Evaluation of Physical Therapy Interventions for Improving Musculoskeletal Pain and Quality of Life in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Outcomes Measures
2.3. Interventions
2.3.1. Geriatric Physical Therapy Group
2.3.2. Standardized Therapeutic Exercise Group
2.4. Statistical Procedure
3. Results
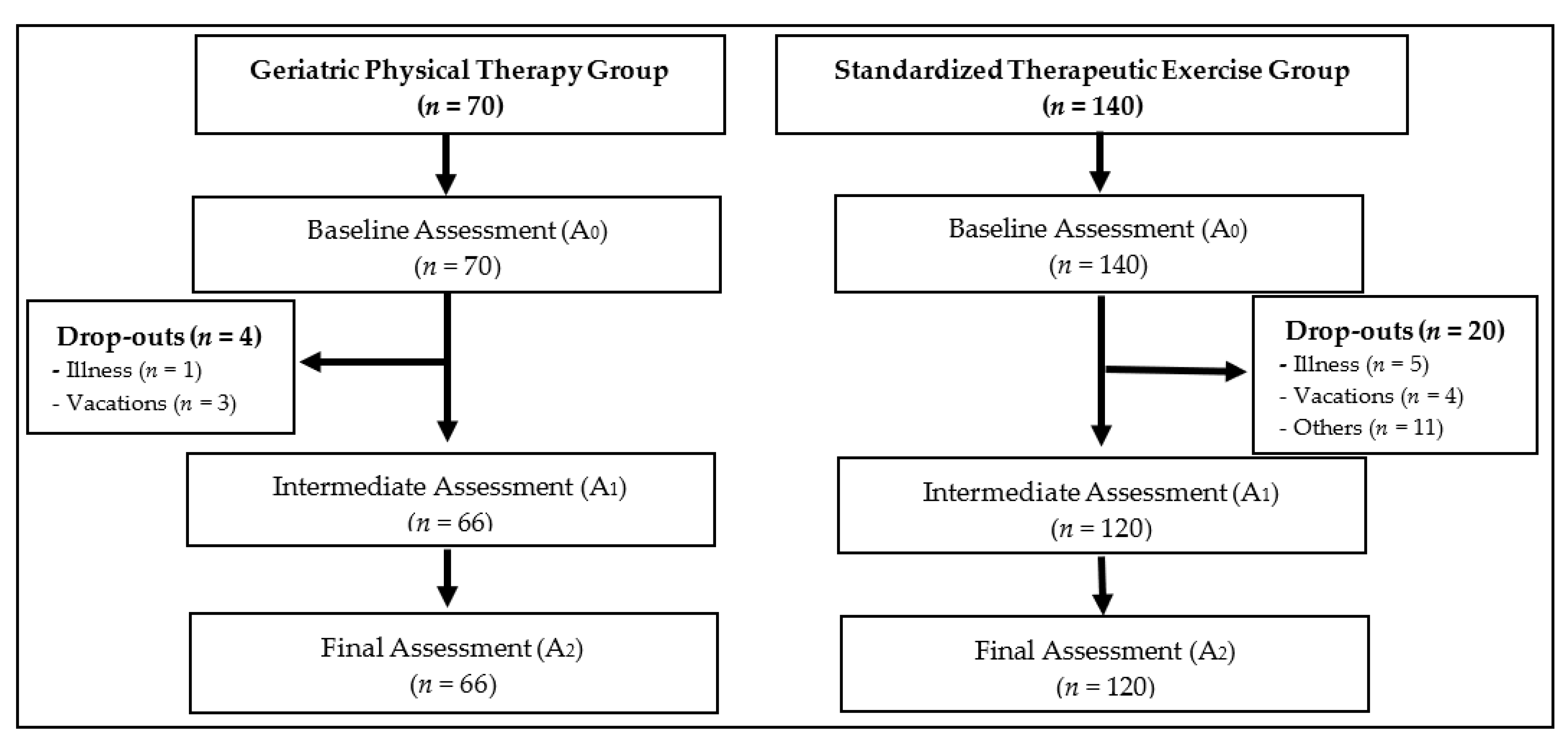
3.1. Participant Flow
3.2. Baseline Data
3.3. Geriatric Physical Therapy Group Intervention
3.4. Standardized Therapeutic Exercise Group Intervention
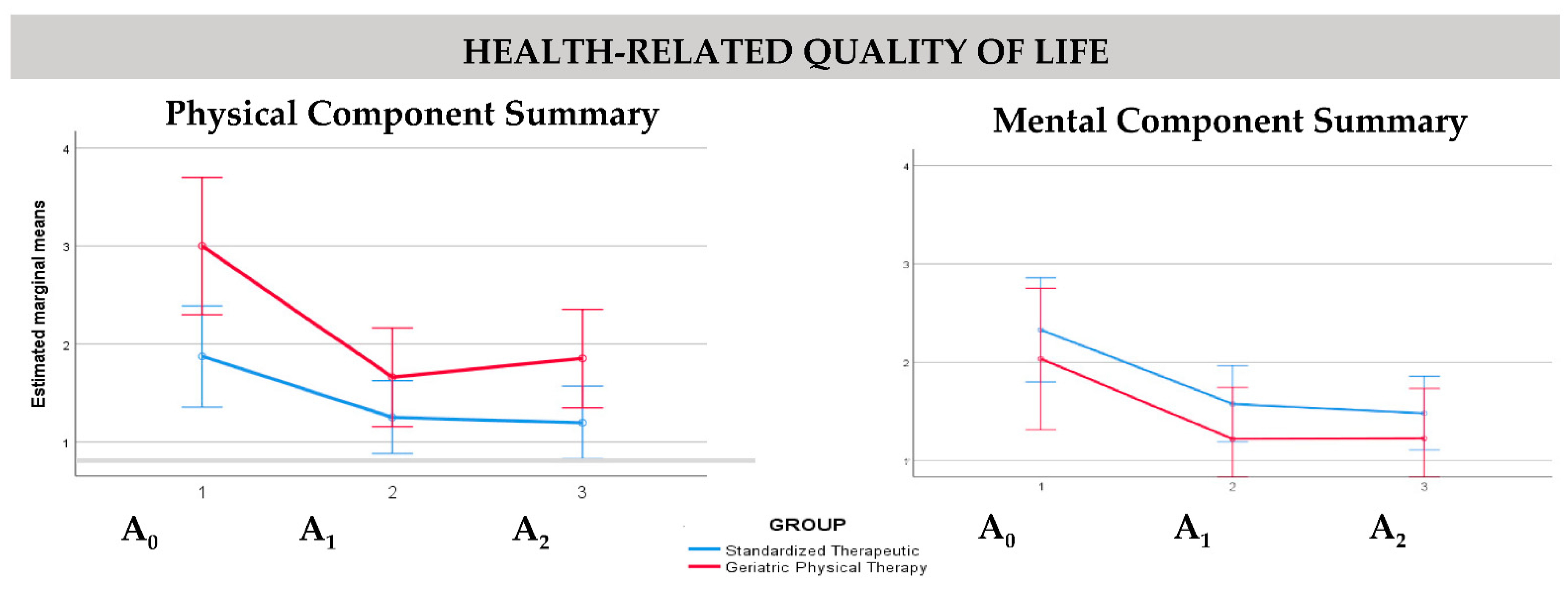
3.5. Comparison between Interventions: Repeated Measures Multivariate Models
3.6. Clinical Effectiveness in the Geriatric Physiotherapy Group and Standardized Therapeutic Exercise Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Organización Mundial de la Salud. Estrategia y Plan de Acción Mundiales Sobre el Envejecimiento y la Salud 2016–2020: Hacia un Mundo en el que Todas las Personas Puedan Vivir una Vida Prolongada y Sana. 69ª Asamblea Mundial de la Salud. 24 de mayo de 2016. OMS, 2016. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_17-sp.pdf?ua=1 (accessed on 8 April 2022).
- United Nations Organization—Década de Envejecimiento Saludable (2020–2030). Available online: https://www.paho.org/es/decada-envejecimiento-saludable-2020-2030 (accessed on 8 April 2022).
- Blázquez-Fernández, C.; Cantarero-Prieto, D.; Pascual-Sáez, M. Quality of Life, Health and the Great Recession in Spain: Why Older People Matter? Int. J. Environ. Res. Public Health 2021, 18, 2028. [Google Scholar] [CrossRef] [PubMed]
- Rondón-García, L.M.; Ramírez-Navarrro, J.M. The Impact of Quality of Life on the Health of Older People from a Multidimensional Perspective. J. Aging Res. 2018, 2018, 4086294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crocker, T.F.; Brown, L.; Clegg, A.; Farley, K.; Franklin, M.; Simpkins, S.; Young, J. Quality of life is substantially worse for community-dwelling older people living with frailty: Systematic review and meta-analysis. Qual. Life Res. 2019, 28, 2041–2056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palacios-Ceña, D.; Alonso-Blanco, C.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Jiménez-García, R.; Fernández-de-las-Peñas, C. Prevalence of neck and low back pain in community-dwelling adults in Spain: An updated population-based national study (2009/10–2011/12). Eur. Spine J. 2015, 24, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-Las-Peñas, C.; Alonso-Blanco, C.; Hernández-Barrera, V.; Palacios-Ceña, D.; Jiménez-García, R.; Carrasco-Garrido, P. Has the prevalence of neck pain and low back pain changed over the last 5 years? A population-based national study in Spain. Spine J. 2013, 13, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, E. The association between elderly people’s sedentary behaviours and their health-related quality of life: Focusing on comparing the young-old and the old-old. Health Qual. Life Outcomes 2019, 17, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, C.; O’Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behaviour affect one another? Prog. Cardiovasc. Dis. 2021, 64, 108–110. [Google Scholar] [CrossRef]
- Kotarska, K.; Nowak, M.A.; Nowak, L.; Król, P.; Sochacki, A.; Sygit, K.; Sygit, M. Physical Activity and Quality of Life of University Students, Their Parents, and Grandparents in Poland—Selected Determinants. Int. J. Environ. Res. Public Health 2021, 18, 3871. [Google Scholar] [CrossRef]
- Langley, P.; Pérez-Hernández, C.; Margarit-Ferri, C.; Ruiz Hidalgo, D.; Lubián López, M. Pain, health related quality of life and healthcare resource utilization in Spain. J. Med. Econ. 2011, 14, 628–638. [Google Scholar] [CrossRef]
- Dueñas, M.; Ojeda, B.; Salazar, A.; Fernández-Palacín, F.; Micó, J.A.; Torres, L.M.; Failde, I. Use and satisfaction with the Healthcare System of the chronic pain patients in Spain: Results from a nationwide study. Curr. Med. Res. Opin. 2016, 32, 1813–1820. [Google Scholar] [CrossRef]
- Valenzuela-Pascual, F.; García-Martínez, E.; Molina-Luque, F.; Soler-González, J.; Blanco-Blanco, J.; Rubí-Carnacea, F.; Climent-Sanz, C.; Briones-Vozmediano, E. Patients’ and primary healthcare professionals’ perceptions regarding chronic low back pain and its management in Spain: A qualitative study. Disabil. Rehabil. 2019, 43, 2568–2577. [Google Scholar] [CrossRef]
- Albaladejo, C.; Kovacs, F.M.; Royuela, A.; Pino, R.D.; Zamora, J. The Efficacy of a Short Education Program and a Short Physiotherapy Program for Treating Low Back Pain in Primary Care A Cluster Randomized Trial. Spine 2010, 35, 483–496. [Google Scholar] [CrossRef]
- Gustavsson, C.; Denison, E.; Koch, L.V. Self-management of persistent neck pain: A randomized controlled trial of a multi-component group intervention in primary health care. Eur. J. Pain 2010, 14, 630.e1–630.e11. [Google Scholar] [CrossRef]
- Zakoscielna, K.; Parmelee, P. Pain Variability and Its Predictors in Older Adults: Depression, Cognition, Functional Status, Health, and Pain. J. Ageing Health 2013, 25, 1329–1339. [Google Scholar] [CrossRef]
- Abdulla, A.; Adams, N.; Bone, M.; Elliott, A.M.; Gaffin, J. Jones, D.; Knaggs, R.; Martin, D.; Sampson, L.; Schofield, P.; et al. Guidance on the management of pain in older people. Age Ageing 2013, 42 (Suppl. S1), i1-57. [Google Scholar]
- Denkinger, M.D.; Lukas, A.; Nikolaus, T.; Peter, R.; Franke, S. Multisite pain, pain frequency and pain severity are associated with depression in older adults: Results from the ActiFE Ulm study. Age Ageing 2014, 43, 510–514. [Google Scholar] [CrossRef] [Green Version]
- Mollinedo-Cardalda, I.; Rodríguez, A.L.; Ferreira, M.; Cancela-Carral, J.M. Benefits of STRENOLD Program on Health-Related Quality of Life in Adults Aged 60 Years or Older. In Common Sport Study. Int. J. Environ. Res. Public Health 2021, 18, 3253. [Google Scholar] [CrossRef]
- Vadalà, G.; Russo, F.; De Salvatore, S.; Cortina, G.; Albo, E.; Papalia, R.; Denaro, V. Physical Activity for the Treatment of Chronic Low Back Pain in Elderly Patients: A Systematic Review. J. Clin. Med. 2020, 9, 1023. [Google Scholar] [CrossRef] [Green Version]
- Czarnecki, P.; Podgórska-Bednarz, J.; Perenc, L. Forms of physical activity of the elderly. Eur. J. Clin. Exp. Med. 2020, 18, 221–228. [Google Scholar] [CrossRef]
- Buckinx, F.; Peyrusqué, É.; Granet, J.; Aubertin-Leheudre, M. Impact of current or past physical activity level on functional capacities and body composition among elderly people: A cross-sectional analysis from the YMCA study. Arch. Public Health 2021, 79, 50. [Google Scholar] [CrossRef]
- Keefe, F.J.; Porter, L.; Somers, T.; Shelby, R.; Wren, A.V. Psychosocial interventions for managing pain in older adults: Outcomes and clinical implications. Br. J. Anaesth. 2013, 111, 89–94. [Google Scholar] [CrossRef] [Green Version]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef]
- Häkkinen, A.; Kautiainen, H.; Hannonen, P.; Ylinen, J. Strength training and stretching versus stretching only in the treatment of patients with chronic neck pain: A randomized one-year follow-up study. Clin. Rehabil. 2008, 22, 592–600. [Google Scholar] [CrossRef]
- Bier, J.D.; Scholten-Peeters, W.G.M.; Staal, J.B.; Pool, J.; van-Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical Practice Guideline for Physical Therapy Assessment and Treatment in Patients with Nonspecific Neck Pain. Phys. Ther. 2018, 98, 162–171. [Google Scholar] [CrossRef] [Green Version]
- Sefton, J.M.; Yarar, C.; Carpenter, D.M.; Berry, J.W. Physiological and clinical changes after therapeutic Massage of the neck and shoulders. Man. Ther. 2011, 16, 487–494. [Google Scholar] [CrossRef]
- Bertozzi, L.; Gardenghi, I.; Turoni, F.; Villafane, J.H.; Capra, F.; Guccione, A.A.; Pillastrini, P. Effect of Therapeutic Exercise on Pain and Disability in the Management of Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis of Randomized Trials. Phys. Ther. 2013, 93, 1026–1036. [Google Scholar] [CrossRef] [Green Version]
- Ma, C.; Szeto, G.P.; Yan, T.; Wu, S.; Lin, C.; Li, L. Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2011, 92, 849–858. [Google Scholar] [CrossRef]
- Hidalgo, B.; Hall, T.; Bossert, J.; Dugeny, A.; Cagnie, B.; Pitance, L. The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. J. Back Musculoskelet. Rehabil. 2017, 30, 1149–1169. [Google Scholar] [CrossRef] [Green Version]
- Fredin, K.; Lorås, H. Manual therapy, exercise therapy or combined treatment in the management of adult neck pain—A systematic review and meta-analysis. Musculoskelet Sci. Pract. 2017, 31, 62–71. [Google Scholar] [CrossRef]
- Rodríguez-Sanz, J.; Malo-Urriés, M.; Corral-de-Toro, J.; López-de-Celis, C.; Lucha-López, M.O.; Tricás-Moreno, J.M.; Lorente, A.I.; Hidalgo-García, C. Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 6601. [Google Scholar] [CrossRef] [PubMed]
- Cherkin, D.C.; Sherman, K.J.; Kahn, J.; Erro, J.H.; Deyo, R.A.; Haneuse, S.J.; Cook, A.J. Effectiveness of focused structural massage and relaxation massage for chronic low back pain: Protocol for a randomized controlled trial. Trials 2009, 10, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puentedura, E.J.; Flynn, T. Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: A narrative review of the literature. Physiother. Theory Pract. 2016, 32, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Zahari, Z.; Ishak, A.; Justine, M. The Effectiveness of Patient Education in Improving Pain, Disability and Quality of Life among Older People with Low Back Pain: A Systematic Review. J. Back Musculoskelet. Rehabil. 2020, 33, 245–254. [Google Scholar] [CrossRef]
- Saracoglu, I.; Arik, M.I.; Afsar, E.; Gokpinar, H.H. The effectiveness of pain neuroscience education combined with manual therapy and home exercise for chronic low back pain: A single-blind randomized controlled trial. Physiother. Theory Pract. 2020, 38, 868–879. [Google Scholar] [CrossRef]
- Cabañero-Martínez, M.J.; Cabrero-García, J.; Richart-Martínez, M.; Muñoz-Mendoza, C.L. The Spanish versions of the Barthel index (BI) and the Katz index (KI) of activities of daily living (ADL): A structured review. Arch. Gerontol. Geriatr. 2009, 49, e77–e84. [Google Scholar] [CrossRef]
- López-García, E.; Banegas, J.R.; Pérez-Regadera, A.G.; Gutiérrez-Fisac, J.L.; Alonso, J.; Rodríguez-Artalejo, F. Valores de referencia de la versión española del Cuestionario de Salud SF-36 en población adulta de más de 60 años. Med. Clin. 2003, 120, 568–573. [Google Scholar] [CrossRef]
- Díaz-Arribas, M.J.; Fernández-Serrano, M.; Royuela, A.; Kovacs, F.M.; Gallego-Izquierdo, T.; Ramos-Sánchez, M.; Llorca-Palomera, R.; Pardo-Hervás, P.; Martín-Pariente, O.S. Minimal Clinically Important Difference in Quality of Life for Patients with Low Back Pain. Spine 2017, 42, 1908–1916. [Google Scholar] [CrossRef]
- Samsa, G.; Edelman, D.; Rothman, M.L.; Williams, G.R.; Lipscomb, J.; Matchar, D. Determining clinically important differences in health status measures: A general approach with illustration to the Health Utilities Index Mark II. Pharmacoecon 1999, 15, 141–155. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Abraira, V.; Royuela, A.; Corcoll, J.; Alegre, L.; Cano, A.; Muriel, A.; Zamora, J.; Gil del Real, M.T.; Gestoso, M.; et al. Minimal Clinically Important Change for Pain Intensity and Disability in Patients with Nonspecific Low Back Pain. Spine 2007, 32, 2915–2920. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Abraira, V.; Royuela, A.; Corcoll, J.; Alegre, L.; Tomás, M.; Mir, M.A.; Cano, A.; Muriel, A.; Zamora, J.; et al. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet. Disord. 2008, 9, 43. [Google Scholar] [CrossRef] [Green Version]
- Alcock, L.; O’Brien, T.D.; Vanicek, N. Age-related changes in physical functioning: Correlates between objective and self-reported outcomes. Physiotherapy 2015, 101, 204–213. [Google Scholar] [CrossRef] [Green Version]
- Silva, A.F.; Cancela, J.M.; Mollinedo, I.; Camões, M.; Bezerra, P. The Relationship between Health Perception and Health Predictors among the Elderly across European Countries. Int. J. Environ. Res. Public Health 2021, 18, 4053. [Google Scholar] [CrossRef]
- Payne, M.E.; Porter Starr, K.N.; Orenduff, M.; Mulder, H.S.; McDonald, S.R.; Spira, A.P.; Pieper, C.F.; Bales, C.W. Quality of Life and Mental Health in Older Adults with Obesity and Frailty: Associations with a Weight Loss Intervention. J. Nutr. Health Aging 2018, 22, 1259–1265. [Google Scholar] [CrossRef]
- Jordan, J.L.; Holden, M.A.; Mason, E.E.J.; Foster, N.E. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst. Rev. 2010, 2010, CD005956. [Google Scholar] [CrossRef]
- Aitken, D.; Buchbinder, R.; Jones, G.; Winzenberg, T. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Aust. Fam. Physician 2015, 44, 39–42. [Google Scholar]
- Söderlund, A.; von Heideken Wågert, P. Adherence to and the Maintenance of Self-Management Behaviour in Older People with Musculoskeletal Pain—A Scoping Review and Theoretical Models. J. Clin. Med. 2021, 10, 303. [Google Scholar] [CrossRef]

| Week | Activities | Duration |
|---|---|---|
| 1–5 | Individualized Physical Therapy Intervention:
| 60′ |
| Therapeutic Education Program group session: Conferences about being physically active and therapeutic exercise routines; pain neuroscience education; measures to improve health status and quality of life; postural hygiene; and preventive measures on risk of falls [24,25]. | 30′ | |
| Home-based program: Individualized therapeutic exercise 4 days a week | 30′ | |
| 6–12 | Home-based program: Individualized therapeutic exercise 4 days a week | 30′ |
| Week | Activities | Duration |
|---|---|---|
| 1–3 | Standardized Physical Therapy Intervention:
| 60′ |
| Therapeutic Education Program group session: Conferences about being physically active and Therapeutic Exercise routines; pain neuroscience education; measures to improve health status and quality of life; postural hygiene; and preventive measures on risk of falls [24,25]. | 30′ | |
| Home based program: Standardized Therapeutic Exercise 4 days a week | 30′ | |
| 4–12 | Home based program: Standardized Therapeutic Exercise 4 days a week | 30′ |
| Geriatric Physical Therapy Group (n = 70) | Standardized Therapeutic Exercise Group (n = 140) | p-Value | |
|---|---|---|---|
| Age | 65.87 ± 4.37 | 66.31 ± 5.66 | 0.54 * |
| Height (m) | 1.62 ± 7.62 | 1.64 ± 7.67 | 0.07 * |
| Weight (kg) | 73.56 ± 13.38 | 72.91 ± 12.05 | 0.72 * |
| Sex (%) | 0.61 ** | ||
| Women | 62.9 | 66.4 | |
| Men | 37.1 | 33.6 | |
| Marital Status (%) | 0.91 ** | ||
| Single | 7.1 | 5 | |
| Married | 75.7 | 79.3 | |
| Widow | 14.3 | 12.9 | |
| Divorced | 2.9 | 2.9 | |
| Work Status (%) | <0.01 ** | ||
| Retired | 62.9 | 46.4 | |
| Active | 12.9 | 32.9 | |
| Housewife | 24.3 | 20.7 | |
| Body mass index (%) | 0.76 ** | ||
| Underweight | 5.7 | 7.9 | |
| Normal range | 41.4 | 45.7 | |
| Overweight | 25.7 | 25 | |
| Obesity | 5.7 | 21 | |
| Health-Related Quality of Life (SF-36v2) | |||
| Physical Function | 83.26 ± 15.79 | 78.81 ± 18.60 | 0.09 * |
| Physical Role | 86.91 ± 19.30 | 81.17 ± 17.67 | <0.01 *** |
| Bodily Pain | 63.12 ± 24.53 | 60.76 ± 21.15 | 0.47 * |
| General Health | 69.89 ± 18.77 | 63.19 ± 18.52 | 0.01 * |
| Vitality | 71.70 ± 17.64 | 65.80 ± 18.42 | 0.03 * |
| Social Function | 91.61 ± 16.71 | 88.15 ± 18.92 | 0.19 * |
| Emotional Role | 90.95 ± 19.74 | 93.58 ± 13.79 | 0.26 * |
| Mental Health | 78.93 ± 18.53 | 77.71 ± 17.07 | 0.64 * |
| PCS | 48.69 ± 8.38 | 45.88 ± 7.54 | 0.02 *** |
| MCS | 54.34 ± 9.39 | 54.31 ± 8.85 | 0.98 * |
| Musculoskeletal Pain (Visual Analogue Scale) | |||
| Non-specific neck pain | 5.57 ± 2.09 | 4.65 ± 2.16 | 0.05 * |
| Non-specific low back pain | 5.74 ± 2.21 | 5.25 ± 1.84 | 0.28 * |
| Geriatric Physical Therapy Group (n = 70) | Baseline (A0) | Intermediate (A1) | Final (A2) | p-Value * | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Health-Related Quality of Life (SF-36v2) | |||||||
| Physical Function | 83.26 | 15.79 | 85.43 | 13.09 | 85.64 | 13.93 | 0.07 |
| Physical Role | 86.91 | 19.30 | 89.56 | 16.26 | 87.06 | 18.41 | 0.11 |
| Bodily Pain | 63.12 | 24.53 | 68.64 | 21.00 | 68.21 | 23.77 | 0.02 |
| General Health | 69.89 | 18.77 | 72.14 | 17.43 | 68.52 | 17.84 | 0.09 |
| Vitality | 71.70 | 17.64 | 73.85 | 17.88 | 72.42 | 20.43 | 0.19 |
| Social Function | 91.61 | 16.71 | 95.00 | 12.66 | 93.57 | 13.91 | 0.18 |
| Emotional Role | 90.95 | 19.74 | 93.93 | 15.14 | 91.55 | 18.08 | 0.39 |
| Mental Health | 78.93 | 18.53 | 82.64 | 15.31 | 81.07 | 17.60 | 0.34 |
| PCS | 48.69 | 8.38 | 49.65 | 7.19 | 49.39 | 8.11 | 0.37 |
| MCS | 54.34 | 9.39 | 56.32 | 7.34 | 54.94 | 9.74 | 0.71 |
| Musculoskeletal Pain (Visual Analogue Scale) | |||||||
| Non-specific neck pain | 5.57 | 2.09 | 3.22 | 2.04 | 3.51 | 2.12 | <0.01 |
| Non-specific low back pain | 5.74 | 2.21 | 3.74 | 2.24 | 3.74 | 2.22 | <0.01 |
| Standardized Therapeutic Exercise Group (n = 140) | Baseline (A0) | Intermediate (A1) | Final (A2) | p-Value * | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Health-Related Quality of Life (SF-36v2) | |||||||
| Physical Function | 78.81 | 18.60 | 80.75 | 16.71 | 80.70 | 16.94 | <0.01 |
| Physical Role | 81.17 | 17.67 | 84.25 | 14.90 | 83.80 | 15.64 | <0.01 |
| Bodily Pain | 60.76 | 21.15 | 66.58 | 19.51 | 67.80 | 21.37 | <0.01 |
| General Health | 63.19 | 18.52 | 64.44 | 18.55 | 63.71 | 18.02 | 0.01 |
| Vitality | 65.80 | 18.42 | 69.37 | 16.53 | 69.33 | 17.18 | <0.01 |
| Social Function | 88.15 | 18.92 | 90.11 | 17.38 | 89.31 | 17.89 | 0.01 |
| Emotional Role | 93.58 | 13.79 | 94.11 | 12.26 | 93.34 | 13.42 | 0.34 |
| Mental Health | 77.71 | 17.07 | 79.82 | 16.87 | 80.25 | 17.79 | <0.01 |
| PCS | 45.88 | 7.54 | 47.32 | 6.76 | 47.34 | 6.91 | <0.01 |
| MCS | 54.31 | 8.85 | 55.06 | 8.16 | 54.91 | 8.44 | 0.03 |
| Musculoskeletal Pain (Visual Analogue Scale) | |||||||
| Non-specific neck pain | 4.65 | 2.16 | 3.24 | 2.18 | 3.15 | 2.09 | <0.01 |
| Non-specific low back pain | 5.25 | 1.84 | 3.75 | 2.12 | 3.57 | 2.05 | <0.01 |
| GPTG (n = 66) % | STEG (n = 120) % | p-Value | OR | IC | |
|---|---|---|---|---|---|
| Health-Related Quality of Life (SF-36v2) | |||||
| Physical Component Summary | 24.6 | 32.5 | 0.26 | 0.68 | 0.34; 1.24 |
| Mental Component Summary | 27.7 | 20.8 | 0.29 | 1.45 | 0.72; 2.93 |
| Musculoskeletal Pain (Visual Analogue Scale) | |||||
| Non-specific neck pain | 34.8 | 19.2 | 0.02 | 2.25 | 1.14; 4.45 |
| Non-specific low back pain | 30.3 | 27.5 | 0.68 | 1.14 | 0.59; 2.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pacheco-da-Costa, S.; Soto-Vidal, C.; Calvo-Fuente, V.; Yuste-Sánchez, M.J.; Sánchez-Sánchez, B.; Asúnsolo-del-Barco, Á. Evaluation of Physical Therapy Interventions for Improving Musculoskeletal Pain and Quality of Life in Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 7038. https://doi.org/10.3390/ijerph19127038
Pacheco-da-Costa S, Soto-Vidal C, Calvo-Fuente V, Yuste-Sánchez MJ, Sánchez-Sánchez B, Asúnsolo-del-Barco Á. Evaluation of Physical Therapy Interventions for Improving Musculoskeletal Pain and Quality of Life in Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(12):7038. https://doi.org/10.3390/ijerph19127038
Chicago/Turabian StylePacheco-da-Costa, Soraya, Concepción Soto-Vidal, Victoria Calvo-Fuente, María José Yuste-Sánchez, Beatriz Sánchez-Sánchez, and Ángel Asúnsolo-del-Barco. 2022. "Evaluation of Physical Therapy Interventions for Improving Musculoskeletal Pain and Quality of Life in Older Adults" International Journal of Environmental Research and Public Health 19, no. 12: 7038. https://doi.org/10.3390/ijerph19127038
APA StylePacheco-da-Costa, S., Soto-Vidal, C., Calvo-Fuente, V., Yuste-Sánchez, M. J., Sánchez-Sánchez, B., & Asúnsolo-del-Barco, Á. (2022). Evaluation of Physical Therapy Interventions for Improving Musculoskeletal Pain and Quality of Life in Older Adults. International Journal of Environmental Research and Public Health, 19(12), 7038. https://doi.org/10.3390/ijerph19127038






