Does Parental Reflective Functioning Mediate the Associations between the Maternal Antenatal and Postnatal Bond with the Child in a Community Sample?
Abstract
:1. Introduction
1.1. Background
1.2. Purpose of This Study
2. Materials and Methods
2.1. Study Design, Sampling, and Setting
2.2. Participants
2.3. Measures
2.3.1. Demographic and Mental Health Form
2.3.2. Edinburgh Postnatal Depression Scale (EPDS)
2.3.3. State and Trait Anxiety Inventory (STAI-Y)
2.3.4. Maternal Antenatal Attachment Scale (MAAS)
2.3.5. Parental Reflective Functioning Questionnaire (PRFQ)
2.3.6. Maternal Postnatal Attachment Scale (MPAS)
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics for Demographic and Mental Health Information
3.2. Descriptive Statistics and Spearman Correlations for the Main Studied Variables
3.3. Hierarchical Regression Models with MAAS Subscales as Predictors of MPAS
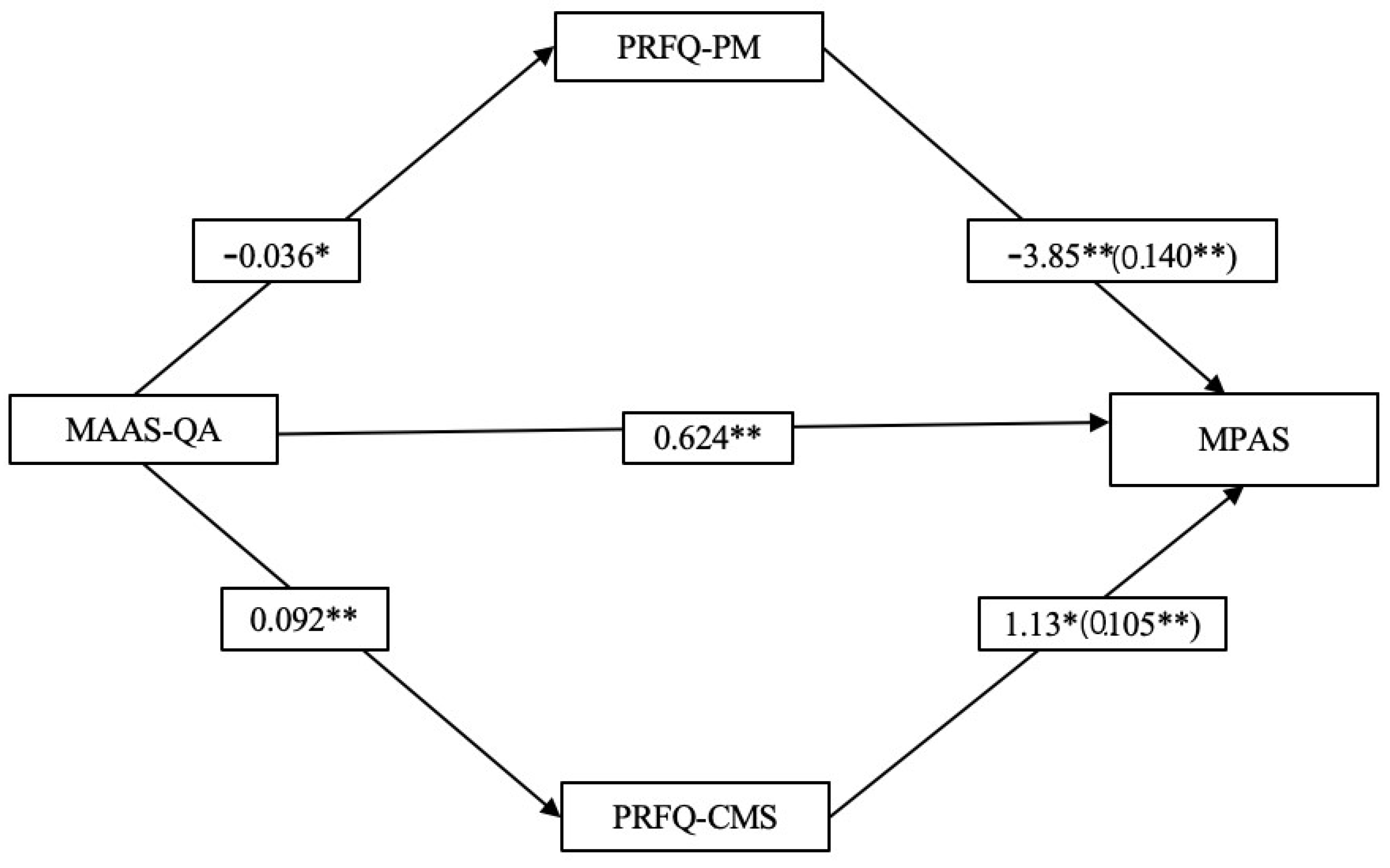
3.4. Mediation Analyses: PRF as Mediator
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Branjerdporn, G.; Meredith, P.; Strong, J.; Garcia, J. Associations between maternal-foetal attachment and infant developmental outcomes: A systematic review. Matern. Child Health J. 2017, 21, 540–553. [Google Scholar] [CrossRef]
- Tichelman, E.; Westerneng, M.; Witteveen, A.B.; van Baar, A.L.; van der Horst, H.E.; de Jonge, A.; Berger, M.Y.; Schellevis, F.G.; Burger, H.; Peters, L.L. Correlates of prenatal and postnatal mother-to-infant bonding quality: A systematic review. PLoS ONE 2019, 14, e0222998. [Google Scholar] [CrossRef] [Green Version]
- Van den Bergh, B.R.H.; Simons, A.M.T. A review of scales to measure the mother-foetus relationship. J. Reprod. Infant Psychol. 2009, 27, 114–126. [Google Scholar] [CrossRef]
- Walsh, J.; Hepper, E.G.; Bahhe, S.R.; Wadephul, F.; Jomeen, J. Maternal-fetal relationships and psychological health: Emerging research directions. J. Reprod. Infant Psychol. 2013, 31, 490–499. [Google Scholar] [CrossRef]
- Cannella, B.L. Maternal-fetal attachment: An integrative review. J. Adv. Nurs. 2005, 50, 60–68. [Google Scholar] [CrossRef]
- Göbel, A.; Stuhrmann, L.Y.; Harder, S.; Schulte-Markwort, M.; Mudra, S. The association between maternal-fetal bonding and prenatal anxiety: An explanatory analysis and systematic review. J. Affect. Disord. 2018, 239, 313–327. [Google Scholar] [CrossRef]
- Ertmann, R.K.; Bang, C.W.; Kriegbaum, M.; Væver, M.S.; Kragstrup, J.; Siersma, V.; Wilson, P.; Lutterodt, M.C.; Smith-Nielsen, J. What factors are most important for the development of the maternal-fetal relationship? A prospective study among pregnant women in Danish general practice. BMC Psychol. 2021, 9, 2. [Google Scholar] [CrossRef]
- Yarcheski, A.; Mahon, N.E.; Yarcheski, T.J.; Hanks, M.M.; Cannella, B.L. A meta-analytic study of predictors of maternal-fetal attachment. Int. J. Nurs. Stud. 2009, 46, 708–715. [Google Scholar] [CrossRef]
- Dipietro, J.A. Psychological and psychophysiological considerations regarding the maternal-fetal relationship. Infant Child Dev. 2010, 19, 27–38. [Google Scholar] [CrossRef] [Green Version]
- Deutsch, H. The Psychology of Women. Vol. 2. Motherhood; Grune & Stratton: New York, NY, USA, 1945. [Google Scholar]
- Winnicott, D.W. Primary maternal preoccupation. In Through Paediatrics to PsychoAnalysis; Winnicott, D.W., Ed.; Basic Books, Inc.: New York, NY, USA; pp. 300–306.
- Cohen, L.J.; Slade, A. The psychology and psychopathology of pregnancy: Reorganization and transformation. In Handbook of Infant Mental Health; Zeanah, C.H., Ed.; Guilford Press: New York, NY, USA, 2000; pp. 22–39. [Google Scholar]
- Zeanah, C.H.; Zeanah, P.D.; Stewart, L.K. Parents’ constructions of their infants’ personalities before and after birth: A descriptive study. Child Psychiatry Hum. Dev. 1990, 20, 191–206. [Google Scholar] [CrossRef]
- Dayton, C.J.; Levendosky, A.A.; Davidson, W.S.; Bogat, G.A. The child as held in the mind of the mother: The influence of prenatal maternal representations on parenting behaviors. Infant Ment. Health J. 2010, 31, 220–241. [Google Scholar] [CrossRef] [Green Version]
- McNamara, J.; Townsend, M.L.; Herbert, J.S. A systemic review of maternal wellbeing and its relationship with maternal fetal attachment and early postpartum bonding. PLoS ONE 2019, 14, e0220032. [Google Scholar] [CrossRef]
- Wittkowski, A.; Vatter, S.; Muhinyi, A.; Garrett, C.; Henderson, M. Measuring bonding or attachment in the parent-infant-relationship: A systematic review of parent-report assessment measures, their psychometric properties and clinical utility. Clin. Psychol. Rev. 2020, 82, 101906. [Google Scholar] [CrossRef]
- Trombetta, T.; Giordano, M.; Santoniccolo, F.; Vismara, L.; Della Vedova, A.M.; Rollè, L. Pre-natal Attachment and Parent-To-Infant Attachment: A Systematic Review. Front. Psychol. 2021, 12, 620942. [Google Scholar] [CrossRef]
- Alismail, F.; Stacks, A.M.; Wong, K.; Brown, S.; Beeghly, M.; Thomason, M. Maternal caregiving representations of the infant in the first year of life: Associations with prenatal and concurrent reflective functioning. Infant Ment. Health J. 2021, 43, 311–327. [Google Scholar] [CrossRef]
- Alvarez-Monjarás, M.; McMahon, T.J.; Suchman, N.E. Does maternal reflective functioning mediate associations between representations of caregiving with maternal sensitivity in a high-risk sample? Psychoanal. Psychol. 2019, 36, 82–92. [Google Scholar] [CrossRef]
- Walsh, J. Definitions matter: If maternal-fetal relationships are not attachment, what are they? Arch. Women’s Ment. Health 2010, 13, 449–451. [Google Scholar] [CrossRef]
- Solomon, J.; George, C. Defining the caregiving system: Towards a theory of caregiving. Infant Ment. Health J. 1996, 17, 183–197. [Google Scholar] [CrossRef]
- Condon, J.T. The assessment of antenatal emotional attachment: Development of a questionnaire instrument. Br. J. Med. Psychol. 1993, 66, 167–183. [Google Scholar] [CrossRef]
- Condon, J.T.; Corkindale, C.J. The Assessment of Parent-to-Infant Attachment: Development of a self-report questionnaire instrument. J. Reprod. Infant Psychol. 1998, 16, 57–77. [Google Scholar] [CrossRef]
- Condon, J.; Corkindale, C. The correlates of antenatal attachment in pregnant women. Br. J. Med. Psychol. 1997, 70, 359–372. [Google Scholar] [CrossRef]
- Tully, K.P.; Stuebe, A.M.; Berbiest, S.B. The 4th trimester: A critical transition period with unmet maternal health needs. Am. J. Obstet. Gynecol. 2017, 217, 37–41. [Google Scholar] [CrossRef]
- Barone, L.; Lionetti, F.; Dellagiulia, A. Maternal-fetal attachment and its correlates in a sample of Italian women: A study using the Prenatal Attachment Inventory. J. Reprod. Infant Psychol. 2014, 32, 230–239. [Google Scholar] [CrossRef]
- Della Vedova, A.M.; Dabrassi, F.; Imbasciati, A. Assessing prenatal attachment in a sample of Italian women. J. Reprod. Infant Psychol. 2008, 26, 86–98. [Google Scholar] [CrossRef]
- De Cock, E.S.A.; Henrichs, J.; Vreeswijk, C.M.J.M.; Maas, A.J.B.M.; Rijk, C.H.A.M.; van Bakel, H.J.A. Continuous feelings of love? The parental bond from pregnancy to toddlerhood. J. Family Psychol. 2016, 30, 125–134. [Google Scholar] [CrossRef]
- Fijałkowska, D.; Bielawska-Batorowicz, E. A longitudinal study of parental attachment: Pre- and post-natal study with couples. J. Reprod. Infant Psychol. 2019, 38, 509–522. [Google Scholar] [CrossRef]
- Le Bas, G.A.; Youssef, G.J.; Macdonald, J.A.; Mattick, R.; Teague, S.J.; Honan, I.; McIntosh, J.E.; Khor, S.; Rossen, L.; Elliott, E.J.; et al. Maternal bonding, negative affect, and infant social-emotional development: A prospective cohort study. J. Affect. Disord. 2021, 281, 926–934. [Google Scholar] [CrossRef]
- Luz, R.; George, A.; Vieux, R.; Spitz, E. Antenatal determinants of parental attachment and parenting alliance: How do mothers and fathers differ? Infant Ment. Health J. 2017, 38, 183–197. [Google Scholar] [CrossRef]
- Petri, E.; Palagini, L.; Bacci, O.; Borri, C.; Teristi, V.; Corezzi, C.; Faraoni, S.; Antonelli, P.; Cargioli, C.; Banti, S.; et al. Maternal–foetal attachment independently predicts the quality of maternal–infant bonding and post-partum psychopathology. J. Mat. Fetal. Neonatal. Med. 2018, 31, 3153–3159. [Google Scholar] [CrossRef]
- Rossen, L.; Hutchinson, D.; Wilson, J.; Burns, L.; Olsson, C.; Allsop, S.; Elliott, E.; Jacobs, S.; Macdonald, J.A.; Mattick, R. Predictors of post-natal mother-infant bonding: The role of antenatal bonding, maternal substance use and mental health. Arch. Women’s Ment. Health 2016, 19, 609–622. [Google Scholar] [CrossRef]
- Rossen, L.; Hutchinson, D.; Wilson, J.; Burns, L.; Allsop, S.; Elliott, E.; Jacobs, S.; Macdonald, J.A.; Olsson, C.; Mattick, R. Maternal bonding through pregnancy and post-natal: Findings from an australian longitudinal study. Am. J. Perinatol. 2017, 34, 808–817. [Google Scholar] [CrossRef]
- Slade, A.; Grienenberger, J.; Bernbach, E.; Levy, D.; Locker, A. Maternal reflective functioning, attachment, and the transmission gap: A preliminary study. Attach. Hum. Dev. 2005, 7, 283–298. [Google Scholar] [CrossRef]
- Luyten, P.; Mayes, L.C.; Nijssens, L.; Fonagy, P. The parental reflective functioning questionnaire: Development and preliminary validation. PLoS ONE 2017, 12, e0176218. [Google Scholar] [CrossRef] [Green Version]
- Slade, A. Parental reflective functioning: An introduction. Attach. Hum. Dev. 2005, 7, 269–281. [Google Scholar] [CrossRef]
- Grienenberger, J.; Kelly, K.; Slade, A. Maternal reflective functioning, mother-infant affective communication, and infant attachment: Exploring the link between mental states and observed caregiving behavior in the intergenerational transmission of attachment. Attach. Hum. Dev. 2005, 7, 299–311. [Google Scholar] [CrossRef]
- Rostad, W.L.; Whitaker, D.J. The association between reflective functioning and parent–child relationship quality. J. Child Fam. Stud. 2016, 25, 2164. [Google Scholar] [CrossRef]
- De Roo, M.; Wong, G.; Rempel, G.R.; Fraser, S.N. Advancing Optimal Development in Children: Examining the Construct Validity of a Parent Reflective Functioning Questionnaire. JMIR Pediatr. Parent. 2019, 2, e11561. [Google Scholar] [CrossRef] [Green Version]
- Waldman-Levi, A.; Finzi-Dottan, R.; Cope, A. Mother-child Joint Play: The Role of Maternal Caregiving and Reflective Function. J. Child. Fam. Stud. 2020, 29, 94–104. [Google Scholar] [CrossRef]
- Røhder, K.; Væver, M.S.; Aarestrup, A.K.; Jacobsen, R.K.; Smith-Nielsen, J.; Schiøtz, M.L. Maternal-fetal bonding among pregnant women at psychosocial risk: The roles of adult attachment style, prenatal parental reflective functioning, and depressive symptoms. PLoS ONE 2020, 15, e0239208. [Google Scholar] [CrossRef]
- Høifødt, R.S.; Nordahl, D.; Landsem, I.P.; Csifcsák, G.; Bohne, A.; Pfuhl, G.; Rognmo, K.; Braarud, H.C.; Goksøyr, A.; Moe, V.; et al. Newborn Behavioral Observation, maternal stress, depressive symptoms and the mother-infant relationship: Results from the Northern Babies Longitudinal Study (NorBaby). BMC Psychiatry 2020, 20, 300. [Google Scholar] [CrossRef]
- Camarneiro, A.P.F.; Justo, J.M.R.d.M. Prenatal attachment and sociodemographic and clinical factors in Portuguese couples. J. Reprod. Infant Psychol. 2017, 35, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.; Hagglof, B.; Eisemann, M. An exploration of prenatal attachment in Swedish expectant mothers. J. Reprod. Infant Psychol. 1999, 17, 369–380. [Google Scholar] [CrossRef]
- Muller, M.E. Development of the Prenatal Attachment Inventory. West. J. Nurs. Res. 1993, 15, 199–215. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Enders, C.K. Using the Expectation Maximization Algorithm to Estimate Coefficient Alpha for Scales with Item-Level Missing Data. Psychol. Methods 2003, 8, 322–337. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychological Association. Ethical Principles of Psychologists and Code of Conduct, 2017 (2002, Amended Effective 1 June 2010, and 1 January 2017). Available online: http://www.apa.org/ethics/code/index.html (accessed on 1 March 2022).
- Van de Vijver, F.; Hambleton, R.K. Translating tests: Some practical guidelines. Eur. Psychol. 1996, 1, 89–99. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Benvenuti, P.; Ferrara, M.; Niccolai, C.; Valoriani, V.; Cox, J.L. The Edinburgh Postnatal Depression Scale: Validation for an Italian sample. J. Affect. Disord. 1999, 53, 137–141. [Google Scholar] [CrossRef]
- Griethuijsen, R.A.L.F.; Eijck, M.W.; Haste, H.; Brok, P.J.; Skinner, N.C.; Mansour, N.; Gencer, A.S.; Boujaoude, S. Global patterns in students’ views of science and interest in science. Res. Sci. Educ. 2014, 45, 581–603. [Google Scholar] [CrossRef]
- Spielberger, C.D. State-Trait Anxiety Inventory: Bibliography, 2nd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1989. [Google Scholar]
- Pedrabissi, L.; Santinello, M. Verifica della validità dello STAI forma y di Spielberger. Boll. Psicol. Appl. Giunti Organ. Spec. 1989, 191–192, 11–14. [Google Scholar]
- Busonera, A.; Cataudella, S.; Lampis, J.; Tommasi, M.; Zavattini, G.C. Investigating validity and reliability evidence for the maternal antenatal attachment scale in a sample of Italian women. Arch. Women’s Ment. Health 2016, 19, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Nijssens, L.; Luyten, P.; Malcorps, S.; Vliegen, N.; Mayes, L. Parental reflective functioning and theory of mind acquisition: A developmental perspective. Br. J. Dev. Psychol. 2021, 39, 584–602. [Google Scholar] [CrossRef]
- Pazzagli, C.; Delvecchio, E.; Raspa, V.; Mazzeschi, C.; Luyten, P. The Parental Reflective Functioning Questionnaire in Mothers and Fathers of School-Aged Children. J. Child Fam. Stud. 2018, 27, 80–90. [Google Scholar] [CrossRef]
- Scopesi, A.; Viterbori, P.; Sponza, S.; Zucchinetti, P. Assessing mother-to-infant attachment: The Italian adaptation of a self-report questionnaire. J. Reprod. Infant Psychol. 2004, 22, 99–109. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, Version 26; IBM Corp: Armonk, NY, USA, 2019. [Google Scholar]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef] [Green Version]
- Shrout, P.E.; Bolger, N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychol. Methods 2002, 7, 422–445. [Google Scholar] [CrossRef]
- Vahidi, E.; Ghanbari, S.; Seyed Mousavi, P.; Safari, F. Psychometric properties of the prenatal-parental reflective functioning questionnaire in Iranian mothers and fathers. Curr. Psychol. 2021, 1–9. [Google Scholar] [CrossRef]
- Álvarez, N.; Lázaro, M.H.; Gordo, L.; Elejalde, L.I.; Pampliega, A.M. Maternal mentalization and child emotion regulation: A comparison of different phases of early childhood. Infant Behav. Dev. 2022, 66, 101681. [Google Scholar] [CrossRef]
- Fonagy, P.; Target, M. Mentalization and the changing aims of child psychoanalysis. Psychoanal. Dialogues 1998, 8, 87–114. [Google Scholar] [CrossRef]
- Fonagy, P.; Gergely, G.; Target, M. The parent–infant dyad and the construction of the subjective self. J. Child Psychol. Psychiatry 2007, 48, 288–328. [Google Scholar] [CrossRef] [PubMed]
- Ordway, M.R.; Webb, D.; Sadler, L.S.; Slade, A. Parental reflective functioning: An approach to enhancing parent-child relationships in pediatric primary care. J. Pediatr. Health Care 2015, 29, 325–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luyten, P.; Nijssens, L.; Fonagy, P.; Mayes, L.C. Parental reflective functioning: Theory, research, and clinical applications. Psychoanal. Study Child 2017, 70, 174–199. [Google Scholar] [CrossRef]
- Rosenman, R.; Tennekoon, V.; Hill, L.G. Measuring bias in self-reported data. Int. J. Behav. Healthc. Res. 2011, 2, 320–332. [Google Scholar] [CrossRef]

| Demographic Variables | N | % |
|---|---|---|
| Educational level | ||
| Upper secondary school | 28 | 25.5 |
| Up to secondary school | 82 | 74.5 |
| Marital status | ||
| Married or Cohabiting | 110 | 100 |
| Duration of the romantic relationship | ||
| Less than 5 years | 29 | 26.4 |
| 5 years or more | 81 | 73.6 |
| Parenting experience | ||
| First-time mother (primiparous) | 98 | 89.1 |
| One or more previous children | 12 | 10.9 |
| Planned pregnancy | ||
| Yes | 83 | 76.1 |
| No | 27 | 23.9 |
| Mn | SD | |
| Pregnancy week | 32.44 | 3.62 |
| Mental health variables | Mn | SD |
| EPDS | 7.47 | 3.87 |
| STAI State | 37.14 | 8.49 |
| STAI Trait | 38.74 | 6.67 |
| Mn | SD | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|---|
| (1) MAAS-QA | 46.76 | 3.11 | 0.473 ** | −0.393 ** | 0.375 ** | 0.286 ** | 0.569 ** |
| (2) MAAS-IP | 25.51 | 3.62 | ---- | −0.125 | 0.160 | 0.279 ** | 0.302 ** |
| (3) PRFQ-PM | 1.50 | 0.56 | ---- | ---- | ---- | ---- | −0.485 ** |
| (4) PRFQ-CMS | 4.41 | 1.17 | ---- | ---- | ---- | ---- | 0.433 ** |
| (5) PRFQ-IC | 6.28 | 0.64 | ---- | ---- | ---- | ---- | 0.185 |
| (6) MPAS | 87.20 | 7.00 | ---- | ---- | ---- | ---- | ---- |
| Dependent Variable: MPAS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | Predictor | B (95% CI) | SE | Β | T | p | R2 | F | gdl | p |
| 1 | 0.269 | 19.287 | 2, 105 | 0.000 | ||||||
| MAAS-QA | 1.14 (0.709; 1.65) | 0.239 | 0.507 | 5.08 | 0.000 | |||||
| MAAS-IP | 0.040 (−0.256; 0.421) | 0.200 | 0.020 | 0.205 | 0.838 | |||||
| 2 | 0.282 | 6.61 | 6, 101 | 0.000 | ||||||
| MAAS-QA | 1.08 (0.601; 1.61) | 0.254 | 0.479 | 4.64 | 0.000 | |||||
| MAAS-IP | 0.078 (−0.322; 0.479) | 0.205 | 0.041 | 0.388 | 0.699 | |||||
| Age | −0.032 (−0.277; 0.244) | 0.132 | −0.020 | −0.226 | 0.822 | |||||
| Education | −1.461 (−4.41; 1.83) | 1.58 | −0.090 | −1.029 | 0.306 | |||||
| Relationship | 1.48 (−1.13; 4.16) | 1.37 | 0.091 | 1.04 | 0.301 | |||||
| Pregnancy | 0.315 (−2.07; 2.71) | 1.21 | 0.019 | 0.224 | 0.823 | |||||
| 3 | 0.359 | 6.09 | 9,98 | 0.000 | ||||||
| MAAS-QA | 0.710 (0.175; 1.29) | 0.277 | 0.315 | 2.86 | 0.005 | |||||
| MAAS-IP | 0.220 (−0.221; 0.659) | 0.220 | 0.114 | 1.10 | 0.276 | |||||
| Age | 0.016 (−0.241; 0.283) | 0.133 | 0.010 | 0.109 | 0.913 | |||||
| Education | −1.35 (−4.27; 1.52) | 1.46 | −0.083 | −0.983 | 0.328 | |||||
| Relationship | 2.30 (−0.152; 4.72) | 1.25 | 0.142 | 1.66 | 0.101 | |||||
| Pregnancy | 1.05 (−1.56; 3.64) | 1.31 | 0.064 | 0.759 | 0.450 | |||||
| EPDS | −0.079 (−0.562; 0.347) | 0.231 | −0.043 | −0.384 | 0.702 | |||||
| STAI-State | −0.014 (−0.259; 0.235) | 0.125 | −0.017 | −0.123 | 0.902 | |||||
| STAI-Trait | −0.292 (−0.520; −0.021) | 0.126 | −0.277 | −2.16 | 0.040 | |||||
| Dependent Variable: MPAS | |||||
|---|---|---|---|---|---|
| Predictor | Coeff | SE | t | p | 95% CI |
| MAAS-QA | 0.624 | 0.191 | 3.27 | 0.001 | 0.246, 1.00 |
| PRFQ-PM | −3.85 | 1.09 | −3.27 | 0.001 | −6.04, −1.67 |
| PRFQ-CMS | 1.14 | 0.554 | 2.05 | 0.043 | 0.036, 2.24 |
| Age | 0.047 | 0.134 | 0.349 | 0.728 | −0.219, 0.312 |
| Education | −1.18 | 1.25 | −0.943 | 0.348 | −3.66, 1.30 |
| Relationship | 2.18 | 1.26 | 1.73 | 0.087 | −0.324, 4.69 |
| Pregnancy | −0.935 | 1.29 | −0.725 | 0.470 | −3.49, 1.62 |
| EPDS | 0.041 | 0.188 | 0.218 | 0.828 | −0.332, 0.415 |
| STAI-State | −0.093 | 0.106 | −0.877 | 0.382 | −0.303, 0.117 |
| STAI-Trait | −0.130 | 0.127 | −1.02 | 0.309 | −0.383, 0.123 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pazzagli, C.; Buratta, L.; Cenci, G.; Coletti, E.; Giuliani, M.L.; Mazzeschi, C. Does Parental Reflective Functioning Mediate the Associations between the Maternal Antenatal and Postnatal Bond with the Child in a Community Sample? Int. J. Environ. Res. Public Health 2022, 19, 6957. https://doi.org/10.3390/ijerph19126957
Pazzagli C, Buratta L, Cenci G, Coletti E, Giuliani ML, Mazzeschi C. Does Parental Reflective Functioning Mediate the Associations between the Maternal Antenatal and Postnatal Bond with the Child in a Community Sample? International Journal of Environmental Research and Public Health. 2022; 19(12):6957. https://doi.org/10.3390/ijerph19126957
Chicago/Turabian StylePazzagli, Chiara, Livia Buratta, Giulia Cenci, Elena Coletti, Maria Luisa Giuliani, and Claudia Mazzeschi. 2022. "Does Parental Reflective Functioning Mediate the Associations between the Maternal Antenatal and Postnatal Bond with the Child in a Community Sample?" International Journal of Environmental Research and Public Health 19, no. 12: 6957. https://doi.org/10.3390/ijerph19126957
APA StylePazzagli, C., Buratta, L., Cenci, G., Coletti, E., Giuliani, M. L., & Mazzeschi, C. (2022). Does Parental Reflective Functioning Mediate the Associations between the Maternal Antenatal and Postnatal Bond with the Child in a Community Sample? International Journal of Environmental Research and Public Health, 19(12), 6957. https://doi.org/10.3390/ijerph19126957






