Abstract
Being unemployed has been linked to various health burdens. In particular, there appears to be an association between unemployment and alcohol-attributable deaths. However, risk estimates presented in a previous review were based on only two studies. Thus, we estimated updated sex-stratified alcohol-attributable mortality risks for unemployed compared with employed individuals. A systematic literature search was conducted in August 2020 using the following databases: Embase, MEDLINE, PsycINFO, and Web of Science. The relative risk (RR) of dying from an alcohol-attributable cause of death for unemployed compared with employed individuals was summarized using sex-stratified random-effects DerSimonian-Laird meta-analyses. A total of 10 studies were identified, comprising about 14.4 million women and 19.0 million men, among whom there were about 3147 and 17,815 alcohol-attributable deaths, respectively. The pooled RRs were 3.64 (95% confidence interval (CI): 2.04–6.66) and 4.93 (95% CI 3.45–7.05) for women and men, respectively. The findings of our quantitative synthesis provide evidence that being unemployed is associated with an over three-fold higher risk of alcohol-attributable mortality compared with being employed. Consequently, a global public health strategy connecting brief interventions and specialized care with social services assisting those currently unemployed is needed.
1. Introduction
Social determinants of health, that is “the conditions in which people are born, grow, live, work and age” [1], are of increasing importance in health care and prevention. Being at the lower end of the socioeconomic spectrum, traditionally indicated by low income, education, or occupational status, is associated with poorer health compared with individuals at the upper end of the spectrum [2]. To address the root causes of highly unequal health outcomes, the World Health Organization established the Commission on Social Determinants of Health in 2005 [3]. Given the persistence of such inequalities, their reduction was also indicated as a global goal in the United Nations Sustainable Development Goals [4].
Although there are a number of core social determinants of health, employment status has been identified as especially important with respect to health outcomes [5]. Unemployment has been linked to detrimental health effects and heightened mortality risks. Specifically, being unemployed is associated with poorer physical health [5] and adverse mental health outcomes [6]. Further, unemployment has repeatedly been shown to be associated with increased all-cause mortality risk [7,8,9,10,11,12,13]. For instance, the hazard of all-cause mortality for those unemployed was increased by an amount equivalent to 10 extra years of age, compared with those employed [14]. Moreover, Roelfs and colleagues [12] found that unemployment was associated with a 63% increase in all-cause mortality risk.
It was forecasted that following a period of decline, the global unemployment rate in 2019 (5.4%) would remain stable for at least two years [15]. Then, unexpectedly, the coronavirus disease 2019 (COVID-19) pandemic resulted in a massive global unemployment crisis, causing the rate to increase to 6.3% in 2021 [16]. According to the International Labour Organization, approximately 33 million people became unemployed due to the COVID-19 crisis. Thus, the negative health outcomes associated with being unemployed are likely to increase throughout the world.
A simulation study [8] predicted that the economic recession due to the COVID-19 pandemic would result in 0.84 million additional deaths over the next 15 years. Although there is a notable impact of economic downturns and rising unemployment rates on all-cause mortality, their impact on alcohol-attributable mortality may be even higher. A review conducted in 2013 reported a 1.5- to 2-fold higher mortality risk for alcohol-attributable causes compared with all causes for individuals with lower socioeconomic status (SES) [17]. Another review examining alcohol-attributable mortality risks showed that unemployment in particular is associated with relative risks (RR) of 6.1 and 12.3 for women and men, respectively [18]. While there appears to be a link between unemployment and alcohol-attributable mortality risks, this review was based on only two studies [19,20]. Therefore, the present work aims to provide updated, sex-stratified estimates on the relative alcohol-attributable mortality risk depending on employment status based on the current evidence.
2. Methods
The current study presents a subset of data from a larger systematic review and meta-analysis; data on other socioeconomic variables are reported elsewhere [21]. In this first review, we performed dose–response meta-analyses for all indicators of SES except employment status, as that is most often dichotomous (e.g., unemployed vs. employed) and does not lend itself well to a dose-response investigation. The study protocol of the present systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA [22], Table S1) and was preregistered in PROSPERO (registration number CRD42019140279).
2.1. Systematic Literature Search
Embase, MEDLINE, PsycINFO, and Web of Science were searched from February 2013 until the last week of August 2020, updating a previous systematic review that included all studies published up to February 2013 [18]. The studies identified in the previous review were reconsidered for inclusion. Studies reporting on alcohol-attributable mortality among unemployed compared with employed individuals (or individuals having the highest level of occupation) of the general adult population were included. Search terms relating to alcohol consumption, mortality, employment status, and study design were used and adapted to each of the databases searched (see Text S1). We manually screened reference lists and cited articles of all identified studies. We did not apply any geographical or language restrictions.
2.2. Study Selection and Inclusion Criteria
Studies were eligible for inclusion if they consisted of original, quantitative research reporting on the relative alcohol-attributable mortality risk by employment status, including a measure of uncertainty (confidence interval [CI] or standard error) or sufficient original data to calculate the risk and/or uncertainty. Alcohol-attributable causes of death were defined as all underlying causes of death that are fully attributable to alcohol use [23]. Studies that included causes with an alcohol-attributable fraction (AAF) of at least 10% globally [24] (see Table S2, and Table S3 for ICD-codes) in addition to 100% attributable causes were also eligible. Study samples had to be based on the general adult (at least 15 years of age) population. Studies that used a longitudinal design with data-linkage, a cross-sectional design (deaths with a population denominator), or case-control design were eligible. For detailed inclusion and exclusion criteria, see Table S4.
Titles and abstracts were screened by three reviewers to exclude records with high certainty. Next, full texts of all potentially eligible records were assessed for inclusion. Reviewer consensus meetings were held to discuss inclusion in cases where eligibility was unclear or reviewers disagreed. To avoid double counting of individuals, studies reporting on overlapping or identical data were excluded, giving preference to age-adjusted and sex-stratified estimates.
2.3. Data Extraction
We extracted data on study population, study design, mortality assessment, employment status, sample size, death counts, results, and adjustment for confounding. Hazards ratios, RRs, and standardized mortality rate ratios were treated as equivalent measures of relative mortality risk. Where available, age-adjusted and sex-stratified risks were extracted with preference. The data extracted in the previous review including studies up to February 2013 were re-evaluated for inclusion before merging the original database with the data resulting from the new searches.
2.4. Quality Assessment
In line with the original systematic review [18], a quality assessment was performed using the following criteria [25]: representativeness of the sample; measurement and definition of the independent and dependent variables; linkage of survey data; age-adjustment (for details of each criterion see Table S4). No aggregate score was applied since these quality aspects differ in regard to their importance.
2.5. Statistical Analysis
Sex-stratified random-effects DerSimonian-Laird meta-analyses [26] were performed to summarize the RR of dying from an alcohol-attributable cause of death for unemployed individuals compared with employed individuals. Between-study heterogeneity was quantified using the I2 statistic [27] and Cochran’s Q [28]. I2 was interpreted based on pre-defined guidelines [29]. Potential publication bias was examined using Egger’s regression-based test [30]. We carried out exploratory sensitivity analyses to investigate the impact of overall study quality (all criteria fulfilled versus at least one criterion not fulfilled; Tables S5 and S6); and the impact of including causes of death that are less than 100% alcohol-attributable as part of the outcome. Sex-stratified DerSimonian-Laird random-effects meta regression models were used for sensitivity analyses [26]. Analyses were carried out in Stata 15 [31].
3. Results
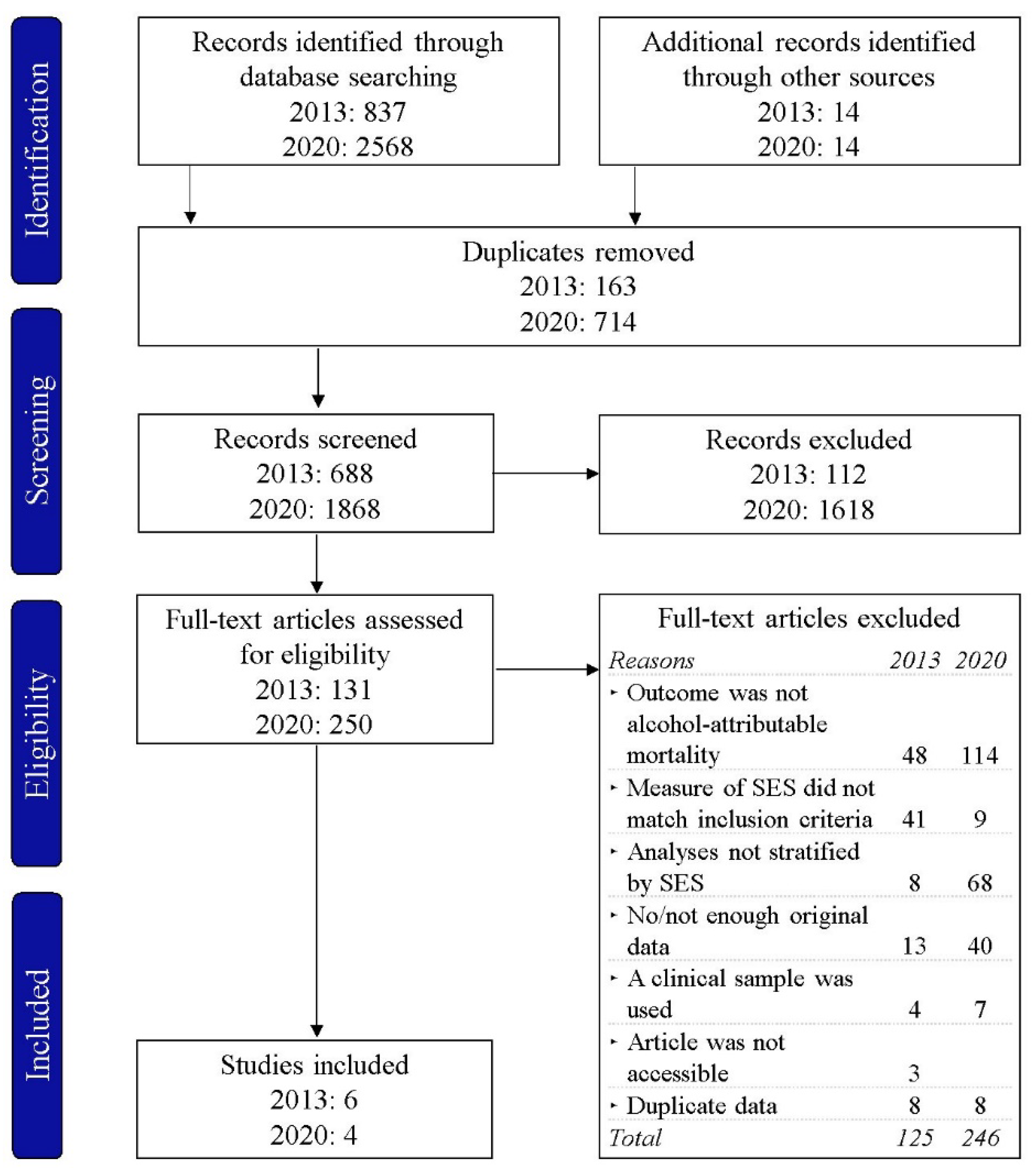
The PRISMA flow chart for study inclusion is shown in Figure 1. A total of ten studies were included in the systematic review, six of which were identified in the review performed in 2013, and four of which were newly identified.
Figure 1.
The PRISMA flow chart of the study selection for the search conducted in 2013 (including studies published up to February 2013) and 2020 (including studies published between January 2013 and August 2020). SES, socioeconomic status.
An overview of all studies included in the present meta-analysis is shown in Table 1. In total, the included studies reported findings based on about 14.4 million women and 19.0 million men, among whom there were about 3147 and 17,815 alcohol-attributable deaths, respectively. The studies included data from seven countries, all of which are European or North American high-income countries. With three studies reporting findings from Finland, two from Sweden, and one each from Canada, Lithuania, Poland (Gdansk), the UK (Northern Ireland), and Spain. The studies reported on data spanning over 40 years from 1970 (earliest baseline) up to 2013 (latest follow-up). The included data were obtained from census-linkage (n = 8) or longitudinal studies (n = 2). Studies differed in regard to their definition of employment status; most studies reported on employed and unemployed individuals (n = 6), while others compared professionals and unemployed (n = 2), employed, short- and long-time unemployed, or the general population and unemployed individuals. The causes of death included in each of the studies are listed in Table S7.

Table 1.
The characteristics of all studies included in the sex-stratified random-effect meta-analyses.
3.1. Relative Risks for Employment Status
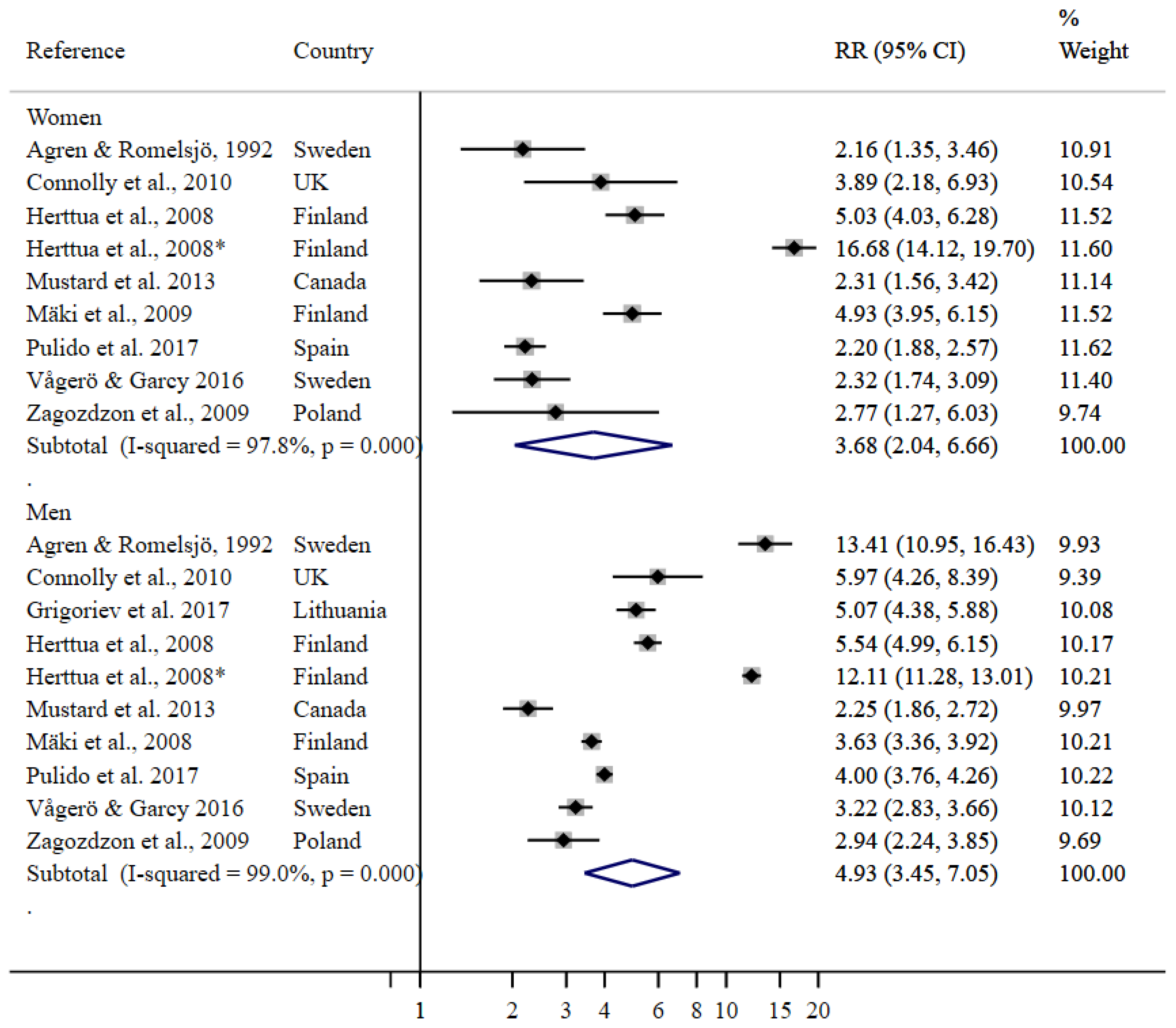
The RRs of dying from an alcohol-attributable cause of death for men and women who were unemployed compared with their employed counterparts were 3.68 (95% CI 2.04–6.66) and 4.93 (95% CI 3.45–7.05), respectively (Figure 2).
Figure 2.
Random-effects meta-regression for employment status. RR, relative risk; CI, confidence interval; UK, United Kingdom. * This estimate is referring to long-term unemployment, whereas the other estimate by Herttua et al. 2008 [20] is referring to short-term unemployment. For women refer to [19,20,32,35,36,37,38,39], for men refer to [19,20,32,33,34,36,37,38,39].
Herttua et al. 2008 [20] used short- and long-term unemployment as two levels of unemployment, both of which were included in the meta-analysis. Among both women and men, the higher point estimate refers to long-term unemployment. All studies used “employed” as the reference category, with the exception of Agren and Romelsjö, 1992 [19] and Connolly et al., 2010 [32] who used “professionals” (the highest level of occupation) as the reference group. Sensitivity analysis did not indicate meaningful differences in the resulting point estimate conditional on overall study quality or the inclusion of causes of death that are less than 100% alcohol-attributable (results available upon request).
3.2. Heterogeneity and Bias Control
Considerable heterogeneity was detected in the sex-stratified meta-analyses, with an I2 > 75% and p < 0.01. According to Egger’s weighted regression test, there was no evidence for the presence of publication bias.
4. Discussion
The present study reports the most comprehensive pooled risk estimates for alcohol-attributable mortality among unemployed relative to employed individuals using the current evidence, which is largely from Western high-income countries. Our findings indicate that overall, unemployed women have a 3.7-fold higher risk of dying from an alcohol-attributable cause of death compared with employed women. For men, the RR is even higher at 4.9. In contrast to the previous review, which included only two risk estimates [18], the RRs found in the present study (based on ten risk estimates for each of the sexes) are noticeably lower.
According to the present results, unemployed men were found to have a slightly higher alcohol-attributable mortality risk than unemployed women, compared with their employed counterparts. SES is interrelated with gender roles, behaviors, and social expectations [40]. Hence, gender may alter employment–health relationships, with men being more affected by unemployment than women [18,36,41,42]. Since women are traditionally less attached to the labor force [43] and have greater opportunities to switch between rewarding social roles (e.g., care giving) and being employed [44], the consequences of unemployment might affect their health less than it does for men. However, women’s labor force participation has increased substantially during the last few decades.
In many European countries, men drink more frequently and in higher quantities than women [45], possibly explaining the gender differences in our risk estimates. Further, it was found that there are larger differences in the prevalence of risky drinking patterns between men of high and low SES compared with women of high and low SES [46]. Particularly, the frequency of drinking-related health problems was significantly associated with unemployment among men [47]. Contrastingly, unemployment was found to be more strongly related to women’s alcohol consumption [48] and unemployment was associated with increased death rates due to alcohol abuse in women only [44].
Regardless of gender identity, a higher proportion of people in higher SES groups are found to be drinkers consuming smaller amounts of alcohol more frequently, whereas more people in lower SES groups are abstainers but those who do drink do so more often in problematic ways [46,49,50,51,52]. Conclusively, low SES groups tend to drink on fewer occasions but in higher quantities compared with high SES groups [53,54], with the unemployed in particular being likely to consume alcohol at risky levels [55]. While findings on the relationship between SES and drinking patterns are mixed [56,57,58], negative health-related consequences of alcohol use are consistently more prevalent among individuals at the lower end of the socioeconomic spectrum. Thus, both differential exposure and vulnerability may play a role when it comes to heightened mortality risks [59].
In the present study, we demonstrated a link between employment status and alcohol-attributable mortality. However, the underlying mechanisms of this association are not well understood. It has not yet been conclusively determined whether the health state affects a person’s employment status (health selection) or whether a person’s employment status determines health (social causation) [60]. For instance, high SES can serve as a buffer for more frequent and rapid cognitive decline [61] and even prevent disability [62]. On the other hand, there is a reverse causality with individuals with disabilities or serious illness facing unemployment [60]. This is in line with the observation that working individuals demonstrate better health [63], also referred to as the healthy worker effect. It may be even more likely that there is no direct pathway but that other individual-level risk factors are influencing SES and health (indirect selection) [60]). For instance, biological determinants, health literacy and health care, environmental exposure, behavior, and lifestyle [64,65] may moderate the SES-health-relationship. Since we included cohort– and case–control studies as well as cross-sectional studies, with the latter not providing any cause–effect information, this requires further investigation.
Strengths and Limitations
The presented review is the most comprehensive review of the current literature on the association between employment status and alcohol-attributable mortality risk, including data from ten individual studies. Moreover, we estimated sex-stratified risks, allowing for a more detailed understanding of the association between unemployment and mortality in men and women. However, some limitations have to be noted. First, we included studies that used different definitions of unemployment. While the majority of studies compared risks related to unemployment and employment, the risk estimates of two studies were based on an unemployed–professionals comparison [19,32], and one study compared unemployed individuals with the general population [39]. These differing definitions of the reference group may have influenced the estimated risks. Second, the included studies report on Western high-income countries. The results of the present review are therefore only generalizable to similarly structured countries in the Western world. Since three articles [20,34,35] included Finnish estimates and two studies [19,38] reported on Swedish data, the northern European region was slightly overrepresented. Despite this relative homogeneity of the included countries, there are several contextual modifying factors at both the individual and population level that likely modify the relationship between unemployment and alcohol-attributable mortality. These include, for example, age and marital status at the individual level and welfare policies and the broader economic context at the population level. While this meta-analysis provides a high-level estimate of the risk relationship, important modifying factors need to be investigated in future, country-specific research. Lastly, the operationalization of alcohol-attributable mortality varied between reviewed articles. Whereas most studies included only 100% alcohol-attributable deaths (see Table S2), few studies [34,35,39] additionally included deaths less than 100% alcohol-attributable (see Tables S3 and S7). However, sensitivity analyses did not indicate meaningful differences in the resulting risk estimate conditional on the operationalization of alcohol attributable causes of death.
5. Conclusions
In the present study, we synthesized all available data on the association between employment status and alcohol-attributable mortality risks. We found that unemployed individuals have a high risk of dying from an alcohol-attributable cause. This has important implications for the social support and welfare system, indicating that preventing unemployment may have considerable public health effects. Initiatives such as the Health in All Policies Approach by the World Health Organization [66] serve as a good starting point to tackle this challenge. Additionally, alcohol screening procedures could be directly applied in counselling centers or at primary health care services [55] to identify individuals at risk extensively and as early as possible to refer them to prevention programs or brief interventions. Alcohol control policies such as the SAFER project or minimum-unit pricing [67,68,69,70] and efforts to reduce global unemployment [71,72,73] further pose well-suited initiatives.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19127354/s1, Text S1: Search terms; Table S1: PRISMA 2009 checklist; Table S2: Diagnoses and ICD-10 codes of 100% alcohol-attributable conditions; Table S3: Diagnoses and ICD-10 codes of conditions with an alcohol-attributable fraction > 10% for mortality globally; Table S4: Inclusion criteria; Table S5: Quality rating; Table S6: Quality checklist. Ratings on population representativeness of the sample, measurement of socioeconomic status (SES), operationalization of alcohol-attributable mortality, data linkage, and age-adjustment for each study included in the meta-analysis. Table S7: Causes of death included in each of the studies.
Funding
The research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health (NIH) under award number R01 AA028009. Content is the responsibility of the authors and does not reflect official positions of the NIAAA or the NIH.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used in this study are available herein.
Acknowledgments
We would like to thank Sherald Sanchez and Carolin Kilian for their support in the systematic literature search.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- World Health Organization. Social Determinants of Health: World Health Organization; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Fiscella, K.; Williams, D.R. Health Disparities Based on Socioeconomic Inequities: Implications for Urban Health Care. Acad. Med. 2004, 79, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Commission on Social Determinants of Health. Closing the Gap in A Generation: Health Equity through Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: San Francisco, CA, USA, 2015. [Google Scholar]
- Hergenrather, K.C.; Zeglin, R.J.; McGuire-Kuletz, M.; Rhodes, S.D. Employment as a Social Determinant of Health: A Systematic Review of Longitudinal Studies Exploring the Relationship Between Employment Status and Physical Health. Rehabil. Res. Policy Educ. 2015, 29, 2–26. [Google Scholar] [CrossRef]
- Wanberg, C.R. The individual experience of unemployment. Annu. Rev. Psychol. 2012, 63, 369–396. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Life Expectancy Gain Due to Employment Status Depends on Race, Gender, Education, and Their Intersections. J. Racial Ethn. Health Disparities 2018, 5, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.; Bianchi, G.; Song, D. The Long-Term Impact of the COVID-19 Unemployment Shock on Life Expectancy and Mortality Rates. In NBER Working Paper Series; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Dunlavy, A.C.; Juárez, S.; Rostila, M. Employment status and risk of all-cause mortality among native- and foreign-origin persons in Sweden. Eur. J. Public Health 2018, 28, 891–897. [Google Scholar] [CrossRef]
- Laliotis, I.; Stavropoulou, C. Crises and mortality: Does the level of unemployment matter? Soc. Sci. Med. 2018, 214, 99–109. [Google Scholar] [CrossRef]
- Nie, J.; Wang, J.; Aune, D.; Huang, W.; Xiao, D.; Wang, Y.; Chen, X. Association between employment status and risk of all-cause and cause-specific mortality: A population-based prospective cohort study. J. Epidemiol. Community Health 2020, 74, 428–436. [Google Scholar] [CrossRef]
- Roelfs, D.J.; Shor, E.; Davidson, K.W.; Schwartz, J.E. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Soc. Sci. Med. 2011, 72, 840–854. [Google Scholar] [CrossRef]
- Yur’yev, A.; Värnik, A.; Värnik, P.; Sisask, M.; Leppik, L. Employment status influences suicide mortality in Europe. Int. J. Soc. Psychiatry 2012, 58, 62–68. [Google Scholar] [CrossRef]
- Tapia Granados, J.A.; House, J.S.; Ionides, E.L.; Burgard, S.; Schoeni, R.S. Individual joblessness, contextual unemployment, and mortality risk. Am. J. Epidemiol. 2014, 180, 280–287. [Google Scholar] [CrossRef]
- Gomis, R.; Kapsos, S.; Kuhn, S. World Employment and Social Outlook: Trends 2020; ILO: Geneva, Switzerland, 2020; pp. 127 (report) + 125p. (executive summary). [Google Scholar]
- Berg, J.; Hilal, A.; El, S.; Horne, R. World Employment and Social Outlook: Trends 2021; ILO: Geneva, Switzerland, 2021. [Google Scholar]
- Probst, C.; Roerecke, M.; Behrendt, S.; Rehm, J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: A systematic review and meta-analysis. Int. J. Epidemiol. 2014, 43, 1314–1327. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Roerecke, M.; Behrendt, S.; Rehm, J. Gender differences in socioeconomic inequality of alcohol-attributable mortality: A systematic review and meta-analysis. Drug Alcohol Rev. 2015, 34, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Ågren, G.; Romelsjü, A. Mortality in alcohol-related diseases in Sweden during 1971–80 in relation to occupation marital-status and citizenship in 1970. Scand. J. Soc. Med. 1992, 20, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Herttua, K.; Mäkelä, P.; Martikainen, P. Changes in alcohol-related mortality and its socioeconomic differences after a large reduction in alcohol prices: A natural experiment based on register data. Am. J. Epidemiol. 2008, 168, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Lange, S.; Kilian, C.; Saul, C.; Rehm, J. The dose-response relationship between socioeconomic deprivation and alcohol-attributable mortality risk-a systematic review and meta-analysis. BMC Med. 2021, 19, 268. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Rehm, J.; Gmel, G.E.; Gmel, G.; Hasan, O.S.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Sanderson, S.; Tatt, I.D.; Higgins, J. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: A systematic review and annotated bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Cochran, W.G. The combination of estimates from different experiments. Biometrics 1954, 10, 101–129. [Google Scholar] [CrossRef]
- Collaboration, T.C. Identifying and measuring heterogeneity. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Green, S., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 2002, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 15 College Station; StataCorp LP: College Station, TX, USA, 2017. [Google Scholar]
- Connolly, S.; O′Reilly, D.; Rosato, M.; Cardwell, C. Area of residence and alcohol-related mortality risk: A five-year follow-up study. Addiction 2011, 106, 84–92. [Google Scholar] [CrossRef]
- Grigoriev, P.; Jasilionis, D.; Stumbrys, D.; Stankūnienė, V.; Shkolnikov, V.M. Individual- and area-level characteristics associated with alcohol-related mortality among adult Lithuanian males: A multilevel analysis based on census-linked data. PLoS ONE 2017, 12, e0181622. [Google Scholar] [CrossRef] [PubMed]
- Mäki, N.E.; Martikainen, P.T. The Effects of Education, Social Class and Income on Non-alcohol- and Alcohol-Associated Suicide Mortality: A Register-based Study of Finnish Men Aged 25–64. Eur. J. Popul. 2008, 24, 385–404. [Google Scholar] [CrossRef]
- Valtonen, M.; Laaksonen, D.E.; Laukkanen, J.; Tolmunen, T.; Rauramaa, R.; Viinamäki, H.; Kauhanen, J.; Lakka, T.; Niskanen, L. Leisure-time physical activity, cardiorespiratory fitness and feelings of hopelessness in men. BMC Public Health 2009, 9, 204. [Google Scholar] [CrossRef] [PubMed]
- Mustard, C.A.; Bielecky, A.; Etches, J.; Wilkins, R.; Tjepkema, M.; Amick, B.C.; Smith, P.M.; Aronson, K.J. Mortality following unemployment in Canada, 1991–2001. BMC Public Health 2013, 13, 441. [Google Scholar] [CrossRef]
- Pulido, J.; Vallejo, F.; Alonso-López, I.; Regidor, E.; Villar, F.; de la Fuente, L.; Domingo-Salvany, A.; Barrio, G. Directly alcohol-attributable mortality by industry and occupation in a Spanish Census cohort of economically active population. Drug Alcohol Depend. 2017, 180, 93–102. [Google Scholar] [CrossRef]
- Vågerö, D.; Garcy, A.M. Does unemployment cause long-term mortality? Selection and causation after the 1992-96 deep Swedish recession. Eur. J. Public Health 2016, 26, 778–783. [Google Scholar] [CrossRef]
- Zagozdzon, P.; Zaborski, L.; Ejsmont, J. Survival and cause-specific mortality among unemployed individuals in Poland during economic transition. J. Public Health 2009, 31, 138–146. [Google Scholar] [CrossRef][Green Version]
- Springer, K.W.; Stellman, J.M.; Jordan-Young, R.M. Beyond a catalogue of differences: A theoretical frame and good practice guidelines for researching sex/gender in human health. Soc. Sci. Med. 2012, 74, 1817–1824. [Google Scholar] [CrossRef] [PubMed]
- Garcy, A.M.; Vågerö, D. The length of unemployment predicts mortality, differently in men and women, and by cause of death: A six year mortality follow-up of the Swedish 1992–1996 recession. Soc. Sci. Med. 2012, 74, 1911–1920. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.L.; Lan, C.F.; Lee, C.H.; Huang, N.; Chou, Y.J. Involuntary unemployment and mortality in Taiwan. J. Formos. Med. Assoc. 2004, 103, 900–907. [Google Scholar] [PubMed]
- Brand, J.E.; Levy, B.R.; Gallo, W.T. Effects of layoffs and plant closings on subsequent depression among older workers. Res. Aging 2008, 30, 701–721. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, A.; Gustafsson, P.E.; Strandh, M.; Virtanen, P.; Janlert, U. It′s no surprise! Men are not hit more than women by the health consequences of unemployment in the Northern Swedish Cohort. Scand. J. Public Health 2011, 39, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Mäkelä, P.; Gmel, G.; Grittner, U.; Kuendig, H.; Kuntsche, S.; Bloomfield, K.; Room, R. Drinking patterns and their gender differences in Europe. Alcohol Alcohol. 2006, 41, i8–i18. [Google Scholar] [CrossRef]
- Grittner, U.; Kuntsche, S.; Gmel, G.; Bloomfield, K. Alcohol consumption and social inequality at the individual and country levels—Results from an international study. Eur. J. Public Health 2013, 23, 332–339. [Google Scholar] [CrossRef]
- Lahelma, E.; Kangas, R.; Manderbacka, K. Drinking and unemployment: Contrasting patterns among men and women. Drug Alcohol Depend. 1995, 37, 71–82. [Google Scholar] [CrossRef]
- Ahlström, S.; Bloomfield, K.; Knibbe, R. Gender Differences in Drinking Patterns in Nine European Countries: Descriptive Findings. Subst. Abus. 2001, 22, 69–85. [Google Scholar] [CrossRef]
- Bloomfield, K. Alcohol Consumption and Alcohol Problems Among Women in European Countries. Subst. Abus. 2000, 21, 223–229. [Google Scholar] [CrossRef]
- Marmot, M. Inequality, deprivation and alcohol use. Addiction 1997, 92, 13–20. [Google Scholar] [CrossRef]
- Van Oers, J.A.; Bongers, I.M.; Van de Goor, L.A.; Garretsen, H.F. Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol. 1999, 34, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Casswell, S.; Pledger, M.; Hooper, R. Socioeconomic status and drinking patterns in young adults. Addiction 2003, 98, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Bellis, M.A.; Hughes, K.; Nicholls, J.; Sheron, N.; Gilmore, I.; Jones, L. The alcohol harm paradox: Using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health 2016, 16, 111. [Google Scholar] [CrossRef]
- Lewer, D.; Meier, P.; Beard, E.; Boniface, S.; Kaner, E. Unravelling the alcohol harm paradox: A population-based study of social gradients across very heavy drinking thresholds. BMC Public Health 2016, 16, 599. [Google Scholar] [CrossRef]
- Henkel, D. Unemployment and Substance Use: A Review of the Literature (1990–2010). Curr. Drug Abus. Rev. 2011, 4, 4–27. [Google Scholar] [CrossRef]
- Blomgren, J.; Martikainen, P.; Mäkelä, P.; Valkonen, T. The effects of regional characteristics on alcohol-related mortality-a register-based multilevel analysis of 1.1 million men. Soc. Sci. Med. 2004, 58, 2523–2535. [Google Scholar] [CrossRef]
- Dietze, P.M.; Jolley, D.J.; Chikritzhs, T.N.; Clemens, S.; Catalano, P.; Stockwell, T. Income inequality and alcohol attributable harm in Australia. BMC Public Health 2009, 9, 70. [Google Scholar] [CrossRef]
- Galea, S.; Ahern, J.; Tracy, M.; Vlahov, D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am. J. Prev. Med. 2007, 32, S195–S202. [Google Scholar] [CrossRef]
- Puka, K.; Buckley, C.; Mulia, N.; Lasserre, A.M.; Rehm, J.; Probst, C. Educational Attainment and Lifestyle Risk Factors Associated with All-Cause Mortality in the United States: Decomposing differential exposure and vulnerability. JAMA Health Forum 2022, 3, e220401. [Google Scholar] [CrossRef]
- Hoffmann, R.; Kröger, H.; Pakpahan, E. Pathways between socioeconomic status and health: Does health selection or social causation dominate in Europe? Adv. Life Course Res. 2018, 36, 23–36. [Google Scholar] [CrossRef]
- Melzer, D.; Izmirlian, G.; Leveille, S.G.; Guralnik, J.M. Educational Differences in the Prevalence of Mobility Disability in Old Age: The Dynamics of Incidence, Mortality, and Recovery. J. Gerontol. 2001, 56, S294–S301. [Google Scholar] [CrossRef] [PubMed]
- Farmer, M.E.; Kittner, S.J.; Rae, D.S.; Bartko, J.J.; Regier, D.A. Education and change in cognitive function: The Epidemiologic Catchment Area Study. Ann. Epidemiol. 1995, 5, 1–7. [Google Scholar] [CrossRef]
- Ross, C.E.; Mirowsky, J. Does Unemployment Affect Health? J. Health Soc. Behav. 1995, 36, 230–243. [Google Scholar] [CrossRef]
- Lastrucci, V.; Lorini, C.; Caini, S.; Florence Health Literacy Research Group; Bonaccorsi, G. Health literacy as a mediator of the relationship between socioeconomic status and health: A cross-sectional study in a population-based sample in Florence. PLoS ONE 2019, 14, e0227007. [Google Scholar] [CrossRef]
- McGinnis, J.M.; Foege, W.H. Actual causes of death in the United States. JAMA 1993, 270, 2207–2212. [Google Scholar] [CrossRef]
- Leppo, K.; Ollila, E.; Pena, S.; Wismar, M.; Cook, S. Health in All Policies: Seizing Opportunities, Implementing Policies; Ministry of Social Affairs and Health: Helsinki, Finlan, 2013. [Google Scholar]
- Holmes, J.; Meng, Y.; Meier, P.S.; Brennan, A.; Angus, C.; Campbell-Burton, A.; Guo, Y.; Hill-McManus, D.; Purshouse, R.C. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: A modelling study. Lancet 2014, 383, 1655–1664. [Google Scholar] [CrossRef]
- Mulia, N.; Jones-Webb, R. Alcohol policy: A tool for addressing health disparities? In Preventing Alcohol-Related Problems: Evidence and Community-Based Initiatives; Giesbrecht, N., Bosma, L., Eds.; APHA Press: Washington, DC, USA, 2017; pp. 377–395. [Google Scholar]
- Roche, A.; Kostadinov, V.; Fischer, J.; Nicholas, R.; O′Rourke, K.; Pidd, K.; Trifonoff, A. Addressing inequities in alcohol consumption and related harms. Health Promot. Int. 2015, 30, ii20–ii35. [Google Scholar] [CrossRef]
- Anderson, P.; O’Donnell, A.; Kaner, E.; Llopis, E.J.; Manthey, J.; Rehm, J. Impact of minimum unit pricing on alcohol purchases in Scotland and Wales: Controlled interrupted time series analyses. Lancet Public Health 2021, 6, e557–e565. [Google Scholar] [CrossRef]
- Ployhart, R.E.; Shepherd, W.J.; Strizver, S.D. The COVID-19 pandemic and new hire engagement: Relationships with unemployment rates, state restrictions, and organizational tenure. J. Appl. Psychol. 2021, 106, 518–529. [Google Scholar] [CrossRef]
- Trish, E.; Fiedler, M.; Ning, N.; Gascue, L.; Adler, L.; Lin, E. Payment for Dialysis Services in the Individual Market. JAMA Intern. Med. 2021, 181, 698–699. [Google Scholar] [CrossRef] [PubMed]
- Blustein, D.L.; Duffy, R.; Ferreira, J.A.; Cohen-Scali, V.; Cinamon, R.G.; Allan, B.A. Unemployment in the time of COVID-19: A research agenda. J. Vocat. Behav. 2020, 119, 103436. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).