Analyzing Trajectories of Acute Cigarette Reduction Post-Introduction of an E-Cigarette Using Ecological Momentary Assessment Data
Abstract
1. Introduction
2. Materials and Methods
Modeling Procedure
3. Results
3.1. Determination of Optimal Number and Order of Trajectory Classes
3.2. CPD Reduction Trajectories Post-EC Introduction
3.3. Differences between Trajectory Classes
3.4. Combustible Cigarette Cravings by Trajectory Class
3.5. Electronic Cigarette Use by Trajectory Class
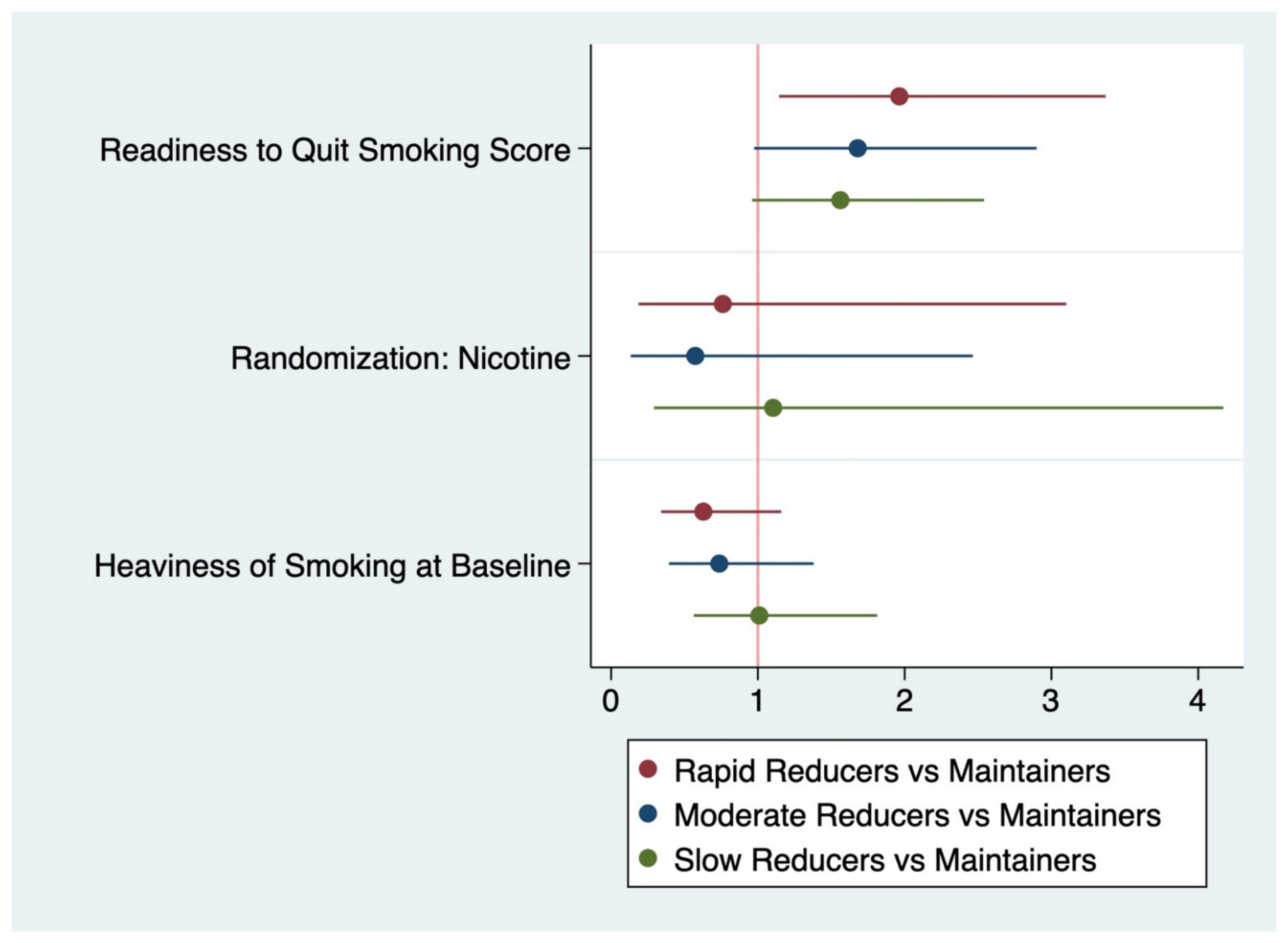
3.6. Class Assignment as Dependent Variable in Multinomial Logistic Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Report on the Global Tobacco Epidemic 2017; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Center for Disease Control and Prevention Smoking & Tobacco Use: Fact Sheet. Available online: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/index.htm (accessed on 1 December 2018).
- Babb, S. Quitting smoking among adults—United States, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 65, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R.; Keely, J.; Naud, S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004, 99, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Hartmann-Boyce, J.; McRobbie, H.; Bullen, C.; Begh, R.; Stead, L.F.; Hajek, P. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 2016, CD010216. [Google Scholar] [CrossRef] [PubMed]
- Brose, L.S.; Hitchman, S.C.; Brown, J.; West, R.; McNeill, A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction 2015, 110, 1160–1168. [Google Scholar] [CrossRef] [PubMed]
- Caponnetto, P.; Campagna, D.; Cibella, F.; Morjaria, J.B.; Caruso, M.; Russo, C.; Polosa, R. EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as Tobacco Cigarettes Substitute: A Prospective 12-Month Randomized Control Design Study. PLoS ONE 2013, 8, e66317. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.A.; Hann, N.; Wilson, A.; Mnatzaganian, G.; Worrall-Carter, L. E-cigarettes and smoking cessation: Evidence from a systematic review and meta-analysis. PLoS ONE 2015, 10, e0122544. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Beard, E.; Kotz, D.; Michie, S.; West, R. Real-world effectiveness of e-cigarettes when used to aid smoking cessation: A cross-sectional population study. Addiction 2014, 109, 1531–1540. [Google Scholar] [CrossRef]
- Hajek, P.; Phillips-Waller, A.; Przulj, D.; Pesola, F.; Myers Smith, K.; Bisal, N.; Li, J.; Parrott, S.; Sasieni, P.; Dawkins, L.; et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N. Engl. J. Med. 2019, 380, 629–637. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, B.; Knight-West, O.; Walker, N.; Parag, V.; Bullen, C. E-cigarettes versus NRT for smoking reduction or cessation in people with mental illness: Secondary analysis of data from the ASCEND trial. Tob. Induced Dis. 2015, 13, 5. [Google Scholar] [CrossRef] [PubMed]
- Tseng, T.-Y.; Ostroff, J.S.; Campo, A.; Gerard, M.; Kirchner, T.; Rotrosen, J.; Shelley, D. A randomized trial comparing the effect of nicotine versus placebo electronic cigarettes on smoking reduction among young adult smokers. Nicotine Tob. Res. 2016, 18, 1937–1943. [Google Scholar] [CrossRef]
- Kirchner, T.R.; Shiffman, S. Ecological momentary assessment. In The Wiley-Blackwell Handbook of Addiction Psychopharmacology; John Wiley & Sons: Hoboken, NJ, USA, 2013; pp. 541–565. [Google Scholar]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Nides, M.A.; Leischow, S.J.; Bhatter, M.; Simmons, M. Nicotine blood levels and short-term smoking reduction with an electronic nicotine delivery system. Am. J. Health Behav. 2014, 38, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Rickert, W.; Robinson, J. Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 1989, 84, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Glover, E.D.; Nilsson, F.; Westin, Å.; Glover, P.N.; Laflin, M.T.; Persson, B. Developmental history of the Glover-Nilsson smoking behavioral questionnaire. Am. J. Health Behav. 2005, 29, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Biener, L.; Abrams, D.B. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991, 10, 360. [Google Scholar] [CrossRef]
- Jones, B.L.; Nagin, D.S. A Stata Plugin for Estimating Group-Based Trajectory Models. J. Contrib. 2012. [Google Scholar] [CrossRef]
- Jones, B.L.; Nagin, D.S. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol. Methods Res. 2007, 35, 542–571. [Google Scholar] [CrossRef]
- Jones, B.L.; Nagin, D.S.; Roeder, K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol. Methods Res. 2001, 29, 374–393. [Google Scholar] [CrossRef]
- Conklin, C.A.; Perkins, K.A.; Sheidow, A.J.; Jones, B.L.; Levine, M.D.; Marcus, M.D. The return to smoking: 1-year relapse trajectories among female smokers. Nicotine Tob. Res. 2005, 7, 533–540. [Google Scholar] [CrossRef]
- Delucchi, K.L.; Matzger, H.; Weisner, C. Dependent and problem drinking over 5 years: A latent class growth analysis. Drug Alcohol Depend. 2004, 74, 235–244. [Google Scholar] [CrossRef]
- Chassin, L.; Presson, C.; Seo, D.-C.; Sherman, S.J.; Macy, J.; Wirth, R.J.; Curran, P. Multiple trajectories of cigarette smoking and the intergenerational transmission of smoking: A multigenerational, longitudinal study of a Midwestern community sample. Health Psychol. 2008, 27, 819. [Google Scholar] [CrossRef] [PubMed]
- Vitaro, F.; Wanner, B.; Brendgen, M.; Gosselin, C.; Gendreau, P.L. Differential contribution of parents and friends to smoking trajectories during adolescence. Addict. Behav. 2004, 29, 831–835. [Google Scholar] [CrossRef] [PubMed]
- Nagin, D.S.; Odgers, C.L. Group-Based Trajectory Modeling in Clinical Research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef] [PubMed]
- Nagin, D.S. Analyzing Developmental Trajectories: A Semiparametric, Group-Based Approach. Psychol. Methods 1999, 4, 139–157. [Google Scholar] [CrossRef]
- Wong, N.C.H.; Cappella, J.N. Antismoking threat and efficacy appeals: Effects on smoking cessation intentions for smokers with low and high readiness to quit. J. Appl. Commun. Res. 2009, 37, 1–20. [Google Scholar] [CrossRef]
- Vangeli, E.; Stapleton, J.; Smit, E.S.; Borland, R.; West, R. Predictors of attempts to stop smoking and their success in adult general population samples: A systematic review. Addiction 2011, 106, 2110–2121. [Google Scholar] [CrossRef]
- Stockings, E.; Bowman, J.; McElwaine, K.; Baker, A.L.; Terry, M.; Clancy, R.; Bartlem, K.; Wye, P.; Bridge, P.; Knight, J.; et al. Readiness to Quit Smoking and Quit Attempts Among Australian Mental Health Inpatients. Nicotine Tob. Res. 2012, 15, 942–949. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Rossi, J.S.; Redding, C.A.; Rosen, A.B.; Tsoh, J.Y.; Humfleet, G.L.; Eisendrath, S.J.; Meisner, M.R.; Hall, S.M. Depressed smokers and stage of change: Implications for treatment interventions. Drug Alcohol Depend. 2004, 76, 143–151. [Google Scholar] [CrossRef]
- Chaiton, M.; Diemert, L.; Cohen, J.E.; Bondy, S.J.; Selby, P.; Philipneri, A.; Schwartz, R. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open 2016, 6, e011045. [Google Scholar] [CrossRef]
- Hymowitz, N.; Cummings, K.M.; Hyland, A.; Lynn, W.R.; Pechacek, T.F.; Hartwell, T.D. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob. Control 1997, 6, S57. [Google Scholar] [CrossRef]
- Gupta, S.K. Intention-to-treat concept: A review. Perspect. Clin. Res. 2011, 2, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Hollis, S.; Campbell, F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999, 319, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Solhan, M.B.; Trull, T.J.; Jahng, S.; Wood, P.K. Clinical assessment of affective instability: Comparing EMA indices, questionnaire reports, and retrospective recall. Psychol. Assess. 2009, 21, 425. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, S. Ecological momentary assessment (EMA) in studies of substance use. Psychol. Assess. 2009, 21, 486. [Google Scholar] [CrossRef]
- Berkman, E.T.; Dickenson, J.; Falk, E.B.; Lieberman, M.D. Using SMS text messaging to assess moderators of smoking reduction: Validating a new tool for ecological measurement of health behaviors. Health Psychol. 2011, 30, 186–194. [Google Scholar] [CrossRef]
- Berg, C.J.; Haardörfer, R.; Payne, J.B.; Getachew, B.; Vu, M.; Guttentag, A.; Kirchner, T.R. Ecological momentary assessment of various tobacco product use among young adults. Addict. Behav. 2018, 92, 38–46. [Google Scholar] [CrossRef]
- Cerrada, C.J.; Ra, C.; Shin, H.-S.; Dzubur, E.; Huh, J. Using Ecological Momentary Assessment to Identify Common Smoking Situations Among Korean American Emerging Adults. Prev. Sci. 2016, 17, 892–902. [Google Scholar] [CrossRef]
- Businelle, M.S.; Ma, P.; Kendzor, D.E.; Reitzel, L.R.; Chen, M.; Lam, C.Y.; Bernstein, I.; Wetter, D.W. Predicting Quit Attempts Among Homeless Smokers Seeking Cessation Treatment: An Ecological Momentary Assessment Study. Nicotine Tob. Res. 2014, 16, 1371–1378. [Google Scholar] [CrossRef][Green Version]
- Shiffman, S.; Paty, J. Smoking patterns and dependence: Contrasting chippers and heavy smokers. J. Abnorm. Psychol. 2006, 115, 509. [Google Scholar] [CrossRef]
- Cokkinides, V.E.; Halpern, M.T.; Barbeau, E.M.; Ward, E.; Thun, M.J. Racial and ethnic disparities in smoking-cessation interventions: Analysis of the 2005 National Health Interview Survey. Am. J. Prev. Med. 2008, 34, 404–412. [Google Scholar] [CrossRef]
- Levinson, A.H.; Pérez-Stable, E.J.; Espinoza, P.; Flores, E.T.; Byers, T.E. Latinos report less use of pharmaceutical aids when trying to quit smoking. Am. J. Prev. Med. 2004, 26, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Thorndike, A.N.; Biener, L.; Rigotti, N.A. Effect on smoking cessation of switching nicotine replacement therapy to over-the-counter status. Am. J. Public Health 2002, 92, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Lipkus, I.M.; Lyna, P.R.; Rimer, B.K. Using tailored interventions to enhance smoking cessation among African-Americans at a community health center. Nicotine Tob. Res. 1999, 1, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Orleans, C.T.; Strecher, V.J.; Schoenbach, V.J.; Salmon, M.A.; Blackmon, C. Smoking cessation initiatives for Black Americans: Recommendations for research and intervention. Health Educ. Res. 1989, 4, 13–25. [Google Scholar] [CrossRef]
- King, T.K.; Borrelli, B.; Black, C.; Pinto, B.M.; Marcus, B.H. Minority women and tobacco: Implications for smoking cessation interventions. Ann. Behav. Med. 1997, 19, 301–313. [Google Scholar] [CrossRef]
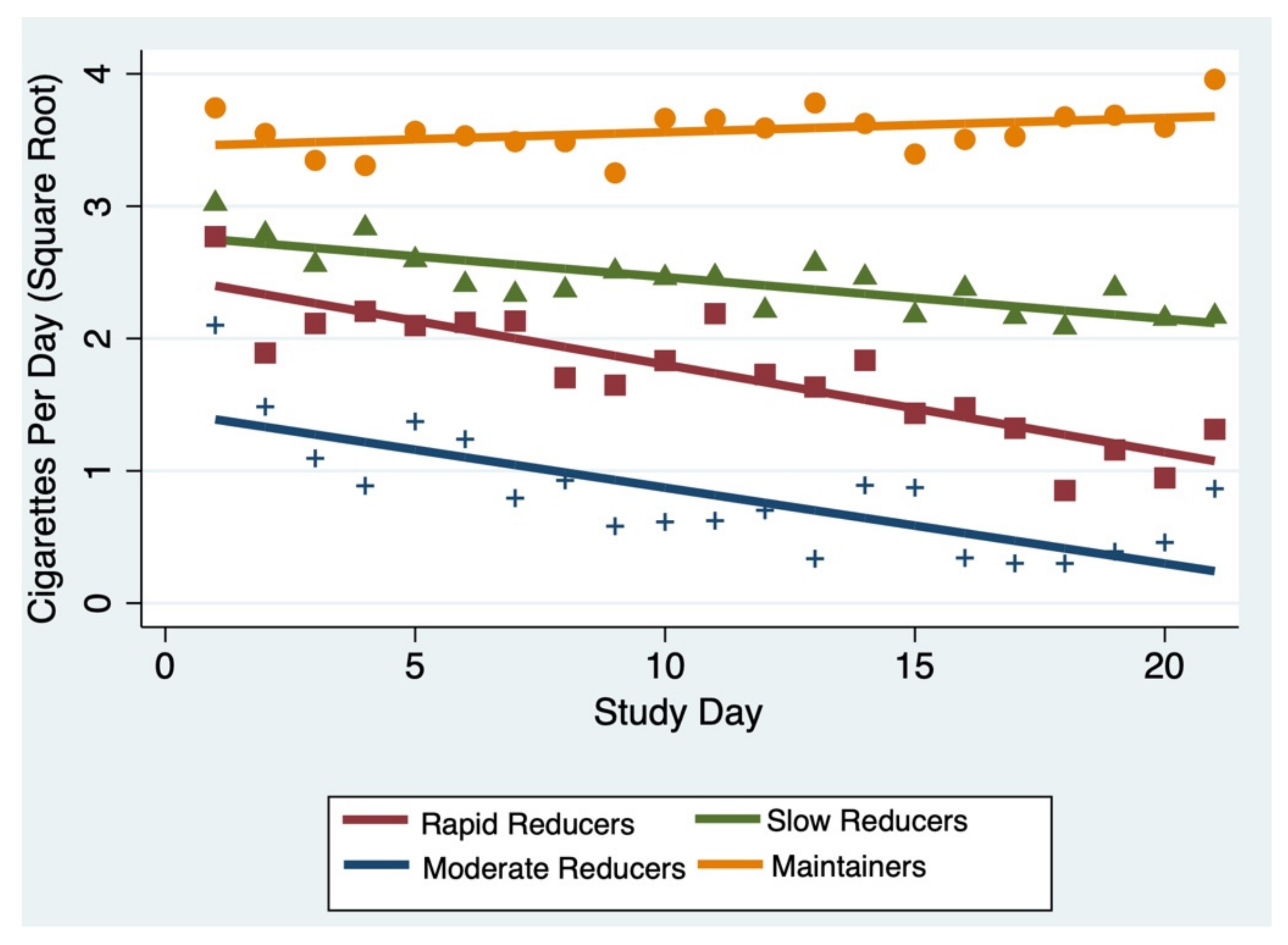
| Class (N, %) | CPD at Start 1 | Linear Coefficient | Standard Error |
|---|---|---|---|
| Rapid Reducers (23, 27%) | 6.3 | −0.07 | 0.01 |
| Moderate Reducers (18, 21%) | 2 | −0.06 | 0.009 |
| Slow Reducers (27, 32%) | 7.8 | −0.03 | 0.009 |
| Maintainers (16, 19%) | 12.3 | 0.01 | 0.009 |
| Total | Outcome = Trajectory Group | ||||
|---|---|---|---|---|---|
| N (%) or Mean (SD) | Rapid Reducers N (%) or Mean (SD) | Moderate Reducers N (%, SD) | Slow Reducers N (%, SD) | Maintainers N (%, SD) | |
| Demographics | |||||
| Age in years | 28.4 (3.9) | 28.5 (3.8) | 28.3 (4.2) | 28.3 (4.0) | 28.4 (4.0) |
| Gender | |||||
| Male | 57 (67.9) | 13 (56.5) | 16 (88.9) | 20 (74.1) | 8 (50.0) |
| Female | 27 (32.1) | 10 (43.5) | 2 (11.1) | 7 (25.9) | 8 (50.0) |
| Education | |||||
| High school or less | 20 (23.8) | 6 (26.0) | 4 (22.2) | 7 (25.9) | 3 (18.8) |
| Some college | 33 (39.3) | 10 (43.5) | 10 (55.5) | 7 (25.9) | 6 (37.5) |
| College or post-graduate | 31 (36.9) | 7 (30.4) | 4 (22.2) | 13 (48.1) | 7 (38.9) |
| Race/Ethnicity | |||||
| Non-Hispanic African American/Black | 20 (24.1) | 5 (21.7) | 6 (33.3) | 4 (14.8) | 5 (31.2) |
| Non-Hispanic white | 28 (33.7) | 10 (43.5) | 3 (16.7) | 9 (33.3) | 6 (37.5) |
| Other non-Hispanic | 14 (16.9) | 2 (8.7) | 3 (16.7) | 8 (29.6) | 1 (6.3) |
| Hispanic of any race | 21 (25.3) | 5 (21.7) | 6 (33.3) | 6 (22.2) | 4 (25.0) |
| Treatment Assignment | |||||
| Control (Placebo) | 42 (50.0) | 11 (47.8) | 10 (55.6) | 13 (48.1) | 8 (50.0) |
| Active Nicotine | 42 (50.0) | 12 (52.2) | 8 (44.4) | 14 (51.9) | 8 (50.0) |
| Tobacco Use | |||||
| Baseline CPD | |||||
| 10 | 22 (26.2) | 7 (30.4) | 6 (33.3) | 8 (29.6) | 1 (6.3) |
| >10 | 62 (73.8) | 16 (69.6) | 12 (66.7) | 19 (70.4) | 15 (93.8) |
| Heaviness of Smoking Index (0–5 scale) * | 2.6 (1.2, 0–5) | 2.2 (1.1) | 2.5 (0.9) | 2.8 (1.2) | 2.9 (1.4) |
| Made serious quit attempts (>1 day) in last year | 41 (48.8) | 14 (60.9) | 9 (50.0) | 12 (44.4) | 6 (37.8) |
| Readiness to Quit (1–10 scale, 1–8 apply to current smokers) | 5.56 (1.4) | 6 (1.1) | 5.8 (1.4) | 5.7 (1.6) | 4.8 (1.1) |
| Confidence in Quit Ability | 6.4 (2.6) | 6.7 (2.6) | 7.2 (2.6) | 6.3 (2.5) | 5.0 (3.2) |
| Smoking behavioral dependence scale (11 items) | |||||
| Mild | 15 (17.9) | 2 (8.7) | 5 (27.8) | 7 (25.9) | 1 (6.3) |
| Moderate | 42 (50.0) | 11 (47.8) | 10 (55.5) | 14 (51.9) | 7 (43.8) |
| Strong to very strong | 27 (32.1) | 10 (43.5) | 3 (16.7) | 6 (22.2) | 8 (50.0) |
| Health Behavior Outcomes | |||||
| Week 1 ECPD | 1.06 (0.74) | 1.0 (0.64) | 1.2 (0.61) | 1.01 (0.96) | 0.94 (0.65) |
| Week 3 ECPD | 0.99 (1.5) | 0.99 (1.5) | 0.92 (0.70) | 1.1 (0.66) | 0.68 (0.47) |
| 50% Smoking reduction obtained at week 3 ** | 47 (59.5) | 14 (60.9) | 16 (88.9) | 15 (55.6) | 2 (12.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guttentag, A.; Tseng, T.-Y.; Shelley, D.; Kirchner, T. Analyzing Trajectories of Acute Cigarette Reduction Post-Introduction of an E-Cigarette Using Ecological Momentary Assessment Data. Int. J. Environ. Res. Public Health 2022, 19, 7452. https://doi.org/10.3390/ijerph19127452
Guttentag A, Tseng T-Y, Shelley D, Kirchner T. Analyzing Trajectories of Acute Cigarette Reduction Post-Introduction of an E-Cigarette Using Ecological Momentary Assessment Data. International Journal of Environmental Research and Public Health. 2022; 19(12):7452. https://doi.org/10.3390/ijerph19127452
Chicago/Turabian StyleGuttentag, Alexandra, Tuo-Yen Tseng, Donna Shelley, and Thomas Kirchner. 2022. "Analyzing Trajectories of Acute Cigarette Reduction Post-Introduction of an E-Cigarette Using Ecological Momentary Assessment Data" International Journal of Environmental Research and Public Health 19, no. 12: 7452. https://doi.org/10.3390/ijerph19127452
APA StyleGuttentag, A., Tseng, T.-Y., Shelley, D., & Kirchner, T. (2022). Analyzing Trajectories of Acute Cigarette Reduction Post-Introduction of an E-Cigarette Using Ecological Momentary Assessment Data. International Journal of Environmental Research and Public Health, 19(12), 7452. https://doi.org/10.3390/ijerph19127452






