Implementation of Virtual Communities of Practice in Healthcare to Improve Capability and Capacity: A 10-Year Scoping Review
Abstract
1. Introduction
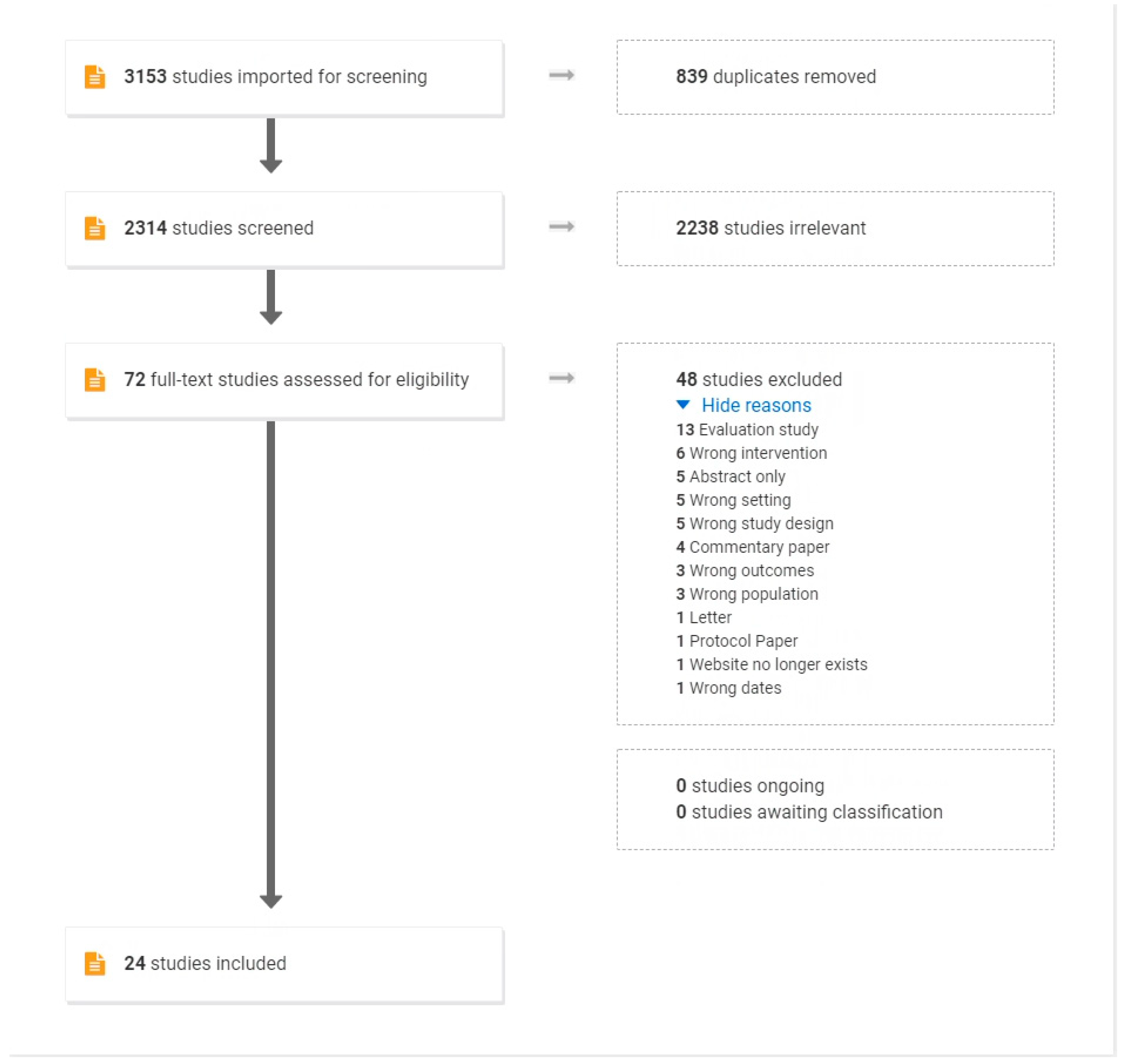
2. Materials and Methods
- (a)
- Identifying the research question
- (b)
- Identifying relevant studies
- (c)
- Study selection criteria
- (d)
- Charting the data
- (e)
- Collating, summarising, and reporting the results
3. Results
3.1. Study Characteristics
3.2. Research Methodology
3.3. Literature Review Papers
3.4. Study Aims
3.5. Background and Purpose of the VCoP
3.6. Dates
3.7. Methods of Recruitment
3.8. VCoP Membership
3.9. Sponsorship and Leadership Roles
3.10. Technology and Infrastructure
3.11. VCoP Development
3.12. Size of the Network
3.13. VCoP Forms of Interaction
3.14. Theoretical Frameworks Supporting Development of the VCoPs
3.15. Outcome Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wenger, E. Communities of Practice: A Brief Introduction. 2004. Available online: https://wenger-trayner.com/introduction-to-communities-of-practice/ (accessed on 26 May 2022).
- Barnett, S.; Jones, S.C.; Bennett, S.; Iverson, D.; Robinson, L.; Paton, C.; Boudry, C. A virtual community of practice for general practice training: A preimplementation survey. JMIR Med. Educ. 2016, 2, e13. [Google Scholar] [CrossRef] [PubMed]
- Fragou, O. A Design Framework for Building a Virtual Community of Practice. In The Challenges of the Digital Transformation in Education, Proceedings of the 21st International Conference on Interactive Collaborative Learning (ICL2018), Kos Island, Greece, 25–28 September 2018; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Mills, J.; Li, C.; Fullerton, S.; Chapman, M.; Jap, J.; Sinclair, C.; Collins, A.; Campbell, E. Staying connected and informed: Online resources and virtual communities of practice supporting palliative care during the novel coronavirus pandemic. Prog. Palliat. Care 2020, 28, 251–253. [Google Scholar] [CrossRef]
- Ikioda, F.; Kendall, S.; Brooks, F.; Reidy, C. Developing an online community of practice to empower health visitors: Findings from a pilot study. J. Health Visit. 2014, 2, 436–440. [Google Scholar] [CrossRef]
- Barnett, S.; Jones, S.C.; Bennett, S.; Iverson, D.; Bonney, A. General practice training and virtual communities of practice-a review of the literature. BMC Fam. Pract. 2012, 13, 87. [Google Scholar] [CrossRef]
- Dieleman, C.; Duncan, E.A. Investigating the purpose of an online discussion group for health professionals: A case example from forensic occupational therapy. BMC Health Serv. Res. 2013, 13, 253. [Google Scholar] [CrossRef]
- McLoughlin, C.; Patel, K.D.; O’Callaghan, T.; Reeves, S. The use of virtual communities of practice to improve interprofessional collaboration and education: Findings from an integrated review. J. Interprof. Care 2017, 32, 136–142. [Google Scholar] [CrossRef]
- Antonacci, G.; Colladon, A.F.; Stefanini, A.; Gloor, P. It is rotating leaders who build the swarm: Social network determinants of growth for healthcare virtual communities of practice. J. Knowl. Manag. 2017, 21, 1218–1239. [Google Scholar] [CrossRef]
- Malinen, S. Understanding user participation in online communities: A systematic literature review of empirical studies. Comput. Hum. Behav. 2015, 46, 228–238. [Google Scholar] [CrossRef]
- Amichai-Hamburger, Y.; Gazit, T.; Bar-Ilan, J.; Perez, O.; Aharony, N.; Bronstein, J.; Dyne, T.S. Psychological factors behind the lack of participation in online discussions. Comput. Hum. Behav. 2016, 55, 268–277. [Google Scholar] [CrossRef]
- Nistor, N.; Baltes, B.; Dascălu, M.; Mihăilă, D.; Smeaton, G.; Trăuşan-Matu, Ş. Participation in virtual academic communities of practice under the influence of technology acceptance and community factors. A learning analytics application. Comput. Hum. Behav. 2014, 34, 339–344. [Google Scholar] [CrossRef]
- Dubé, L.; Bourhis, A.; Jacob, R. Towards a typology of virtual communities of practice. Interdiscip. J. Inf. Knowl. Manag. 2006, 1, 69–93. [Google Scholar] [CrossRef]
- Sims, J.M. Communities of practice: Telemedicine and online medical communities. Technol. Forecast. Soc. Chang. 2018, 126, 53–63. [Google Scholar] [CrossRef]
- University of New Mexico, H.S. Project ECHO 2022. Available online: https://hsc.unm.edu/echo/ (accessed on 26 May 2022).
- Lewiecki, E.M.; Jackson, A.; Lake, A.F.; Carey, J.J.; Belaya, Z.; Melnichenko, G.A.; Rochelle, R. Bone health TeleECHO: A force multiplier to improve the care of skeletal diseases in underserved communities. Curr. Osteoporos. Rep. 2019, 17, 474–482. [Google Scholar] [CrossRef] [PubMed]
- Nickson, C.P.; Cadogan, M.D. Free Open Access Medical education (FOAM) for the emergency physician. Emerg. Med. Australas. 2014, 26, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Roland, D.; Spurr, J.; Cabrera, D. Preliminary evidence for the emergence of a health care online community of practice: Using a netnographic framework for Twitter hashtag analytics. J. Med. Internet Res. 2017, 19, e7072. [Google Scholar] [CrossRef]
- Cadogan, M.; Thoma, B.; Chan, T.M.; Lin, M. Free Open Access Meducation (FOAM): The rise of emergency medicine and critical care blogs and podcasts (2002–2013). Emerg. Med. J. 2014, 31, e76–e77. [Google Scholar] [CrossRef]
- Thoma, B.; Brazil, V.; Spurr, J.; Palaganas, J.; Eppich, W.; Grant, V.; Cheng, A. Establishing a Virtual Community of Practice in Simulation: The Value of Social Media. Simul. Healthc. 2018, 13, 124–130. [Google Scholar] [CrossRef]
- Ranmuthugala, G.; Plumb, J.J.; Cunningham, F.C.; Georgiou, A.; Westbrook, J.I.; Braithwaite, J. How and why are communities of practice established in the healthcare sector? A systematic review of the literature. BMC Health Serv. Res. 2011, 11, 273. [Google Scholar] [CrossRef]
- Wenger, E.; McDermott, R.A.; Snyder, W. Cultivating Communities of Practice: A Guide to Managing Knowledge; Harvard Business Press: Brighton, MA, USA, 2002. [Google Scholar]
- Probst, G.; Borzillo, S. Why communities of practice succeed and why they fail. Eur. Manag. J. 2008, 26, 335–347. [Google Scholar] [CrossRef]
- Li, L.C.; Grimshaw, J.M.; Nielsen, C.; Judd, M.; Coyte, P.C.; Graham, I.D. Use of communities of practice in business and health care sectors: A systematic review. Implement. Sci. 2009, 4, 27. [Google Scholar] [CrossRef]
- Shaw, L.; Jazayeri, D.; Kiegaldie, D.; Morris, M. Virtual communities of practice to improve clinical outcomes in healthcare: Protocol for a 10-year scoping review. BMJ Open 2021, 11, e046998. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute: Adelaide, Australia, 2020. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Pratte, G.; Hurtubise, K.; Rivard, L.; Berbari, J.; Camden, C. Developing a web platform to support a community of practice: A mixed methods study in pediatric physiotherapy. J. Contin. Educ. Health Prof. 2018, 38, 19–24. [Google Scholar] [CrossRef]
- Rolls, K.D.; Hansen, M.M.; Jackson, D.; Elliott, D. Intensive care nurses on social media: An exploration of knowledge exchange on an intensive care virtual community of practice. J. Clin. Nurs. 2020, 29, 1381–1397. [Google Scholar] [CrossRef]
- Vinson, C.A. Using concept mapping to develop a conceptual framework for creating virtual communities of practice to translate cancer research into practice. Prev. Chronic Dis. 2014, 11, E68. [Google Scholar] [CrossRef][Green Version]
- Galheigo, S.M.; Braga, C.P.; Magalhães, L.; Kinsella, E.A. An occupational therapy community of practice within pediatric acute care: Fostering professional, social and cultural capital in resource challenged settings. Cad. Bras. Ter. Ocup. 2019, 27, 776–791. [Google Scholar] [CrossRef]
- Mayrhofer, A.; Goodman, C.; Holman, C. Establishing a community of practice for dementia champions (innovative practice). Dementia 2015, 14, 259–266. [Google Scholar] [CrossRef]
- Adedoyin, A.C.A. Deploying virtual communities of practice as a digital tool in social work: A rapid review and critique of the literature. Soc. Work Educ. 2016, 35, 357–370. [Google Scholar] [CrossRef]
- Ranmuthugala, G.; Cunningham, F.C.; Plumb, J.J.; Long, J.; Georgiou, A.; Westbrook, J.I.; Braithwaite, J. A realist evaluation of the role of communities of practice in changing healthcare practice. Implement. Sci. 2011, 6, 49. [Google Scholar] [CrossRef] [PubMed]
- Rolls, K.; Hansen, M.; Jackson, D.; Elliott, D. How health care professionals use social media to create virtual communities: An integrative review. J. Med. Internet Res. 2016, 18, e5312. [Google Scholar] [CrossRef] [PubMed]
- Lewis, H.; Becevic, M.; Myers, D.; Helming, D.; Mutrux, R.; Fleming, D.A.; Edison, K. Dermatology ECHO-an innovative solution to address limited access to dermatology expertise. Rural Remote Health 2018, 18, 4415. [Google Scholar] [CrossRef] [PubMed]
- Coleman, A. A virtual community of practice framework to support doctors’ practices in national health insurance (NHI) in South Africa. Stud. Ethno Med. 2012, 6, 155–160. [Google Scholar] [CrossRef][Green Version]
- Farrell, M.M.; La Porta, M.; Gallagher, A.; Vinson, C.; Bernal, S.B. Peer Reviewed: Research to Reality: Moving Evidence Into Practice Through an Online Community of Practice. Prev. Chronic Dis. 2014, 11, E78. [Google Scholar] [CrossRef]
- Alary Gauvreau, C.A.; Le Dorze, G.; Kairy, D.; Croteau, C. Evaluation of a community of practice for speech-language pathologists in aphasia rehabilitation: A logic analysis. BMC Health Serv. Res. 2019, 19, 530. [Google Scholar] [CrossRef]
- Dearing, J.W.; Greene, S.M.; Stewart, W.F.; Williams, A.E. If we only knew what we know: Principles for knowledge sharing across people, practices, and platforms. Transl. Behav. Med. 2011, 1, 15–25. [Google Scholar] [CrossRef]
- Friberger, M.G.; Falkman, G. Collaboration processes, outcomes, challenges and enablers of distributed clinical communities of practice. Behav. Inf. Technol. 2013, 32, 519–531. [Google Scholar] [CrossRef]
- Wolbrink, T.A.; Kissoon, N.; Mirza, N.; Burns, J.P. Building a global, online community of practice: The OPENPediatrics World Shared Practices Video Series. Acad. Med. 2017, 92, 676–679. [Google Scholar] [CrossRef]
- Lewis, L.A.; Koston, Z.; Quartley, M.; Adsit, J. Virtual communities of practice: Bridging research and practice using Web 2.0. J. Educ. Technol. Syst. 2010, 39, 155–161. [Google Scholar] [CrossRef]
- Abos Mendizabal, G.; Nuño Solinís, R.; Zaballa González, I. HOBE+, a case study: A virtual community of practice to support innovation in primary care in Basque Public Health Service. BMC Fam. Pract. 2013, 14, 168. [Google Scholar] [CrossRef]
- Landes, S.J.; Smith, B.N.; Weingardt, K.R. Supporting grass roots implementation of an evidence-based psychotherapy through a virtual community of practice: A case example in the Department of Veterans Affairs. Cogn. Behav. Pract. 2019, 26, 453–465. [Google Scholar] [CrossRef]
- Murad, A.; Hyde, N.; Chang, S.; Lederman, R.; Bosua, R.; Pirotta, M.; Audehm, R.; Yates, C.J.; Briggs, A.M.; Gorelik, A.; et al. Quantifying Use of a Health Virtual Community of Practice for General Practitioners’ Continuing Professional Development: A Novel Methodology and Pilot Evaluation. J. Med. Internet Res. 2019, 21, e14545. [Google Scholar] [CrossRef] [PubMed]
- Ting, D.K.; Thoma, B.; Luckett-Gatopoulos, S.; Thomas, A.; Syed, S.; Bravo, M.; Zaver, F.; Purdy, E.; Kwok, E.S.; Chan, T.M. Canadi EM: Accessing a virtual community of practice to create a canadian national medical education institution. AEM Educ. Train. 2019, 3, 86–91. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho-Filho, M.A.; Tio, R.A.; Steinert, Y. Twelve tips for implementing a community of practice for faculty development. Med. Teach. 2020, 42, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.; Korjonen, H.; Keswani, A.; Hughes, E. Virtual communities of practice: Can they support the prevention agenda in public health? Online J. Public Health Inform. 2015, 7, e222. [Google Scholar] [CrossRef]
- Littlewood, N.; Gordon, B.; Department of Health. Digital Health Capability Framework for Health Professionals; 1 Treasury Place: Melbourne, VIC, Australia, 2021. [Google Scholar]
- Australian Digital Health Agency. Australia’s National Digital Health Strategy. Available online: https://www.digitalhealth.gov.au/sites/default/files/2020-11/Australia%27s%20National%20Digital%20Health%20Strategy%20-%20Safe%2C%20seamless%20and%20secure.pdf (accessed on 26 May 2022).
- Australian Digital Health Agency. National Nursing and Midwifery Digital Health Capability Framework. 2020. Available online: https://www.digitalhealth.gov.au/sites/default/files/2020-11/National_Nursing_and_Midwifery_Digital_Health_Capability_Framework_publication.pdf (accessed on 26 May 2022).
- National Health Service. A Health and Digital Care Capabilities Framework. 2018. Available online: https://www.hee.nhs.uk/sites/default/files/documents/Digital%20Literacy%20Capability%20Framework%202018.pdf (accessed on 26 May 2022).
- Morris, M.E.; Webster, K.; Jones, C.; Hill, A.-M.; Haines, T.; McPhail, S.; Kiegaldie, D.; Slade, S.; Jazayeri, D.; Heng, H.; et al. Interventions to reduce falls in hospitals: A systematic review and meta-analysis. Age Ageing 2022, 51, afac077. [Google Scholar] [CrossRef]
| Methods of Recruitment for Participants | Number of Reports 1 |
|---|---|
| 4 | |
| Self-volunteere after hearing about study | 2 |
| Purposive sampling | 1 |
| Hospital survey | 1 |
| Recruited by/via researcher | 1 |
| Actively promoted (e.g., on relevant websites or email banner) | 1 |
| Not stated | 10 |
| Population Description | Number of Reports 1 |
|---|---|
| Allied health clinicians | 12 |
| Specialist physicians | 10 |
| Researchers | 4 |
| GPs | 3 |
| Nurses | 3 |
| Medical students | 2 |
| Healthcare managers | 1 |
| Dentists | 1 |
| Not specifically stated (e.g., ‘primary health care professionals’) and ‘health and social care professionals’ | 4 |
| Technological Infrastructure | Number of Reports 1 |
|---|---|
| Web based/digital platforms (e.g., Web 2.0, Microsoft SharePointWeb) | 14 |
| Videoconferencing (e.g., Adobe Connect, Zoom) | 3 |
| Email (e.g., distribution of newsletter) | 2 |
| Social network sites | 1 |
| Podcasts | 1 |
| Platform not stated, but discusses issues such as ease of use, access, flexibility | 1 |
| Forms of Interaction | Number of Reports 1 |
|---|---|
| Online discussion platforms ( e.g., forum posts, case studies, clinical questions) | 9 |
| Online live discussions (e.g., case-based, clinical questions, hot topics) | 7 |
| Web-based provision of resources | 8 |
| Online meetings | 5 |
| Emails with news/updates/notifications | 5 |
| Provision of recorded meetings | 3 |
| On-line live presentations | 3 |
| YouTube videos/webinars | 2 |
| Blog | 1 |
| Implementation registry | 1 |
| Tele-mentoring | 1 |
| Guest speaker/clinical expert | 1 |
| Podcast | 1 |
| Theoretical Framework | Number of Papers |
|---|---|
| No specific framework | 6 |
| Wenger’s CoP framework | 4 |
| Barnett et al. | 2 |
| Probst and Borzillo | 2 |
| Project ECHO | 2 |
| Theoretical concepts of constructivism, social learning, situated learning | 1 |
| Proposed social framework | 1 |
| Implementation registry | 1 |
| Participatory action research | 1 |
| World shared practices | 1 |
| Developed cluster map | 1 |
| Not applicable | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shaw, L.; Jazayeri, D.; Kiegaldie, D.; Morris, M.E. Implementation of Virtual Communities of Practice in Healthcare to Improve Capability and Capacity: A 10-Year Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 7994. https://doi.org/10.3390/ijerph19137994
Shaw L, Jazayeri D, Kiegaldie D, Morris ME. Implementation of Virtual Communities of Practice in Healthcare to Improve Capability and Capacity: A 10-Year Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(13):7994. https://doi.org/10.3390/ijerph19137994
Chicago/Turabian StyleShaw, Louise, Dana Jazayeri, Debra Kiegaldie, and Meg E. Morris. 2022. "Implementation of Virtual Communities of Practice in Healthcare to Improve Capability and Capacity: A 10-Year Scoping Review" International Journal of Environmental Research and Public Health 19, no. 13: 7994. https://doi.org/10.3390/ijerph19137994
APA StyleShaw, L., Jazayeri, D., Kiegaldie, D., & Morris, M. E. (2022). Implementation of Virtual Communities of Practice in Healthcare to Improve Capability and Capacity: A 10-Year Scoping Review. International Journal of Environmental Research and Public Health, 19(13), 7994. https://doi.org/10.3390/ijerph19137994






