Coping with the Experience of Bad Sleep and Fatigue Associated with the Nursing Clinical Practicum
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Sample
2.4. Instrument
2.4.1. Open-Ended Question Questionnaire
2.4.2. Beck Anxiety Inventory
2.5. Procedure
2.6. Ethical Considerations
2.7. Data Analysis
2.8. Rigor for Qualitative Data
3. Results
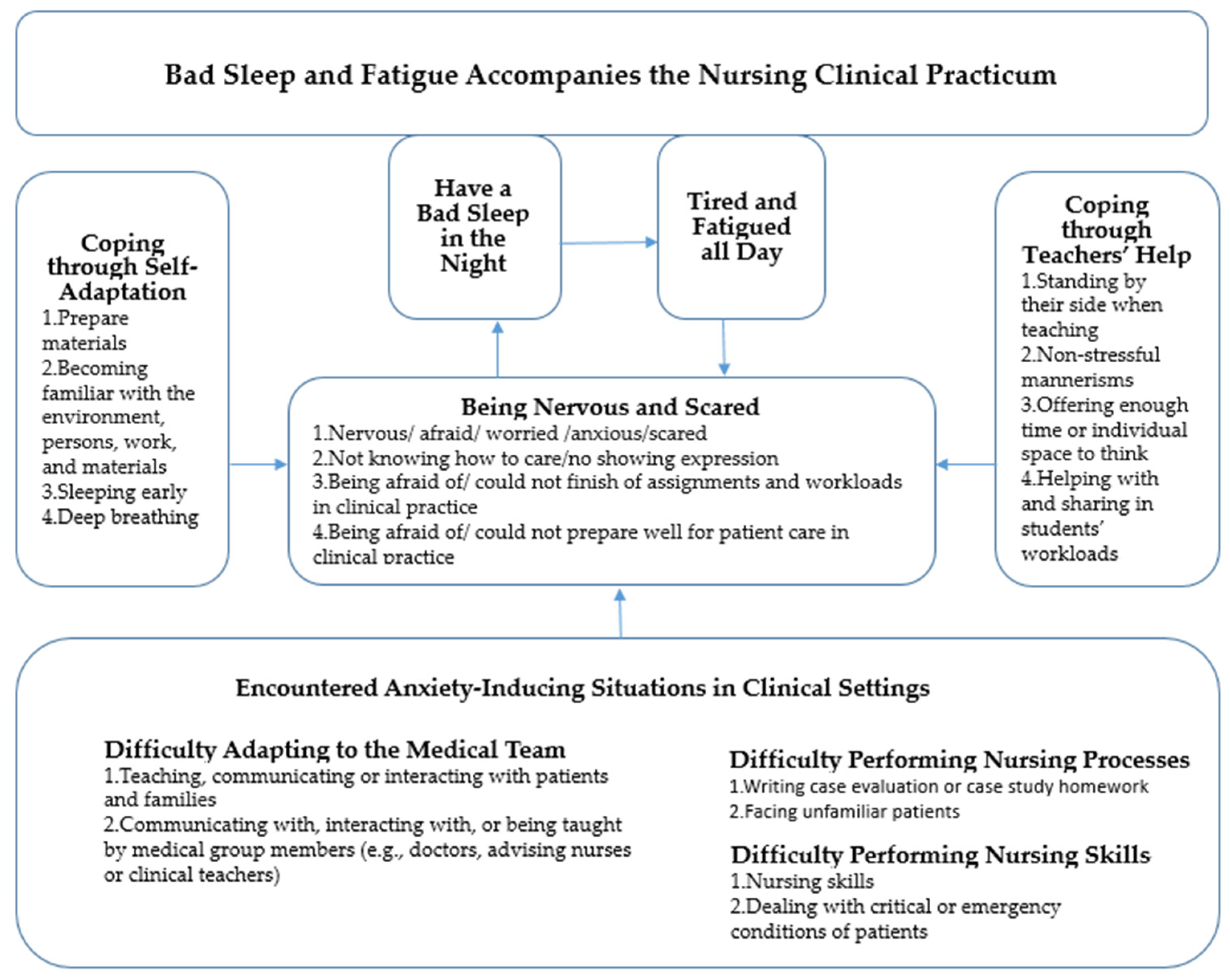
- Theme 1: Encountered Anxiety-Inducing Situations in Clinical Settings
- Sub-theme 1: Difficulty Adapting to the Medical Team
- Teaching, communicating, or interacting with patients and families
- 2.
- Communicating with, interacting with, or being taught by medical group members (e.g., doctors, advising nurses, or clinical teachers)
- Sub-theme 2: Difficulty Performing Nursing Processes
- 1.
- Writing case evaluation or case study homework
- 2.
- Facing unfamiliar patients
- Sub-theme 3: Difficulty Performing Nursing Skills
- 1.
- Nursing skills
- 2.
- Dealing with critical or emergency conditions of patients
- Theme 2: Being Nervous and Scared
- Sub-theme 1: Nervous/afraid/worried/anxious/scared
- Sub-theme 2: Not knowing how to care/not showing expression
- Sub-theme 3: Being afraid of/could not finish assignments and workload in clinical practice
- Sub-theme 4: Being afraid of/could not prepare well for patient care in clinical practice
- Theme 3: Coping through Self-Adaption
- Sub-theme 1: Preparing materials
- Sub-theme 2: Becoming familiar with the environment, persons, work, and materials
- Sub-theme 3: Sleeping early
- Sub-theme 4: Deep breathing
- Theme 4: Coping through Teachers’ Help
- Sub-theme 1: Standing by their side when teaching
- Sub-theme 2: Non-stressful mannerisms
- Sub-theme 3: Offering enough time or individual space to think
- Sub-theme 4: Helping with and sharing in students’ workloads
- Theme 5: Have a Bad Sleep in the Night
- Theme 6: Tired and Fatigued all Day
4. Discussion
4.1. Bad Sleep and Fatigue Accompanied Students in the Nursing Clinical Practicum
4.2. Encountering Anxiety-Inducing Situations in Clinical Setting Made Nursing Students Feel Nervous and Scared
4.3. Coping Style of Nursing Students: Self-Adaptation and Teachers’ Help
5. Limitations and Strengths
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kuntarti Rustina, Y.; Umar, J.; Irawati, D. Concept Analysis of Caring Personality for Nursing: A Review. Pertanika J. Soc. Sci. Humanit. 2020, 28, 2485–2504. [Google Scholar] [CrossRef]
- Nesje, K. Personality and professional commitment of students in nursing, social work, and teaching: A comparative survey. Int. J. Nurs. Stud. 2016, 53, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Makarova, O.; Kovardakova, M.; Shabanova, A. Professional Competence as an Essential Characteristic of a University Student’s Personality. Advances in Social Science. Educ. Humanit. Res. 2022, 646, 264–272. [Google Scholar]
- Luo, Y.; Meng, R.; Li, J.; Liu, B.; Cao, X.; Ge, W. Self-compassion may reduce anxiety and depression in nursing students: A pathway through perceived stress. Public Health 2019, 174, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.H.; Lee, C.T.; Espin, S. Undergraduate nursing students’ experiences of anxiety-producing situations in clinical practicums: A descriptive survey study. Nurse Educ. Today 2019, 76, 103–108. [Google Scholar] [CrossRef]
- Tang, C.Y. Learning Experience of Chinese Nursing Students during Clinical Practicum: A Descriptive Qualitative Study. Nurs. Rep. 2021, 11, 495–505. [Google Scholar] [CrossRef]
- Wang, L.H.; Lin, C.C.; Han, C.Y.; Huang, Y.L.; Hsiao, P.R.; Chen, L.C. Undergraduate nursing student academic resilience during medical surgical clinical practicum: A constructivist analysis of Taiwanese experience. J. Prof. Nurs. 2021, 37, 521–528. [Google Scholar] [CrossRef]
- Graj, E.; Sheen, J.; Dudley, A.; Wendy Sutherland-Smith, W. Adverse health events associated with clinical placement: A systematic review. Nurse Educ. Today 2019, 76, 178–190. [Google Scholar] [CrossRef]
- Nickerson, C. Yerkes-Dodson Law. Simply Psychology. 15 November 2021. Available online: www.simplypsychology.org/what-is-the-yerkes-dodson-law.html (accessed on 15 November 2021).
- Al-Ghareeb, A.; McKenna, L.; Cooper, S. The influence of anxiety on student nurse performance in a simulated clinical setting: A mixed methods design. Int. J. Nurs. Stud. 2019, 98, 57–66. [Google Scholar] [CrossRef]
- Polat, S.; Kutlu, L.; Ay, F.; Purisa, S.; Erkan, H.A. Decision-making styles, anxiety levels, and critical thinking levels of nurses. Jpn. J. Nurs. Sci. 2019, 16, 309–321. [Google Scholar] [CrossRef]
- Dalcali, B.K.; Durgun, H.; Taş, A.S. Anxiety levels and sleep quality in nursing students during the COVID-19 pandemic. Perspect. Psychiatr. Care 2021, 57, 1999–2005. [Google Scholar] [CrossRef] [PubMed]
- Sandler, C.X.; Lloyd, A.R. Chronic fatigue syndrome: Progress and possibilities. Med. J. Aust. 2020, 212, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Yiğitalp, G.; Aydın, L.Z. Determination of sleep quality, fatigue and related factors in nursing students. J. Nurs. Midwifery Sci. 2021, 8, 212–218. [Google Scholar] [CrossRef]
- Pourabdian, S.; Lotfi, S.; Yazdanirad, S.; Golshiri, P.; Hassanzadeh, A. Evaluation of the effect of fatigue on the coping behavior of international truck. Psychology 2020, 8, 70. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; Shu, Q.; Cui, Q.; Wang, L.; Liu, C.; Wu, H. The Mediating Role of Psychological Capital in the Relationship Between Occupational Stress and Fatigue: A Cross-Sectional Study Among 1104 Chinese Physicians. Front. Public Health 2020, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Mark, G.; Smith, A.P. Coping and Its Relation to Gender, Anxiety, Depression, Fatigue, Cognitive Difficulties and Somatic Symptoms. J. Educ. Soc. Behav. Sci. 2018, 25, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, Y.; Cusack, L. Undergraduate nursing students’ strategies for coping with their first clinical placement: Descriptive survey study. Nurse Educ. Today 2018, 69, 104–108. [Google Scholar] [CrossRef]
- Liu, J.; Yang, Y.; Chen, J.; Zhan, Y.; Zeng, Y.; Li, J. Stress and coping styles among nursing students during the initial period of the clinical practicum: A cross-section study. Int. J. Nurs. Sci. 2022, 9, 222–229. [Google Scholar] [CrossRef]
- Creswell, J.W.; Klassen, A.C.; Plano Clark, V.L.; Smith, K.C. Best Practices for Mixed Methods Research in the Health Sciences. National Institutes of Health. Available online: https://obssr.od.nih.gov/sites/obssr/files/Best_Practices_for_Mixed_Methods_Research.pdf (accessed on 1 November 2021).
- Tashakkori, A.; Teddlie, C. SAGE Handbook of Mixed Methods in Social & Behavioral Research, 2nd ed.; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Strauss, A.; Corbin, J. Basics of Qualitative Research: Grounded Theory Procedures & Techniques; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 1990. [Google Scholar]
- Charmaz, K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2006. [Google Scholar]
- Ligita, T.; Harvey, N.; Wicking, K.; Nurjannah, I.; Francis, K. A practical example of using theoretical sampling throughout a grounded theory study A methodological paper. Qual. Res. J. 2020, 20, 116–126. [Google Scholar] [CrossRef]
- Teychenne, M.; Ball, K.; Salmon, J. Promoting Physical Activity and Reducing Sedentary Behavior in Disadvantaged Neighborhoods: A Qualitative Study of What Women Want. PLoS ONE 2012, 7, e49583. [Google Scholar] [CrossRef][Green Version]
- Sullivan-Bolyai, S.; Bova, C.; Harper, D. Developing and refining interventions in persons with health disparities: The use of Qualitative Description. Nurs. Outlook 2005, 53, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Che, H.H.; Lu, M.L.; Chen, H.C.; Chang, S.W.; Lee, Y.J. Validation of the Chinese version of the beck anxiety inventory. Formos. J. Med. 2006, 10, 447–454. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef]
- Aldiabat, K.M.; Le Navenec, C. Data staturation: The mysterious step in Grounded Theory methodology. Qual. Rep. 2018, 23, 245–261. [Google Scholar]
- Ryan-Nicholls, K.D.; Will, C.I. Rigor in qualitative research: Mechanisms for control. Nurse Res. 2009, 16, 70–85. [Google Scholar] [CrossRef]
- Thomas, E.; Magilvy, J.K. Qualitative rigor or research validity in qualitative research. J. Spec. Pediatr. Nurs. 2011, 16, 151–155. [Google Scholar] [CrossRef]
- Pitsavos, C.; Panagiotakos, D.B.; Papageorgiou, C.; Tsetsekou, E.; Soldatos, C.; Stefanadis, C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: The ATTICA Study. Atherosclerosis 2006, 185, 320–326. [Google Scholar] [CrossRef]
- Vogelzangs, N.; Beekman, A.T.F.; de Jonge, P.; Penninx, B.W.J.H. Anxiety disorders and inflammation in a large adult cohort. Transl. Psychiatry 2013, 3, e249. [Google Scholar] [CrossRef]
- Yang, L.; Wang, M.; Guo, Y.Y.; Sun, T.; Li, Y.J.; Yang, Q.; Zhang, K.; Liu, S.B.; Zhao, M.G.; Wu, Y.M. Systemic inflammation induces anxiety disorder through CXCL12/CXCR4 pathway. Brain Behav. Immun. 2016, 56, 352–362. [Google Scholar] [CrossRef]
- Martin, S.; Vincent, A.; Taylor, A.W.; Atlantis, E.; Jenkins, A.; Januszewski, A.; O’Loughlin, P.; Wittert, G. Lower urinary tract symptoms, depression, anxiety and systemic inflammatory factors in men: A population-based cohort study. PLoS ONE 2015, 10, e0137903. [Google Scholar] [CrossRef]
- Song, L.; Quan, X.; Su, L.; Wang, K.; Wang, H.; Wu, L.; Chen, C.; Li, S.; Xiang, W.; Chen, L.; et al. Inflammation and behavioral symptoms in preoperational glioma patients: Is depression, anxiety, and cognitive impairment related to markers of systemic inflammation? Brain Behav. 2020, 10, e01771. [Google Scholar] [CrossRef] [PubMed]
- Michopoulos, V.; Powers, A.; Gillespie, C.F.; Ressler, K.J.; Jovanovic, T. Inflammation in fear- and anxiety-based disorders: PTSD, GAD, and beyond. Neuropsychopharmacol. Rev. 2017, 42, 254–270. [Google Scholar] [CrossRef] [PubMed]
- Kalyani, M.N.; Jamshidi, N.; Molazem, Z.; Torabizadeh, C.; Sharif, F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open 2019, 9, e028052. [Google Scholar] [CrossRef] [PubMed]
- Mamaghani, E.A.; Rahmani, A.; Hassankhani, H.; Zamanzadeh, V.; Campbell, S.; Fast, O.; Irajpour, A. Experiences of Iranian Nursing Students Regarding Their Clinical Learning Environment. Asian Nurs. Res. 2018, 12, 216–222. [Google Scholar] [CrossRef]
- Baluwa, M.A.; Lazaro, M.; Mhango, L.; Msiska, G. Stress and Coping Strategies Among Malawian Undergraduate Nursing Students. Adv. Med. Educ. Pract. 2021, 12, 547–556. [Google Scholar] [CrossRef]
- Woodward, S.; Hendy, C. Leading and coping with change. J. Chang. Manag. 2004, 4, 155–183. [Google Scholar] [CrossRef]
- Sucuoğlu, E.; Muhammad Bello Nawaila, M.B.; Stella Mseer Shimave, S.M. Gender Difference and Test Anxiety: A Case Study of First Year Psychology and Nursing Students. Int. J. Sci. Res. 2017, 73, 229–243. [Google Scholar] [CrossRef]
- Ortega, R.H.; Pascual, J.L.G.; Araque, A.M.F. Impact of an intervention program with reinforcement on nursing students’ stress and anxiety levels in their clinical practices. Nurse Educ. Pract. 2021, 55, 103179. [Google Scholar] [CrossRef]
- Vurala, P.I.; Körpea, G.; Inangilb, D. Emotional freedom techniques (EFT) to reduce exam anxiety in Turkish nursing students. Eur. J. Integr. Med. 2019, 32, 101002. [Google Scholar] [CrossRef]
- Cornine, A. Reducing Nursing Student Anxiety in the Clinical Setting: An Integrative Review. Nurs. Educ. Perspect. 2020, 41, 229–234. [Google Scholar] [CrossRef]
- Aloufi, M.A.; Jarden, R.J.; Gerdtz, M.F.; Kapp, S. Reducing stress, anxiety and depression in undergraduate nursing students: Systematic review. Nurse Educ. Today 2021, 102, 104877. [Google Scholar] [CrossRef] [PubMed]
- Kennya, L.-A.T.; Gastona, T.; Powersa, K.; Ashley Isaac-Dockeryb, A. Anxiety in nursing students: The impact of using mobile technology with quick response codes. Nurse Educ. Today 2020, 89, 104382. [Google Scholar] [CrossRef] [PubMed]
- Derya, Y.A.; Akça, E.I.; Özsahin, Z.; Kapidere, M. Integration of technology to clinical teaching: The impact of mobile and web-based software automation designed for midwifery students on motivation, time management and anxiety levels. Midwifery 2022, 106, 103248. [Google Scholar] [CrossRef]
- Shahsavari, H.; Shahrzad Ghiyasvandian, S.; Houser, M.L.; Zakerimoghadam, M.; Kermanshahi, S.S.N. Effect of a clinical skills refresher course on the clinical performance, anxiety and self-efficacy of the final year undergraduate nursing students. Nurse Educ. Pract. 2017, 27, 151–156. [Google Scholar] [CrossRef]
- Kachaturoff, M.; Caboral-Stevens, M.; Gee, M.; Lan, V.M. Effects of peer-mentoring on stress and anxiety levels of undergraduate nursing students: An integrative review. J. Prof. Nurs. 2020, 36, 223–228. [Google Scholar] [CrossRef]
- Ioannou, A.; Papastavrou, E.; Charalambous, A. Virtual Reality and Symptoms Management of Anxiety, Depression, Fatigue, and Pain: A Systematic Review. Open Nurs. 2020, 6, 2377960820936163. [Google Scholar] [CrossRef]
- Devi, H.M.; Purborini, N.; Chang, H.-J. Mediating effect of resilience on association among stress, depression, and anxiety in Indonesian nursing students. J. Prof. Nurs. 2021, 37, 706–713. [Google Scholar] [CrossRef]
- Savitsky, B.; Findling, Y.; Ereli, A.; Tova Hendel, T. Anxiety and coping strategies among nursing students during the COVID-19 pandemic. Nurse Educ. Pract. 2020, 46, 102809. [Google Scholar] [CrossRef]
- AtienzaJacob, M.; Cantero, Z.L. Low-grade inflammation in the relationship between sleep disruption, dysfunctional adiposity, and cognitive decline in aging. Sleep Med. Rev. 2018, 42, 171–183. [Google Scholar] [CrossRef]
- Lasselin, J.; Layé, S.; Dexpert, S.; Aubert, A.; Gonzalez, C.; Gin, H.; Capuron, L.; Fatigue, C.L. symptoms relate to systemic inflammation in patients with type 2 diabetes. Brain Behav. Immun. 2012, 26, 1211–1219. [Google Scholar] [CrossRef]
| Variables | n (%) | Pre-Practicum M (S.D.) | Post-Practicum M (S.D.) |
|---|---|---|---|
| Age | 37 (100) | 10.21 (6.87) | 11.62 (6.13) |
| Nursing program | |||
| 4-year BSN | 8 (21.6) | 13.88 (8.10) | 13.63 (4.50) |
| 2-year BSN | 13 (35.1) | 10.15 (6.93) | 10.31 (5.60) |
| 5-year ABSN | 16 (43.2) | 8.69 (5.88) | 11.69 (7.22) |
| Practice setting | |||
| Med. and sur. | 18 (48) | 8.39 (6.00) | 12.06 (7.27) |
| Obs. | 8 (21.6) | 11.38 (7.33) | 11.00 (7.17) |
| Ped. | 2 (5.4) | 9.50 (0.71) | 9.50 (2.12) |
| Psy. | 4 (10.8) | 15.00 (8.37) | 9.50 (1.29) |
| Com. | 5 (13.5) | 12.20 (8.90) | 13.60 (2.88) |
| BAI components (pre) | |||
| Neurophysiological symptoms | 30 (81.1) | 11.93 (6.54) | 10.33 (4.89) |
| Autonomic symptoms | 34 (91.9) | 11.15 (6.54) | 11.71 (6.39) |
| Subjective symptoms | 24 (64.9) | 13.50 (6.28) | 10.46 (5.48) |
| Panic symptoms | 32 (86.5) | 11.28 (6.75) | 11.69 (6.50) |
| BAI components (post) | |||
| Neurophysiological symptoms | 34 (91.9) | 9.82 (6.86) | 12.32 (5.69) |
| Autonomic symptoms | 35 (94.6) | 10.14 (7.01) | 12.29 (5.61) |
| Subjective symptoms | 26 (70.3) | 10.65 (7.53) | 13.35 (6.14) |
| Panic symptoms | 34 (91.9) | 9.68 (6.54) | 12.35 (5.68) |
| Practicum-related anxiety symptom | 13 (35.1) | 10.62 (7.70) | 11.23 (6.33) |
| Fatigue | 3 (8.1) | 7.67 (2.52) | 8.67 (1.15) |
| Bad sleep | 2 (5.4) | 2.50 (3.54) | 9.00 (1.41) |
| Nervous and scared | 10 (27.0) | 12.30 (7.73) | 11.80 (7.18) |
| Coping strategy used | 23 (62.2) | 13.13 (6.98) | 12.13 (6.12) |
| Self-adaptation | 3 (8.1) | 6.33 (3.51) | 11.00 (2.65) |
| Teachers’ help | 21 (56.8) | 13.95 (6.72) | 12.19 (6.37) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, M.-H.; Tzeng, C.-Y.; Chuang, Y.-H.; Chang, P.-C.; Chung, M.-H. Coping with the Experience of Bad Sleep and Fatigue Associated with the Nursing Clinical Practicum. Int. J. Environ. Res. Public Health 2022, 19, 7479. https://doi.org/10.3390/ijerph19127479
Lai M-H, Tzeng C-Y, Chuang Y-H, Chang P-C, Chung M-H. Coping with the Experience of Bad Sleep and Fatigue Associated with the Nursing Clinical Practicum. International Journal of Environmental Research and Public Health. 2022; 19(12):7479. https://doi.org/10.3390/ijerph19127479
Chicago/Turabian StyleLai, Mei-Hsin, Chyn-Yuan Tzeng, Yeu-Hui Chuang, Pi-Chen Chang, and Min-Huey Chung. 2022. "Coping with the Experience of Bad Sleep and Fatigue Associated with the Nursing Clinical Practicum" International Journal of Environmental Research and Public Health 19, no. 12: 7479. https://doi.org/10.3390/ijerph19127479
APA StyleLai, M.-H., Tzeng, C.-Y., Chuang, Y.-H., Chang, P.-C., & Chung, M.-H. (2022). Coping with the Experience of Bad Sleep and Fatigue Associated with the Nursing Clinical Practicum. International Journal of Environmental Research and Public Health, 19(12), 7479. https://doi.org/10.3390/ijerph19127479








