Histological and Biological Response to Different Types of Biomaterials: A Narrative Single Research Center Experience over Three Decades
Abstract
1. Introduction
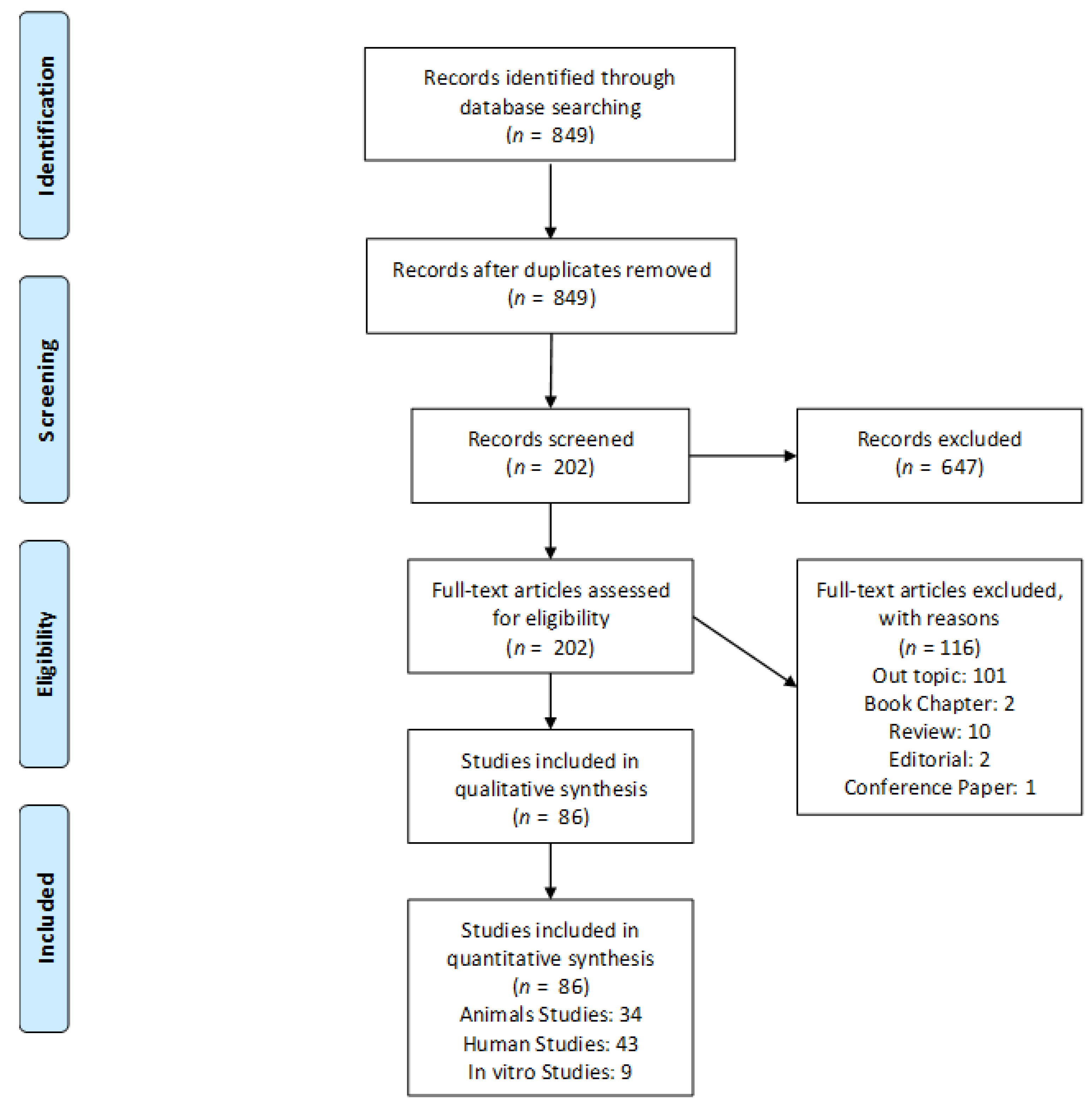
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Selection of the Studies
3. Results
3.1. Anorganic Bovine Bone (ABB)
3.2. Porcine Bone (PB)
- collagenated cortico-cancellous porcine bone
- collagenated cortical porcine bone
3.3. Equine Bone (EQ)
3.4. Biphasic Calcium Phosphate (BCP)
3.5. Calcium Carbonate
3.6. Bioglass
3.7. Porous Hydroxyapatite (Porous HA)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scarano, A.; Lorusso, F.; Ravera, L.; Mortellaro, C.; Piattelli, A. Bone Regeneration in Iliac Crestal Defects: An Experimental Study on Sheep. BioMed Res. Int. 2016, 2016, 4086870. [Google Scholar] [CrossRef]
- Scarano, A.; Degidi, M.; Iezzi, G.; Pecora, G.; Piattelli, M.; Orsini, G.; Caputi, S.; Perrotti, V.; Mangano, C.; Piattelli, A. Maxillary Sinus Augmentation with Different Biomaterials: A Comparative Histologic and Histomorphometric Study in Man. Implant Dent. 2006, 15, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Iezzi, G.; Degidi, M.; Piattelli, A.; Mangano, C.; Scarano, A.; Shibli, J.A.; Perrotti, V. Comparative Histological Results of Different Biomaterials Used in Sinus Augmentation Procedures: A Human Study at 6 Months. Clin. Oral Implant. Res. 2012, 23, 1369–1376. [Google Scholar] [CrossRef] [PubMed]
- Piattelli, A.; Scarano, A.; Russo, P.; Matarasso, S. Evaluation of Guided Bone Regeneration in Rabbit Tibia Using Bioresorbable and Non-Resorbable Membranes. Biomaterials 1996, 17, 791–796. [Google Scholar] [CrossRef]
- Scarano, A.; Perrotti, V.; Artese, L.; Degidi, M.; Degidi, D.; Piattelli, A.; Iezzi, G. Blood Vessels Are Concentrated within the Implant Surface Concavities: A Histologic Study in Rabbit Tibia. Odontology 2014, 102, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Piattelli, A.; Scarano, A.; Coraggio, F.; Matarasso, S. Early Tissue Reactions to Polylactic Acid Resorbable Membranes: A Histological and Histochemical Study in Rabbit. Biomaterials 1998, 19, 889–896. [Google Scholar] [CrossRef]
- Mangano, C.; Piattelli, A.; Scarano, A.; Raspanti, M.; Shibli, J.A.; Mangano, F.G.; Perrotti, V.; Iezzi, G. A Light and Scanning Electron Microscopy Study of Human Direct Laser Metal Forming Dental Implants. Int. J. Periodontics Restor. Dent. 2014, 34, e9–e17. [Google Scholar] [CrossRef]
- Giuliani, A.; Iezzi, G.; Mazzoni, S.; Piattelli, A.; Perrotti, V.; Barone, A. Regenerative Properties of Collagenated Porcine Bone Grafts in Human Maxilla: Demonstrative Study of the Kinetics by Synchrotron Radiation Microtomography and Light Microscopy. Clin. Oral Investig. 2018, 22, 505–513. [Google Scholar] [CrossRef]
- Majzoub, Z.; Cordioli, G.; Aramouni, P.K.; Vigolo, P.; Piattelli, A. Guided Bone Regeneration Using Demineralized Laminar Bone Sheets versus GTAM Membranes in the Treatment of Implant-Associated Defects. A Clinical and Histological Study. Clin. Oral Implant. Res. 1999, 10, 406–414. [Google Scholar] [CrossRef]
- Scarano, A.; Valbonetti, L.; Degidi, M.; Pecci, R.; Piattelli, A.; de Oliveira, P.S.; Perrotti, V. Implant-Abutment Contact Surfaces and Microgap Measurements of Different Implant Connections Under 3-Dimensional X-ray Microtomography. Implant Dent. 2016, 25, 656–662. [Google Scholar] [CrossRef]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A Narrative Review of the Histological and Histomorphometrical Evaluation of the Peri-Implant Bone in Loaded and Unloaded Dental Implants. A 30-Year Experience (1988–2018). Int. J. Environ. Res. Public Health 2020, 17, 2088. [Google Scholar] [CrossRef] [PubMed]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A 30-Year (1988–2018) Retrospective Microscopical Evaluation of Dental Implants Retrieved for Different Causes: A Narrative Review. Int. J. Periodontics Restor. Dent. 2020, 40, e211–e227. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Perrotti, V.; Piattelli, A.; Iezzi, G. Eight-Year Results of Site Retention of Anorganic Bovine Bone and Anorganic Bovine Matrix. J. Oral Implantol. 2013, 39, 727–732. [Google Scholar] [CrossRef]
- Orsini, G.; Traini, T.; Scarano, A.; Degidi, M.; Perrotti, V.; Piccirilli, M.; Piattelli, A. Maxillary Sinus Augmentation with Bio-Oss® Particles: A Light, Scanning, and Transmission Electron Microscopy Study in Man. J. Biomed. Mater. Res. 2005, 74B, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Orsini, G.; Scarano, A.; Degidi, M.; Caputi, S.; Iezzi, G.; Piattelli, A. Histological and Ultrastructural Evaluation of Bone around Bio-Oss Particles in Sinus Augmentation. Oral Dis. 2007, 13, 586–593. [Google Scholar] [CrossRef]
- Testori, T.; Iezzi, G.; Manzon, L.; Fratto, G.; Piattelli, A.; Weinstein, R.L. High Temperature-Treated Bovine Porous Hydroxyapatite in Sinus Augmentation Procedures: A Case Report. Int. J. Periodontics Restor. Dent. 2012, 32, 295–301. [Google Scholar]
- Traini, T.; Degidi, M.; Sammons, R.; Stanley, P.; Piattelli, A. Histologic and Elemental Microanalytical Study of Anorganic Bovine Bone Substitution Following Sinus Floor Augmentation in Humans. J. Periodontol. 2008, 79, 1232–1240. [Google Scholar] [CrossRef]
- Carinci, F.; Piattelli, A.; Degidi, M.; Palmieri, A.; Perrotti, V.; Scapoli, L.; Martinelli, M.; Laino, G.; Pezzetti, F. Genetic Effects of Anorganic Bovine Bone (Bio-Oss) on Osteoblast-like MG63 Cells. Arch. Oral Biol. 2006, 51, 154–163. [Google Scholar] [CrossRef]
- Chackartchi, T.; Iezzi, G.; Goldstein, M.; Klinger, A.; Soskolne, A.; Piattelli, A.; Shapira, L. Sinus Floor Augmentation Using Large (1–2 Mm) or Small (0.25–1 Mm) Bovine Bone Mineral Particles: A Prospective, Intra-Individual Controlled Clinical, Micro-Computerized Tomography and Histomorphometric Study. Clin. Oral Implant. Res. 2011, 22, 473–480. [Google Scholar] [CrossRef]
- Corinaldesi, G.; Piersanti, L.; Piattelli, A.; Iezzi, G.; Pieri, F.; Marchetti, C. Augmentation of the Floor of the Maxillary Sinus with Recombinant Human Bone Morphogenetic Protein-7: A Pilot Radiological and Histological Study in Humans. Br. J. Oral Maxillofac. Surg. 2013, 51, 247–252. [Google Scholar] [CrossRef]
- Traini, T.; Piattelli, A.; Caputi, S.; Degidi, M.; Mangano, C.; Scarano, A.; Perrotti, V.; Iezzi, G. Regeneration of Human Bone Using Different Bone Substitute Biomaterials. Clin. Implant. Dent. Relat. Res. 2015, 17, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Traini, T.; Valentini, P.; Iezzi, G.; Piattelli, A. A Histologic and Histomorphometric Evaluation of Anorganic Bovine Bone Retrieved 9 Years after a Sinus Augmentation Procedure. J. Periodontol. 2007, 78, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Perrotti, V.; Calasso, S.; Piattelli, A.; Sinjari, B.; Iezzi, G. Bone Formation in Sinus Augmentation Procedures Using Autologous Bone, Porcine Bone, and a 50:50 Mixture: A Human Clinical and Histological Evaluation at 2 Months. Clin. Oral Implant. Res. 2015, 26, 1180–1184. [Google Scholar] [CrossRef]
- Giuliani, A.; Manescu, A.; Mohammadi, S.; Mazzoni, S.; Piattelli, A.; Mangano, F.; Iezzi, G.; Mangano, C. Quantitative Kinetics Evaluation of Blocks Versus Granules of Biphasic Calcium Phosphate Scaffolds (HA/β-TCP 30/70) by Synchrotron Radiation X-Ray Microtomography: A Human Study. Implant Dent. 2016, 25, 6–15. [Google Scholar] [CrossRef]
- Mijiritsky, E.; Ferroni, L.; Gardin, C.; Bressan, E.; Zanette, G.; Piattelli, A.; Zavan, B. Porcine Bone Scaffolds Adsorb Growth Factors Secreted by MSCs and Improve Bone Tissue Repair. Materials 2017, 10, 1054. [Google Scholar] [CrossRef] [PubMed]
- Tetè, S.; Zizzari, V.L.; Vinci, R.; Zara, S.; Di Tore, U.; Manica, M.; Cataldi, A.; Mortellaro, C.; Piattelli, A.; Gherlone, E. Equine and Porcine Bone Substitutes in Maxillary Sinus Augmentation: A Histological and Immunohistochemical Analysis of VEGF Expression. J. Craniofac. Surg. 2014, 25, 835–839. [Google Scholar] [CrossRef] [PubMed]
- Barone, A.; Toti, P.; Piattelli, A.; Iezzi, G.; Derchi, G.; Covani, U. Extraction Socket Healing in Humans after Ridge Preservation Techniques: Comparison between Flapless and Flapped Procedures in a Randomized Clinical Trial. J. Periodontol. 2014, 85, 14–23. [Google Scholar] [CrossRef]
- Scarano, A.; Ceccarelli, M.; Marchetti, M.; Piattelli, A.; Mortellaro, C. Soft Tissue Augmentation with Autologous Platelet Gel and β-TCP: A Histologic and Histometric Study in Mice. BioMed Res. Int. 2016, 2016, 2078104. [Google Scholar] [CrossRef]
- Tetè, S.; Vinci, R.; Zizzari, V.L.; Zara, S.; La Scala, V.; Cataldi, A.; Gherlone, E.; Piattelli, A. Maxillary Sinus Augmentation Procedures through Equine-Derived Biomaterial or Calvaria Autologous Bone: Immunohistochemical Evaluation of OPG/RANKL in Humans. Eur. J. Histochem. 2013, 57, e10. [Google Scholar] [CrossRef]
- Artese, L.; Piattelli, A.; Di Stefano, D.A.; Piccirilli, M.; Pagnutti, S.; D’Alimonte, E.; Perrotti, V. Sinus Lift with Autologous Bone Alone or in Addition to Equine Bone: An Immunohistochemical Study in Man. Implant Dent. 2011, 20, 383–388. [Google Scholar] [CrossRef]
- Perrotti, V.; Nicholls, B.M.; Piattelli, A. Human Osteoclast Formation and Activity on an Equine Spongy Bone Substitute. Clin. Oral Implant. Res. 2009, 20, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Perrotti, V.; Shibli, J.A.; Mangano, F.; Ricci, L.; Piattelli, A.; Iezzi, G. Maxillary Sinus Grafting with Biphasic Calcium Phosphate Ceramics: Clinical and Histologic Evaluation in Man. Int. J. Oral Maxillofac. Implant. 2013, 28, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Sinjari, B.; Shibli, J.A.; Mangano, F.; Hamisch, S.; Piattelli, A.; Perrotti, V.; Iezzi, G. A Human Clinical, Histological, Histomorphometrical, and Radiographical Study on Biphasic HA-Beta-TCP 30/70 in Maxillary Sinus Augmentation. Clin. Implant. Dent. Relat. Res. 2015, 17, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Perrotti, V.; Degidi, M.; Piattelli, A.; Iezzi, G. Bone Regeneration with Algae-Derived Hydroxyapatite: A Pilot Histologic and Histomorphometric Study in Rabbit Tibia Defects. Int. J. Oral Maxillofac. Implant. 2012, 27, 336–340. [Google Scholar]
- Mangano, C.; Iaculli, F.; Piattelli, A.; Mangano, F.; Shibli, J.A.; Perrotti, V.; Iezzi, G. Clinical and Histologic Evaluation of Calcium Carbonate in Sinus Augmentation: A Case Series. Int. J. Periodontics Restor. Dent. 2014, 34, e43–e49. [Google Scholar] [CrossRef]
- Pettinicchio, M.; Traini, T.; Murmura, G.; Caputi, S.; Degidi, M.; Mangano, C.; Piattelli, A. Histologic and Histomorphometric Results of Three Bone Graft Substitutes after Sinus Augmentation in Humans. Clin. Oral Investig. 2012, 16, 45–53. [Google Scholar] [CrossRef]
- Pettinicchio, M.; Sammons, R.; Caputi, S.; Piattelli, A.; Traini, T. Bone Regeneration in Sinus Augmentation Procedures with Calcium Sulphate. Microstructure and Microanalytical Investigations. Aust. Dent. J. 2012, 57, 200–206. [Google Scholar] [CrossRef]
- Giuliani, A.; Manescu, A.; Larsson, E.; Tromba, G.; Luongo, G.; Piattelli, A.; Mangano, F.; Iezzi, G.; Mangano, C. In Vivo Regenerative Properties of Coralline-Derived (Biocoral) Scaffold Grafts in Human Maxillary Defects: Demonstrative and Comparative Study with Beta-Tricalcium Phosphate and Biphasic Calcium Phosphate by Synchrotron Radiation x-Ray Microtomography. Clin. Implant. Dent. Relat. Res. 2014, 16, 736–750. [Google Scholar] [CrossRef]
- Inchingolo, F.; Hazballa, D.; Inchingolo, A.D.; Malcangi, G.; Marinelli, G.; Mancini, A.; Maggiore, M.E.; Bordea, I.R.; Scarano, A.; Farronato, M.; et al. Innovative Concepts and Recent Breakthrough for Engineered Graft and Constructs for Bone Regeneration: A Literature Systematic Review. Materials 2022, 15, 1120. [Google Scholar] [CrossRef]
- Chan, C.; Thompson, I.; Robinson, P.; Wilson, J.; Hench, L. Evaluation of Bioglass/Dextran Composite as a Bone Graft Substitute. Int. J. Oral Maxillofac. Surg. 2002, 31, 73–77. [Google Scholar] [CrossRef]
- Piattelli, A.; Scarano, A.; Piattelli, M.; Coraggio, F.; Matarasso, S. Bone Regeneration Using Bioglass: An Experimental Study in Rabbit Tibia. J. Oral Implantol. 2000, 26, 257–261. [Google Scholar] [CrossRef]
- Lisboa-Filho, P.N.; Gomes-Ferreira, P.H.S.; Batista, F.R.S.; Momesso, G.A.C.; Faverani, L.P.; Okamoto, R. Bone Repair with Raloxifene and Bioglass Nanoceramic Composite in Animal Experiment. Connect. Tissue Res. 2018, 59, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Scarano, A.; Iezzi, G.; Orsini, G.; Perrotti, V.; Mangano, F.; Montini, S.; Piccirilli, M.; Piattelli, A. Maxillary Sinus Augmentation Using an Engineered Porous Hydroxyapatite: A Clinical, Histological, and Transmission Electron Microscopy Study in Man. J. Oral Implantol. 2006, 32, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Bechara, K.; Dottore, A.M.; Kawakami, P.Y.; Gehrke, S.A.; Coelho, P.G.; Piattelli, A.; Iezzi, G.; Shibli, J.A. A Histological Study of Non-Ceramic Hydroxyapatite as a Bone Graft Substitute Material in the Vertical Bone Augmentation of the Posterior Mandible Using an Interpositional Inlay Technique: A Split Mouth Evaluation. Ann. Anat. 2015, 202, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Doi, K.; Oue, H.; Morita, K.; Kajihara, S.; Kubo, T.; Koretake, K.; Perrotti, V.; Iezzi, G.; Piattelli, A.; Akagawa, Y. Development of Implant/Interconnected Porous Hydroxyapatite Complex as New Concept Graft Material. PLoS ONE 2012, 7, e49051. [Google Scholar] [CrossRef]
- Scarano, A.; Inchingolo, F.; Murmura, G.; Traini, T.; Piattelli, A.; Lorusso, F. Three-Dimensional Architecture and Mechanical Properties of Bovine Bone Mixed with Autologous Platelet Liquid, Blood, or Physiological Water: An In Vitro Study. Int. J. Mol. Sci. 2018, 19, 1230. [Google Scholar] [CrossRef]
- Mangano, C.; Scarano, A.; Perrotti, V.; Iezzi, G.; Piattelli, A. Maxillary Sinus Augmentation with a Porous Synthetic Hydroxyapatite and Bovine-Derived Hydroxyapatite: A Comparative Clinical and Histologic Study. Int. J. Oral Maxillofac. Implant. 2007, 22, 980–986. [Google Scholar]
- Cosso, M.G.; de Brito, R.B.; Piattelli, A.; Shibli, J.A.; Zenóbio, E.G. Volumetric Dimensional Changes of Autogenous Bone and the Mixture of Hydroxyapatite and Autogenous Bone Graft in Humans Maxillary Sinus Augmentation. A Multislice Tomographic Study. Clin. Oral Implant. Res. 2014, 25, 1251–1256. [Google Scholar] [CrossRef]
- Amerio, P.; Vianale, G.; Reale, M.; Muraro, R.; Tulli, A.; Piattelli, A. The Effect of Deproteinized Bovine Bone on Osteoblast Growth Factors and Proinflammatory Cytokine Production. Clin. Oral Implant. Res. 2010, 21, 650–655. [Google Scholar] [CrossRef]
- Iezzi, G.; Degidi, M.; Scarano, A.; Petrone, G.; Piattelli, A. Anorganic Bone Matrix Retrieved 14 Years after a Sinus Augmentation Procedure: A Histologic and Histomorphometric Evaluation. J. Periodontol. 2007, 78, 2057–2061. [Google Scholar] [CrossRef]
- Carinci, F.; Piattelli, A.; Guida, L.; Perrotti, V.; Laino, G.; Oliva, A.; Annunziata, M.; Palmieri, A.; Pezzetti, F. Effects of Emdogain on Osteoblast Gene Expression. Oral Dis. 2006, 12, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Degidi, M.; Perrotti, V.; Piattelli, A.; Iezzi, G. Sinus Augmentation with Phycogene Hydroxyapatite: Histological and Histomorphometrical Results after 6 Months in Humans. A Case Series. Oral Maxillofac. Surg. 2012, 16, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Nardi, D.; Piattelli, A. Buccal Bone Plate in Immediately Placed and Restored Implant with Bio-Oss(®) Collagen Graft: A 1-Year Follow-up Study. Clin. Oral Implant. Res. 2013, 24, 1201–1205. [Google Scholar] [CrossRef] [PubMed]
- Guazzo, R.; Gardin, C.; Bellin, G.; Sbricoli, L.; Ferroni, L.; Ludovichetti, F.S.; Piattelli, A.; Antoniac, I.; Bressan, E.; Zavan, B. Graphene-Based Nanomaterials for Tissue Engineering in the Dental Field. Nanomaterials 2018, 8, 349. [Google Scholar] [CrossRef] [PubMed]
- Bressan, E.; Ferroni, L.; Gardin, C.; Sbricoli, L.; Gobbato, L.; Ludovichetti, F.S.; Tocco, I.; Carraro, A.; Piattelli, A.; Zavan, B. Graphene Based Scaffolds Effects on Stem Cells Commitment. J. Transl. Med. 2014, 12, 296. [Google Scholar] [CrossRef]
- Mangano, C.; Piattelli, A.; Tettamanti, L.; Mangano, F.; Mangano, A.; Borges, F.; Iezzi, G.; d’Avila, S.; Shibli, J.A. Engineered Bone by Autologous Osteoblasts on Polymeric Scaffolds in Maxillary Sinus Augmentation: Histologic Report. J. Oral Implantol. 2010, 36, 491–496. [Google Scholar] [CrossRef]
- Strocchi, R.; Orsini, G.; Iezzi, G.; Scarano, A.; Rubini, C.; Pecora, G.; Piattelli, A. Bone Regeneration with Calcium Sulfate: Evidence for Increased Angiogenesis in Rabbits. J. Oral Implantol. 2002, 28, 273–278. [Google Scholar] [CrossRef]
- Scarano, A.; Orsini, G.; Pecora, G.; Iezzi, G.; Perrotti, V.; Piattelli, A. Peri-Implant Bone Regeneration with Calcium Sulfate: A Light and Transmission Electron Microscopy Case Report. Implant Dent. 2007, 16, 195–203. [Google Scholar] [CrossRef]
- Serino, G.; Biancu, S.; Iezzi, G.; Piattelli, A. Ridge Preservation Following Tooth Extraction Using a Polylactide and Polyglycolide Sponge as Space Filler: A Clinical and Histological Study in Humans. Clin. Oral Implant. Res. 2003, 14, 651–658. [Google Scholar] [CrossRef]
- Imbronito, A.V.; Scarano, A.; Orsini, G.; Piattelli, A.; Arana-Chavez, V.E. Ultrastructure of Bone Healing in Defects Grafted with a Copolymer of Polylactic/Polyglycolic Acids. J. Biomed. Mater. Res. Part A 2005, 74, 215–221. [Google Scholar] [CrossRef]
- Carinci, F.; Palmieri, A.; Perrotti, V.; Piattelli, A.; Cenzi, R.; Brunell, G.; Martinelli, M.; Arlotti, M.; Pezzetti, F. Genetic Effects of Medpor on Osteoblast-like Cells. J. Craniofac. Surg. 2006, 17, 1243–1250. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Carinci, F.; Assenza, B.; Piattelli, M.; Murmura, G.; Piattelli, A. Vertical Ridge Augmentation of Atrophic Posterior Mandible Using an Inlay Technique with a Xenograft without Miniscrews and Miniplates: Case Series. Clin. Oral Implant. Res. 2011, 22, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Piattelli, A.; Assenza, B.; Quaranta, A.; Perrotti, V.; Piattelli, M.; Iezzi, G. Porcine Bone Used in Sinus Augmentation Procedures: A 5-Year Retrospective Clinical Evaluation. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2010, 68, 1869–1873. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Piattelli, A.; Perrotti, V.; Iezzi, G. Dense Hydroxyapatite Inserted into Postextraction Sockets: A Histologic and Histomorphometric 20-Year Case Report. J. Periodontol. 2008, 79, 929–933. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Pecora, G.; Piattelli, M.; Piattelli, A. Osseointegration in a Sinus Augmented with Bovine Porous Bone Mineral: Histological Results in an Implant Retrieved 4 Years after Insertion. A Case Report. J. Periodontol. 2004, 75, 1161–1166. [Google Scholar] [CrossRef]
- Iezzi, G.; Rubini, C.; Fioroni, M.; Piattelli, A. Peripheral Dentinogenic Ghost Cell Tumor of the Gingiva. J. Periodontol. 2007, 78, 1635–1638. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; de Oliveira, P.S.; Traini, T.; Lorusso, F. Sinus Membrane Elevation with Heterologous Cortical Lamina: A Randomized Study of a New Surgical Technique for Maxillary Sinus Floor Augmentation without Bone Graft. Materials 2018, 11, 1457. [Google Scholar] [CrossRef]
- Scarano, A.; Murmura, G.; Vantaggiato, G.; Lauritano, D.; Silvestre-Rangil, J.; Di Cerbo, A.; Lorusso, F. Delayed Expansion of Atrophic Mandible (Deam): A Case Report. Oral Implantol. 2017, 10, 190–196. [Google Scholar] [CrossRef]
- Chiang, Y.-C.; Wang, Y.-C.; Kung, J.-C.; Shih, C.-J. Antibacterial Silver-Containing Mesoporous Bioglass as a Dentin Remineralization Agent in a Microorganism-Challenged Environment. J. Dent. 2021, 106, 103563. [Google Scholar] [CrossRef]
- Perrotti, V.; Nicholls, B.M.; Horton, M.A.; Piattelli, A. Human Osteoclast Formation and Activity on a Xenogenous Bone Mineral. J. Biomed. Mater. Res. A 2009, 90, 238–246. [Google Scholar] [CrossRef]
- Carinci, F.; Papaccio, G.; Laino, G.; Palmieri, A.; Brunelli, G.; D’Aquino, R.; Graziano, A.; Lanza, V.; Scapoli, L.; Martinelli, M.; et al. Comparison between Genetic Portraits of Osteoblasts Derived from Primary Cultures and Osteoblasts Obtained from Human Pulpar Stem Cells. J. Craniofac. Surg. 2008, 19, 616–625; discussion 626–627. [Google Scholar] [CrossRef] [PubMed]
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Traini et al., Clin Implant Dent Relat Res. 2015 [21] | in the same experimental time, equine group specimens showed evident resorption phenomena, | no or little signs of resorption were evident in the porcine group specimens. | sinus augmentation | Human | 295 patients | Maxillary sinus | Anorganic bovine bone (ABB) Dense hydroxyapatite (dHA) DAC Porous hydroxyapatite (porHA) Cortical/cancellous porcine bone (cortPB) Macroporous biphasic calcium phosphate (Ca2PO4); Demineralized freeze-dried bone allograft (DFDBA) Calcium carbonate (CaCO3); Polymer of polylactic and polyglycolide acids (PLL/PLG) Anorganic bovine bone with synthetic peptide P-15 (P-15) PepGen P-15™; sulphate (CaSO4) Surgiplaster sinus; | - | 6 months |
| Testori et al., Int J Periodontics Restorative Dent. 2012 [16] | excellent properties of particular hydroxyapatite porous microstructure with a high percentage of interconnected micropores that promote the ingrowth of osteogenic cells and vessels, making graft integration easier and faster. | Histomorphometry showed that the percentages of newly formed bone, residual grafted particles, and marrow spaces were 25.1 ± 2.3%, 37.3 ± 1.1%, and 38.5 ± 3.1%, respectively. | Histological and histo—morpho--metrical analysis | human | 1 case bilaterally | split case | High temperature-treated bovine porous hydroxyapatite | - | 9 months |
| Degidi et al., J Oral Implantol. 2013 [13] | Implant placement into extraction sockets can result in favorable radiological results even in the presence of evident alterations of the buccal bone wall. | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone with significant differences with the controls (p < 0.05). | Histological and histo—morpho--metrical analysis | human | 1 patients, 2 sites | split case | Anorganic bovine bone | anorganic bovine matrix added to a cell-binding peptide (PepGen P-15) | 8 years |
| Iezzi et al., Clin Oral Implants Res. 2012 [3] | within the limitations of the present study, the data provided support the fact that all these biomaterials can be used, successfully, in sinus augmentation procedures. | Histomorphometry showed that, in all biomaterials, newly formed bone and residual grafted material particles represented about 30%. | Histological and histo—morpho--metrical analysis | human | 15 patients 30 sinuses, 82 implants | split cases | phycogene hydroxyapatite, biphasic calcium phosphate ceramics, calcium carbonate, porcine bone and anorganic bovine bone | - | 6 months |
| Chackartchi Clin Oral Implants Res. 2011 [19] | Both sizes of BBM granules preformed equally and achieved the aim of the sinus floor augmentation procedure clinically and histologically. | Histo-morpho-metric analysis revealed that both granule sizes produced the same pattern of bone formation, | Histological and histo-morpho-metrical analysis | human | 10 patients/20 sinuses | split cases | two different particle sizes of bovine bone mineral (BBM) | - | 6 months |
| Traini et al., J Periodontol 2007 [22] | The tissue pattern appeared composed by residual ABB particles in close contact to the newly formed bone. The bone mineralized matrix around the ABB had collagen fibers randomly oriented and more osteocytes embedded. The results demonstrate both a high level of osteo-conductivity and a “biomimetic” behavior over the long term. | We observed a mean amount of newly formed bone of 46.0 ± 4.67%, ABB remnants of 16.0 ± 5.89%, and marrow spaces of 38.0 ± 8.93%. The osteocyte index was 4.43 for bone around ABB and 3.27 in the trabecular bone at a distance from the particles. | Histological and histo-morpho-metrical analysis | human | Case Report | Sinus Augmentation | anorganic bovine bone | - | 6 months |
| Orsini et al., Oral Dis 2007 [15] | Bio-Oss particles did not interfere with bone-healing processes after sinus augmentation procedures and promoted new bone formation. This study can help clinicians to understand better the morphological characteristics of bone regeneration processes using Bio-Oss after 20 months and, most importantly, after a longer | Under transmission electron microscopy, it was possible to characterize the bone-biomaterial interface; in the 20-month specimen an electron-dense layer was seen, whereas, almost no electron-dense lines were seen at the interface in the 7-year specimen. | Histological and histo-morpho-metrical analysis, TEM | human | Case Report | Sinus Augmentation | anorganic bovine bone + collagen membrane | - | 6 months |
| Carinci et al., Arch Oral Biol. 2006 [18] | he data reported are, to our knowledge, the first genetic portrait of Bio-Oss effects. They can be relevant to our improved understanding of the molecular mechanism underlying bone regenerative procedures and as a model for comparing other materials with similar clinical effects. | The log2 ratios for all the targets on the array were then calibrated using the normalization factor, and log2 ratios outside the 99.7% confidence interval (the median 3 times S.D. = 0.52) were determined as significantly changed in the treated cells. | Gene expression Microarray | osteoblast-like MG63 cells | In vitro study | Cells culture | anorganic bovine bone | Not treated cells | - |
| Orsini et al., J Biomed Mater Res B Appl Biomater. 2005 [14] | The analyses showed that Bio-Oss particles do not interfere with the normal osseous healing process after sinus lift procedures and promote new bone formation. | newly formed compact bone was present. In the first bone lamella collagen fibers contacting the Bio-Oss surface were oriented at 243.73 ± 7.12 degrees (mean ± SD), while in the rest of the lamella they were oriented at 288.05 ± 4.86 degrees (mean ± SD) with a statistically significant difference of 44.32 degrees (p < 0.001). | Histological and histo-morpho-metrical analysis, TEM, SEM | 12 patients | Human | Sinus Augmentation | anorganic bovine bone | - | 6 months |
| Corinaldesi et al., Br J Oral Maxillofac Surg. 2013 [20] | In this pilot controlled trial of the use of rhBMP-7, histological analyses showed that it resulted in the formation of less bone than treatment with inorganic bovine hydroxyapatite. | Histological and histo-morpho-metric analyses of biopsy specimens showed that there was significantly more new bone on the control side (19.9 (6.8)%) than on the test side (6.6 (4.8)%). | Histological histo-morphometry | Human | 9 patients/18 sinuses | Maxillary sinus | rhBMP-7 (Osigraft) with deproteinized bone substitute (0.5 g on the test side) | deproteinized bone alone (2.0 g on the control side) | 6 months |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Mijiritsky et al., Material 2017 [25] | The controlled release of active growth factors from porcine bone granules can enhance and promote bone regeneration. | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone with significant differences with the controls (p < 0.05). | In vitro MCS Stem cells + Bone porcine granules activity | Rat | 12 | Calvarial defects | MCS Stem cells + Bone porcine granules | Native bone granules | 1 h, 6, 12, 24 h, 3 and 7 days. (in vitro) |
| Giuliani et al., Clin Oral Investig. 2018 [8] | MicroCT revealed that in the grafted sites there were a greater number of trabeculae, | Increase of the SV/TV and of the SNr, with a significant growth from 3 to 6 months from grafting (SV/TV: p = 0.003; SNr: p < 0.001) could be observed. | Porcine Bone MP3 in extraction sockets | Human | 28 | Porcine Bone MP3 in extraction sockets | Porcine Bone MP3 in extraction sockets | Unfilled | 12 months |
| Scarano et al., Biomed res. 2016 [1] | these data suggest that these biomaterials have higher biocompatibility and are capable of inducing faster and greater bone formation. | SEM-EDS analysis showed a Ca/P ratio of 1.8 for BO, 2.2 for EP, and 1.5 for P-15. Under CPLM, BO showed no significant difference for transverse (18.4 ± 2.7%) and longitudinal (16.3 ± 1.8%) bone collagen fibers (p = 0.195); | GBR in iliac sheep crest | sheep | 4 animals | peri implant defects | Porcine cortico-cancellous mix: Equine blocks: Porcine collagenated. | - | 4 months |
| Cassetta et al., Clin Oral Implants Res. 2015 [23] | The clinical and histological results of this study indicated that porcine bone alone or in combination with autologous bone are biocompatible and osteoconductive materials and can be successfully used in sinus augmentation procedures. | Histomorphometry showed that the percentage of newly formed bone was 35.2 ± 3.6%, marrow spaces 35.6 ± 2.3%, and residual grafted material 37.1 ± 3.8%. | Human | Human | 10 patients | Maxillary sinus | 100% autologous bone (Group A), 100% porcine bone (Group B), and a 50:50 mixture of autologous and porcine bone (Group C) | - | 2 months |
| Tetè J Craniofac Surg. 2014 [26] | a more rapid and intense vascularization was achieved in equine bone substitute group, as demonstrated by immunohistochemical analysis for VEGF expression. | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone | sinus augmentation | Human | 10 patients | Maxillary sinus | equine bone, porcine bone | - | 6 months |
| Barone et al., J Periodontol. 2014 [27] | Porcine bone alone or in combination with autologous bone are biocompatible and osteoconductive materials and can be successfully used in sinus augmentation procedures. | Osteoblast grown on Bio-Oss showed a normal RNA expression of osteo--nectin, integrin beta1 and PDGF. | Socket Preservation | Human | 64 patients | Post extractive socket | Flapless | full-thickness mucoperiosteal flap | 2 weeks |
| Traini et al., Clin Implant Dent Relat Res. 2015 [21] | in the same experimental time, equine group specimens showed evident resorption phenomena, | no or little signs of resorption were evident in the porcine group specimens. | sinus augmentation | Human | 295 patients | Maxillary sinus | Anorganic bovine bone (ABB) Dense hydroxyapatite (dHA) DAC Porous hydroxyapatite (porHA) Cortical/cancellous porcine bone (cortPB) Macroporous biphasic calcium phosphate (Ca2PO4); Demineralized freeze-dried bone allograft (DFDBA) Calcium carbonate (CaCO3); Polymer of polylactic and polyglycolide acids (PLL/PLG) Anorganic bovine bone with synthetic peptide P-15 (P-15) PepGen P-15™; sulphate (CaSO4) Surgiplaster sinus; | - | 6 months |
| Iezzi et al., Clin Oral Implants Res. 2012 [3] | within the limitations of the present study, the data provided support the fact that all these biomaterials can be used, successfully, in sinus augmentation procedures. | Histomorphometry showed that, in all biomaterials, newly formed bone and residual grafted material particles represented about 30%. | Histological and histo-morpho-metrical analysis | human | 15 patients 30 sinuses, 82 implants | split cases | phycogene hydroxyapatite, biphasic calcium phosphate ceramics, calcium carbonate, porcine bone and anorganic bovine bone | - | 6 months |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Scarano et al., Biomed res. 2016 [1] | these data suggest that these biomaterials have higher biocompatibility and are capable of inducing faster and greater bone formation. | SEM-EDS analysis showed a Ca/P ratio of 1.8 for BO, 2.2 for EP, and 1.5 for P-15. Under CPLM, BO showed no significant difference for transverse (18.4 ± 2.7%) and longitudinal (16.3 ± 1.8%) bone collagen fibers (p = 0.195); | GBR in iliac sheep crest | sheep | 4 animals | peri implant defects | Porcine cortico-cancellous mix: Equine blocks: Porcine collagenated. | - | 4 months |
| Tetè J Craniofac Surg. 2014 [26] | a more rapid and intense vascularization was achieved in equine bone substitute group, as demonstrated by immunohistochemical analysis for VEGF expression. | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone | sinus augmentation | Human | 10 patients | Maxillary sinus | equine bone, porcine bone | - | 6 months |
| Traini et al., Clin Implant Dent Relat Res. 2015 [21] | in the same experimental time, equine group specimens showed evident resorption phenomena, | no or little signs of resorption were evident in the porcine group specimens. | sinus augmentation | Human | 295 patients | Maxillary sinus | Anorganic bovine bone (ABB) Dense hydroxyapatite (dHA) DAC Porous hydroxyapatite (porHA) Cortical/cancellous porcine bone (cortPB) Macroporous biphasic calcium phosphate (Ca2PO4); Demineralized freeze-dried bone allograft (DFDBA) Calcium carbonate (CaCO3); Polymer of polylactic and polyglycolide acids (PLL/PLG) Anorganic bovine bone with synthetic peptide P-15 (P-15) PepGen P-15™; sulphate (CaSO4) Surgiplaster sinus; | - | 6 months |
| Tete et al., Eur J Histochem. 2013 [29] | It can be concluded that calcium carbonate was shown to be clinically suitable for sinus elevation procedures after 1 to 5 years of follow-up and histologically biocompatible and osteoconductive. | Histomorphometry showed that the percentage of newly formed bone was 35.2 ± 3.6%, marrow spaces 35.6 ± 2.3%, and residual grafted material 37.1 ± 3.8%. | sinus augmentation | Human | 20 patients | Maxillary sinus | equine bone, | autologous | 6 months |
| Artese et al., Implant Dent. 2011 [30] | The results obtained showed that the mixture of autologous and equine bone was biocompatible | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone with significant differences with the controls (p < 0.05). | Histological and histo-morpho-metrical analysis | human | 16 patients | split cases | autologous and equine bone | - | 6 months |
| Perrotti et al., Clin Oral Implants Res. 2009 [31] | This study enables clinicians to tailor the usage of equine spongy bone and presents a model, which can be applied to the preclinical assessment of bone substitute material’s resorbability and resorption rates. | cells were functionally active on equine spongy bone with statistically significant differences compared with the control in the release of tartrate-resistant acid phosphatase (TRAcP5b) at days 14 and 21 of culture. | RT PCR | In vitro culture | Peripheral blood mononuclear cells | Human osteoclasts (OCLs) | equine spongy bone | - | 21 days |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Mangano Int J Oral Maxillofac Implants. 2013 [32] | the mixture of HA and autogenous bone graft showed lower degree of resorption and higher dimensional stability when compared with autogenous bone graft alone, at least at 180 days of healing. | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone with significant differences with the controls (p < 0.05). | sinus augmentation | Human | 12 sites | Maxillary sinus | Macro-porous biphasic-calcium phosphate (MBCP) comprising hydroxyapatite/tricalcium phosphate (HA/TCP) 60/40 | - | 6 months |
| Scarano et al., Int J Oral Maxillofac Implants. 2012 [34] | Data from the preliminary results demonstrated that MBCP is a biocompatible and osteoconductive material that can be successfully used as a grafting material for sinus floor augmentation. | Histologic investigation showed that the macro-porous biphasic calcium phosphate grafted particles were embedded and integrated in the newly formed bone; this bone was in close and tight contact with the biomaterial particles. | Histological and histo-morpho-metrical analysis | rabbit | 6 animals, 24 specimens | rabbit tibiae | algae-derived hydroxyapatite | - | 4 weeks |
| Iezzi et al., Clin Oral Implants Res. 2012 [3] | within the limitations of the present study, the data provided support the fact that all these biomaterials can be used, successfully, in sinus augmentation procedures. | Histomorphometry showed that, in all biomaterials, newly formed bone and residual grafted material particles represented about 30%. | Histological and histo-morpho-metrical analysis | human | 15 patients 30 sinuses, 82 implants | split cases | phycogene hydroxyapatite, biphasic calcium phosphate ceramics, calcium carbonate, porcine bone and anorganic bovine bone | - | 6 months |
| Giuliani et al., Implant Dent. 2016 [24] | The scaffold morphology was confirmed to influence the long-term kinetics of bone regeneration. Considering the whole mineralized | Large amount of newly formed bone was detected in the retrieved specimens, together with a good rate of biomaterial resorption and the formation of a homogeneous and rich net of new vessels. | Synchrotron Radiation X-ray Microtomography | Maxillary sinus | 14 subjects | Block vs particles Tri-calcic Phosphate Beta | - | 8 months | 9 months |
| Mangano et al., Clin Oral Implants Res 2015 [33] | The findings indicated a high biocompatibility and osteo-conductivity of HA-beta-TCP 30/70, for sinus augmentation procedures | The histomorphometric analysis revealed 26 ± 2% of residual grafted biomaterial, 29 ± 3% of newly formed bone, and 45 ± 2% of marrow spaces. | Histological and histo-morpho-metrical analysis | human | 12 patients | Sinus Augmentation | beta-TCP 30/70 | - | 6 months |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Mangano et al., Int J Periodontics Restorative Dent. 2014 [35] | calcium carbonate was shown to be clinically suitable for sinus elevation procedures after 1 to 5 years of follow-up and histologically biocompatible and osteoconductive. | The osteoclast-like cells preferred the small-size BBM particles and not the large particles both in the small-size and the large-size granules group. | sinus augmentation | Human | 24 patients, 68 implants | Maxillary sinus | calcium carbonate | - | 1–5 years |
| Tete et al., Eur J Histochem. 2013 [29] | It can be concluded that calcium carbonate was shown to be clinically suitable for sinus elevation procedures after 1 to 5 years of follow-up and histologically biocompatible and osteoconductive. | Histomorphometry showed that the percentage of newly formed bone was 35.2 ± 3.6%, marrow spaces 35.6 ± 2.3%, and residual grafted material 37.1 ± 3.8%. | sinus augmentation | Human | 20 patients | Maxillary sinus | equine bone, | autologous | 6 months |
| Iezzi et al., Clin Oral Implants Res. 2012 [3] | within the limitations of the present study, the data provided support the fact that all these biomaterials can be used, successfully, in sinus augmentation procedures. | Histomorphometry showed that, in all biomaterials, newly formed bone and residual grafted material particles represented about 30%. | Histological and histo-morpho-metrical analysis | human | 15 patients 30 sinuses, 82 implants | split cases | Phyco-gene hydroxyapatite, biphasic calcium phosphate ceramics, calcium carbonate, porcine bone and anorganic bovine bone | - | 6 months |
| Pettinicchio et al., Aust Dent J. 2012 [37] | the clinical use of heterologous particulate equine-derived biomaterial may ensure long-term predictability of implant-prosthetic rehabilitation | Osteoblast grown on Bio-Oss showed a normal RNA expression of osteo-nectin, integrin beta1 and PDGF. | Scanning electron microscopy (SEM) and energy dispersive X-ray spectroscopy (EDS) | human | 6 specimens | Maxillary sinus | calcium sulphate | - | 6 months |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Scarano et al., Implant Dent. 2006 [2] | All biomaterials examined resulted in being biocompatible and seemed to improve new bone formation in maxillary sinus lift. No signs of inflammation were present. The data are very encouraging because of the high number of successfully treated patients and the good quality of bone found in the retrieved specimens. | Some biomaterials were more resorbable than others. Included are the histomorphometry clarified features of the newly formed bone around the different grafted particles. | Histological and histo-morpho-metrical analysis | human | 94 patients | Sinus Augmentation | demineralized freeze-dried bone allograft Biocoral [Inoteb, St. Gonnery, France], Bio-glass [US Biomaterials, Alachua, FL], Fisiograft [Ghimas, Bologna, Italy], PepGen P-15 [Dentsply Friadent CeraMed, Lakewood, CO], calcium sulfate, Bio-Oss [Geistlich Pharma AG, Wohlhusen, Switzerland] | autologous bone, | 6 months |
| Giuliani Clin Implant Dent Relat Res. 2014 [38] | A full-thickness mucoperiosteal flap gave significantly more negative results than that of the less-demanding flapless procedure, with an increased width resorption of the post-extraction site. | Histo-morpho-metric analysis revealed that both granule sizes produced the same pattern of bone formation, surrounding the graft granules, and producing a shape of a network, “bridging” between the BBM particles. | Posterior jaws defect | Human | 12 patients | Jaws | coralline-derived (bio-coral) scaffold grafts | Beta-tricalcium phosphate and biphasic-calcium phosphate | 6 months |
| Piattelli et al., J Oral Implantol. 2000 [29] | BG seems to be a highly osteoconductive material. | In control sites, bone was observed only in the peripheral areas of the defects, while in test sites, newly formed bone was found around all BG particles, even those located in the central portion of the defect. | Histological histo-morphometry | rabbits | 9 animals | tibial metaphysis | Bio-glass (BG) | Empty defects | 4 weeks |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| Bechara et al., Ann Anat 2015 [44] | both intra-oral autologous bone and ncHA may be elected as inter-positional grafting materials to vertically augment posterior atrophic mandibles. | Bone density and marrow spaces were similar between groups. Correlations between the ISQ values and the histometric variables were not observed (p > 0.05). | Human | Human | 12 patients | Posterior mandible | test group that received an inter-positional inlay resorbable non-ceramic hydroxyapatite | Inter-positional inlay autologous bone graft | 8 months + impant placement |
| Traini et al., Clin Implant Dent Relat Res. 2015 [21] | in the same experimental time, equine group specimens showed evident resorption phenomena, | no or little signs of resorption were evident in the porcine group specimens. | sinus augmentation | Human | 295 patients | Maxillary sinus | Anorganic bovine bone (ABB) Dense hydroxyapatite (dHA) DAC Porous hydroxyapatite (porHA) Cortical/cancellous porcine bone (cortPB) Macroporous biphasic calcium phosphate (Ca2PO4); Demineralized freeze-dried bone allograft (DFDBA) Calcium carbonate (CaCO3); Polymer of polylactic and polyglycolide acids (PLL/PLG) Anorganic bovine bone with synthetic peptide P-15 (P-15) PepGen P-15™; sulphate (CaSO4) Surgiplaster sinus; | - | 6 months |
| Scarano et al., Oral Maxillofac Surg. 2012 [52] | that phycogene hydroxyapatite can be used, successfully, for sinus augmentation procedures. | Histomorphometry showed that the percentage of newly formed bone was 35.2 ± 3.6%, marrow spaces 35.6 ± 2.3%, and residual grafted material 37.1 ± 3.8%. | Histological and histo-morpho-metrical analysis | human | 10 patients | split cases | phycogene hydroxyapatite | - | 6 months |
| Mangano et al., J Oral Implantol. 2006 [43] | After a mean 3 years after implantation, all implants are clinically in function and no surgical or prosthetic complications have occurred. Under light microscopy, newly formed bone was 38.5 ± 4.5%, whereas the residual biomaterial represented 12 ± 2.3% and the marrow spaces represented 44.6 ± 4.2%. | Bone was closely apposed to the biomaterials particles as shown in light microscopy and transmission electron microscopy. | Histological and histo-morpho-metrical analysis | human | 24 subjects | Sinus Augmentation | Porous hydroxyapatite (HA) | - | 6 months |
| Doi et al., PLoS ONE. 2012 [45] | IPCHA/implant complex might be able to achieve both bone reconstruction and implant stability. implant/interconnected porous hydroxyapatite complex as new concept graft material. | The ISQs of complex groups was 77.8 ± 2.9 in the 6-month, 72.0 ± 5.7 in the 3-month and 47.4 ± 11.0 in the 2-month. The BICs of complex groups was 2.18 ± 3.77 in the 2-month, 44.03 ± 29.58 in the 3-month, and 51.23 ± 8.25 in the 6-month. | ISQ measurement, histology | dog femur | 4 animals | jaws defects | implant/interconnected porous hydroxyapatite complex | implants were placed directly into the femur without any bone substrate. | 2, 6 months |
| Scarano et al., Int J Mol Sci. 2018 [46] | composite sticky graft block increased the mechanical properties | Histomorphometry showed that the percentage of newly formed bone was 35.2 ± 3.6%, marrow spaces 35.6 ± 2.3%, and residual grafted material 37.1 ± 3.8%. | Bone Graft Compressive Loading Test | In Vitro | 30 | - | APL + graft, Blood + Graft, Physiologic Water + Graft | - | - |
| Cosso et al., Clin Oral Implants Res. 2014 [48] | Bone density and marrow spaces were similar between groups. | EP showed a significant difference between transverse (4 ± 0.7%) and longitudinal (7.6 ± 2.5%) bone collagen fibers (p = 0.015); | sinus augmentation | Human | 10 patients, 20 sinus augmentation | Maxillary sinus | autogenous bone and the mixture of hydroxyapatite | autogenous bone | 15–180 days |
| Degidi et al., Clin Oral Implants Res. 2013 [53] | None of the evaluated biomaterials seemed to be ideal. | BO showed no significant difference for transverse (18.4 ± 2.7%) and longitudinal (16.3 ± 1.8%) bone collagen fibers (p = 0.195); | Cone-Beam Computed Tomography (CBCT) assessment | Human | 69 implant | jaws 15/25 site | Bio-Oss(®) collagen graft: | - | 12 months |
| Testori et al., Int J Periodontics Restorative Dent. 2012 [16] | Excellent properties of particular hydroxyapatite porous microstructure with a high percentage of interconnected micropores that promote the ingrowth of osteogenic cells and vessels, making graft integration easier and faster. | Histomorphometry showed that the percentages of newly formed bone, residual grafted particles, and marrow spaces were 25.1 ± 2.3%, 37.3 ± 1.1%, and 38.5 ± 3.1%, respectively. | Histological and histo-morpho-metrical analysis | human | 1 case bilaterally | human | High temperature-treated bovine porous hydroxyapatite | - | 9 months |
| Degidi et al., J Oral Implantol. 2013 [13] | Implant placement into extraction sockets can result in favorable radiological results even in the presence of evident alterations of the buccal bone wall. | The higher and lower intensities of vascular endothelial growth factor and NOS3 expression were prevalent in the sites grafted with autologous bone with significant differences with the controls (p < 0.05). | Histological and histo-morph-ometrical analysis | human | 1 patients, 2 sites | split case | Anorganic bovine bone | anorganic bovine matrix added to a cell-binding peptide (PepGen P-15) | 8 years |
| Chackartchi Clin Oral Implants Res. 2011 [19] | Both sizes of BBM granules preformed equally and achieved the aim of the sinus floor augmentation procedure clinically and histologically. | Histo-morpho-metric analysis revealed that both granule sizes produced the same pattern of bone formation, | Histological and histo-morpho-metrical analysis | human | 10 patients/20 sinuses | split cases | two different particle sizes of bovine bone mineral (BBM) | - | 6 months |
| Pettinicchio Clin Oral Investig. 2012 [36] | Bio-Oss® (BO), Engipore® (EP), and PepGen P-15® (P-15). BO particles appeared perfectly osseo-integrated in the trabecular bone. | EP showed a significant difference between transverse (4 ± 0.7%) and longitudinal (7.6 ± 2.5%) bone collagen fibers (p = 0.015); | Histological and histo-morpho-metrical analysis | human | 20 patients | human | Bio-Oss® (BO), Engipore® (EP), and PepGen P-15® (P-15) | - | 6 months |
| Amerio et al., Clin Oral Implants Res. 2010 [49] | Our findings further support the evidence that Bio-Oss is an excellent biomaterial that does not enhance the production of proinflammatory cytokines. | Compared with control osteoblasts it showed a reduced expression of BSP, BMP-2 and BMP-7, IL-6 and TNF-alpha. | RT PCR | In Vitro | Cell cultures | In vitro | Bio-Oss® (BO) + osteoblast | - | 7, 14, 21 days |
| Iezzi et al., J Periodontol 2007 [50] | Vital, mature bone was formed and maintained over a long period with no chronic inflammatory cell infiltrate, foreign body response, or other adverse effects. | Histomorphometry showed that the mean amount of mature, compact bone was 71.0 ± 2.28%, the mean amount of ABM was 22.1 ± 3.18%, and the mean amount of marrow spaces was 11.2 ± 5.42%. | Histological and histo-morpho-metrical analysis | human | Case Report | Sinus Augmentation | Anorganic bone matrix | - | 6 months |
| Traini et al., J Periodontol 2007 [22] | The tissue pattern appeared composed by residual ABB particles in close contact to the newly formed bone. The bone mineralized matrix around the ABB had collagen fibers randomly oriented and more osteocytes embedded. The results demonstrate both a high level of osteo-conductivity and a “biomimetic” behavior over the long term. | We observed a mean amount of newly formed bone of 46.0 ± 4.67%, ABB remnants of 16.0 ± 5.89%, and marrow spaces of 38.0 ± 8.93%. The osteocyte index was 4.43 for bone around ABB and 3.27 in the trabecular bone at a distance from the particles. | Histological and histo-morpho-metrical analysis | human | Case Report | Sinus Augmentation | anorganic bovine bone | - | 6 months |
| Orsini et al., Oral Dis 2007 [15] | Bio-Oss particles did not interfere with bone-healing processes after sinus augmentation procedures and promoted new bone formation. This study can help clinicians to understand better the morphological characteristics of bone regeneration processes using Bio-Oss after 20 months and, most importantly, after a longer | . Under transmission electron microscopy, it was possible to characterize the bone-biomaterial interface; in the 20-month specimen an electron-dense layer was seen, whereas, almost no electron-dense lines were seen at the interface in the 7-year specimen. | Histological and histo-morpho-metrical analysis, TEM | human | Case Report | Sinus Augmentation | anorganic bovine bone + collagen membrane | - | 6 months |
| Carinci et al., Arch Oral Biol. 2006 [18] | he data reported are, to our knowledge, the first genetic portrait of Bio-Oss effects. They can be relevant to our improved understanding of the molecular mechanism underlying bone regenerative procedures and as a model for comparing other materials with similar clinical effects. | The log2 ratios for all the targets on the array were then calibrated using the normalization factor, and log2 ratios outside the 99.7% confidence interval (the median 3 times S.D. = 0.52) were determined as significantly changed in the treated cells. | Gene expression Microarray | osteoblast-like MG63 cells | In vitro study | Cell culture | anorganic bovine bone | Not treated cells | - |
| Orsini et al., J Biomed Mater Res B Appl Biomater. 2005 [14] | The analyses showed that Bio-Oss particles do not interfere with the normal osseous healing process after sinus lift procedures and promote new bone formation. | newly formed compact bone was present. In the first bone lamella collagen fibers contacting the Bio-Oss surface were oriented at 243.73 ± 7.12 degrees (mean ± SD), while in the rest of the lamella they were oriented at 288.05 ± 4.86 degrees (mean ± SD) with a statistically significant difference of 44.32 degrees (p < 0.001). | Histological and histo-morpho-metrical analysis, TEM, SEM | 12 patients | Human | Sinus Augmentation | anorganic bovine bone | - | 6 months |
| Mangano et al., J Oral Implantol. 2006 [43] | Intimate binding between bone and HA particles was present after a long-term implantation period (20 years). The fact that HA particles were surrounded closely by bone is very promising for the long-term stability of the augmentation. | Histomorphometry showed that bone represented 25.4 ± 3.2%, marrow spaces represented 41.3 ± 5.2%, and residual HA particles represented 38.1 ± 4.1%. | Histological and histo-morpho-metrical analysis | human | Case report | Post-extraction sockets | Dense hydroxyapatite | - | 6 months |
| Authors | Study Findings | Results | Biomaterials and Methodologies Characteristics | Study Model Model | Sample Size | Defect | Test Group | Control Group | Timepoints |
|---|---|---|---|---|---|---|---|---|---|
| [54] | - | - | - | - | - | - | - | - | - |
| Scarano et al., Biomed res int 2016 [1] | APG with β-TCP preserves skin morphology, without immune response, with an excellent tolerability and is a promising scaffold for cells and biomaterial for soft tissue augmentation. β-TCP added with APG was able to increase the bio-stimulating effect on fibroblasts and quicken resorption. | The margins of β-TCP granules were clear and not diffused near tissues. | The aim of the study was to evaluate microporous tricalcium phosphate (β-TCP) and autologous platelet gel (APG) mix in mice for oral and maxillofacial soft tissue augmentation. | in vivo Mice | 10 | Cheek | β-TCP/APG gel was injected into one cheek | β-TCP/APG gel was injected into one cheek; the other was used as control | - |
| [55] | - | - | - | - | - | - | - | - | - |
| Doi et al., PLoS ONE. 2012 [45] | IPCHA/implant complex might be able to achieve both bone reconstruction and implant stability. implant/interconnected porous hydroxyapatite complex as new concept graft material. | The ISQs of complex groups was 77.8 ± 2.9 in the 6-month, 72.0 ± 5.7 in the 3-month and 47.4 ± 11.0 in the 2-month. The BICs of complex groups was 2.18 ± 3.77 in the 2-month, 44.03 ± 29.58 in the 3-month, and 51.23 ± 8.25 in the 6-month. | ISQ measurement, histology | dog femur | 4 animals | jaws defects | implant/interconnected porous hydroxyapatite complex | implants were placed directly into the femur without any bone substrate. | 2, 6 months |
| Corinaldesi et al., Br J Oral Maxillofac Surg. 2013 [20] | In this pilot controlled trial of the use of rhBMP-7, histological analyses showed that it resulted in the formation of less bone than treatment with inorganic bovine hydroxyapatite. | Histological and histo-morpho-metric analyses of biopsy specimens showed that there was significantly more new bone on the control side (19.9 (6.8)%) than on the test side (6.6 (4.8)%). | Histological histo-morphometry | Human | 9 patients/18 sinuses | Maxillary sinus | rhBMP-7 (Osigraft) with deproteinized bone substitute (0.5 g on the test side) | deproteinized bone alone (2.0 g on the control side) | 6 months |
| Mangano et al., J Oral Implantol. 2010 [56] | Data from this case report demonstrate that the newly formed bone provided by engineered bone tissue | Augmented maxillary sinus with engineered bone presented a mean of 28.89% and 71.11% of bone and medullary spaces, respectively. | Histological histo-morphometry | Human | Case report | Maxillary sinus | autologous osteoblasts on polymeric scaffolds | - | 6 months |
| Strocchi et al., J Oral Implantol. 2002 [57] | The presence of more blood vessels in the sites treated with CS could help to explain the good results reported in the literature with the use of CS. | The defects in group 3 (3 rabbits) were filled with autologous bone. A total of 54 defects were filled (18 with CS and e-PTFE membranes, 18 with CS alone, and 18 with autologous bone). No postoperative deaths or complications occurred. All nine animals were sacrificed at 4 weeks. MVD results were as follows: in the first group, 9.88 ± 4.613; in the second group, 7.92 ± 1.998; and in the third group, 5.56 ± 1.895. p = 0.000 was highly significant. | Histological histo-morphometry | rabbits | 9 animals | tibial metaphysis | he defects were filled in a random way. The defects of group 1 (3 rabbits) were filled with CS granules (Surgiplaster, Classimplant, Rome, Italy) and covered with e-PTFE membranes. The defects in group 2 (3 rabbits) were filled with CS granules (Surgiplaster). The defects in group 3 (3 rabbits) were filled | autologous bone. | 4 weeks |
| Scarano et al., Implant Dent. 2007 [58] | The results confirm the high biocompatibility and rapid resorption of calcium sulfate. | In light microscopy, trabecular bone was present. No remnants of calcium sulfate were present. Transmission electron microscopy showed, in the areas of the interface with the implant surface, features of mature bone with many osteocytes. | Histological histo-morphometry, SEM | Human | Case report | Peri-implant defect | Calcium sulfate | - | 6 months |
| Serino et al., Clin Oral Implants Res. 2003. [59] | Alveolar bone resorption following tooth extraction may be prevented or reduced by the use of a bioabsorbable synthetic sponge of polylactide-polyglycolide acid. The quality of bone formed seemed to be optimal for dental implant insertion. | the mesial-buccal site, a loss of bone height of 0.2 mm (1.4 SD) in the test and 0.6 mm (1.1 SD) in the controls; in the mid-buccal portion a gain of 1.3 mm (1.9 SD) in the test and a loss of 0.8 mm (1.6 SD) in the controls; and in the distal portion a loss of 0.1 mm (1.1 SD) in the test and of 0.8 (1.5 SD) mm in the controls. | Histological histomorphometry, | Human | 36 subjects | polylactide and polyglycolide sponge | Empty defect | - | 6 months |
| Imbronito et al., J Biomed Mater Res A. 2005 [60] | In areas where the degrading copolymer formed accumulates, an amorphous multilayered material was identified between the connective tissue and the copolymer. In summary, the copolymer of PLA/PGA studied appears to be an osteoconductive material when it is used to fill bone defects. | In areas where the degrading copolymer was present in small amounts, newly formed bone matrix was detected; it was deposited by osteoblast-like cells in close relation to the copolymer | Histological histo-morphometry, | 5 Rabbits | 36 subjects | Maxillary sinus | polylactide and polyglycolide sponge | Empty defect | 60 days |
| Carinci et al., J Craniofac Surg. 2006 [61] | he data reported are, to our knowledge, the first genetic portrait of osteoblast-like cells cultured on PP. They are relevant to better understanding of the molecular mechanism of bone-PP interaction and as a model for comparing other materials used for bone reconstruction. | (1) signal transduction, (2) transcription, (3) translation, (4) cell cycle regulation, (5) vesicular transport, and (6) production of cytoskeletal elements, cell-adhesion molecules and extracellular matrix components. | DNA microarrays | In vitro culture | osteoblast-like cells | osteoblast-like cell lines (i.e., MG-63) | Porous polyethylene | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tumedei, M.; Mijiritsky, E.; Mourão, C.F.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. Histological and Biological Response to Different Types of Biomaterials: A Narrative Single Research Center Experience over Three Decades. Int. J. Environ. Res. Public Health 2022, 19, 7942. https://doi.org/10.3390/ijerph19137942
Tumedei M, Mijiritsky E, Mourão CF, Piattelli A, Degidi M, Mangano C, Iezzi G. Histological and Biological Response to Different Types of Biomaterials: A Narrative Single Research Center Experience over Three Decades. International Journal of Environmental Research and Public Health. 2022; 19(13):7942. https://doi.org/10.3390/ijerph19137942
Chicago/Turabian StyleTumedei, Margherita, Eitan Mijiritsky, Carlos Fernando Mourão, Adriano Piattelli, Marco Degidi, Carlo Mangano, and Giovanna Iezzi. 2022. "Histological and Biological Response to Different Types of Biomaterials: A Narrative Single Research Center Experience over Three Decades" International Journal of Environmental Research and Public Health 19, no. 13: 7942. https://doi.org/10.3390/ijerph19137942
APA StyleTumedei, M., Mijiritsky, E., Mourão, C. F., Piattelli, A., Degidi, M., Mangano, C., & Iezzi, G. (2022). Histological and Biological Response to Different Types of Biomaterials: A Narrative Single Research Center Experience over Three Decades. International Journal of Environmental Research and Public Health, 19(13), 7942. https://doi.org/10.3390/ijerph19137942











