Behavioral Intention and Its Predictors toward COVID-19 Booster Vaccination among Chinese Parents: Applying Two Behavioral Theories
Abstract
:1. Introduction
2. Materials and Methods
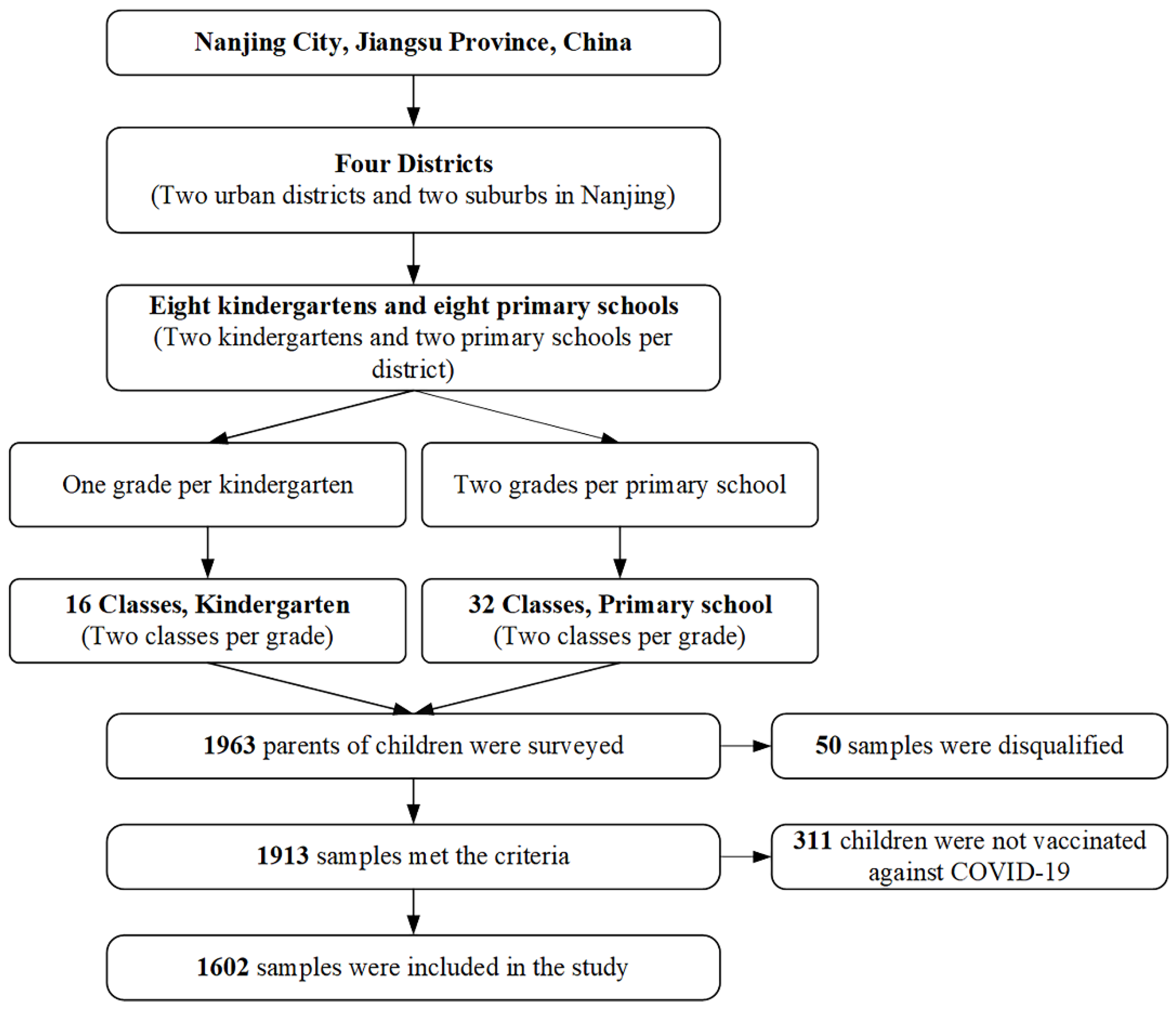
2.1. Data Collection
2.2. Questionnaire Design
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics and Other Intention-Related Factors
3.2. Parents’ Psychological Perception
3.3. Parents’ Intentions Regarding Booster Vaccination in Children
3.4. Univariate and Multivariate Analysis of Intention and Psychological Perceptions
3.5. Covariates-Adjusted Multivariate Analysis of Intention and Psychological Perceptions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The Lancet Infectious Diseases. The intersection of COVID-19 and mental health. Lancet. Infect. Dis. 2020, 20, 1217. [Google Scholar] [CrossRef]
- Mehta, N.S.; Mytton, O.T.; Mullins, E.W.S.; Fowler, T.A.; Falconer, C.L.; Murphy, O.B.; Langenberg, C.; Jayatunga, W.J.P.; Eddy, D.H.; Nguyen-Van-Tam, J.S. SARS-CoV-2 (COVID-19): What Do We Know About Children? A Systematic Review. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 2469–2479. [Google Scholar] [CrossRef] [PubMed]
- Ladhani, S.N.; Amin-Chowdhury, Z.; Davies, H.G.; Aiano, F.; Hayden, I.; Lacy, J.; Sinnathamby, M.; de Lusignan, S.; Demirjian, A.; Whittaker, H.; et al. COVID-19 in children: Analysis of the first pandemic peak in England. Arch. Dis. Child. 2020, 105, 1180–1185. [Google Scholar] [CrossRef] [PubMed]
- CDC COVID-19 Response Team. Coronavirus Disease 2019 in Children—United States, February 12–April 2, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 422–426. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Korean Society of Infectious Diseases. Report on the Epidemiological Features of Coronavirus Disease 2019 (COVID-19) Outbreak in the Republic of Korea from January 19 to March 2, 2020. J. Korean Med. Sci. 2020, 35, e112. [Google Scholar] [CrossRef]
- Snape, M.D.; Viner, R.M. COVID-19 in children and young people. Science 2020, 370, 286–288. [Google Scholar] [CrossRef]
- Frederiksen, L.S.F.; Zhang, Y.; Foged, C.; Thakur, A. The Long Road Toward COVID-19 Herd Immunity: Vaccine Platform Technologies and Mass Immunization Strategies. Front. Immunol. 2020, 11, 1817. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 22 February 2022).
- National Health Commission of the People’s Republic of China. Questions and Answer on COVID-19 Vaccination for People Aged 3–11 Years Old. Available online: http://www.nhc.gov.cn/xcs/yqfkdt/202111/79103c66c2de404b8e50583816f5e31e.shtml (accessed on 23 March 2022).
- Xia, S.; Zhang, Y.; Wang, Y.; Wang, H.; Yang, Y.; Gao, G.F.; Tan, W.; Wu, G.; Xu, M.; Lou, Z.; et al. Safety and immunogenicity of an inactivated COVID-19 vaccine, BBIBP-CorV, in people younger than 18 years: A randomised, double-blind, controlled, phase 1/2 trial. Lancet Infect. Dis. 2022, 22, 196–208. [Google Scholar] [CrossRef]
- Han, B.; Song, Y.; Li, C.; Yang, W.; Ma, Q.; Jiang, Z.; Li, M.; Lian, X.; Jiao, W.; Wang, L.; et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: A double-blind, randomised, controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2021, 21, 1645–1653. [Google Scholar] [CrossRef]
- Hause, A.M.; Baggs, J.; Marquez, P.; Myers, T.R.; Gee, J.; Su, J.R.; Zhang, B.; Thompson, D.; Shimabukuro, T.T.; Shay, D.K. COVID-19 Vaccine Safety in Children Aged 5–11 Years—United States, November 3–December 19, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1755–1760. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, Y.; Mandel, M.; Bar-On, Y.M.; Bodenheimer, O.; Freedman, L.; Haas, E.J.; Milo, R.; Alroy-Preis, S.; Ash, N.; Huppert, A. Waning Immunity after the BNT162b2 Vaccine in Israel. N. Engl. J. Med. 2021, 385, e85. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, B.; Lotan, R.; Kalkstein, N.; Peretz, A.; Perez, G.; Ben-Tov, A.; Chodick, G.; Gazit, S.; Patalon, T. Correlation of SARS-CoV-2-breakthrough infections to time-from-vaccine. Nat. Commun. 2021, 12, 6379. [Google Scholar] [CrossRef]
- Bar-On, Y.M.; Goldberg, Y.; Mandel, M.; Bodenheimer, O.; Freedman, L.; Kalkstein, N.; Mizrahi, B.; Alroy-Preis, S.; Ash, N.; Milo, R.; et al. Protection of BNT162b2 Vaccine Booster against COVID-19 in Israel. N. Engl. J. Med. 2021, 385, 1393–1400. [Google Scholar] [CrossRef] [PubMed]
- Hause, A.M.; Baggs, J.; Marquez, P.; Myers, T.R.; Su, J.R.; Blanc, P.G.; Gwira Baumblatt, J.A.; Woo, E.J.; Gee, J.; Shimabukuro, T.T.; et al. Safety Monitoring of COVID-19 Vaccine Booster Doses Among Adults—United States, September 22, 2021–February 6, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Mattiuzzi, C.; Lippi, G. Efficacy of COVID-19 vaccine booster doses in older people. Eur. Geriatr. Med. 2022, 13, 275–278. [Google Scholar] [CrossRef]
- Israeli Ministry of Health. The Vaccination Committee Recommends: 3 Weeks between the First and Second Dose also for Children 5–11. Available online: https://www.gov.il/en/Departments/news/21112021-04 (accessed on 25 March 2022).
- Alfieri, N.L.; Kusma, J.D.; Heard-Garris, N.; Davis, M.M.; Golbeck, E.; Barrera, L.; Macy, M.L. Parental COVID-19 vaccine hesitancy for children: Vulnerability in an urban hotspot. BMC Public Health 2021, 21, 1662. [Google Scholar] [CrossRef]
- Horiuchi, S.; Sakamoto, H.; Abe, S.K.; Shinohara, R.; Kushima, M.; Otawa, S.; Yui, H.; Akiyama, Y.; Ooka, T.; Kojima, R.; et al. Factors of parental COVID-19 vaccine hesitancy: A cross sectional study in Japan. PLoS ONE 2021, 16, e0261121. [Google Scholar] [CrossRef]
- Wang, Q.; Xiu, S.; Zhao, S.; Wang, J.; Han, Y.; Dong, S.; Huang, J.; Cui, T.; Yang, L.; Shi, N.; et al. Vaccine Hesitancy: COVID-19 and Influenza Vaccine Willingness among Parents in Wuxi, China-A Cross-Sectional Study. Vaccines 2021, 9, 342. [Google Scholar] [CrossRef]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Parra Cotanda, C.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L.; et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, R.; Zhou, Z.; Fan, J.; Liang, J.; Cai, L.; Peng, L.; Ren, F.; Lin, W. Parental psychological distress and attitudes towards COVID-19 vaccination: A cross-sectional survey in Shenzhen, China. J. Affect. Disord. 2021, 292, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Prestwich, A.; Webb, T.L.; Conner, M. Using theory to develop and test interventions to promote changes in health behaviour: Evidence, issues, and recommendations. Curr. Opin. Psychol. 2015, 5, 1–5. [Google Scholar] [CrossRef]
- Ghaffari, M.; Rakhshandehrou, S.; Tezval, J.; Harooni, J.; Armoon, B. Skin cancer-related coping appraisal among farmers of rural areas: Applying protection motivation theory. J. Cosmet. Dermatol. 2019, 18, 1830–1836. [Google Scholar] [CrossRef]
- Taheri-Kharameh, Z.; Bashirian, S.; Heidarimoghadam, R.; Poorolajal, J.; Barati, M.; Rásky, É. Predictors of Fall Protective Behaviors among Iranian Community-Dwelling Older Adults: An Application of the Protection Motivation Theory. Clin. Interv. Aging 2020, 15, 123–129. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.Y.; Broström, A.; Årestedt, K.; Mårtensson, J.; Steinke, E.E.; Pakpour, A.H. Using extended theory of planned behavior to determine factors associated with help-seeking behavior of sexual problems in women with heart failure: A longitudinal study. J. Psychosom. Obstet. Gynaecol. 2020, 41, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Ling, M.; Kothe, E.J.; Mullan, B.A. Predicting intention to receive a seasonal influenza vaccination using Protection Motivation Theory. Soc. Sci. Med. 2019, 233, 87–92. [Google Scholar] [CrossRef] [Green Version]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef]
- Maddux, J.E.; Rogers, R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. J. Exp. Soc. Psychol. 1983, 19, 469–479. [Google Scholar] [CrossRef]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior; Kuhl, J., Beckmann, J., Eds.; Action Control. SSSP Springer Series in Social Psychology; Springer: Berlin/Heidelberg, Germany, 1985; pp. 11–39. [Google Scholar] [CrossRef]
- Huang, P.C.; Hung, C.H.; Kuo, Y.J.; Chen, Y.P.; Ahorsu, D.K.; Yen, C.F.; Lin, C.Y.; Griffiths, M.D.; Pakpour, A.H. Expanding Protection Motivation Theory to Explain Willingness of COVID-19 Vaccination Uptake among Taiwanese University Students. Vaccines 2021, 9, 1046. [Google Scholar] [CrossRef]
- Wang, P.W.; Ahorsu, D.K.; Lin, C.Y.; Chen, I.H.; Yen, C.F.; Kuo, Y.J.; Griffiths, M.D.; Pakpour, A.H. Motivation to Have COVID-19 Vaccination Explained Using an Extended Protection Motivation Theory among University Students in China: The Role of Information Sources. Vaccines 2021, 9, 380. [Google Scholar] [CrossRef]
- Fan, C.W.; Chen, I.H.; Ko, N.Y.; Yen, C.F.; Lin, C.Y.; Griffiths, M.D.; Pakpour, A.H. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Hum. Vaccin. Immunother. 2021, 17, 3413–3420. [Google Scholar] [CrossRef]
- Guidry, J.P.D.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control 2021, 49, 137–142. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross-Sectional Online Survey. JMIR Pediatr. Parent. 2020, 3, e24827. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression; John Wiley & Sons: New York, NY, USA, 2000. [Google Scholar]
- Wan, X.; Huang, H.; Shang, J.; Xie, Z.; Jia, R.; Lu, G.; Chen, C. Willingness and influential factors of parents of 3-6-year-old children to vaccinate their children with the COVID-19 vaccine in China. Hum. Vaccin. Immunother. 2021, 17, 3969–3974. [Google Scholar] [CrossRef]
- Wang, X.X.; Liu, L.Y.; Pei, M.Y.; Li, X.G.; Li, N. Willingness of the General Public to Receive A COVID-19 Vaccine Booster—China, April–May 2021. China CDC Wkly. 2022, 4, 66–70. [Google Scholar] [CrossRef]
- Wu, F.; Yuan, Y.; Deng, Z.; Yin, D.; Shen, Q.; Zeng, J.; Xie, Y.; Xu, M.; Yang, M.; Jiang, S.; et al. Acceptance of COVID-19 booster vaccination based on the protection motivation theory: A cross-sectional study in China. J. Med. Virol. 2022. [Google Scholar] [CrossRef]
- Yadete, T.; Batra, K.; Netski, D.M.; Antonio, S.; Patros, M.J.; Bester, J.C. Assessing Acceptability of COVID-19 Vaccine Booster Dose among Adult Americans: A Cross-Sectional Study. Vaccines 2021, 9, 1424. [Google Scholar] [CrossRef]
- Godeau, D.; Petit, A.; Richard, I.; Roquelaure, Y.; Descatha, A. Return-to-work, disabilities and occupational health in the age of COVID-19. Scand. J. Work. Environ. Health 2021, 47, 408–409. [Google Scholar] [CrossRef]
- Jiangsu Commission of Health. Eighty Percent of the Permanent Residents Have Received Full COVID-19 Vaccination in Jiangsu Province. Available online: http://wjw.jiangsu.gov.cn/art/2021/11/18/art_81791_10118132.html (accessed on 28 March 2022).
- Li, L.; Wang, J.; Nicholas, S.; Maitland, E.; Leng, A.; Liu, R. The Intention to Receive the COVID-19 Vaccine in China: Insights from Protection Motivation Theory. Vaccines 2021, 9, 445. [Google Scholar] [CrossRef]
- Xiao, Q.; Liu, X.; Wang, R.; Mao, Y.; Chen, H.; Li, X.; Liu, X.; Dai, J.; Gao, J.; Fu, H.; et al. Predictors of Willingness to Receive the COVID-19 Vaccine after Emergency Use Authorization: The Role of Coping Appraisal. Vaccines 2021, 9, 967. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatric Infect. Dis. J. 2021, 40, e134–e136. [Google Scholar] [CrossRef]
- Pastorino, R.; Villani, L.; Mariani, M.; Ricciardi, W.; Graffigna, G.; Boccia, S. Impact of COVID-19 Pandemic on Flu and COVID-19 Vaccination Intentions among University Students. Vaccines 2021, 9, 70. [Google Scholar] [CrossRef]
- Eberhardt, J.; Ling, J. Predicting COVID-19 vaccination intention using protection motivation theory and conspiracy beliefs. Vaccine 2021, 39, 6269–6275. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Xiao, X.; Wong, R.M. Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine 2020, 38, 5131–5138. [Google Scholar] [CrossRef]
- Hayashi, Y.; Romanowich, P.; Hantula, D.A. Predicting Intention to Take a COVID-19 Vaccine in the United States: Application and Extension of Theory of Planned Behavior. Am. J. Health Promot. AJHP 2022, 36, 710–713. [Google Scholar] [CrossRef]
- Hagger, M.S.; Hamilton, K. Predicting COVID-19 booster vaccine intentions. Appl. Psychol. Health Well-Being 2022, 14, 1–23. [Google Scholar] [CrossRef]
| Variables | Number (n)/M(Q) | Percentage (%) |
|---|---|---|
| Demographic characteristics of parents | ||
| Parents’ age (years) a | 32.0 (34.0, 35.0) | |
| below 34 | 673 | 42.0 |
| 34 and above | 929 | 58.0 |
| Type of participants | ||
| Father or other parent | 386 | 24.1 |
| Mother | 1216 | 75.9 |
| Education | ||
| College or below | 686 | 42.8 |
| College and above | 916 | 57.2 |
| Residence | ||
| Urban | 211 | 13.2 |
| Rural | 1391 | 86.8 |
| Marital status | ||
| Unmarried, divorced, widowed | 65 | 4.1 |
| Married | 1537 | 95.9 |
| Per capita monthly income (RMB) b | ||
| Less than RMB 15,000 | 1073 | 67.0 |
| RMB 15,000 and above | 529 | 33.0 |
| Demographic characteristics of children | ||
| Children’s age (years) c | 7.0 (6.0, 8.0) | |
| 7 years and below | 972 | 60.7 |
| 8 years and older | 630 | 39.3 |
| Whether is the single-child family | ||
| No | 707 | 44.1 |
| Yes | 895 | 55.9 |
| Gender | ||
| Boy | 837 | 52.2 |
| Girl | 765 | 47.8 |
| Other intention related factors | ||
| Family member had been quarantined due to COVID-19 containment | ||
| No | 1510 | 94.3 |
| Yes | 92 | 5.7 |
| Family member had been infected with COVID-19 | ||
| No | 1599 | 99.8 |
| Yes | 3 | 0.2 |
| Family member had been involved in COVID-19 prevention and control efforts | ||
| No | 1308 | 81.6 |
| Yes | 294 | 18.4 |
| Parents’ COVID-19 vaccinations | ||
| Vaccinated three doses | 440 | 27.5 |
| Vaccinated two doses | 1079 | 67.4 |
| Vaccinated one dose | 29 | 1.8 |
| Not vaccinated | 54 | 3.4 |
| This child had been vaccinated against self-funded vaccines (e.g., influenza vaccine, chickenpox vaccine, hand-foot-and-mouth disease vaccine, etc.) | ||
| No | 597 | 37.3 |
| Yes | 1005 | 62.7 |
| Health status of child | ||
| Good and below | 215 | 13.4 |
| healthy | 1387 | 86.6 |
| This child had respiratory or gastrointestinal issues in the last month | ||
| No | 1334 | 83.3 |
| Yes | 268 | 16.7 |
| This child had an allergy history | ||
| No | 1355 | 84.6 |
| Yes | 247 | 15.4 |
| This child had any contraindication to the COVID-19 vaccine | ||
| No | 1389 | 86.7 |
| Yes/Unclear | 213 | 13.3 |
| Child’s COVID-19 vaccinations | ||
| Vaccinated two doses | 1176 | 73.4 |
| Vaccinated one dose | 426 | 26.6 |
| Variables | Number (n) | Percentage (%) |
|---|---|---|
| PMT factors | ||
| Severity | ||
| No | 188 | 11.7 |
| Yes | 1414 | 88.3 |
| Susceptibility | ||
| No | 605 | 37.8 |
| Yes | 997 | 62.2 |
| Response efficacy | ||
| No | 280 | 17.5 |
| Yes | 1322 | 82.5 |
| Self-efficacy | ||
| No | 225 | 14.0 |
| Yes | 1377 | 86.0 |
| Response cost | ||
| No | 1199 | 74.8 |
| Yes | 403 | 25.2 |
| TPB factors | ||
| Attitude | ||
| No | 214 | 13.4 |
| Yes | 1388 | 86.6 |
| Subjective norms | ||
| No | 483 | 30.1 |
| Yes | 1119 | 69.9 |
| Behavioral control | ||
| No | 302 | 18.9 |
| Yes | 1300 | 81.1 |
| Variables | Number (n) | Percentage (%) |
|---|---|---|
| Having intention to get your child a booster vaccination | ||
| Absolutely disagree | 37 | 2.3 |
| Disagree | 34 | 2.1 |
| Neutrality | 229 | 14.3 |
| agree | 670 | 41.8 |
| Absolutely agree | 632 | 39.5 |
| Having intention to actively respond to advocacy on booster vaccination for children | ||
| Absolutely disagree | 33 | 2.1 |
| Disagree | 24 | 1.5 |
| Neutrality | 224 | 14.0 |
| agree | 677 | 42.3 |
| Absolutely agree | 644 | 40.2 |
| Having intention to actively follow up information on booster vaccination for children | ||
| Absolutely disagree | 37 | 2.3 |
| Disagree | 11 | 0.7 |
| Neutrality | 164 | 10.2 |
| agree | 702 | 43.8 |
| Absolutely agree | 688 | 42.9 |
| Having intention to proactively learn the process of booster vaccination in children | ||
| Absolutely disagree | 34 | 2.1 |
| Disagree | 13 | 0.8 |
| Neutrality | 162 | 10.1 |
| agree | 702 | 43.8 |
| Absolutely agree | 691 | 43.1 |
| Having intention to proactively understand the precautions for children after vaccination for booster needle | ||
| Absolutely disagree | 35 | 2.2 |
| Disagree | 10 | 0.6 |
| Neutrality | 139 | 8.7 |
| agree | 683 | 42.6 |
| Absolutely agree | 735 | 45.9 |
| Intention a | ||
| Yes | 1398 | 87.3 |
| No | 204 | 12.7 |
| Variables | Intention n (%) | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|---|
| No | Yes | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Severity | ||||||
| No | 32 (17.0) | 156 (83.0) | 1 | 0.061 | 1 | 0.154 |
| Yes | 172 (12.2) | 1242 (87.8) | 1.481 (0.981, 2.237) | 0.683 (0.405, 1.154) | ||
| Susceptibility | ||||||
| No | 108 (17.9) | 497 (82.1) | 1 | <0.001 | 1 | 0.858 |
| Yes | 96 (9.6) | 901 (90.4) | 2.039 (1.517, 2.742) | 0.963 (0.642, 1.447) | ||
| Response efficacy | ||||||
| No | 107 (38.2) | 173 (61.8) | 1 | <0.001 | 1 | 0.001 |
| Yes | 97 (7.3) | 1225 (92.7) | 7.811 (5.686, 10.730) | 2.246 (1.391, 3.627) | ||
| Self-efficacy | ||||||
| No | 87 (38.7) | 138 (61.3) | 1 | <0.001 | 1 | 0.336 |
| Yes | 117 (8.5) | 1260 (91.5) | 6.789 (4.889, 9.429) | 1.282 (0.773, 2.125) | ||
| Response cost | ||||||
| No | 149 (12.4) | 1050 (87.6) | 1 | 0.525 | 1 | 0.001 |
| Yes | 55 (13.6) | 348 (86.4) | 0.898 (0.644, 1.252) | 0.515 (0.345, 0.771) | ||
| Attitude | ||||||
| No | 102 (47.7) | 112 (52.3) | 1 | <0.001 | 1 | 0.001 |
| Yes | 102 (7.3) | 1286 (92.7) | 11.482 (8.209, 16.061) | 2.415 (1.407, 4.147) | ||
| Subjective norms | ||||||
| No | 128 (26.5) | 355 (73.5) | 1 | <0.001 | 1 | 0.428 |
| Yes | 76 (6.8) | 1043 (93.2) | 4.948 (3.635, 6.735) | 1.211 (0.755, 1.943) | ||
| Behavioral control | ||||||
| No | 122 (40.4) | 180 (59.6) | 1 | <0.001 | 1 | <0.001 |
| Yes | 82 (6.3) | 1218 (93.7) | 10.067 (7.306, 13.874) | 3.456 (2.023, 5.902) | ||
| Variables | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| ORa (95% CI) | p Value | ORa (95% CI) | p Value | ORa (95% CI) | p Value | |
| Severity | ||||||
| No | 1 | 0.175 | 1 | 0.242 | 1 | 0.340 |
| Yes | 0.689 (0.402, 1.181) | 0.722 (0.419, 1.246) | 0.764 (0.440, 1.328) | |||
| Susceptibility | ||||||
| No | 1 | 0.828 | 1 | 0.800 | 1 | 0.737 |
| Yes | 1.046 (0.694, 1.577) | 1.055 (0.698, 1.593) | 1.074 (0.707, 1.634) | |||
| Response efficacy | ||||||
| No | 1 | 0.002 | 1 | 0.002 | 1 | 0.002 |
| Yes | 2.170 (1.334, 3.530) | 2.142 (1.312, 3.498) | 2.238 (1.360, 3.682) | |||
| Self-efficacy | ||||||
| No | 1 | 0.320 | 1 | 0.385 | 1 | 0.387 |
| Yes | 1.297 (0.777, 2.164) | 1.257 (0.750, 2.108) | 1.261 (0.745, 2.135) | |||
| Response cost | ||||||
| No | 1 | 0.001 | 1 | 0.001 | 1 | 0.001 |
| Yes | 0.501 (0.334, 0.751) | 0.491 (0.326, 0.738) | 0.484 (0.319, 0.732) | |||
| Attitude | ||||||
| No | 1 | 0.001 | 1 | 0.001 | 1 | 0.001 |
| Yes | 2.474 (1.427, 4.288) | 2.641 (1.516, 4.600) | 2.619 (1.480, 4.636) | |||
| Subjective norms | ||||||
| No | 1 | 0.414 | 1 | 0.513 | 1 | 0.764 |
| Yes | 1.220 (0.757, 1.966) | 1.174 (0.727, 1.895) | 1.077 (0.662, 1.755) | |||
| Behavioral control | ||||||
| No | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 |
| Yes | 3.562 (2.073, 6.119) | 3.680 (2.139, 6.333) | 3.743 (2.165, 6.471) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, M.; Liu, L.; Gu, S.-Y.; Peng, X.-Q.; Zhang, C.; Wu, Q.-F.; Xu, X.-P.; You, H. Behavioral Intention and Its Predictors toward COVID-19 Booster Vaccination among Chinese Parents: Applying Two Behavioral Theories. Int. J. Environ. Res. Public Health 2022, 19, 7520. https://doi.org/10.3390/ijerph19127520
Zhou M, Liu L, Gu S-Y, Peng X-Q, Zhang C, Wu Q-F, Xu X-P, You H. Behavioral Intention and Its Predictors toward COVID-19 Booster Vaccination among Chinese Parents: Applying Two Behavioral Theories. International Journal of Environmental Research and Public Health. 2022; 19(12):7520. https://doi.org/10.3390/ijerph19127520
Chicago/Turabian StyleZhou, Meng, Li Liu, Shu-Yan Gu, Xue-Qing Peng, Chi Zhang, Qi-Feng Wu, Xin-Peng Xu, and Hua You. 2022. "Behavioral Intention and Its Predictors toward COVID-19 Booster Vaccination among Chinese Parents: Applying Two Behavioral Theories" International Journal of Environmental Research and Public Health 19, no. 12: 7520. https://doi.org/10.3390/ijerph19127520
APA StyleZhou, M., Liu, L., Gu, S.-Y., Peng, X.-Q., Zhang, C., Wu, Q.-F., Xu, X.-P., & You, H. (2022). Behavioral Intention and Its Predictors toward COVID-19 Booster Vaccination among Chinese Parents: Applying Two Behavioral Theories. International Journal of Environmental Research and Public Health, 19(12), 7520. https://doi.org/10.3390/ijerph19127520





