“Room to Reflect”: A Pilot Workplace Resiliency Intervention for Nurses
Abstract
:1. Introduction
1.1. Current Well-Being Interventions
1.2. Gaps in Well-Being Interventions
1.3. Addressing the Gap
2. Conceptual Overview and Context of Intervention
3. Materials and Methods
3.1. Study Design and Aims
3.2. Room to Reflect Intervention
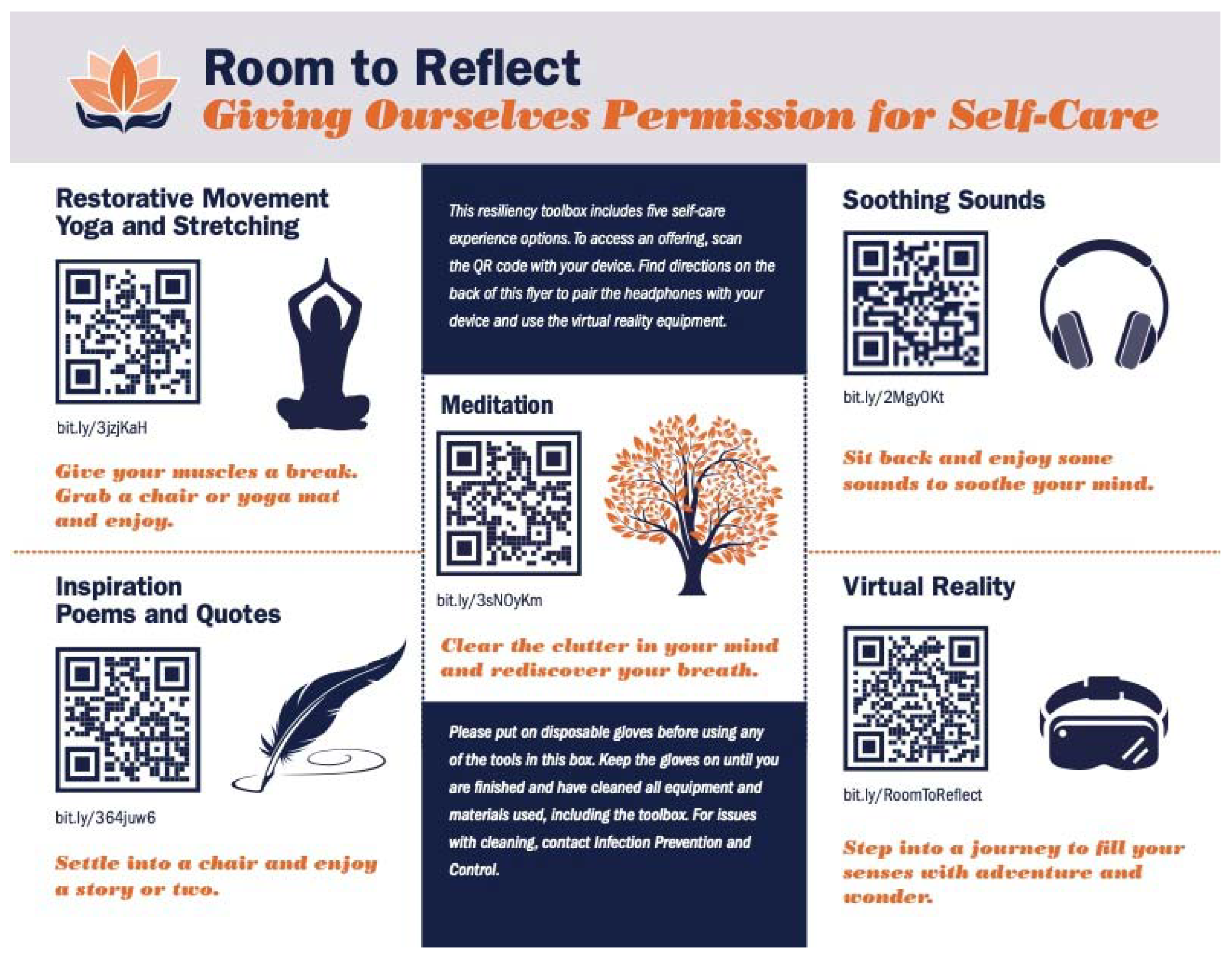
3.2.1. Mobile Toolbox
3.2.2. Quick Response Offerings: Audio and Visual
3.2.3. Pocket Guide
3.2.4. R2R Offering Development
3.3. Sample
3.4. Study Procedures
3.4.1. Questionnaire Dissemination
3.4.2. Research Assistant Role
3.5. Variables and Questionnaire Tools
3.5.1. Demographics
3.5.2. Connor Davidson Resilience Scale 10
3.5.3. Feasibility
3.5.4. Accessibility
3.5.5. Effectiveness
3.5.6. RN Manager Evaluation
3.6. Data Analysis
4. Results
4.1. Effectiveness: Resilience
4.2. Feasibility: Program Use and Barriers
4.3. Accessibility: Space and Support for Use
4.4. Restoration/Relaxation and Ease of Use
4.5. RN Manager Evaluation
5. Discussion
5.1. Limitations
5.2. Future Studies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being; The National Academies Press: Washington, DC, USA, 2019. [Google Scholar] [CrossRef]
- Manzano García, G.; Ayala Calvo, J.C. The threat of COVID-19 and Its Influence on Nursing Staff Burnout. J. Adv. Nurs. 2021, 77, 832–844. [Google Scholar] [CrossRef] [PubMed]
- Murat, M.; Köse, S.; Savaşer, S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int. J. Ment. Health Nurs. 2020, 30, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Shechter, A.; Chiuzan, C.; Shang, Y.; Ko, G.; Diaz, F.; Venner, H.K.; Shaw, K.; Cannone, D.E.; Mcmurry, C.L.; Sullivan, A.M.; et al. Prevalence, incidence, and factors associated with posttraumatic stress at three-month follow-up among New York City healthcare workers after the first wave of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 262. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Sun, C.; Chen, J.J.; Jen, H.J.; Kang, X.L.; Kao, C.C.; Chou, K.R. A Large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int. J. Ment. Health Nurs. 2021, 30, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Hsieh, A.P.; Tan, A.; Teall, A.M.; Weberg, D.; Jun, J.; Gawlik, K.; Hoying, J. Associations Among nurses’ mental/physical health, lifestyle behaviors, shift length, and workplace wellness support during COVID-19. Nurs. Adm. Q. 2022, 46, 5–18. [Google Scholar] [CrossRef] [PubMed]
- White, J.H. A phenomenological study of nurse managers’ and assistant nurse managers’ experiences during the COVID-19 pandemic in the United States. J. Nurs. Manag. 2021, 29, 1525–1534. [Google Scholar] [CrossRef]
- Boagaert, V. Developing resilience to combat nurse burnout. Quick Saf. 2019, 50, 1–4. [Google Scholar]
- Wei, H.; Roberts, P.; Strickler, J.; Corbett, R.W. Nurse leaders’ strategies to foster nurse resilience. J. Nurs. Manag. 2019, 27, 681–687. [Google Scholar] [CrossRef]
- Rushton, C.H.; Pappas, S. Systems to address burnout and support well-being: Implications for intensive care unit nurses. AACN Adv. Crit. Care 2020, 31, 141–145. [Google Scholar] [CrossRef]
- McAllister, M.; Lowe, J.B. Preparing for practice: Becoming resilient. In The Resilient Nurse: Empowering Your Practice; Springer Publishing Company: New York, NY, USA, 2011; pp. 1–22. [Google Scholar]
- Arrogante, O.; Aparicio-Zaldivar, E. Burnout and health among critical care professionals: The mediational role of resilience. Intensive Crit. Care Nurs. 2017, 42, 110–115. [Google Scholar] [CrossRef]
- Deldar, K.; Froutan, R.; Dalvand, S.; Gheshlagh, R.G.; Mazloum, S.R. The relationship between resiliency and burnout in Iranian nurses: A systematic review and meta-analysis. Open Access Maced. J. Med. Sci. 2018, 6, 2250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, H.; Sewell, K.A.; Woody, G.; Rose, M.A. The state of the science of nurse work environments in the United States: A systematic review. Int. J. Nurs. Sci. 2018, 5, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Chang, S.O. Exploring nurse perceptions and experiences of resilience: A meta-synthesis study. BMC Nurs. 2022, 21, 26. [Google Scholar] [CrossRef]
- Shanafelt, T.; Farley, H.; Wang, H.; Ripp, J.; CHARM CHO Network. Responsibilities and job characteristics of health care chief wellness officers in the United States. Mayo Clin. Proc. 2020, 95, 2563–2566. [Google Scholar] [CrossRef] [PubMed]
- Salmela, L.; Woehrle, T.; Marleau, E.; Kitch, L. Implementation of a “serenity room”: Promoting resiliency in the ED. Nursing2020 2020, 50, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Davidson, J.E.; Graham, P.; Montross-Thomas, L.; Norcross, W.; Zerbi, G. Code lavender: Cultivating intentional acts of kindness in response to stressful work situations. Explore 2017, 13, 181–185. [Google Scholar] [CrossRef]
- Goodman, M.J.; Schorling, J.B. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int. J. Psychiatry Med. 2012, 43, 119–128. [Google Scholar] [CrossRef]
- Cohen-Katz, J.; Wiley, S.; Capuano, T.; Baker, D.M.; Deitrick, L.; Shapiro, S. The effects of mindfulness-based stress reduction on nurse stress and burnout: A qualitative and quantitative study, Part III. Holist. Nurs. Pract. 2005, 19, 78–86. [Google Scholar] [CrossRef]
- Lengacher, C.; Reich, R.; Park, J.; Jim, H.; Ramesar, S.; Paterson, C.; Alinat, C.; Cousin, L.; Le, A.; Elias, M.; et al. A three arm randomized controlled trial on the efficacy of mindfulness-based stress reduction treatment on cognitive impairment among breast cancer survivors. Psycho-oncology 2017, 26, 82–83. [Google Scholar] [CrossRef] [Green Version]
- Zhai, X.; Ren, L.; Liu, Y.; Liu, C.; Su, X.; Feng, B. Resilience training for nurses: A meta-analysis. J. Hosp. Palliat. Nurs. 2021, 23, 544–550. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion Publishing: New York, NY, USA, 1994. [Google Scholar]
- Germer, C.K.; Neff, K.D. Self-compassion in clinical practice. J. Clin. Psychol. 2013, 69, 856–867. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Haro, M.V.; López-del-Hoyo, Y.; Campos, D.; Linehan, M.M.; Hoffman, H.G.; García-Palacios, A.; Modrego-Alarcón, M.; Borao, L.; García-Campayo, J. Meditation experts try virtual reality mindfulness: A pilot study evaluation of the feasibility and acceptability of virtual reality to facilitate mindfulness practice in people attending a mindfulness conference. PLoS ONE 2017, 12, e0187777. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, C.; Mulligan, P. Replenish at work: An integrative program to decrease stress and promote a culture of wellness in the intensive care unit. Crit. Care Nurs. Clin. N. Am. 2020, 32, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, T.; Meyer, R.M.L.; Grefe, D.; Gold, J.I. An on-the-job mindfulness-based intervention for pediatric ICU nurses: A pilot. J. Pediatric Nurs. 2015, 30, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Braganza, S.; Young, J.; Sweeny, A.; Brazil, V. OneED: Embedding a mindfulness-based wellness programme into an emergency department. Emerg. Med. Australas. 2018, 30, 678–686. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Poulin, P.A.; Seidman-Carlson, R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl. Nurs. Res. 2006, 19, 105–109. [Google Scholar] [CrossRef]
- Udod, S.; MacPhee, M.; Baxter, P. Rethinking resilience: Nurses and nurse leaders emerging from the post–COVID-19 environment. JONA J. Nurs. Adm. 2021, 51, 537–540. [Google Scholar] [CrossRef]
- Mintz-Binder, R.; Andersen, S.; Sweatt, L.; Song, H. Exploring strategies to build resiliency in nurses during work hours. J. Nurs. Adm. 2021, 51, 185–191. [Google Scholar] [CrossRef]
- Andersen, S.; Mintz-Binder, R.; Sweatt, L.; Song, H. Building nurse resilience in the workplace. Appl. Nurs. Res. 2021, 59, 151433. [Google Scholar] [CrossRef]
- Buetler, K.A.; Penalver-Andres, J.; Özen, Ö.; Ferriroli, L.; Müri, R.M.; Cazzoli, D.; Marchal-Crespo, L. “Tricking the Brain” using immersive virtual reality: Modifying the self-perception over embodied avatar influences motor cortical excitability and action initiation. Front. Hum. Neurosci. 2022, 15, 787487. [Google Scholar] [CrossRef]
- Riva, G.; Bernardelli, L.; Browning, M.H.E.M.; Castelnuovo, G.; Cavedoni, S.; Chirico, A.; Cipresso, P.; de Paula, D.M.B.; di Lernia, D.; Fernández-Álvarez, J.; et al. COVID feel good—An easy self-help virtual reality protocol to overcome the psychological burden of coronavirus. Front. Psychiatry 2020, 11, 996. [Google Scholar] [CrossRef] [PubMed]
- Browning, M.H.E.M.; Mimnaugh, K.J.; van Riper, C.J.; Laurent, H.K.; LaValle, S.M. Can simulated nature support mental health? Comparing short, single-doses of 360-degree nature videos in virtual reality with the outdoors. Front. Psychol. 2020, 10, 2667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wigram, T. The Psychological and physiological effects of low frequency sound and music. Music. Ther. Perspect. 1995, 13, 16–23. [Google Scholar] [CrossRef] [Green Version]
- Rogers, D.R.B.; Ei, S.; Rogers, K.R.; Cross, C.L. Evaluation of a multi-component approach to cognitive–behavioral therapy (CBT) using guided visualizations, cranial electrotherapy stimulation, and vibroacoustic sound. Complement. Ther. Clin. Pract. 2007, 13, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Greco, P.; Laschinger, H.K.S.; Wong, C. Leader Empowering behaviours, staff nurse empowerment and work engagement/burnout. Nurs. Leadersh. 2006, 19, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Grant, A.M.; Fried, Y. Work matters: Job design in classic and contemporary perspectives. In APA Handbook of Industrial and Organizational Psychology; Zedeck, S., Ed.; American Psychological Association: Washington, DC, USA, 2011. [Google Scholar]
- Rosa, H. Social acceleration: Ethical and political consequences of a desynchronized high-speed society. Constellations 2003, 10, 3–33. [Google Scholar] [CrossRef]
- Tetrick, L.E.; Winslow, C.J. Workplace stress management interventions and health promotion. Annu. Rev. Organ. Psychol. Organ. Behav. 2015, 2, 16–17. [Google Scholar] [CrossRef] [Green Version]
- Cocchiara, R.A.; Peruzzo, M.; Mannocci, A.; Ottolenghi, L.; Villari, P.; Polimeni, A.; Guerra, F.; Torre, G. The use of yoga to manage stress and burnout in healthcare workers: A systematic review. J. Clin. Med. 2019, 8, 284. [Google Scholar] [CrossRef] [Green Version]
- Fawcett, S.; Torres, J.; Jones, L.; Moffett, M.; Bradford, K.; Mantilla, M.R.; Cupertino, A.P.; de los Rios, J.B.; Collie-Akers, V. Assuring health access and culturally competent health services through the latino health for all coalition. Health Promot. Pract. 2018, 19, 765–774. [Google Scholar] [CrossRef]
- Adamson, K.; Sengsavang, S.; Charise, A.; Wall, S.; Kinross, L.; Balkaran, M. Narrative training as a method to promote nursing empathy within a pediatric rehabilitation setting. J. Pediatric Nurs. 2018, 42, e2–e9. [Google Scholar] [CrossRef]
- Muszkat, M.; Yehuda, A.B.; Moses, S.; Naparstek, Y. Teaching empathy through poetry: A clinically based model. Med. Educ. 2020, 44, 503. [Google Scholar] [CrossRef] [PubMed]
- Ratcliffe, E. Sound and soundscape in restorative natural environments: A narrative literature review. Front. Psychol. 2021, 12, 963. [Google Scholar] [CrossRef] [PubMed]
- Bates, V.; Hickman, C.; Manchester, H.; Prior, J.; Singer, S. Beyond landscape’s visible realm: Recorded sound, nature, and wellbeing. Health Place 2020, 61, 102271. [Google Scholar] [CrossRef] [PubMed]
- Beverly, E.I.; Hommema, L.I.; Coates, K.; Duncan, G.; GableID, B.; Gutman, T.; Love, M.; LoveID, C.; Pershing, M.; StevensID, N. A tranquil virtual reality experience to reduce subjective stress among COVID-19 frontline healthcare workers. PLoS ONE 2022, 17, e0262703. [Google Scholar] [CrossRef] [PubMed]
- Nijland, J.W.H.M.; Veling, W.; Lestestuiver, B.P.; van Driel, C.M.G. Virtual Reality relaxation for reducing perceived stress of intensive care nurses during the COVID-19 pandemic. Front. Psychol. 2021, 12, 4257. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The connor-davidson resilience scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Fain, K.M.; Nelson, J.T.; Tse, T.; Williams, R.J. Race and ethnicity reporting for clinical trials in clinicaltrials.gov and publications. Contemp. Clin. Trials 2021, 101, 106237. [Google Scholar] [CrossRef]
- Aloba, O.; Olabisi, O.; Aloba, T. The 10-item connor–davidson resilience scale: Factorial structure, reliability, validity, and correlates among student nurses in southwestern Nigeria. J. Am. Psychiatr. Nurses Assoc. 2016, 22, 43–51. [Google Scholar] [CrossRef]
- Jo, S.; Kurt, S.; Bennett, J.A.; Mayer, K.; Pituch, K.A.; Simpson, V.; Skibiski, J.; Takagi, E.; Karaaslan, M.M.; Ozluk, B.; et al. Nurses’ resilience in the face of coronavirus (COVID-19): An international view. Nurs. Health Sci. 2021, 23, 646–657. [Google Scholar] [CrossRef]
- Grimes, A.; Sparke, V.; Rouen, C.; West, C. Preparedness and resilience of student nurses in northern queensland Australia for disasters. Int. J. Disaster Risk Reduct. 2020, 48, 101585. [Google Scholar] [CrossRef]
- Nie, N.H.; Bent, D.H.; Hull, C.H. SPSS: Statistical Package for the Social Sciences; McGraw-Hill: New York, NY, USA, 1975; Volume 227. [Google Scholar]
- Kelly, L.A.; Gee, P.M.; Butler, R.J. Impact of nurse burnout on organizational and position turnover. Nurs. Outlook 2020, 69, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Carter, M.; Turner, K.M. Enhancing nurse manager resilience in a pandemic. Nurse Lead. 2021, 19, 622–624. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, M.; Williams, D.R.; le Menestrel, S. The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity; National Academy of Sciences: Washington, DC, USA, 2021; ISBN 0309685060. [Google Scholar]
- White, E.M.; Aiken, L.H.; McHugh, M.D. Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. J. Am. Geriatr. Soc. 2019, 67, 2065–2071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aiken, L.H.; Clarke, S.P.; Sloane, D.M.; Sochalski, J.; Silber, J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002, 288, 137–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armstrong, D.; Moore, J.; Fraher, E.P.; Frogner, B.K.; Pittman, P.; Spetz, J. COVID-19 and the health workforce. Med. Care Res. Rev. MCRR 2020, 78, 4S–6S. [Google Scholar] [CrossRef] [PubMed]
- Sonnentag, S. The recovery paradox: Portraying the complex interplay between job stressors, lack of recovery, and poor well-being. Res. Organ. Behav. 2018, 38, 169–185. [Google Scholar] [CrossRef]
- Steege, L.M.; Rainbow, J.G. Fatigue in hospital nurses—‘Supernurse’ culture is a barrier to addressing problems: A qualitative interview study. Int. J. Nurs. Stud. 2017, 67, 20–28. [Google Scholar] [CrossRef]
- Hockaday, M.S. Trauma leadership strategies to prevent and reduce burnout in urban academic trauma centers. J. Trauma Nurs. 2017, 24, 345–350. [Google Scholar] [CrossRef]
- Larson, R.B. Controlling social desirability bias. Int. J. Market. Res. 2019, 61, 534–547. [Google Scholar] [CrossRef]
- Johns, G. Advances in the treatment of context in organizational research. Annu. Rev. Organ. Psychol. Organ. Behav. 2018, 5, 21–46. [Google Scholar] [CrossRef]


| Toolbox Offerings | Rationale for Selection | Description |
|---|---|---|
| Restorative Movement Yoga and Stretching | Associated with reductions in health care worker stress and anxiety; improvements in self-regulation and self-compassion [42,43]. | Short guided video exercises in chair yoga, gentle stretches, and mindful movement. Participants used mobile devices and noise-canceling headphones. |
| Inspirational Poems and Quotes | Interventions with poetry readings associated with increased empathy for families, co-workers, and patients [44,45]. | Written and recorded short stories/poems. Participants access offerings with their mobile devices and noise-canceling headphones. |
| Meditation | Associated with reductions in perceived stress and burnout, as well as increased compassion. | Brief guided exercises on paying attention to the body and breathing. Participants listen with noise-canceling headphones. |
| Soothing Sounds | Sounds considered to be calming with low frequency are associated with improvements in sleep, quality of life, and depression [46,47]. | Curated sounds of nature from rain, to birds, to the roaring river rapids. Participants listened with noise-canceling headphones. |
| Virtual Reality | Curated landscapes emanating calming scenes associated with decreases in anxiety and stress and increases in social connectedness [25,33,34,35,48,49]. | VR 1 goggles compatible with mobile devices. Participants used their mobile devices to engage in 3D 2 visual experiences including animals, nature and art. |
| Sound Machine | Transmission of low frequency noises or calming sounds associated with reductions in anxiety, depressive symptoms, and sleep difficulty [36,37,46,47]. | Compact and portable with a timer; a variety of soothing sounds of nature to provide a relaxing and peaceful experience. |
| Pocket Guide | Easily accessible self-care practices for physical use and reading associated with stress reduction and increased resiliency [31,32]. | 3 × 5 laminated card stamped with QR 3 codes associated with pictorial representations of four everyday activities (e.g., Wash, Wipe, Walk, and Wait) conducive to mindfulness practices. |
| “W” Practice | Description |
|---|---|
| Wash | Prompts included 3 suggestions: (1) A simple breathing technique while approaching the sink (2) Awareness of senses while washing the hands (sight, hearing, touch) (3) Awareness of thoughts |
| Wipe | Prompts include the idea of transition from one task to the next with 2 suggestions: (1) Awareness of thoughts with prompts on how to identify and let go (2) A simple breathing technique to focus on the present moment and sensations. |
| Walk | Prompts include 4 suggestions: (1) Simple focus on the physical aspect of walking and paying attention to thoughts (2) Shorter walk prompt: Focusing on the breath while walking (3) Longer walk prompt: Focusing on all the senses (4) Practice of non-judgment of thoughts as “clouds in the sky” |
| Wait | Prompts identify examples of situations where waiting may occur during a busy day along with suggestions: (1) Simple breathing techniques with each encounter (2) Identifying thoughts (3) Present moment practice of using sensations (smell, touch, hearing) |
| Survey | Format | Description | Sample Question |
|---|---|---|---|
| CD-RISC 1 Score | Likert-style questions | Measures perceived resilience | I am able to adapt to change. |
| Demographics | Single-select answers | Assesses sample characteristics | How many years of clinical experience do you have? |
| Frequency of Access | Single-select answer | Amount of times R2R 2 was accessed | How many times did you access the R2R program offerings? |
| Barriers to Access | Select all that apply; free-text | Factors that prevented access to R2R | What barriers did you encounter that prevented R2R use? |
| Restoration/Relaxation | Dichotomous yes/no | Perceptions of effectiveness in feeling restored using R2R | Did you experience feeling relaxed and restored using Virtual Reality? |
| Ease of Program Access | Likert-style questions | Assesses level of ease accessing aspects of program | How easy was the Virtual Reality to use? |
| Appropriateness of Space | Dichotomous yes/no | Assesses quality of space to use R2R | Did you feel that the space for R2R was appropriate? |
| Support for Program | Dichotomous yes/no | Assesses perceived support use R2R | Did you have leadership/co-worker support for R2R? |
| Impact of Program 3 | Dichotomous yes/no; select all that apply | Assesses managers’ perceived impact of R2R on unit | Did you feel that R2R had an impact on your unit? |
| Supporting Program 3 | Select all that apply | Assess managers’ ability to support staff | How did you support R2R on your unit? |
| Implementation of Program, Barriers 3 | Select all that apply | Assess managers’ perceived barriers | What barriers did you find in implementing R2R on your unit? |
| Characteristics | Count | % |
|---|---|---|
| Clinical Ladder | ||
| Clinician 1 | 3 | 3.1 |
| Clinician 2 | 53 | 55.2 |
| Clinician 3 | 24 | 25.0 |
| Clinician 4 | 8 | 8.3 |
| Other, no specification | 1 | 0.2 |
| Manager/Assistant Manager | 8 | 8.2 |
| Length of RN 1 practice | ||
| Less than 1 year | 3 | 3. |
| 1–5 | 29 | 29.9 |
| 6–10 | 18 | 18.6 |
| 11–15 | 13 | 13.4 |
| Greater than 15 | 34 | 34.1 |
| Race | Count | |
| Asian/Asian American | 3 | 3.1 |
| Black/African American/African/Caribbean | 7 | 7.2 |
| Hispanic/Latinx | 1 | 1.0 |
| White/European/Middle East/North African | 84 | 86.6 |
| Other | 2 | 2.1 |
| Ethnicity | ||
| Hispanic | 3 | 3.2 |
| Non-Hispanic | 91 | 96.8 |
| Gender | ||
| Male | 12 | 12.4 |
| Female | 85 | 87.6 |
| Age | ||
| 20–30 | 24 | 24.7 |
| 31–40 | 27 | 27.8 |
| 41–50 | 21 | 21.7 |
| 51–60 | 18 | 18.6 |
| 61+ | 7 | 7.2 |
| Pre-Intervention | ||||
|---|---|---|---|---|
| Variable | 1. Resilience | 2. Gender | 3. Age | 4. Clinical Ladder |
| 1. Resilience Scale | - | −0.08 | 0.26 ** | 0.10 |
| 2. Gender | −0.08 | - | 0.08 | 0.27 * |
| 3. Age | 0.26 ** | 0.08 | - | 0.22 * |
| 4. Clinical Ladder | 0.10 | 0.27 * | 0.22 * | - |
| Post-Intervention | ||||
| Variable | 1. Resilience | 2. Gender | 3. Age | 4. Clinical Ladder |
| 1. Resilience Scale | - | −0.11 | 0.25 | 0.16 |
| 2. Gender | −0.11 | - | 0.08 | 0.27 ** |
| 3. Age | 0.25 | 0.08 | - | 0.22 * |
| 4. Clinical Ladder | 0.17 | 0.27 ** | 0.22 * | - |
| Variable | Baseline | Post-Intervention | ||||
|---|---|---|---|---|---|---|
| Staff (n = 89) | NMs 1 (n = 8) | Staff (n = 50) | NMs (n = 7) | |||
| M (SD) | M (SD) | p-value | M (SD) | M (SD) | p-value | |
| CD-RISC2 | 28.9 (4.8) | 27.9 (4.1) | 0.65 | 29.7 (5.0) | 40.0 (4.2) | 0.88 |
| Pre-Intervention (All) | Pre-Intervention (Dropouts) | Post-Intervention | Post-Preintervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | n | M | SD | n | M | SD | p-Value | |
| Staff | 89 | 28.9 | 4.8 | 39 | 28.3 | 4.5 | 50 | 29.7 | 5 | 50 | −0.8 | 4.1 | 0.19 |
| NMs 1 | 8 | 27.9 | 4.1 | 1 | 29 | N/A | 7 | 30 | 4.2 | 7 | −2.5 | 1.5 | <0.05 |
| Combined | 97 | 28.7 | 4.7 | 40 | 28.4 | 4.4 | 57 | 29.7 | 4.9 | 57 | −0.9 | 3.9 | 0.07 |
| Study Question | Subcategory | No | Yes | NA | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Staff Nurse Evaluation | |||||||
| Did you have leadership or co-worker support to use R2R? | 13 | 22.8 | 38 | 66.7 | 6 | 10.5 | |
| Did you feel that the space was appropriate? | 14 | 27.5 | 26 | 50.9 | 11 | 21.6 | |
| Did you feel relaxed/restored using the offerings? | Pocket Guide | 3 | 5.3 | 24 | 42.1 | 30 | 52.6 |
| Restorative Movement | 2 | 3.5 | 13 | 22.8 | 42 | 73.7 | |
| Inspiration | 4 | 7.0 | 8 | 14.1 | 45 | 78.9 | |
| Meditation | 1 | 1.8 | 16 | 28.1 | 40 | 70.1 | |
| Soothing Sounds | 1 | 1.8 | 18 | 31.6 | 38 | 66.6 | |
| Virtual Reality | 1 | 1.8 | 17 | 29.8 | 39 | 68.4 | |
| Sound Bar | 2 | 3.5 | 4 | 7.0 | 51 | 89.5 | |
| Nurse Manager Evaluation | |||||||
| Did you feel that the program was successfully implemented? | 2 | 28.6 | 5 | 71.4 | |||
| Component | Ease of Use, n (%) | ||||
|---|---|---|---|---|---|
| Very Easy | Easy | Neither Easy Nor Difficult | Difficult | Not Used | |
| Pocket Guide | 23 (40.4) | 8 (14.0) | 0 | 0 | 20 (35.1) |
| Restorative Movement | 4 (7.0) | 11 (19.3) | 1 (1.8) | 0 | 35 (61.4) |
| Inspiration | 6 (10.5) | 9 (15.8) | 2 (3.5) | 0 | 34 (59.7) |
| Meditation | 7 (12.3) | 12 (21.1) | 0 | 1(1.8) | 31 (54.4) |
| Soothing Sounds | 7 (12.3) | 8 (14.0) | 3 (5.3) | 0 | 33 (57.9) |
| Virtual Reality | 4 (7.0) | 9 (15.8) | 8 (14.0) | 1 (1.8) | 28 (49.1) |
| Sound Bar | 2 (3.5) | 5 (8.8) | 2 (3.5) | 0 | 40 (70.2) |
| Format | Offering | Count (%) |
|---|---|---|
| Virtual Reality Video | Experience Animals | 154 (35) |
| Experience Wonder | 122 (27.7) | |
| Experience Nature | 120 (27.3) | |
| Experience Guided Meditation | 15 (3.4) | |
| Experience Travel | 29 (6.6) | |
| Total VR | 440 | |
| Other Video | Body Movement | 77 (100) |
| Total General Video | 77 | |
| Audio | Meditation | 57 (45.6) |
| Inspirational Poems and Quotes | 48 (38.4) | |
| Soothing Sounds | 20 (16.0) | |
| Total Audio | 125 | |
| Pocket Guide | Wash | 135 (47.4) |
| Wait | 55 (19.3) | |
| Wipe | 51 (17.9) | |
| Walk | 44 (15.4) | |
| Total Pocket Guide | 285 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muir, K.J.; Webb-Jones, J.; Farish, N.; Barker, K.; Miller-Davis, C.; Galloway, S. “Room to Reflect”: A Pilot Workplace Resiliency Intervention for Nurses. Int. J. Environ. Res. Public Health 2022, 19, 7272. https://doi.org/10.3390/ijerph19127272
Muir KJ, Webb-Jones J, Farish N, Barker K, Miller-Davis C, Galloway S. “Room to Reflect”: A Pilot Workplace Resiliency Intervention for Nurses. International Journal of Environmental Research and Public Health. 2022; 19(12):7272. https://doi.org/10.3390/ijerph19127272
Chicago/Turabian StyleMuir, K. Jane, Jeanell Webb-Jones, Nancy Farish, Kimberley Barker, Claiborne Miller-Davis, and Susan Galloway. 2022. "“Room to Reflect”: A Pilot Workplace Resiliency Intervention for Nurses" International Journal of Environmental Research and Public Health 19, no. 12: 7272. https://doi.org/10.3390/ijerph19127272
APA StyleMuir, K. J., Webb-Jones, J., Farish, N., Barker, K., Miller-Davis, C., & Galloway, S. (2022). “Room to Reflect”: A Pilot Workplace Resiliency Intervention for Nurses. International Journal of Environmental Research and Public Health, 19(12), 7272. https://doi.org/10.3390/ijerph19127272






