Perceptions of Telehealth Services for Hearing Loss in South Africa’s Public Healthcare System
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Materials for Data Collection
2.3. Procedures
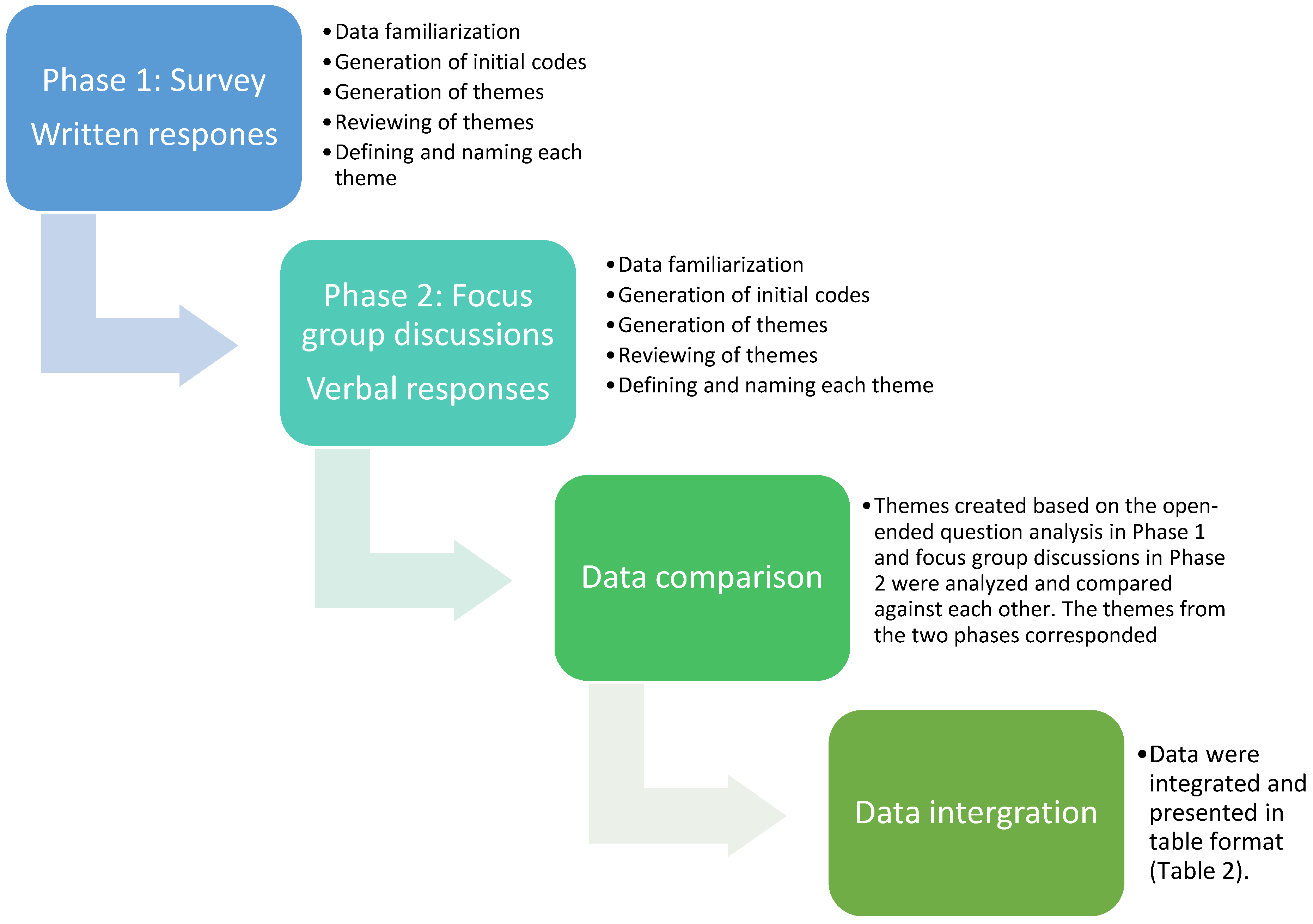
2.4. Data Analysis
3. Results
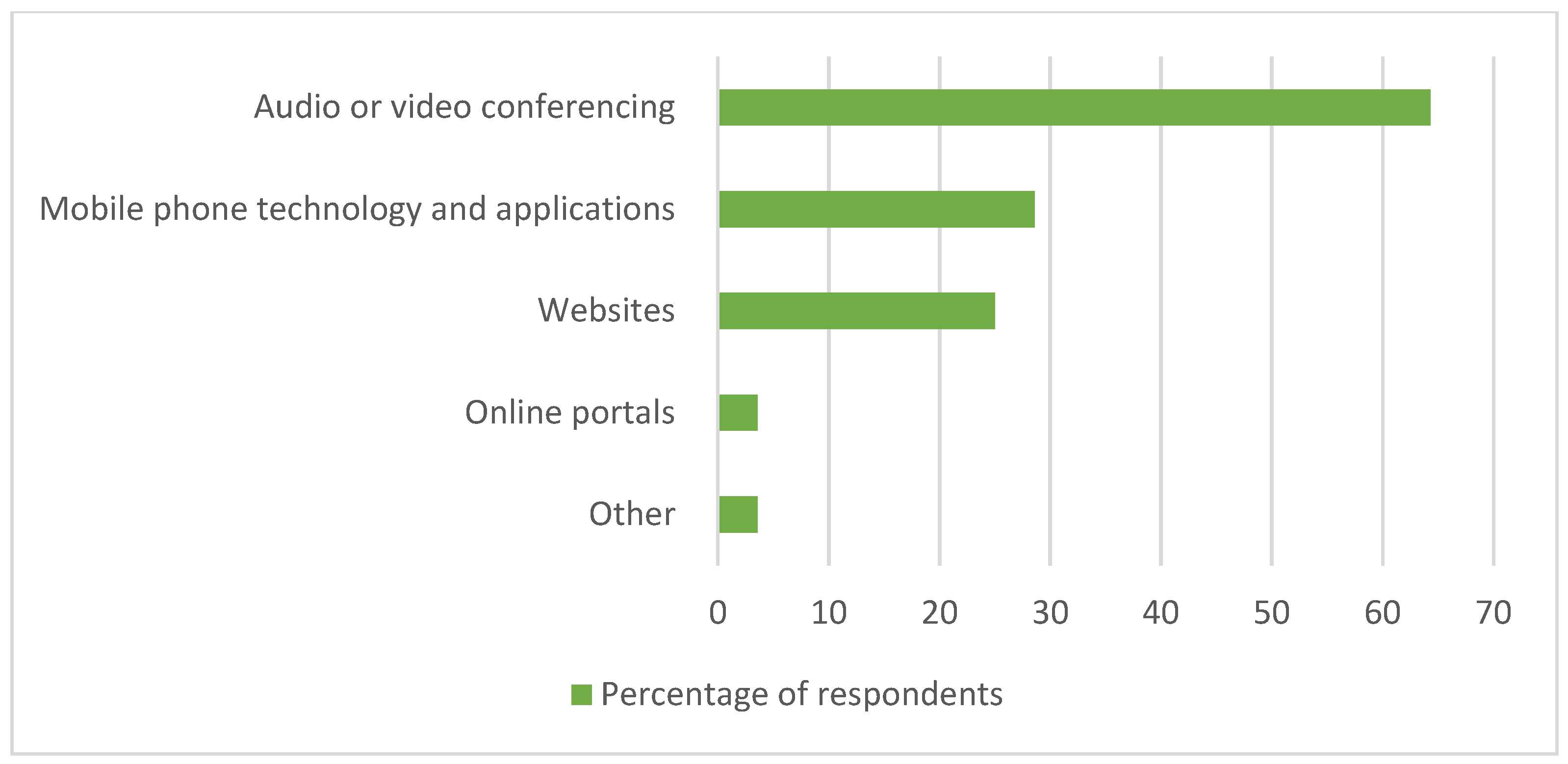
3.1. Quantitative Results
3.2. Qualitative Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Report on Hearing. Available online: https://www.who.int/publications/i/item/world-report-on-hearing (accessed on 21 April 2021).
- Brodie, A.; Smith, B.; Ray, J. The impact of rehabilitation on quality of life after hearing loss: A systematic review. Eur. Arch. Otorhinolaryngol. 2018, 275, 2435–2440. [Google Scholar] [CrossRef] [PubMed]
- Shield, B.; Evaluation of the Social and Economic Costs of Hearing Impairment. A Report for Hear-It. Available online: https://www.hear-it.org/sites/default/files/multimedia/documents/Hear_It_Report_October_2006.pdf (accessed on 2 June 2019).
- Ratanjee-Vanmali, H.; Swanepoel, D.W.; Laplante-Lévesque, A. Characteristics, Behaviours and readiness of persons seeking hearing healthcare online. Int. J. Audiol. 2019, 58, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, D.W.; Le Roux, R. Improving Equitable Access to Hearing Care. Hear. J. 2018, 71, 43. [Google Scholar] [CrossRef]
- World Health Organization. Addressing the Rising Prevalence of Hearing Loss. Available online: https://apps.who.int/iris/bitstream/handle/10665/260336/9789241550260-eng.pdf?sequence=1&ua=1 (accessed on 4 June 2019).
- The Lancet. Hearing loss: An important global health concern. Lancet 2016, 387, 2351. [Google Scholar] [CrossRef]
- Wilson, B.S.; Tucci, D.L.; Merson, M.H.; O’Donoghue, G.M. Global hearing health care: New findings and perspectives. Lancet 2017, 390, 2503–2515. [Google Scholar] [CrossRef]
- Tao, K.F.M.; Moreira, T.d.C.; Jayakody, D.M.P.; Swanepoel, D.W.; Brennan-Jones, C.G.; Coetzee, L.; Eikelboom, R.H. Teleaudiology hearing aid fitting follow-up consultations for adults: Single blinded crossover randomised control trial and cohort studies. Int. J. Audiol. 2021, 60, S49–S60. [Google Scholar] [CrossRef]
- Muñoz, K.; Nagaraj, N.K.; Nichols, N. Applied tele-audiology research in clinical practice during the past decade: A scoping review. Int. J. Audiol. 2020, 60, S4–S12. [Google Scholar] [CrossRef]
- Swanepoel, D.W.; Clark, J.L.; Koekemoer, D.; Hall, J.W., III; Krumm, M.; Ferrari, D.V.; McPherson, B.; Olusanya, B.O.; Mars, M.; Russo, I.; et al. Telehealth in audiology: The need and potential to reach underserved communities. Int. J. Audiol. 2010, 49, 195–202. [Google Scholar] [CrossRef]
- Goulios, H.; Patuzzi, R.B. Audiology education and practice from an international perspective. Int. J. Audiol. 2008, 47, 647–664. [Google Scholar] [CrossRef]
- Mulwafu, W.; Ensink, R.; Kuper, H.; Fagan, J. Survey of ENT services in sub-Saharan Africa: Little progress between 2009 and 2015. Glob. Health Action 2017, 10, 1289736. [Google Scholar] [CrossRef]
- World Health Organization. Multi-Country Assessment of National Capacity. Available online: https://www.who.int/publications/i/item/9789241506571 (accessed on 16 July 2021).
- Swanepoel, D.W. eHealth Technologies Enable more Accessible Hearing Care. Semin. Hear. 2020, 41, 133–140. [Google Scholar] [CrossRef]
- Kamenov, K.; Martinez, R.; Kunjumen, T.; Chadha, S. Ear and Hearing Care Workforce: Current Status and its Implications. Ear Hear. 2021, 42, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Haile, L.M.; Kamenov, K.; Briant, P.S.; Orji, A.U.; Steinmetz, J.D.; Abdoli, A.; Abdollahi, M.; Abu-Gharbieh, E.; Afshin, A.; Ahmed, H.; et al. Hearing loss prevalence and years lived with disability, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet 2021, 397, 996–1009. [Google Scholar] [CrossRef]
- Swanepoel, D.; Clark, J.L. Hearing healthcare in remote or resource-constrained environments. J. Laryngol. Otol. 2019, 133, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.L.; Swanepoel, D.W. Technology for hearing loss—As We Know it, and as We Dream it. Disabil. Rehabil. Assist. Technol. 2014, 9, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, D.W.; Hall, J.W. Making Audiology Work during COVID-19 and beyond. Hear. J. 2020, 73, 20, 22, 23, 24. [Google Scholar] [CrossRef]
- Turolla, A.; Rossettini, G.; Viceconti, A.; Palese, A.; Geri, T. Musculoskeletal Physical Therapy during the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys. Ther. 2020, 100, 1260–1264. [Google Scholar] [CrossRef]
- Eikelboom, R.H.; Bennett, R.J.; Manchaiah, V.; Parmar, B.; Beukes, E.; Rajasingam, S.L.; Swanepoel, D.W. International survey of audiologists during the COVID-19 pandemic: Use of and attitudes to telehealth. Int. J. Audiol. 2022, 61, 283–292. [Google Scholar] [CrossRef]
- Expanding Insurance Coverage of Teleaudiology. Hear. J. 2020, 73, 16. [CrossRef]
- Swanepoel, D.W. New hearing healthcare service-delivery models with connected technologies. ENT Audiol. News 2019, 28, 48–50. [Google Scholar]
- Ratanjee-Vanmali, H.; Swanepoel, D.W.; Laplante-Lévesque, A. Patient uptake, experience, and satisfaction using web-based and face-to-face hearing health services: Process evaluation study. J. Med. Internet Res. 2020, 22, e15875. [Google Scholar] [CrossRef] [PubMed]
- Ravi, R.; Gunjawate, D.R.; Yerraguntla, K.; Driscoll, C. Knowledge and Perceptions of Teleaudiology among Audiologists: A Systematic Review. J. Audiol. Otol. 2018, 22, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Eikelboom, R.H.; Swanepoel, D.W. International Survey of Audiologists’ Attitudes Toward Telehealth. Am. J. Audiol. 2016, 25, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Pichora-Fuller, M.K.; Malkowski, M.; Boretzki, M.; Launer, S. A survey of the attitudes of practitioners toward teleaudiology. Int. J. Audiol. 2014, 53, 850–860. [Google Scholar] [CrossRef]
- Elbeltagy, R.; Waly, E.H.; Bakry, H.M. Teleaudiology practice in COVID-19 pandemic in Egypt and Saudi Arabia. J. Otol. 2022, 17, 78–83. [Google Scholar] [CrossRef]
- Zaitoun, M.; Alqudah, S.; Al Mohammad, H. Audiology practice during COVID-19 crisis in Jordan and Arab countries. Int. J. Audiol. 2022, 61, 21–28. [Google Scholar] [CrossRef]
- Saunders, G.H.; Roughley, A. Audiology in the time of COVID-19: Practices and opinions of audiologists in the UK. Int. J. Audiol. 2021, 60, 255–262. [Google Scholar] [CrossRef]
- Mayosi, B.M.; Benatar, S.R. Health and Health Care in South Africa—20 Years after Mandela. N. Engl. J. Med. 2014, 371, 1344–1353. [Google Scholar] [CrossRef]
- Pillay, M.; Tiwari, R.; Kathard, H.; Chikte, U. Sustainable workforce: South African Audiologists and Speech Therapists. Hum. Resour. Health 2020, 18, 47. [Google Scholar] [CrossRef]
- South African Department of Health Regulations relating to categories of hospitals. Gov. Gaz. 2012, 185, 3–28. [CrossRef]
- Yusoff, M.S.B. ABC of Content Validation and Content Validity Index Calculation. Educ. Med. J. 2019, 11, 49–54. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Hutcheson, G. The Multivariate Social Scientist; SAGE Publications, Ltd.: London, UK, 1999; ISBN 9780761952015. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2018; ISBN 1526419513/9781526419514. [Google Scholar]
- Darusalam, G. Kesahan dan Kebolehpercayaan Dalam Kajian Kuantitatif dan Kualitatif. J. Inst. Perguran Islam 2008, 61–82. [Google Scholar]
- van Griethuijsen, R.A.L.F.; van Eijck, M.W.; Haste, H.; den Brok, P.J.; Skinner, N.C.; Mansour, N.; Savran Gencer, A.; BouJaoude, S. Global Patterns in Students’ Views of Science and Interest in Science. Res. Sci. Educ. 2015, 45, 581–603. [Google Scholar] [CrossRef]
- Zhan, Z.; Wei, Q.; Hong, J.-C. Cellphone addiction during the COVID-19 outbreak: How online social anxiety and cyber danger belief mediate the influence of personality. Comput. Human Behav. 2021, 121, 106790. [Google Scholar] [CrossRef]
- Bonett, D.G. Sample Size Requirements for Testing and Estimating Coefficient Alpha. J. Educ. Behav. Stat. 2002, 27, 335–340. [Google Scholar] [CrossRef]
- Byrne, D. A worked example of Braun and Clarke’s approach to reflexive thematic analysis. Qual. Quant. 2022, 56, 1391–1412. [Google Scholar] [CrossRef]
- Parmar, B.; Beukes, E.; Rajasingam, S. The impact of COVID-19 on provision of UK audiology services & on attitudes towards delivery of telehealth services. Int. J. Audiol. 2022, 61, 228–238. [Google Scholar] [CrossRef]
- Kerr, G.; Tuomi, S.; Müller, A. Costs involved in using a cochlear implant in South Africa. S. Afr. J. Commun. Disord. 2012, 59, 16–26. [Google Scholar] [CrossRef][Green Version]
- Bhamjee, A.; le Roux, T.; Schlemmer, K.; Graham, M.; Mahomed-asmail, F. Audiologists’ perceptions of hearing healthcare resources and services in South Africa’s public healthcare system. Heal. Serv. Insights 2022. submitted. [Google Scholar] [CrossRef]
- Theunissen, M.; Swanepoel, D. Early hearing detection and intervention services in the public health sector in South Africa. Int. J. Audiol. 2008, 47, S23–S29. [Google Scholar] [CrossRef] [PubMed]
- Bush, M.L.; Thompson, R.; Irungu, C.; Ayugi, J. The Role of Telemedicine in Auditory Rehabilitation. Otol. Neurotol. 2016, 37, 1466–1474. [Google Scholar] [CrossRef] [PubMed]
- Ratanjee-Vanmali, H.; Swanepoel, D.W.; Laplante-Lévesque, A. Digital proficiency is not a significant barrier for taking up hearing services with a hybrid online and face-to-face model. Am. J. Audiol. 2020, 29, 785–808. [Google Scholar] [CrossRef]
- Mcintyre, D.; Ataguba, J. Access to Quality Health Care in South Africa: Is the Health Sector Contributing to Addressing the Inequality Challenge? Available online: https://www.parliament.gov.za/storage/app/media/Pages/2017/october/High_Level_Panel/Commissioned_reports_for_triple_challenges_of_poverty_unemployment_and_inequality/Diagnostic_Report_on_Access_to_Quality_Healthcare.pdf (accessed on 30 March 2022).
- Gladden, C.; Beck, L.; Chandler, D. Tele-audiology: Expanding Access to Hearing Care and Enhancing Patient Connectivity. J. Am. Acad. Audiol. 2015, 26, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Statista Smartphone Users in South Africa 2014–2023. Available online: https://www.statista.com/statistics/488376/forecast-of-smartphone-users-in-south-africa/ (accessed on 15 February 2021).
- Wallace, K. Audiologist’s Role in Promoting Tech Literacy. Hear. J. 2020, 73, 44–45. [Google Scholar] [CrossRef]
- Krumm, M. A Review of Contemporary Tele-Audiology Literature. J. Hear. Sci. 2016, 6, 9–21. [Google Scholar] [CrossRef]
- Kim, J.; Jeon, S.; Kim, D.; Shin, Y. A Review of Contemporary Teleaudiology: Literature Review, Technology, and Considerations for Practicing. J. Audiol. Otol. 2021, 25, 1–7. [Google Scholar] [CrossRef]
- Coco, L. Teleaudiology: Strategies, Considerations during a Crisis and Beyond. Hear. J. 2020, 73, 26, 28, 29. [Google Scholar] [CrossRef]
- Koen, B.; Loosveldt, G.; Vandenplas, C.; Stoop, I. Response rates in the European Social Survey: Increasing, decreasing, or a matter of fieldwork efforts? Surv. Methods Insights Field 2018, 1–12. [Google Scholar] [CrossRef]
- De Koning, R.; Egiz, A.; Kotecha, J.; Ciuculete, A.C.; Ooi, S.Z.Y.; Bankole, N.D.A.; Erhabor, J.; Higginbotham, G.; Khan, M.; Dalle, D.U.; et al. Survey Fatigue during the COVID-19 Pandemic: An Analysis of Neurosurgery Survey Response Rates. Front. Surg. 2021, 8, 690680. [Google Scholar] [CrossRef]
- Guest, G.; Namey, E.; McKenna, K. How Many Focus Groups Are Enough? Building an Evidence Base for Nonprobability Sample Sizes. Field Methods 2017, 29, 3–22. [Google Scholar] [CrossRef]
- Knudsen, L.V.; Laplante-Lévesque, A.; Jones, L.; Preminger, J.E.; Nielsen, C.; Lunner, T.; Hickson, L.; Naylor, G.; Kramer, S.E. Conducting qualitative research in audiology: A tutorial. Int. J. Audiol. 2012, 51, 83–92. [Google Scholar] [CrossRef] [PubMed]

| Telehealth use by audiologists | % (n) |
| Unaware of what telehealth entails | 8.2 (8) |
| Not willing to use telehealth | 2.1 (2) |
| Willing, but no resources | 74.2 (72) |
| Using telehealth, and it is effective | 8.2 (8) |
| Other | 7.2 (7) |
| Use of telehealth services pre-COVID-19 setting | % (n) |
| No | 87.6 (85) |
| Yes | 7.2 (7) |
| Unsure | 5.2 (5) |
| Use of telehealth services currently (during COVID-19 setting) | % (n) |
| No | 71.1 (69) |
| Yes | 19.6 (19) |
| Unsure | 9.3 (9) |
| Willingness to use telehealth services * | % (n) |
| No | 6.4 (4) |
| Yes | 84.1 (53) |
| Unsure | 9.5 (6) |
| Themes and Sub-Themes | Description | Illustrative Examples |
|---|---|---|
| 1. Clinical practices | ||
| Limitations of remote hearing healthcare | Not applicable to all populations; hearing loss and language barriers affect telehealth communication. | ‘Certain information is better understood by physical contact rather than electronic contact. Patients with multiple disabilities may struggle even further.’ ‘Hearing loss and language barriers through telephones and other technology can hamper ability to communicate.’ |
| Impersonal nature; negative impact on patient relationship. | ‘In a field like Audiology, where patients’ main difficulty is hearing, it may be difficult to impossible to get messages across to them effectively.’ | |
| Quality of service and audiologists’ preferences for face-to-face consultations. | ‘For me, even if the infrastructure is in place, I am not really in favour of telehealth. I prefer to render quality face to face interaction types of services and feel that this can’t be replaced by telehealth.’ | |
| Limitations of South Africa’s public healthcare setting | Limitations and challenges in the healthcare system question the feasibility and the viability of telehealth within this setting. | ‘Public health institutions, especially at primary healthcare level and those in rural areas are also too poorly equipped to be able to effectively provide these services. Telehealth in South Africa’s public health system thus faces large barriers to be successfully implemented at this time.’ |
| Policy and protocol | Lack of policies, protocols, and guidelines to guide the use of telehealth. | ‘My concern is with the record-keeping. When patients come in for an appointment, I know the procedure. With telehealth, there are no clear guidelines. Also, there are no protocols to distinguish when to use what form of telehealth and no guidelines.’ |
| Knowledge and training | Increased telehealth training needed for audiologists; knowledge and training to hospital management and policymakers; promotion and awareness of telehealth services. | ‘The telehealth system is grossly underdeveloped and requires additional training by all healthcare workers.’ ‘If leaders and those in power can be educated about telehealth, it can be easier to have access to equipment necessary for telehealth.’ ‘There is a lack of public awareness and understanding of the potential benefits of telehealth’. |
| 2. Hearing healthcare resources | ||
| Information systems and technology | Lack of IT and software support required, including limited or no access to the internet at hospitals. | ‘Telehealth services are a great challenge in low resourced hospitals or rural communities. Thus, access to reliable internet and coverage remains the greatest barrier to achieving telehealth services.’ |
| Equipment and infrastructure | Lack of equipment and infrastructural resources. | ‘Unfortunately, the public health system hasn’t really invested in procurement of equipment which is telehealth compatible.’ |
| Human resources | Shortage of audiology staff in many of the South African public sector hospitals. | ‘In government, we know that the organogram is constantly changing, posts are frozen if therapists leave, and new therapists are seldom hired, so the staffing, in addition to the hospital’s infrastructure, is a big challenge to telehealth.’ |
| 3. Patient restrictions impacting hearing healthcare | ||
| Financial resources | Many patients are unable to afford the resources required to access telehealth services. | ‘South Africa’s public healthcare system is largely used by people from poor socio-economic backgrounds, and thus unable to access the technology required to receive telehealth services.’ |
| Education | High percentage of uneducated and/ or illiterate patients receive public healthcare sector services. | ‘A majority of our patients are not educated, thus making the use of teleaudiology almost impossible.’ ‘Most patients are from very poor backgrounds and are illiterate.’ |
| Employment | Employment status impacts patients’ ability to access telehealth services. | ‘Most patients served in public are unemployed.’ |
| 4. Perceived benefits of telehealth | ||
| Accessibility to services | Increased accessibility of cost-efficient and time-efficient audiology services to a broader population,-eliminating transport and travelling costs; the convenience of telehealth for patients and audiologists. | ‘I believe telehealth has the potential to bridge the access gap for patients, particularly those living in rural areas who have limited access to hearing health professionals.’ ‘For me, the biggest advantage is the convenience. The convenience for ourselves as well as our patients. It means that reduces their travel time and a whole lot of anxiety.’ |
| COVID-19 pandemic | Current COVID-19 pandemic highlights the usefulness and the value of telehealth services as a means of infection control and minimizing the risk of contact. | ‘Telehealth services is a viable solution considering the pandemic’ ‘It would assist a lot, especially during this pandemic (to reduce infection).’ |
| Potential and willingness to use | Recognition of potential use of telehealth and willingness to use it; the need to adapt and to modify telehealth practices according to available resources. | ‘Telehealth requires adaption. Many might display hesitation, but we need to keep up and ‘go with the flow’ in an ethical way using evidence-based practices for telehealth.’ ‘I believe that telehealth has the ability to work well in the public sector.’ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhamjee, A.; le Roux, T.; Swanepoel, D.W.; Graham, M.A.; Schlemmer, K.; Mahomed-Asmail, F. Perceptions of Telehealth Services for Hearing Loss in South Africa’s Public Healthcare System. Int. J. Environ. Res. Public Health 2022, 19, 7780. https://doi.org/10.3390/ijerph19137780
Bhamjee A, le Roux T, Swanepoel DW, Graham MA, Schlemmer K, Mahomed-Asmail F. Perceptions of Telehealth Services for Hearing Loss in South Africa’s Public Healthcare System. International Journal of Environmental Research and Public Health. 2022; 19(13):7780. https://doi.org/10.3390/ijerph19137780
Chicago/Turabian StyleBhamjee, Aaqilah, Talita le Roux, De Wet Swanepoel, Marien Alet Graham, Kurt Schlemmer, and Faheema Mahomed-Asmail. 2022. "Perceptions of Telehealth Services for Hearing Loss in South Africa’s Public Healthcare System" International Journal of Environmental Research and Public Health 19, no. 13: 7780. https://doi.org/10.3390/ijerph19137780
APA StyleBhamjee, A., le Roux, T., Swanepoel, D. W., Graham, M. A., Schlemmer, K., & Mahomed-Asmail, F. (2022). Perceptions of Telehealth Services for Hearing Loss in South Africa’s Public Healthcare System. International Journal of Environmental Research and Public Health, 19(13), 7780. https://doi.org/10.3390/ijerph19137780






