daytime was 74%, which is similar to the findings of Rahman et al. [
36]. Regarding the malarial vector, 59% of the respondents correctly answered that the biting period of malarial vectors was during nighttime, which is a higher number than found in a previous study by Saha et al. [
31]. When asked about the breeding environment of mosquito vectors, about 86% of the participants replied that mosquitoes could breed in stagnant water, while 63% answered that mosquitoes could be born in both clean and dirty water. These data can be compared with a previous study by Abir et al., where most of the participants were aware of the fact that mosquitoes lay eggs in clear water [
37]. However, a previous study by Dhar–Chowdhury et al. claimed a much lower percentage (87%) of awareness among residents of Dhaka City [
38].
In regard to the knowledge about the symptoms of dengue fever, three-fourths of the respondents (75%) replied that muscle pain was the most common symptom alongside fever. Most of the respondents’ knowledge accuracy regarding other common symptoms of dengue fever was significant, including rash (58%), vomiting (57%), and pain behind the eyes (49%). However, a considerable number of participants did not know most of these common symptoms. This result can be compared with another similar study about dengue fever among university students in Bangladesh, where the accuracy of knowledge among respondents was much higher than in the current study (joint pains (92.5%), muscle pain (82.4%), and pain behind the eyes (70%)) [
32]. However, this fact can be linked to the educational background of the respondents, as only 43.6% of respondents from the present study had an education of undergraduate level or above compared to the aforementioned study conducted on the university students. That study claimed a statistically significant relation between the KAP level of respondents and their academic attainment [
32]. In the case of filariasis, major symptoms, along with fever, known to respondents were elephantiasis of different organs (66%), axillary lymphadenopathy (93%), and skin exfoliation (25%). When asked about symptoms of malarial fever, 56% of the participants said that vomiting was the major symptom of malaria besides fever, while 55% and 44% of the respondents acknowledged muscle pain and diarrhea to be other significant symptoms, respectively. This can be compared to a previous study by Saha et al. [
31] about malarial symptoms, where 63% of the respondents knew the principal signs and symptoms of malaria accurately. The present study showed that the overall mean knowledge score among the respondents was 60.7 ± 18.1, which is satisfactory. Most of the participants had a moderate knowledge (45.0%) about mosquito-borne diseases, which is essential for the prevention of MBD outbreaks.
Regarding the attitudes toward mosquito-borne diseases, the majority of the participants of the present study responded positively, as about 97% of the respondents acknowledged the effects of MBDs. Overall, 68% of the participants had good attitudes towards mosquito-borne disease eradication and prevention. Most of the respondents in this study agreed that mosquito-borne diseases are a major problem in Bangladesh (97%) and can be fatal (93%), but they were also hopeful about the prevention of mosquito-borne diseases (95%). These data support a recent study conducted in Bangladesh claiming that 85% of the population agreed that MBDs such as dengue could be prevented [
32]. However, in a similar study conducted in Western Australia, people showed much less concern about MBDs as only 25% of the respondents acknowledged mosquitoes as a health risk, while a major portion of them (43%) considered the bug as a nuisance [
39].
When asked about awareness among general people, 97% of the respondents agreed that more awareness should be generated for effective prevention, and 79% replied that they were aware of the mosquitoes breeding in their surroundings. On the subject of the role of government in the prevention and eradication of mosquito-borne diseases in Bangladesh, 46% of the participants responded positively, as they felt the government is taking enough steps to prevent mosquito-borne diseases, but 39% were dissatisfied with the involvement of government in the matter. When opinions about the role of citizens were inquired about, most of the participants (97%) strongly agreed that an active role of the citizen is required in addition to the government to prevent mosquito-borne diseases. More than half of the respondents (64%) fear that there is a chance of new types of MBDs emerging in Bangladesh.
The majority of the respondents (95%) considered “unawareness” as the major obstacle in preventing MBDs, reflecting the fact that a major proportion of the population is still ignorant of information regarding MBDs, such as mosquitoes, their breeding habitats, signs and symptoms related to different kinds of MBDs, and preventive measures. Other factors deemed by participants as obstacles in MBD prevention included negative public attachment (53%), less effective role of government (49%), and financial constraints (34%). Though most of the respondents demonstrated positive attitudes toward MBD control and prevention, they also indicated insufficient measures taken by the government in this regard. However, a majority of respondents also acknowledged the impact of their individual actions on the community in the prevention and control of MBDs. In fact, in countries like Bangladesh, it is quite impossible for the government to control MBDs alone. Similar studies conducted in Western Australia and Congo noted a stark difference, however, citing the local participants’ attitude towards community, as they recognize their duties only for self-protection for their own household, but not for local communities [
40,
41].
On inquiring about practices among respondents to prevent MBDs, bed nets were found to be the most common. Of the participants, 94% were found to use bed nets regularly to prevent mosquito bites, while other popular preventive measures included mosquito coils (86%), fans (45%), electric bats (42%), and insecticide sprays (33%). These practices are common across the region, as similar practices were noted in several previous studies conducted in Bangladesh [
31], India [
42], and Jamaica [
35]. About three-fourths of the participants claimed that they clean their surroundings, but only half of the participants were practicing regular cleaning of their household water storage, reflecting a gap in practice for proper control of mosquito breeding.
Interestingly, a large portion of the respondents (73%) were reluctant to contact the local government in case of increased mosquito infestations, indicating a communication gap between the local government and the people. In contrast, the Western Australian people mentioned in a previous study were more trusting of their government’s actions [
41], which in turn provided the decision-makers an opportunity to get closer to the community and for healthcare personnel to be involved and maximize the educational activities among the population. In Bangladesh, the government could achieve a similar level of involvement with the people by proper and effective utilization of media, including the internet and visual platforms, to encourage a dependable relationship between government and local communities to successfully control and prevent mosquito-borne diseases. Social and environmental awareness and responsibilities should also be acknowledged for an effective prevention regime.
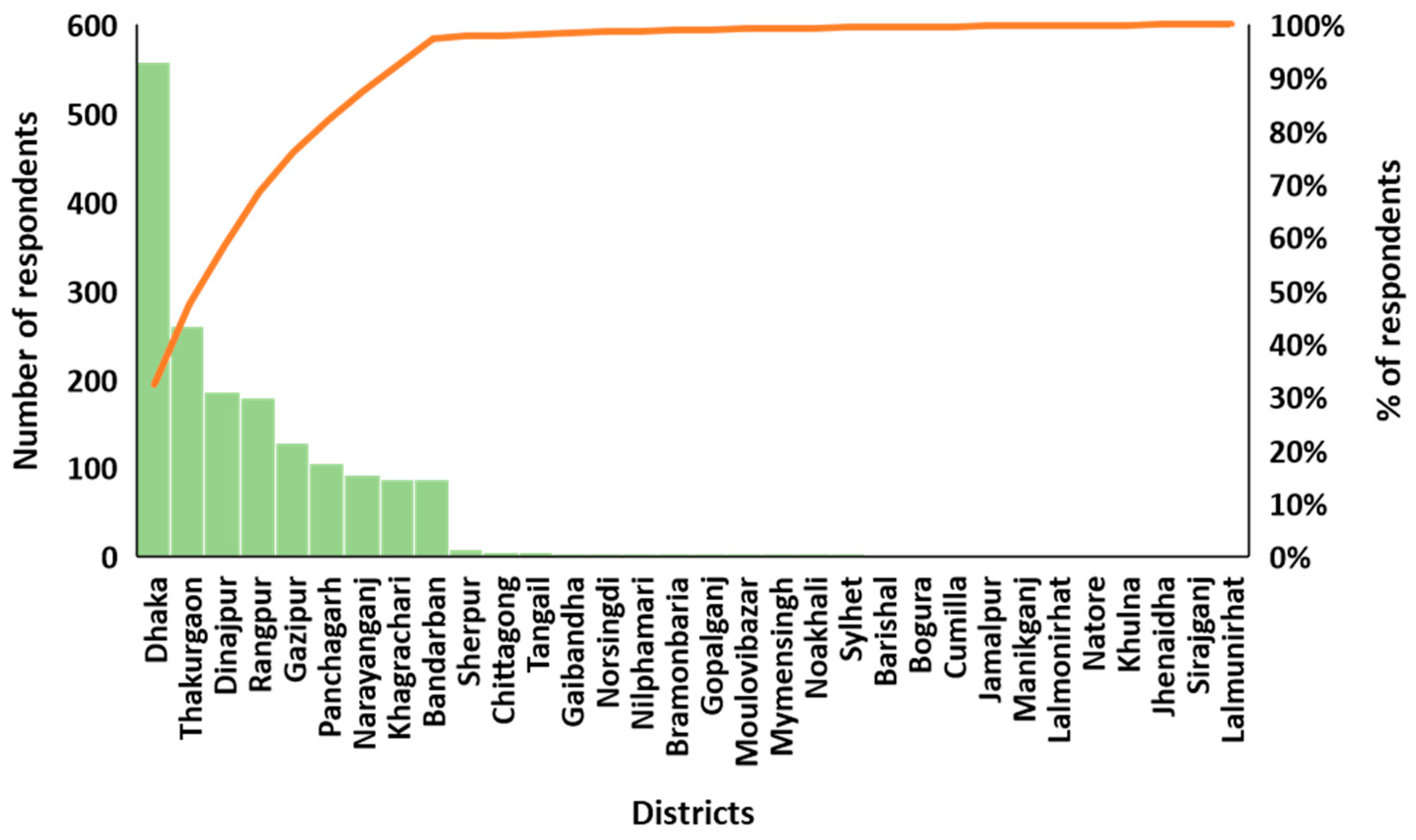
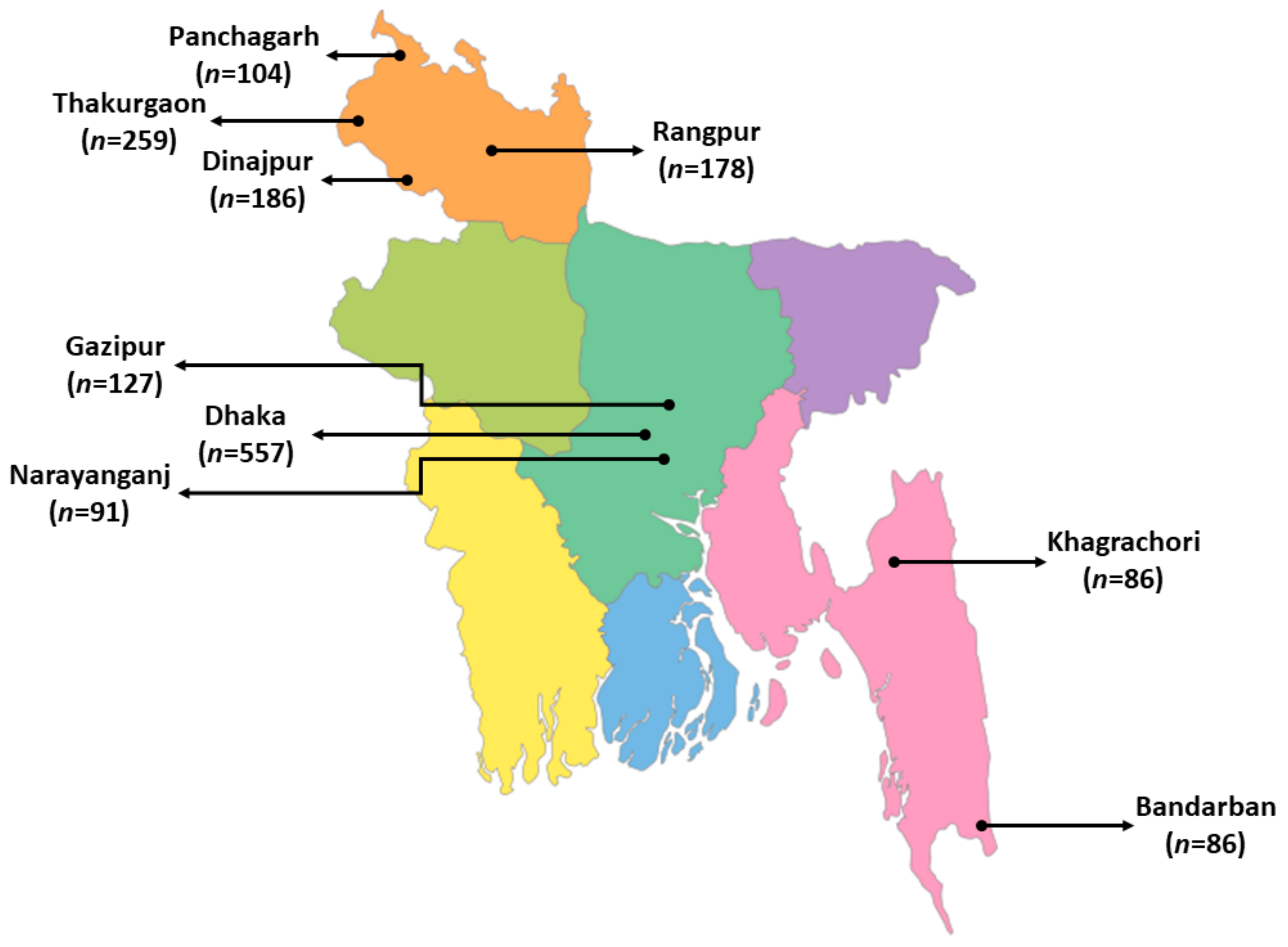
Although we collected a large sample in our current study, it does not properly represent the whole country due to the skewness of the responses from big cities. It is important to point out as a weakness of this study the possibility of bias in the sampling. Despite our best efforts to obtain a representative sample of survey respondents, we completely relied on our volunteers and students from Jahangirnagar University and a local research team, who collected data from their hometown or residing town. Our questionnaire was a closed type, which helped us avoid non-response bias. If a respondent did not understand the question, the person collecting the data told him or her to try again. People often do not practice what they preach. Their attitude might be different when the researcher is away. The results should be taken cautiously with more constructive measures.