Employment Status and Alcohol-Attributable Mortality Risk—A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Systematic Literature Search
2.2. Study Selection and Inclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
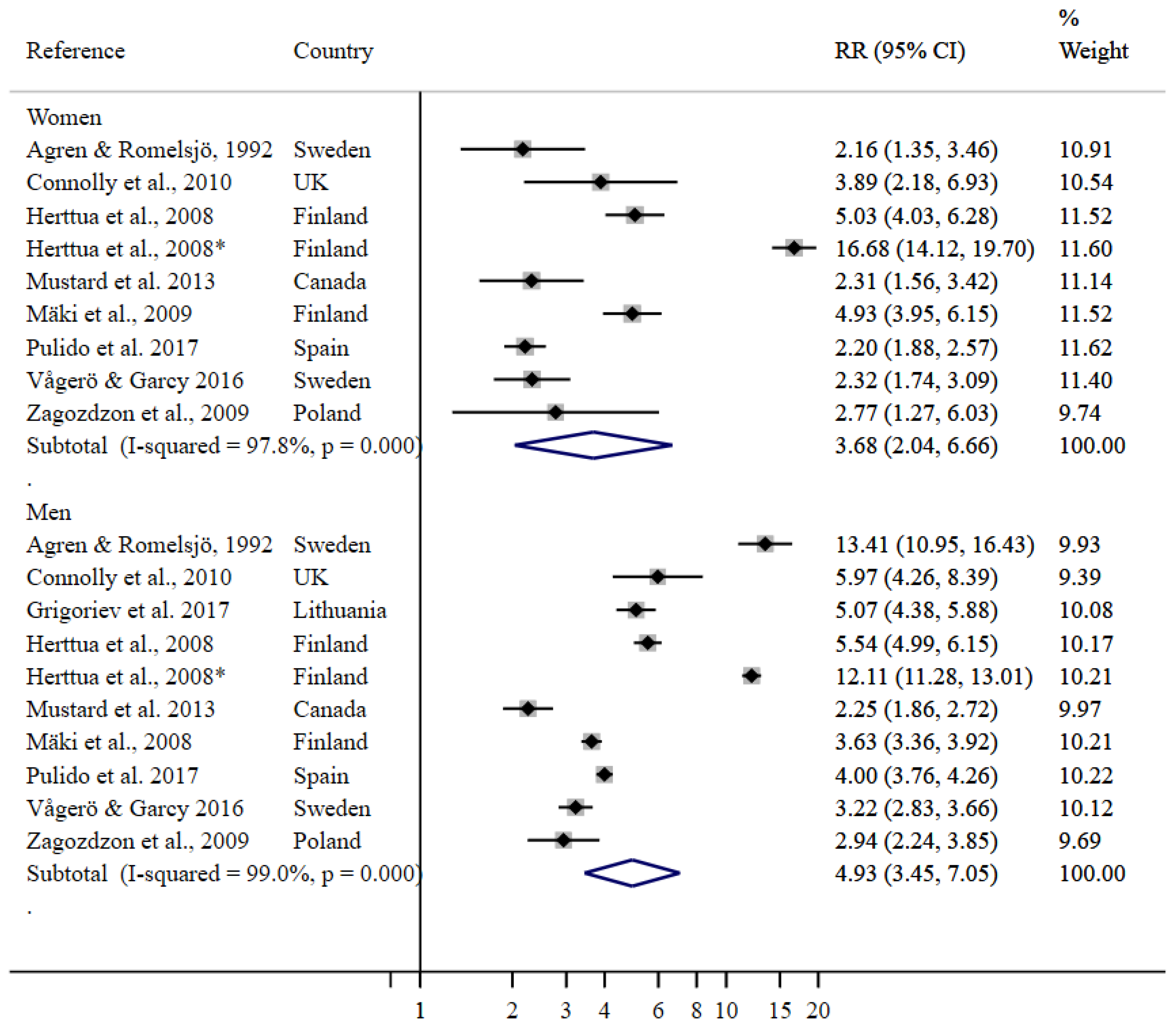
3.1. Relative Risks for Employment Status
3.2. Heterogeneity and Bias Control
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Social Determinants of Health: World Health Organization; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Fiscella, K.; Williams, D.R. Health Disparities Based on Socioeconomic Inequities: Implications for Urban Health Care. Acad. Med. 2004, 79, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Commission on Social Determinants of Health. Closing the Gap in A Generation: Health Equity through Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: San Francisco, CA, USA, 2015. [Google Scholar]
- Hergenrather, K.C.; Zeglin, R.J.; McGuire-Kuletz, M.; Rhodes, S.D. Employment as a Social Determinant of Health: A Systematic Review of Longitudinal Studies Exploring the Relationship Between Employment Status and Physical Health. Rehabil. Res. Policy Educ. 2015, 29, 2–26. [Google Scholar] [CrossRef]
- Wanberg, C.R. The individual experience of unemployment. Annu. Rev. Psychol. 2012, 63, 369–396. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Life Expectancy Gain Due to Employment Status Depends on Race, Gender, Education, and Their Intersections. J. Racial Ethn. Health Disparities 2018, 5, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.; Bianchi, G.; Song, D. The Long-Term Impact of the COVID-19 Unemployment Shock on Life Expectancy and Mortality Rates. In NBER Working Paper Series; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Dunlavy, A.C.; Juárez, S.; Rostila, M. Employment status and risk of all-cause mortality among native- and foreign-origin persons in Sweden. Eur. J. Public Health 2018, 28, 891–897. [Google Scholar] [CrossRef]
- Laliotis, I.; Stavropoulou, C. Crises and mortality: Does the level of unemployment matter? Soc. Sci. Med. 2018, 214, 99–109. [Google Scholar] [CrossRef]
- Nie, J.; Wang, J.; Aune, D.; Huang, W.; Xiao, D.; Wang, Y.; Chen, X. Association between employment status and risk of all-cause and cause-specific mortality: A population-based prospective cohort study. J. Epidemiol. Community Health 2020, 74, 428–436. [Google Scholar] [CrossRef]
- Roelfs, D.J.; Shor, E.; Davidson, K.W.; Schwartz, J.E. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Soc. Sci. Med. 2011, 72, 840–854. [Google Scholar] [CrossRef]
- Yur’yev, A.; Värnik, A.; Värnik, P.; Sisask, M.; Leppik, L. Employment status influences suicide mortality in Europe. Int. J. Soc. Psychiatry 2012, 58, 62–68. [Google Scholar] [CrossRef]
- Tapia Granados, J.A.; House, J.S.; Ionides, E.L.; Burgard, S.; Schoeni, R.S. Individual joblessness, contextual unemployment, and mortality risk. Am. J. Epidemiol. 2014, 180, 280–287. [Google Scholar] [CrossRef]
- Gomis, R.; Kapsos, S.; Kuhn, S. World Employment and Social Outlook: Trends 2020; ILO: Geneva, Switzerland, 2020; pp. 127 (report) + 125p. (executive summary). [Google Scholar]
- Berg, J.; Hilal, A.; El, S.; Horne, R. World Employment and Social Outlook: Trends 2021; ILO: Geneva, Switzerland, 2021. [Google Scholar]
- Probst, C.; Roerecke, M.; Behrendt, S.; Rehm, J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: A systematic review and meta-analysis. Int. J. Epidemiol. 2014, 43, 1314–1327. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Roerecke, M.; Behrendt, S.; Rehm, J. Gender differences in socioeconomic inequality of alcohol-attributable mortality: A systematic review and meta-analysis. Drug Alcohol Rev. 2015, 34, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Ågren, G.; Romelsjü, A. Mortality in alcohol-related diseases in Sweden during 1971–80 in relation to occupation marital-status and citizenship in 1970. Scand. J. Soc. Med. 1992, 20, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Herttua, K.; Mäkelä, P.; Martikainen, P. Changes in alcohol-related mortality and its socioeconomic differences after a large reduction in alcohol prices: A natural experiment based on register data. Am. J. Epidemiol. 2008, 168, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Lange, S.; Kilian, C.; Saul, C.; Rehm, J. The dose-response relationship between socioeconomic deprivation and alcohol-attributable mortality risk-a systematic review and meta-analysis. BMC Med. 2021, 19, 268. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Rehm, J.; Gmel, G.E.; Gmel, G.; Hasan, O.S.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Sanderson, S.; Tatt, I.D.; Higgins, J. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: A systematic review and annotated bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Cochran, W.G. The combination of estimates from different experiments. Biometrics 1954, 10, 101–129. [Google Scholar] [CrossRef]
- Collaboration, T.C. Identifying and measuring heterogeneity. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Green, S., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 2002, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 15 College Station; StataCorp LP: College Station, TX, USA, 2017. [Google Scholar]
- Connolly, S.; O′Reilly, D.; Rosato, M.; Cardwell, C. Area of residence and alcohol-related mortality risk: A five-year follow-up study. Addiction 2011, 106, 84–92. [Google Scholar] [CrossRef]
- Grigoriev, P.; Jasilionis, D.; Stumbrys, D.; Stankūnienė, V.; Shkolnikov, V.M. Individual- and area-level characteristics associated with alcohol-related mortality among adult Lithuanian males: A multilevel analysis based on census-linked data. PLoS ONE 2017, 12, e0181622. [Google Scholar] [CrossRef] [PubMed]
- Mäki, N.E.; Martikainen, P.T. The Effects of Education, Social Class and Income on Non-alcohol- and Alcohol-Associated Suicide Mortality: A Register-based Study of Finnish Men Aged 25–64. Eur. J. Popul. 2008, 24, 385–404. [Google Scholar] [CrossRef]
- Valtonen, M.; Laaksonen, D.E.; Laukkanen, J.; Tolmunen, T.; Rauramaa, R.; Viinamäki, H.; Kauhanen, J.; Lakka, T.; Niskanen, L. Leisure-time physical activity, cardiorespiratory fitness and feelings of hopelessness in men. BMC Public Health 2009, 9, 204. [Google Scholar] [CrossRef] [PubMed]
- Mustard, C.A.; Bielecky, A.; Etches, J.; Wilkins, R.; Tjepkema, M.; Amick, B.C.; Smith, P.M.; Aronson, K.J. Mortality following unemployment in Canada, 1991–2001. BMC Public Health 2013, 13, 441. [Google Scholar] [CrossRef]
- Pulido, J.; Vallejo, F.; Alonso-López, I.; Regidor, E.; Villar, F.; de la Fuente, L.; Domingo-Salvany, A.; Barrio, G. Directly alcohol-attributable mortality by industry and occupation in a Spanish Census cohort of economically active population. Drug Alcohol Depend. 2017, 180, 93–102. [Google Scholar] [CrossRef]
- Vågerö, D.; Garcy, A.M. Does unemployment cause long-term mortality? Selection and causation after the 1992-96 deep Swedish recession. Eur. J. Public Health 2016, 26, 778–783. [Google Scholar] [CrossRef]
- Zagozdzon, P.; Zaborski, L.; Ejsmont, J. Survival and cause-specific mortality among unemployed individuals in Poland during economic transition. J. Public Health 2009, 31, 138–146. [Google Scholar] [CrossRef][Green Version]
- Springer, K.W.; Stellman, J.M.; Jordan-Young, R.M. Beyond a catalogue of differences: A theoretical frame and good practice guidelines for researching sex/gender in human health. Soc. Sci. Med. 2012, 74, 1817–1824. [Google Scholar] [CrossRef] [PubMed]
- Garcy, A.M.; Vågerö, D. The length of unemployment predicts mortality, differently in men and women, and by cause of death: A six year mortality follow-up of the Swedish 1992–1996 recession. Soc. Sci. Med. 2012, 74, 1911–1920. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.L.; Lan, C.F.; Lee, C.H.; Huang, N.; Chou, Y.J. Involuntary unemployment and mortality in Taiwan. J. Formos. Med. Assoc. 2004, 103, 900–907. [Google Scholar] [PubMed]
- Brand, J.E.; Levy, B.R.; Gallo, W.T. Effects of layoffs and plant closings on subsequent depression among older workers. Res. Aging 2008, 30, 701–721. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, A.; Gustafsson, P.E.; Strandh, M.; Virtanen, P.; Janlert, U. It′s no surprise! Men are not hit more than women by the health consequences of unemployment in the Northern Swedish Cohort. Scand. J. Public Health 2011, 39, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Mäkelä, P.; Gmel, G.; Grittner, U.; Kuendig, H.; Kuntsche, S.; Bloomfield, K.; Room, R. Drinking patterns and their gender differences in Europe. Alcohol Alcohol. 2006, 41, i8–i18. [Google Scholar] [CrossRef]
- Grittner, U.; Kuntsche, S.; Gmel, G.; Bloomfield, K. Alcohol consumption and social inequality at the individual and country levels—Results from an international study. Eur. J. Public Health 2013, 23, 332–339. [Google Scholar] [CrossRef]
- Lahelma, E.; Kangas, R.; Manderbacka, K. Drinking and unemployment: Contrasting patterns among men and women. Drug Alcohol Depend. 1995, 37, 71–82. [Google Scholar] [CrossRef]
- Ahlström, S.; Bloomfield, K.; Knibbe, R. Gender Differences in Drinking Patterns in Nine European Countries: Descriptive Findings. Subst. Abus. 2001, 22, 69–85. [Google Scholar] [CrossRef]
- Bloomfield, K. Alcohol Consumption and Alcohol Problems Among Women in European Countries. Subst. Abus. 2000, 21, 223–229. [Google Scholar] [CrossRef]
- Marmot, M. Inequality, deprivation and alcohol use. Addiction 1997, 92, 13–20. [Google Scholar] [CrossRef]
- Van Oers, J.A.; Bongers, I.M.; Van de Goor, L.A.; Garretsen, H.F. Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol. 1999, 34, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Casswell, S.; Pledger, M.; Hooper, R. Socioeconomic status and drinking patterns in young adults. Addiction 2003, 98, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Bellis, M.A.; Hughes, K.; Nicholls, J.; Sheron, N.; Gilmore, I.; Jones, L. The alcohol harm paradox: Using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health 2016, 16, 111. [Google Scholar] [CrossRef]
- Lewer, D.; Meier, P.; Beard, E.; Boniface, S.; Kaner, E. Unravelling the alcohol harm paradox: A population-based study of social gradients across very heavy drinking thresholds. BMC Public Health 2016, 16, 599. [Google Scholar] [CrossRef]
- Henkel, D. Unemployment and Substance Use: A Review of the Literature (1990–2010). Curr. Drug Abus. Rev. 2011, 4, 4–27. [Google Scholar] [CrossRef]
- Blomgren, J.; Martikainen, P.; Mäkelä, P.; Valkonen, T. The effects of regional characteristics on alcohol-related mortality-a register-based multilevel analysis of 1.1 million men. Soc. Sci. Med. 2004, 58, 2523–2535. [Google Scholar] [CrossRef]
- Dietze, P.M.; Jolley, D.J.; Chikritzhs, T.N.; Clemens, S.; Catalano, P.; Stockwell, T. Income inequality and alcohol attributable harm in Australia. BMC Public Health 2009, 9, 70. [Google Scholar] [CrossRef]
- Galea, S.; Ahern, J.; Tracy, M.; Vlahov, D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am. J. Prev. Med. 2007, 32, S195–S202. [Google Scholar] [CrossRef]
- Puka, K.; Buckley, C.; Mulia, N.; Lasserre, A.M.; Rehm, J.; Probst, C. Educational Attainment and Lifestyle Risk Factors Associated with All-Cause Mortality in the United States: Decomposing differential exposure and vulnerability. JAMA Health Forum 2022, 3, e220401. [Google Scholar] [CrossRef]
- Hoffmann, R.; Kröger, H.; Pakpahan, E. Pathways between socioeconomic status and health: Does health selection or social causation dominate in Europe? Adv. Life Course Res. 2018, 36, 23–36. [Google Scholar] [CrossRef]
- Melzer, D.; Izmirlian, G.; Leveille, S.G.; Guralnik, J.M. Educational Differences in the Prevalence of Mobility Disability in Old Age: The Dynamics of Incidence, Mortality, and Recovery. J. Gerontol. 2001, 56, S294–S301. [Google Scholar] [CrossRef] [PubMed]
- Farmer, M.E.; Kittner, S.J.; Rae, D.S.; Bartko, J.J.; Regier, D.A. Education and change in cognitive function: The Epidemiologic Catchment Area Study. Ann. Epidemiol. 1995, 5, 1–7. [Google Scholar] [CrossRef]
- Ross, C.E.; Mirowsky, J. Does Unemployment Affect Health? J. Health Soc. Behav. 1995, 36, 230–243. [Google Scholar] [CrossRef]
- Lastrucci, V.; Lorini, C.; Caini, S.; Florence Health Literacy Research Group; Bonaccorsi, G. Health literacy as a mediator of the relationship between socioeconomic status and health: A cross-sectional study in a population-based sample in Florence. PLoS ONE 2019, 14, e0227007. [Google Scholar] [CrossRef]
- McGinnis, J.M.; Foege, W.H. Actual causes of death in the United States. JAMA 1993, 270, 2207–2212. [Google Scholar] [CrossRef]
- Leppo, K.; Ollila, E.; Pena, S.; Wismar, M.; Cook, S. Health in All Policies: Seizing Opportunities, Implementing Policies; Ministry of Social Affairs and Health: Helsinki, Finlan, 2013. [Google Scholar]
- Holmes, J.; Meng, Y.; Meier, P.S.; Brennan, A.; Angus, C.; Campbell-Burton, A.; Guo, Y.; Hill-McManus, D.; Purshouse, R.C. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: A modelling study. Lancet 2014, 383, 1655–1664. [Google Scholar] [CrossRef]
- Mulia, N.; Jones-Webb, R. Alcohol policy: A tool for addressing health disparities? In Preventing Alcohol-Related Problems: Evidence and Community-Based Initiatives; Giesbrecht, N., Bosma, L., Eds.; APHA Press: Washington, DC, USA, 2017; pp. 377–395. [Google Scholar]
- Roche, A.; Kostadinov, V.; Fischer, J.; Nicholas, R.; O′Rourke, K.; Pidd, K.; Trifonoff, A. Addressing inequities in alcohol consumption and related harms. Health Promot. Int. 2015, 30, ii20–ii35. [Google Scholar] [CrossRef]
- Anderson, P.; O’Donnell, A.; Kaner, E.; Llopis, E.J.; Manthey, J.; Rehm, J. Impact of minimum unit pricing on alcohol purchases in Scotland and Wales: Controlled interrupted time series analyses. Lancet Public Health 2021, 6, e557–e565. [Google Scholar] [CrossRef]
- Ployhart, R.E.; Shepherd, W.J.; Strizver, S.D. The COVID-19 pandemic and new hire engagement: Relationships with unemployment rates, state restrictions, and organizational tenure. J. Appl. Psychol. 2021, 106, 518–529. [Google Scholar] [CrossRef]
- Trish, E.; Fiedler, M.; Ning, N.; Gascue, L.; Adler, L.; Lin, E. Payment for Dialysis Services in the Individual Market. JAMA Intern. Med. 2021, 181, 698–699. [Google Scholar] [CrossRef] [PubMed]
- Blustein, D.L.; Duffy, R.; Ferreira, J.A.; Cohen-Scali, V.; Cinamon, R.G.; Allan, B.A. Unemployment in the time of COVID-19: A research agenda. J. Vocat. Behav. 2020, 119, 103436. [Google Scholar] [CrossRef] [PubMed]

| Reference | Country, Region/City | Study Years | Study Design | Age Range (Years) | Sample Size by Sex | Number of Deaths by Sex | Employment Status |
|---|---|---|---|---|---|---|---|
| Agren & Romelsjö, 1992 [19] | Sweden | 1970–1975 | Census-linkage | 25–46 | 2,008,000 (W), 2,044,000 (M) | 405 (W), 2237 (M) | professional, unemployed |
| Connolly et al. 2010 [32] | UK, Northern Ireland | 2001–2006 | Longitudinal | 25–74 | 369,245 (W), 351,382 (M) | 201 (W), 377 (M) | professional, unemployed |
| Grigoriev et al. 2017 [33] | Lithuania | 2011–2013 | Census-linkage | 30–64 | 1,246,000 (M) | 1424 (M) | employed, unemployed, inactive/disabled, other inactive |
| Herttua et al. 2008 [20] | Finland | 2000–2003 | Longitudinal | 30–59 | 2,018,000 (W), 1,891,000 (M) | 555 (W), 2749 (M) | employed, short unemployment, long unemployment |
| Mäki et al. 2008 [34] | Finland | 1990–2001 | Census-linkage | 25–64 | 1,051,626 (M) | 2703 (M) | employed, unemployed |
| Mäki et al. 2009 [35] | Finland | 1990–2001 | Census-linkage | 25–64 | 1,109,497 (W) | 563 (W) | employed, unemployed |
| Mustard et al. 2013 [36] | Canada | 1991–2001 | Census-linkage | 30–69 | 711,600 (W), 888,000 (M) | 207 (W), 926 (M) | employed, unemployed |
| Pulido et al. 2017 [37] | Spain | 2001–2011 | Census-linkage | 25–64 | 6,374,624 (W), 9,601,876 (M) | 602 (W), 5239 (M) | employed, unemployed |
| Vågerö & Garcy, 2016 [38] | Sweden | 1992–2002 | Census-linkage | 25–59 | 1,645,002 (W), 1,747,167 (M) | 314 (W), 960 (M) | employed, unemployed |
| Zagozdzon et al. 2009 [39] | Poland, Gdansk | 1999–2004 | Census-linkage | 20–59 (W), 20–64 (M) | 182,387 (W), 185,461 (M) | 300 (W), 1200 (M) | general population, unemployed |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saul, C.; Lange, S.; Probst, C. Employment Status and Alcohol-Attributable Mortality Risk—A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 7354. https://doi.org/10.3390/ijerph19127354
Saul C, Lange S, Probst C. Employment Status and Alcohol-Attributable Mortality Risk—A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(12):7354. https://doi.org/10.3390/ijerph19127354
Chicago/Turabian StyleSaul, Celine, Shannon Lange, and Charlotte Probst. 2022. "Employment Status and Alcohol-Attributable Mortality Risk—A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 12: 7354. https://doi.org/10.3390/ijerph19127354
APA StyleSaul, C., Lange, S., & Probst, C. (2022). Employment Status and Alcohol-Attributable Mortality Risk—A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(12), 7354. https://doi.org/10.3390/ijerph19127354








