Foundation Level Barriers to the Widespread Adoption of Digital Solutions by Care Homes: Insights from Three Scottish Studies
Abstract
:1. Introduction
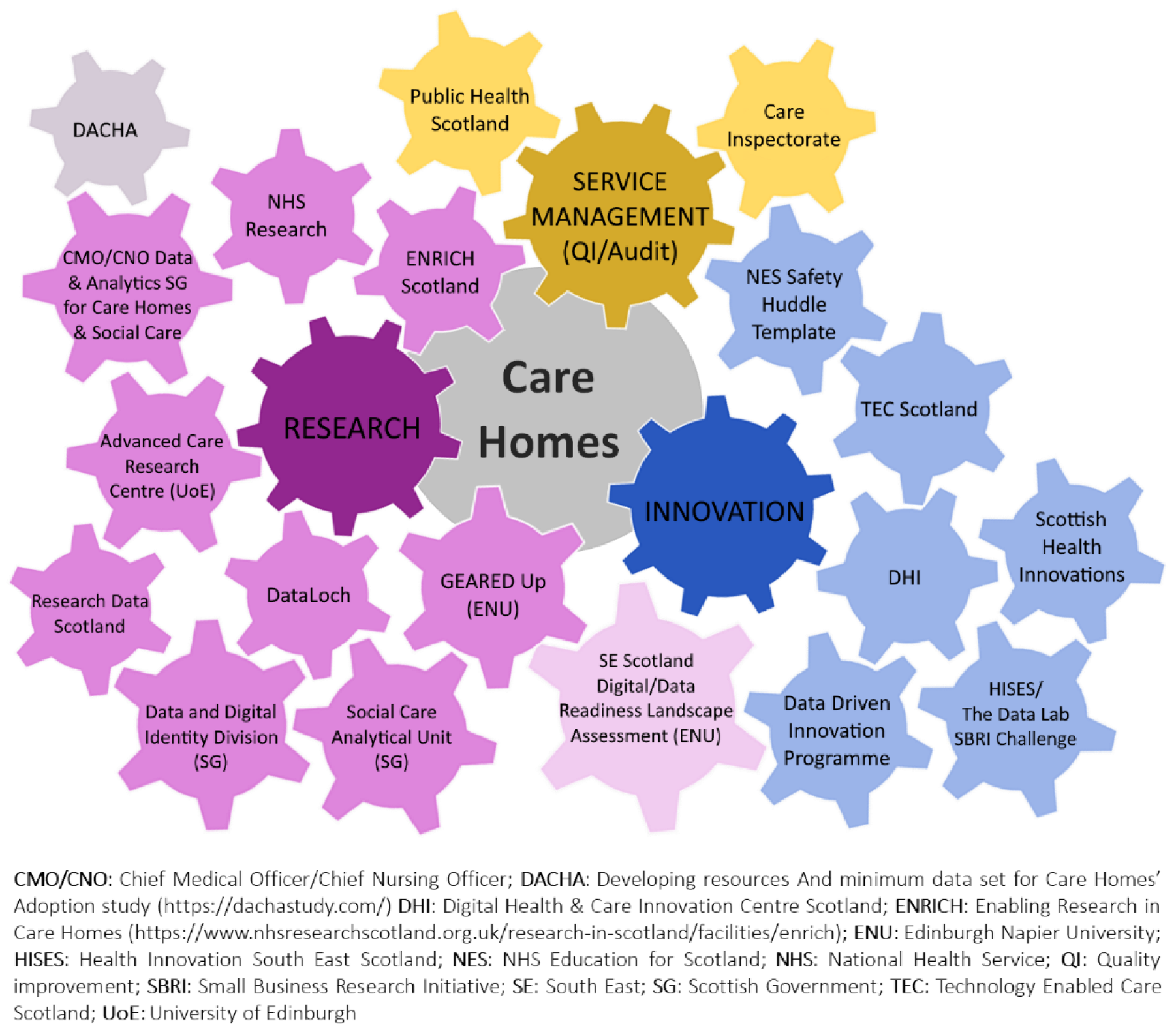
2. Research Studies
2.1. Care Home Data Platform
2.2. Landscape Assessment of Data and Digital Readiness of Scottish Care Homes (LADDeR)
2.3. Governance, Ethics, Access & Readiness through an Exemplar Demonstration (GEARED Up)
3. Foundation Level Barriers
3.1. Connectivity of Care Homes
3.2. Capabilities for Digital Data Collection
3.3. Access to Data to Inform and Drive Digital Solutions
3.4. The Need for Trust in the Use of Care Home Data
3.5. The Need for Certainty and Coordination
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hall, A.; Wilson, C.B.; Stanmore, E.; Todd, C. Implementing monitoring technologies in care homes for people with dementia: A qualitative exploration using normalization process theory. Int. J. Nurs. Stud. 2017, 72, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Atherton, I.M.; Lynch, E.; Williams, A.J.; Witham, M.D. Barriers and Solutions to Linking and Using Health and Social Care Data. Br. J. Soc. Work 2015, 45, 1614–1622. [Google Scholar] [CrossRef] [Green Version]
- Care Quality Commission. Enabling Innovation and Adoption in Health and Social Care: Developing a Shared View. February 2021. Available online: https://www.cqc.org.uk/sites/default/files/20210208_InnovationPrinciples_report.pdf (accessed on 9 March 2022).
- Bell, D.; Comas-Herrera, A.; Henderson, D.; Jones, S.; Lemmon, E.; Moro, M.; Murphy, S.; O’Reilly, D.; Patrignani, P. COVID-19 Mortality and Long-Term Care: A UK Comparison. Article in LTCcovid.org, International LongTerm Care Policy Network, CPEC-LSE. 2020. Available online: https://ltccovid.org/wp-content/uploads/2020/08/COVID-19-mortality-in-long-term-care-final-Sat-29-v1.pdf (accessed on 28 February 2022).
- Office for National Statistics. National Population Projections: 2020-Based Interim. January 2022. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2020basedinterim (accessed on 28 February 2022).
- Bone, A.E.; Gomes, B.; Etkind, S.N.; Verne, J.; Murtagh, F.; Evans, C.J.; Higginson, I.J. What is the impact of population ageing on the future provision of end-of-life care? Population-based projections of place of death. Palliat. Med. 2018, 32, 329–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barker, R.O.; Hanratty, B.; Kingston, A.; Ramsay, S.E.; Matthews, F.E. Changes in the health and functioning of care home residents over two decades: What can we learn from population-based studies? Age Ageing 2021, 50, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Public Health Scotland. Acute Hospital Activity and NHS Beds Information (Annual). March 2021. Available online: https://publichealthscotland.scot/publications/acute-hospital-activity-and-nhs-beds-information-annual/acute-hospital-activity-and-nhs-beds-information-annual-annual-year-ending-31-march-2021/#:~:text=The%20average%20number%20of%20available,ago%20(2015%2F16) (accessed on 28 February 2022).
- The King’s Fund. NHS Hospital Bed Numbers: Past, Present, Future. Available online: https://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers (accessed on 28 February 2022).
- Deloitte Centre for Health Solutions. Connected health: How Digital Technology Is Transforming Health and Social Care. 2015. Available online: https://www2.deloitte.com/content/dam/Deloitte/uk/Documents/life-sciences-health-care/deloitte-uk-connected-health.pdf (accessed on 9 March 2022).
- Greenhalgh, T.; Wherton, J.; Papoutsi, C.; Lynch, J.; Wherton, J.H.; Papoutsi, C.; Lynch, J.; Hughes, G.; A’Court, C.; Hinder, S.; et al. Beyond Adoption: A New Framework for Theorizing and Evaluating Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies. J. Med. Internet Res. 2017, 19, e367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunn, F.; Goodman, C.; Corazzini, K.; Sharpe, R.; Handley, M.; Lynch, J.; Meyer, J.; Dening, T.; Gordon, A.L. Setting priorities to inform assessment of care homes’ readiness to participate in healthcare innovation: A systematic mapping review and consensus process. Int. J. Environ. Res. Public Health 2020, 17, 987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenhalgh, T.; Robert, G.; Macfarlane, F.; Bate, P.; Kyriakidou, O. Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Q. 2004, 82, 581–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Institute of Public Care. Adoption and Scalability of Technology Innovation in the Adult Social Care Sector: Rapid Research Review. February 2021. Available online: https://ipc.brookes.ac.uk/files/publications/Digital-tech-rapid-research-review-Feb-2021.pdf (accessed on 9 March 2022).
- Goodman, C.; Sharpe, R.; Russell, C.; Meyer, J.; Gordon, A.; Dening, T.; Corazzini, K.N.; Lynch, J.; Bunn, F. Care Home Readiness: A Rapid Review and Consensus Workshops on How Organisational Context Affects Care Home Engagement with Health Care Innovation; NHS England: London, UK, 2017; p. 78. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Papoutsi, C. Spreading and scaling up innovation and improvement. BMJ 2019, 365, l2068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scottish Government. A National Care Service for Scotland: Consultation. August 2021. Available online: https://www.gov.scot/publications/national-care-service-scotland-consultation/documents/ (accessed on 9 March 2022).
- Scottish Government. National Care Service: Consultation Analysis. February 2022. Available online: https://www.gov.scot/publications/national-care-service-consultation-analysis-responses/ (accessed on 9 March 2022).
- Scottish Government. Scotland’s Digital Health & Care Strategy: Enabling, Connecting & Empowering. April 2018. Available online: https://www.gov.scot/publications/scotlands-digital-health-care-strategy-enabling-connecting-empowering/pages/10/ (accessed on 9 March 2022).
- Scottish Government & COSLA. Enabling, Connecting and Empowering: Care in the Digital Age. Scotland’s Digital Health and Care Strategy. October 2021. Available online: https://www.gov.scot/binaries/content/documents/govscot/publications/strategy-plan/2018/04/scotlands-digital-health-care-strategy-enabling-connecting-empowering/documents/00534657-pdf/00534657-pdf/govscot%3Adocument/00534657.pdf (accessed on 9 March 2022).
- Hockley, J.; Watson, J.; Harrison, J.; Randall, M.; Primary Palliative Care Research Group. Vision for a Teaching/Research-Based Care Home. The Usher Institute, University of Edinburgh, 2016. Available online: https://www.ed.ac.uk/files/atoms/files/the_vision_for_a_teachingresearch-based_care_home_0.pdf (accessed on 9 March 2022).
- Johnston, L.; Hockley, J.; Henderson, D.A.; Shenkin, S.D. The Development of a Care Home Data Platform in Scotland: Insights from the Care Home Innovation Partnership, Lothian. medRxiv 2020. [Google Scholar] [CrossRef]
- Johnston, L.; Koikkalainen, H.; Anderson, L.; Lapok, P.; Lawson, A.; Shenkin, S. Landscape Assessment of Data and Digital Readiness in Scottish Care Homes Final Report. April 2022. Available online: https://ladder.napier.ac.uk/blog/ (accessed on 5 April 2022).
- Health Innovation South East Scotland. Care Home Data Platform Innovation Foundation Challenge. Available online: https://hises.edinburghbioquarter.com/care-home-innovation-challenge (accessed on 9 March 2022).
- Technology Enabled Care. Connecting People Connecting Services: Digital Approaches in Care Homes Action Plan. 2021. Available online: https://tec.scot/sites/default/files/2021-06/Digital-Approches-in-Care-Homes-Action-Plan-Final.pdf (accessed on 9 March 2022).
- The King’s Fund. Digital Change in Health and Social Care. June 2018. Available online: https://www.kingsfund.org.uk/sites/default/files/2018-06/Digital_change_health_care_Kings_Fund_June_2018.pdf (accessed on 9 March 2022).
- Burton, J.K.; Goodman, C.; Guthrie, B.; Gordon, A.L.; Hanratty, B.; Quinn, T.J. Closing the UK care home data gap–methodological challenges and solutions. Int. J. Popul. Data Sci. 2020, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, C.; Smallman, M.; Wilson, J. Making Older People Visible: Solving the Denominator Problem in Care Home Data. 2021. Available online: https://ukpandemicethics.org/wp-content/uploads/2021/06/Making-older-people-visible-in-care-home-data-by-solving-the-denominator-problem.pdf (accessed on 9 March 2022).
- Moore, D.C.; Hanratty, B. Out of sight, out of mind? A review of data available on the health of care home residents in longitudinal and nationally representative cross-sectional studies in the UK and Ireland. Age Ageing 2013, 42, 798–803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bharti, N.; O’Donovan, C.; Smallman, M.; Wilson, J. Public Trust, Deliberative Engagement and Health Data Projects: Beyond Legal Provisions. Engag. Sci. Technol. Soc. 2021, 7, 125–133. [Google Scholar] [CrossRef]
- The King’s Fund. Shaping the Future of Digital Technology in Health and Social Care. April 2021. Available online: https://www.kingsfund.org.uk/sites/default/files/2021-04/Shaping%20the%20future%20of%20digital%20technology%20in%20health%20and%20social%20care.pdf (accessed on 9 March 2022).
- Curry, N.; Oung, C. Fractured and Forgotten? The Social Care Provider Market in England. Research Report, Nuffield Trust. 2021. Available online: https://www.nuffieldtrust.org.uk/research/fractured-and-forgotten-the-social-care-provider-market-in-england (accessed on 9 March 2022).
- NHS Research Scotland. Data Safe Haven–Information. Available online: https://www.nhsresearchscotland.org.uk/research-in-scotland/data/safe-havens (accessed on 1 March 2022).
- SAIL Databank—The Secure Anonymised Linkage Databank. 2022. Available online: https://saildatabank.com (accessed on 1 March 2022).
- Scottish Council for Development and Industry. Mind the Gap: How Data, Digital and Technology Can Help Scotland Recover from COVID-19, Transform Health & Social Care and Boost Our Economy. 2021. Available online: https://www.scdi.org.uk/policy/mindthegap/ (accessed on 9 March 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnston, L.; Koikkalainen, H.; Anderson, L.; Lapok, P.; Lawson, A.; Shenkin, S.D. Foundation Level Barriers to the Widespread Adoption of Digital Solutions by Care Homes: Insights from Three Scottish Studies. Int. J. Environ. Res. Public Health 2022, 19, 7407. https://doi.org/10.3390/ijerph19127407
Johnston L, Koikkalainen H, Anderson L, Lapok P, Lawson A, Shenkin SD. Foundation Level Barriers to the Widespread Adoption of Digital Solutions by Care Homes: Insights from Three Scottish Studies. International Journal of Environmental Research and Public Health. 2022; 19(12):7407. https://doi.org/10.3390/ijerph19127407
Chicago/Turabian StyleJohnston, Lucy, Heidi Koikkalainen, Lynda Anderson, Paul Lapok, Alistair Lawson, and Susan D. Shenkin. 2022. "Foundation Level Barriers to the Widespread Adoption of Digital Solutions by Care Homes: Insights from Three Scottish Studies" International Journal of Environmental Research and Public Health 19, no. 12: 7407. https://doi.org/10.3390/ijerph19127407
APA StyleJohnston, L., Koikkalainen, H., Anderson, L., Lapok, P., Lawson, A., & Shenkin, S. D. (2022). Foundation Level Barriers to the Widespread Adoption of Digital Solutions by Care Homes: Insights from Three Scottish Studies. International Journal of Environmental Research and Public Health, 19(12), 7407. https://doi.org/10.3390/ijerph19127407






