The Effectiveness of Behavioral Interventions in Adults with Post-Traumatic Stress Disorder during Clinical Rehabilitation: A Rapid Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy and Eligibility Criteria
- Population: Adults (aged 18 or over) with a diagnosis of PTSD based on any of the following: DSM-III (APA 1980), DSM-III-R (APA 1987), DSM-IV (APA 2000), DSM-5 (APA 2013), ICD-9 (WHO 1979), or ICD-10 (WHO 1992) were included. The onset and diagnosis of PTSD must have occurred after experiencing physical injury or life-threatening disease (e.g., brain injury, spinal cord injury, neck strain injuries, infectious diseases such as COVID-19), and secondary to comorbidity requiring rehabilitation intervention(s). No restrictions on symptom severity or the type of physical injury or illness (including COVID-19) were applied.
- Interventions: In the selection of interventions, the authors adhered to the definition that defines rehabilitation as “A multimodal person-centred process, including functioning interventions targeting body functions, and/or activities and participation, and/or the interaction with the environment, with the goal of optimizing functioning for persons with health conditions experiencing disability or likely to experience disability and/or persons with disability” [21]. All behavioral interventions recommended by both the American Psychological Association (APA) and National Institute for Health and Clinical Excellence (NICE) current guidelines for the reduction in PTSD symptoms [3,22] and the improvement of functioning as part of a multidisciplinary rehabilitation treatment were included.
- The list of considered interventions comprises the following therapies: cognitive-behavioral therapy, cognitive processing therapy, cognitive therapy, prolonged exposure therapy, brief eclectic psychotherapy, eye movement desensitization and reprocessing therapy, narrative exposure therapy, trauma-focused cognitive-behavioral therapy, supported trauma-focused computerized and cognitive-behavioral therapy—alone or combined with any other treatments and/or usual care. No delivery modality restriction was applied.
- Comparators: The comparators were PTSD interventions with any other intervention (e.g., usual care, drugs), waitlist, or no-treatment care.
- Outcomes: Considering the complexity and heterogeneity of the outcomes used in research on PTSD improvement trajectories within the rehabilitative process, the outcomes were categorized and assessed as follows:
- Primary outcomes:
- PTSD symptom reduction (e.g., Clinician-Administered PTSD Scale—all versions; PTSD Checklist—all versions);
- Physical, social, executive, and cognitive functioning (e.g., De Morton Mobility Index, Roland Morris Disability Questionnaire, Global Assessment of Functioning–functioning and symptoms; Wechsler Adult Intelligence Scale—all versions).
- Secondary outcome:
- Quality of life (e.g., Human Service Scale Short Form-36 Health Survey; WHO Quality of Life–Brief).
- Adults diagnosed with PTSD after injury or illness experiencing non-physical (i.e., emotional/psychological) trauma and/or witnessing a traumatic event requiring only behavioral interventions;
- Studies assessing mixed-trauma populations (i.e., with different PTSD-related causes and no separate data), subsyndromal participants (i.e., PTSS), or without an official or clear diagnosis of PTSD, or interventions for the prevention of PTSD;
- Non-RCT study designs such as conference abstracts, protocol stages, pilot, and crossover designs were excluded.
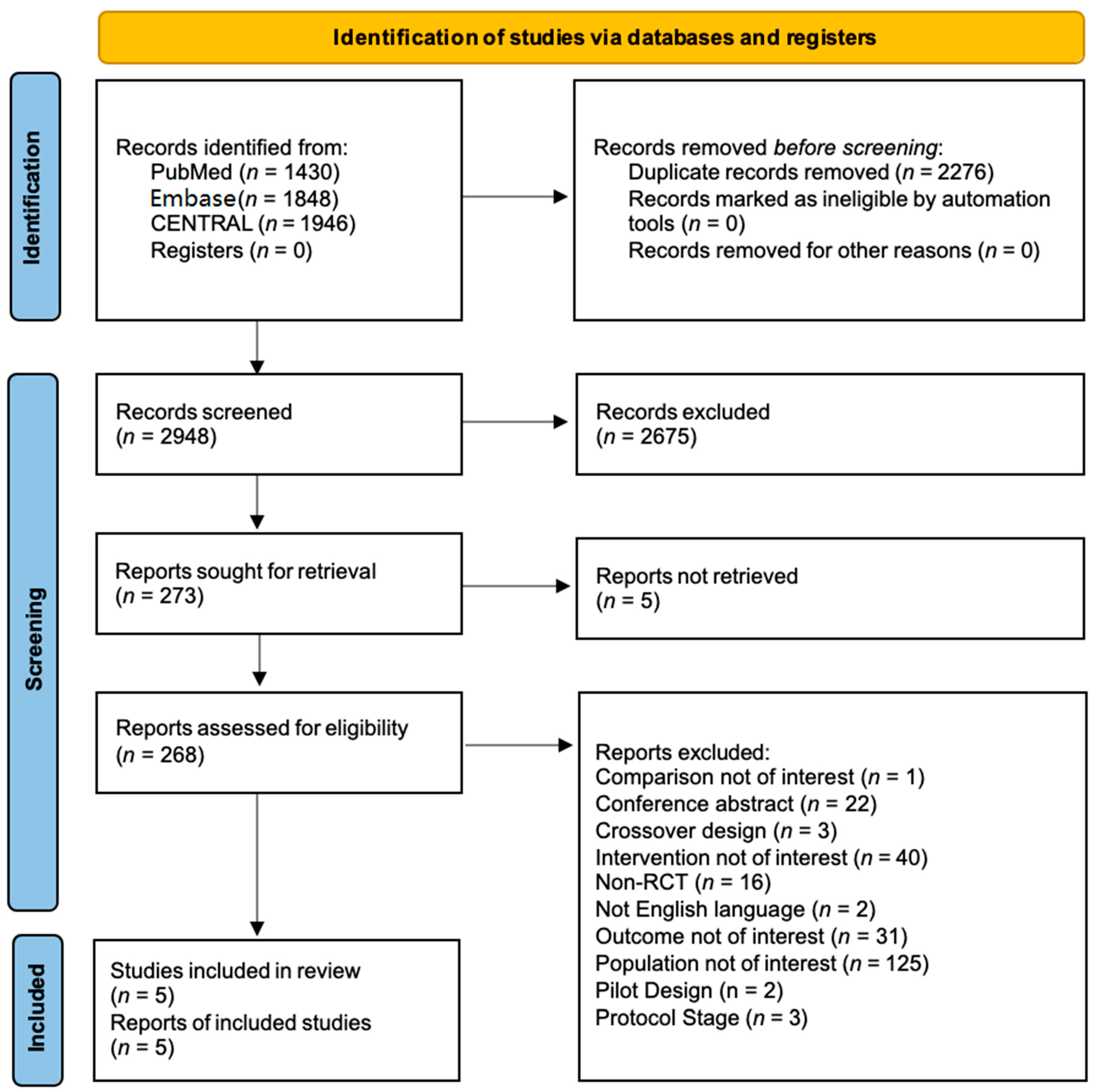
2.2. Study Selection and Data Extraction
2.3. Quality Assessment
2.4. Summary of Findings and Assessment of the Certainty of Evidence
2.5. Data Synthesis
3. Results
3.1. Characteristics of Included Studies
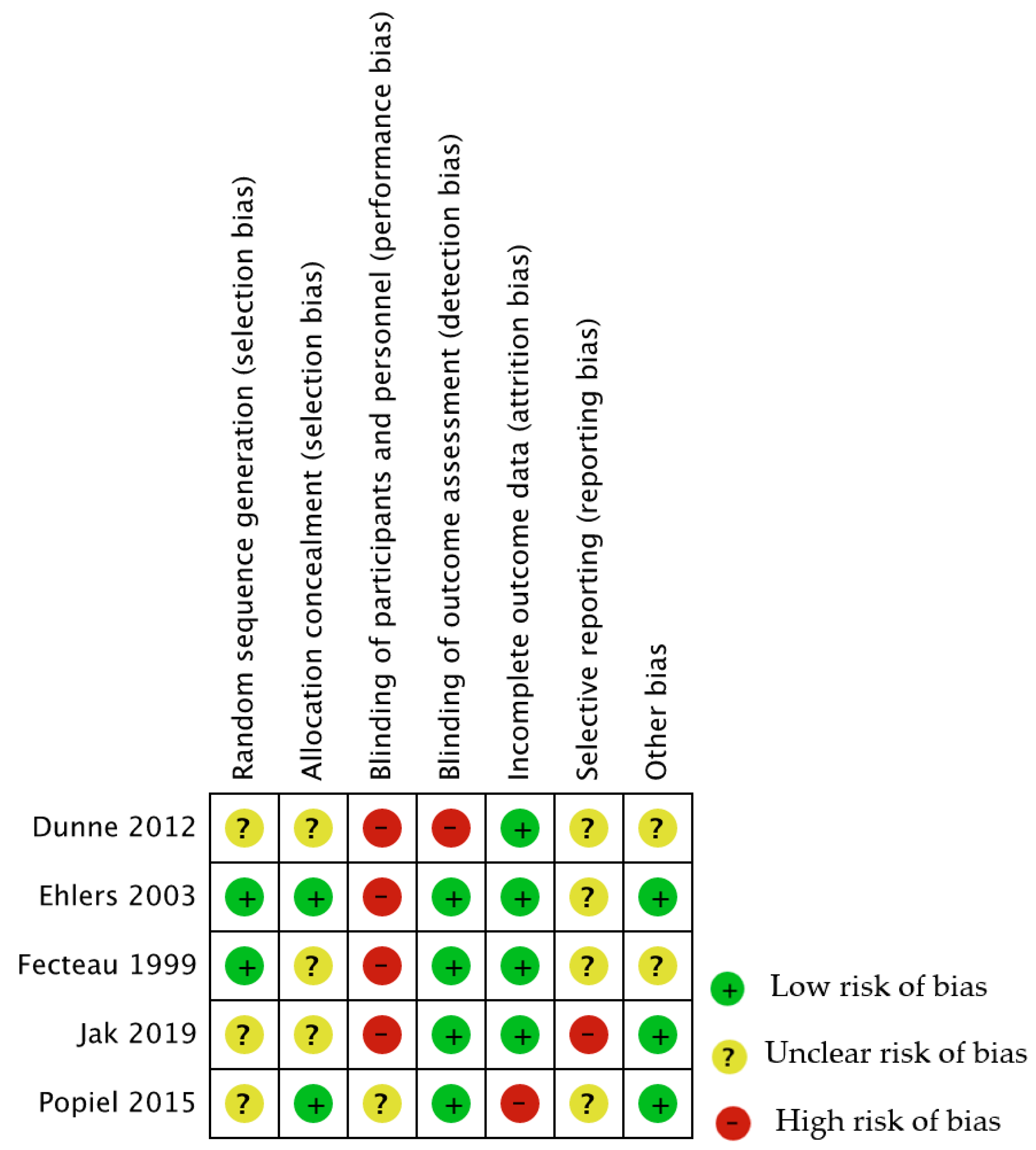
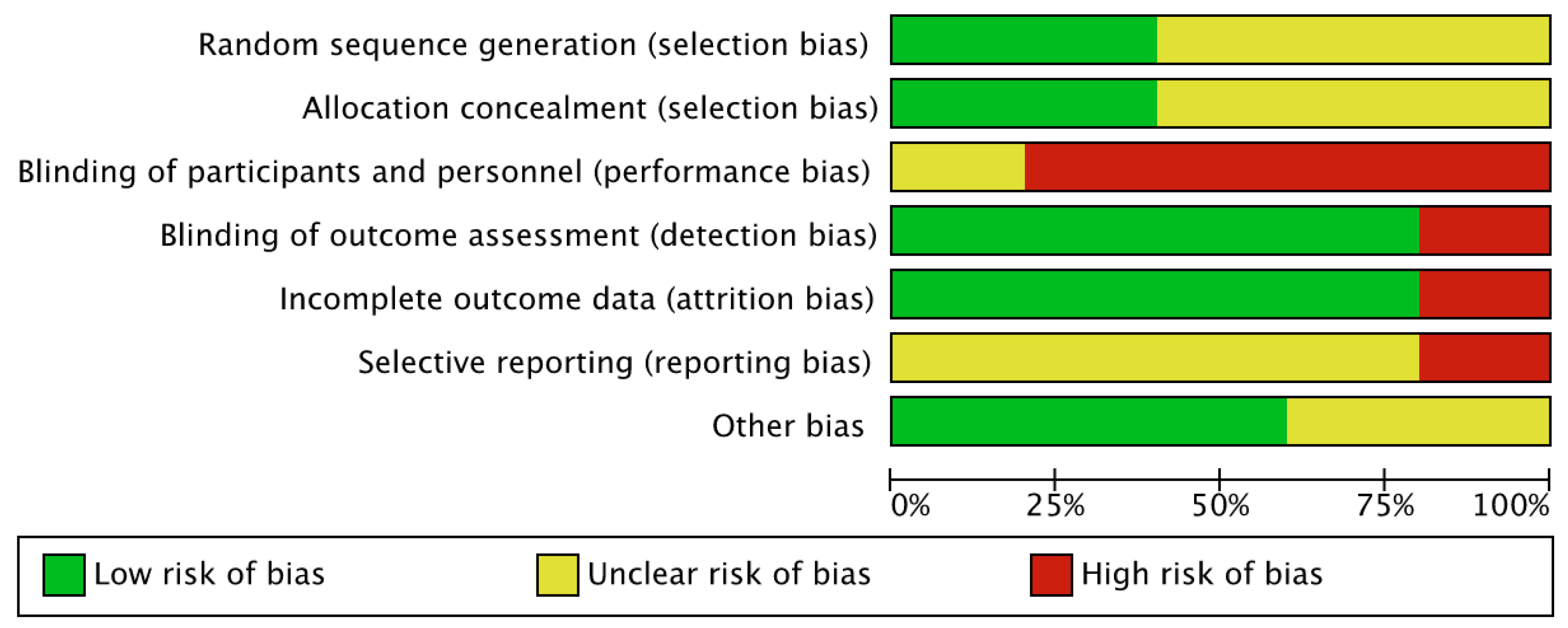
3.2. Risk of Included Studies
3.3. Effects of Interventions
3.3.1. Cognitive-Behavioral Therapy versus Waitlist
3.3.2. Trauma-Focused Cognitive-Behavioral Therapy Compared versus Waitlist
3.3.3. Symptom Management and Rehabilitation Therapy–Cognitive Processing Therapy versus Cognitive Processing Therapy
3.3.4. Prolonged Exposure Therapy versus Paroxetine
3.3.5. Cognitive Therapy versus Repeated Assessments
3.4. Certainty of Evidence
4. Discussion
4.1. PTSD in COVID-19 Survivors
4.2. Limitations and Implications
- Focus investigations on the etiology and mechanisms by which trauma causes PTSD;
- Provide clear definition;
- Spread awareness on critical differences that may impact clinical outcomes among patients who survived a life-threatening disease and those who experience psychological trauma.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Risk of Bias
- Random Sequence Generation (selection bias)
- Allocation Concealment (selection bias)
- Blinding of Participants and Personnel (performance bias)
- Blinding of Outcome Assessor (detection bias)
- Incomplete Data Outcome (attrition bias)
- Selective Reporting
References
- Rehabilitation and COVID-19. Available online: https://www.who.int/teams/noncommunicable-diseases/covid-19/rehabilitation (accessed on 22 September 2021).
- Bruijning, J.E.; van Rens, G.; Fick, M.; Knol, D.L.; van Nispen, R. Longitudinal observation, evaluation and interpretation of coping with mental (emotional) health in low vision rehabilitation using the Dutch ICF Activity Inventory. Health Qual. Life Outcomes 2014, 12, 182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guideline Development Panel for the Treatment of PTSD in Adults, American Psychological Association Summary of the clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Am. Psychol. 2019, 74, 596–607. [CrossRef] [PubMed]
- Edmondson, D. An Enduring Somatic Threat Model of Posttraumatic Stress Disorder Due to Acute Life-Threatening Medical Events. Soc. Personal. Psychol. Compass 2014, 8, 118–134. [Google Scholar] [CrossRef] [PubMed]
- Cordova, M.J.; Riba, M.B.; Spiegel, D. Post-traumatic stress disorder and cancer. Lancet Psychiatry 2017, 4, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Janiri, D.; Carfì, A.; Kotzalidis, G.D.; Bernabei, R.; Landi, F.; Sani, G. Posttraumatic Stress Disorder in Patients After Severe COVID-19 Infection. JAMA Psychiatry 2021, 78, 567–569. [Google Scholar] [CrossRef]
- Yuan, K.; Gong, Y.-M.; Liu, L.; Sun, Y.-K.; Tian, S.-S.; Wang, Y.-J.; Zhong, Y.; Zhang, A.-Y.; Su, S.-Z.; Liu, X.-X.; et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: A meta-analysis and systematic review. Mol. Psychiatry 2021, 26, 4982–4998. [Google Scholar] [CrossRef]
- Wade, D.T. Rehabilitation after COVID-19: An evidence-based approach. Clin. Med. 2020, 20, 359–365. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Xiao, S.; Luo, D.; Xiao, Y. Survivors of COVID-19 are at high risk of posttraumatic stress disorder. Glob. Health Res. Policy 2020, 5, 29. [Google Scholar] [CrossRef]
- Tu, Y.; Zhang, Y.; Li, Y.; Zhao, Q.; Bi, Y.; Lu, X.; Kong, Y.; Wang, L.; Lu, Z.; Hu, L. Post-traumatic stress symptoms in COVID-19 survivors: A self-report and brain imaging follow-up study. Mol. Psychiatry 2021, 26, 7475–7480. [Google Scholar] [CrossRef]
- Kaseda, E.T.; Levine, A.J. Post-traumatic stress disorder: A differential diagnostic consideration for COVID-19 survivors. Clin. Neuropsychol. 2020, 34, 1498–1514. [Google Scholar] [CrossRef] [PubMed]
- Greene, T.; El-Leithy, S.; Billings, J.; Albert, I.; Birch, J.; Campbell, M.; Ehntholt, K.; Fortune, L.; Gilbert, N.; Grey, N.; et al. Anticipating PTSD in severe COVID survivors: The case for screen-and-treat. Eur. J. Psychotraumatol. 2022, 13, 1959707. [Google Scholar] [CrossRef] [PubMed]
- Garton, A.L.A.; Sisti, J.A.; Gupta, V.P.; Christophe, B.R.; Connolly, E.S. Poststroke Post-Traumatic Stress Disorder. Stroke 2017, 48, 507–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gros, D.F.; Lancaster, C.L.; Horner, M.D.; Szafranski, D.D.; Back, S.E. The influence of traumatic brain injury on treatment outcomes of Concurrent Treatment for PTSD and Substance Use Disorders Using Prolonged Exposure (COPE) in veterans. Compr. Psychiatry 2017, 78, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Watkins, L.E.; Sprang, K.R.; Rothbaum, B.O. Treating PTSD: A Review of Evidence-Based Psychotherapy Interventions. Front. Behav. Neurosci. 2018, 12, 258. [Google Scholar] [CrossRef] [PubMed]
- Fait, K.; Vilchinsky, N.; Dekel, R.; Levi, N.; Hod, H.; Matetzky, S. Cardiac-disease-induced PTSD and Fear of illness progression: Capturing the unique nature of disease-related PTSD. Gen. Hosp. Psychiatry 2018, 53, 131–138. [Google Scholar] [CrossRef]
- Edmondson, D.; Richardson, S.; Fausett, J.K.; Falzon, L.; Howard, V.J.; Kronish, I.M. Prevalence of PTSD in Survivors of Stroke and Transient Ischemic Attack: A Meta-Analytic Review. PLoS ONE 2013, 8, e66435. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Garritty, C.; Gartlehner, G.; Kamel, C.; King, V.J.; Nussbaumer-Streit, B.; Stevens, A.; Hamel, C.; Affengruber, L.; Cochrane Rapid Reviews Methods Group. Cochrane Rapid Reviews Interim Guidance from the Cochrane Rapid Reviews Methods Group. Cochrane 2020. Available online: https://methods.cochrane.org/rapidreviews/sites/methods.cochrane.org.rapidreviews/files/public/uploads/cochrane_rr_-_guidance-23mar2020-final.pdf (accessed on 2 August 2021).
- Negrini, S.; Meyer, T.; Arienti, C.; Kiekens, C.; Pollock, A.; Selb, M.; Stucki, G.; 3rd Cochrane Rehabilitation Methodology Meeting Participants. The 3rd Cochrane Rehabilitation Methodology Meeting: “Rehabilitation definition for scientific research purposes”. Eur. J. Phys. Rehabil. Med. 2020, 56, 658–660. [Google Scholar] [CrossRef]
- Overview|Post-Traumatic Stress Disorder|Guidance|NICE. Available online: https://www.nice.org.uk/guidance/ng116 (accessed on 27 July 2021).
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Chapter 14: Completing ‘Summary of Findings’ Tables and Grading the Certainty of the Evidence. Available online: https://training.cochrane.org/handbook/current/chapter-14 (accessed on 27 July 2021).
- Popiel, A.; Zawadzki, B.; Pragłowska, E.; Teichman, Y. Prolonged exposure, paroxetine and the combination in the treatment of PTSD following a motor vehicle accident. A randomized clinical trial—The “TRAKT” study. J. Behav. Ther. Exp. Psychiatry 2015, 48, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Jak, A.J.; Jurick, S.; Crocker, L.D.; Sanderson-Cimino, M.; Aupperle, R.; Rodgers, C.S.; Thomas, K.R.; Boyd, B.; Norman, S.B.; Lang, A.J.; et al. SMART-CPT for veterans with comorbid post-traumatic stress disorder and history of traumatic brain injury: A randomised controlled trial. J. Neurol. Neurosurg. Psychiatry 2019, 90, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, A.; Clark, D.M.; Hackmann, A.; McManus, F.; Fennell, M.; Herbert, C.; Mayou, R. A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Arch. Gen. Psychiatry 2003, 60, 1024–1032. [Google Scholar] [CrossRef] [Green Version]
- Dunne, R.L.; Kenardy, J.; Sterling, M. A randomized controlled trial of cognitive-behavioral therapy for the treatment of PTSD in the context of chronic whiplash. Clin. J. Pain 2012, 28, 755–765. [Google Scholar] [CrossRef]
- Fecteau, G.; Nicki, R. Cognitive Behavioural Treatment of Post Traumatic Stress Disorder after Motor Vehicle Accident. Behav. Cogn. Psychother. 1999, 27, 201–214. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Dennett, L.; Arienti, C.; Dahchi, M.; Arokoski, J.; Heinemann, A.W.; Malmivaara, A. Blinding in Rehabilitation Research: Empirical Evidence on the Association Between Blinding and Treatment Effect Estimates. Am. J. Phys. Med. Rehabil. 2020, 99, 198–209. [Google Scholar] [CrossRef]
- Coventry, P.A.; Meader, N.; Melton, H.; Temple, M.; Dale, H.; Wright, K.; Cloitre, M.; Karatzias, T.; Bisson, J.; Roberts, N.P.; et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: Systematic review and component network meta-analysis. PLOS Med. 2020, 17, e1003262. [Google Scholar] [CrossRef]
- Merz, J.; Schwarzer, G.; Gerger, H. Comparative Efficacy and Acceptability of Pharmacological, Psychotherapeutic, and Combination Treatments in Adults With Posttraumatic Stress Disorder: A Network Meta-analysis. JAMA Psychiatry 2019, 76, 904–913. [Google Scholar] [CrossRef]
- Cody, M.W.; Beck, J.G. Physical Injury, PTSD Symptoms, and Medication Use: Examination in Two Trauma Types: Physical Injury, PTSD Symptoms, and Medication Use. J. Trauma. Stress 2014, 27, 74–81. [Google Scholar] [CrossRef]
- Jowett, S.; Shevlin, M.; Hyland, P.; Karatzias, T. Posttraumatic Stress Disorder and Persistent Somatic Symptoms During the COVID-19 Pandemic: The Role of Sense of Threat. Psychosom. Med. 2021, 83, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, N.; Laydon, D.; Nedjati Gilani, G.; Imai, N.; Ainslie, K.; Baguelin, M.; Bhatia, S.; Boonyasiri, A.; Cucunuba Perez, Z.; Cuomo-Dannenburg, G.; et al. Report 9: Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID19 Mortality and Healthcare Demand. Available online: http://spiral.imperial.ac.uk/handle/10044/1/77482 (accessed on 20 March 2020).
- Ahmed, H.; Patel, K.; Greenwood, D.C.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’Connor, R.; Jones, A.; et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, jrm00063. [Google Scholar] [CrossRef] [PubMed]
- Risk Factors of Delayed Onset Posttraumatic Stress Disorder in Chronically Critically Ill Patients. Available online: https://oce-ovid-com.ezproxy1.lib.asu.edu/article/00005053-201710000-00005/PDF (accessed on 2 March 2022).
- Hatch, R.; McKechnie, S.; Griffiths, J. Psychological intervention to prevent ICU-related PTSD: Who, when and for how long? Crit. Care 2011, 15, 141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arienti, C.; Armijo-Olivo, S.; Minozzi, S.; Tjosvold, L.; Lazzarini, S.G.; Patrini, M.; Negrini, S. Methodological Issues in Rehabilitation Research: A Scoping Review. Arch. Phys. Med. Rehabil. 2021, 102, 1614–1622.e14. [Google Scholar] [CrossRef] [PubMed]
| Author(s) (Year) | Title | Country | Aims | Type of Population | No. PP | Diagnostic Instruments |
|---|---|---|---|---|---|---|
| Dunne et al. (2012) [29] | A Randomized Controlled Trial of Cognitive-Behavioral Therapy for the Treatment of PTSD in the Context of Chronic Whiplash. | Australia | Assess if trauma-focused cognitive-behavioral therapy reduces PTSD diagnosis, symptoms, and physiological reactivity to trauma cues. | Chronic whiplash-associated disorders | 26 | Structured clinical interview for DSM-IV |
| Fecteau and Nicki (1999) [30] | Cognitive-Behavioural Treatment of Post-Traumatic Stress Disorder after Motor Vehicle Accident. | Canada | Evaluate the efficacy of cognitive-behavioral therapy for PTSD following motor vehicle accident trauma. | Motor vehicle accident survivors | 20 | Clinically administrated PTSD scale-2 for DSM-IV |
| Jak et al. (2019) [27] | SMART-CPT for Veterans with Comorbid Post-Traumatic Stress Disorder and History of Traumatic Brain Injury: A Randomised Controlled Trial. | USA | Compare a novel treatment, symptom management, and rehabilitation therapy—cognitive processing therapy to cognitive processing therapy to evaluate its efficacy in PTSD symptoms and cognitive function improvements. | Veterans with traumatic brain injury | 100 | Clinically administrated PTSD scale-2 DSM-IV |
| Popiel et al. (2015) [26] | Prolonged Exposure, Paroxetine and the Combination in the Treatment of PTSD Following a Motor Vehicle Accident. A Randomized Clinical trial—The “TRAKT” study. | Poland | Compared the efficacy of prolonged exposure and medication when used as a monotherapy in treating PTSD. | Motor vehicle accident survivors | 228 | Structured clinical interview for DSM-IV |
| Ehlers et al. (2003) [28] | A Randomized Controlled Trial of Cognitive Therapy, a Self-Help Booklet, and Repeated Assessments AS Early Interventions for Posttraumatic Stress Disorder. | UK | Determine whether cognitive therapy or a self-help booklet is more effective in preventing chronic PTSD than repeated assessments. | Motor vehicle accident survivors | 85 | Structured clinical interview for DSM-IV; Post-traumatic diagnostic scale |
| Author(s) (Year) | Comparison | Outcomes | Outcome Measures | PP Analyzed | Effect Estimates (95% CI) |
|---|---|---|---|---|---|
| Dunne et al. (2012) [29] | Trauma-focused cognitive-behavioral therapy vs. Waitlist | PTSD Symptoms Severity | Post-Traumatic Diagnostic Scale | 23 | −7.69 (−14.29–−1.09) |
| Quality of Life | Short Form Health Survey-36 (Physical Health Total) | 11.00 (−2.71–24.71) | |||
| Short Form Health Survey-36 (Mental Health Total) | 7.31 (−8.02–22.64) | ||||
| Disability | Neck Disability Index | −5.16 (−15.58–5.26) | |||
| Fecteau and Nicki (1999) [30] | Cognitive-behavioral therapy vs. waitlist | PTSD Symptoms Severity | Clinically Administrated PTSD Scale-2 | 20 | −37.10 (−61.38–−12.82) |
| Jak et al. (2019) [27] | Symptom management and rehabilitation therapy–cognitive processing therapy vs. Cognitive processing therapy | PTSD Symptoms Severity | PTSD Check List-Specific | 100 | −0.48 (−6.45–5.49) |
| Cognitive Function | Wechsler Adult Intelligence Scale-IV (Processing Speed) | 0.34 (−4.78–5.46) | |||
| Wechsler Adult Intelligence Scale-IV (Digit Span) | 1.04 (−2.48–1.92) | ||||
| Delis–Kaplan Executive Function System (Color–Word Interference) | −0.28 (−0.16–2.24) | ||||
| Delis–Kaplan Executive Function System (Trail Making) | −0.02 (−0.80–0.76) | ||||
| Wisconsin Card Sorting Test—64 (Total Errors) | 6.45 (3.00–9.90) | ||||
| California Verbal Learning Test II (Learning Tot.) | 4.39 (−0.54–9.32) | ||||
| General Life Satisfaction | Quality of Life Inventory-B | 0.21 (−0.33–0.75) | |||
| Popiel et al. (2015) [26] | Prolonged exposure vs. paroxetine | Symptoms Remission | Post-traumatic Diagnostic Scale | 140 | 1.51 (−0.98–2.32) |
| Ehlers et al. (2003) [28] | Cognitive therapy vs. repeated assessments | PTSD Symptoms Severity | Post-Traumatic Diagnostic Scale (Frequency) | 54 | −14.30 (−20.05–−8.55) |
| Post-Traumatic Diagnostic Scale (Distress) | −12.50 (−18.55–−6.45) | ||||
| Clinically Administrated PTSD Scale-SX (Frequency) | −14.40 (−20.66–−8.14) | ||||
| Clinically Administrated PTSD Scale-SX (Intensity) | −14.40 (−20.66–−8.14) | ||||
| Disability | Sheehan Disability Scale | −1.90 (−3.17–−0.63) | |||
| Clinically Administrated PTSD Scale-SX (Disability) | −0.70 (−1.10–−0.30) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gimigliano, F.; Young, V.M.; Arienti, C.; Bargeri, S.; Castellini, G.; Gianola, S.; Lazzarini, S.G.; Moretti, A.; Heinemann, A.W.; Negrini, S. The Effectiveness of Behavioral Interventions in Adults with Post-Traumatic Stress Disorder during Clinical Rehabilitation: A Rapid Review. Int. J. Environ. Res. Public Health 2022, 19, 7514. https://doi.org/10.3390/ijerph19127514
Gimigliano F, Young VM, Arienti C, Bargeri S, Castellini G, Gianola S, Lazzarini SG, Moretti A, Heinemann AW, Negrini S. The Effectiveness of Behavioral Interventions in Adults with Post-Traumatic Stress Disorder during Clinical Rehabilitation: A Rapid Review. International Journal of Environmental Research and Public Health. 2022; 19(12):7514. https://doi.org/10.3390/ijerph19127514
Chicago/Turabian StyleGimigliano, Francesca, Vanessa M. Young, Chiara Arienti, Silvia Bargeri, Greta Castellini, Silvia Gianola, Stefano G. Lazzarini, Antimo Moretti, Allen W. Heinemann, and Stefano Negrini. 2022. "The Effectiveness of Behavioral Interventions in Adults with Post-Traumatic Stress Disorder during Clinical Rehabilitation: A Rapid Review" International Journal of Environmental Research and Public Health 19, no. 12: 7514. https://doi.org/10.3390/ijerph19127514
APA StyleGimigliano, F., Young, V. M., Arienti, C., Bargeri, S., Castellini, G., Gianola, S., Lazzarini, S. G., Moretti, A., Heinemann, A. W., & Negrini, S. (2022). The Effectiveness of Behavioral Interventions in Adults with Post-Traumatic Stress Disorder during Clinical Rehabilitation: A Rapid Review. International Journal of Environmental Research and Public Health, 19(12), 7514. https://doi.org/10.3390/ijerph19127514