Relationship between Self-Perception of Aging and Quality of Life in the Different Stages of Reproductive Aging in Mexican Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Sample Size
2.3. Assessment of Self-Perception of Aging
2.4. Assessment of Quality of Life+
2.5. Data Analysis
3. Results
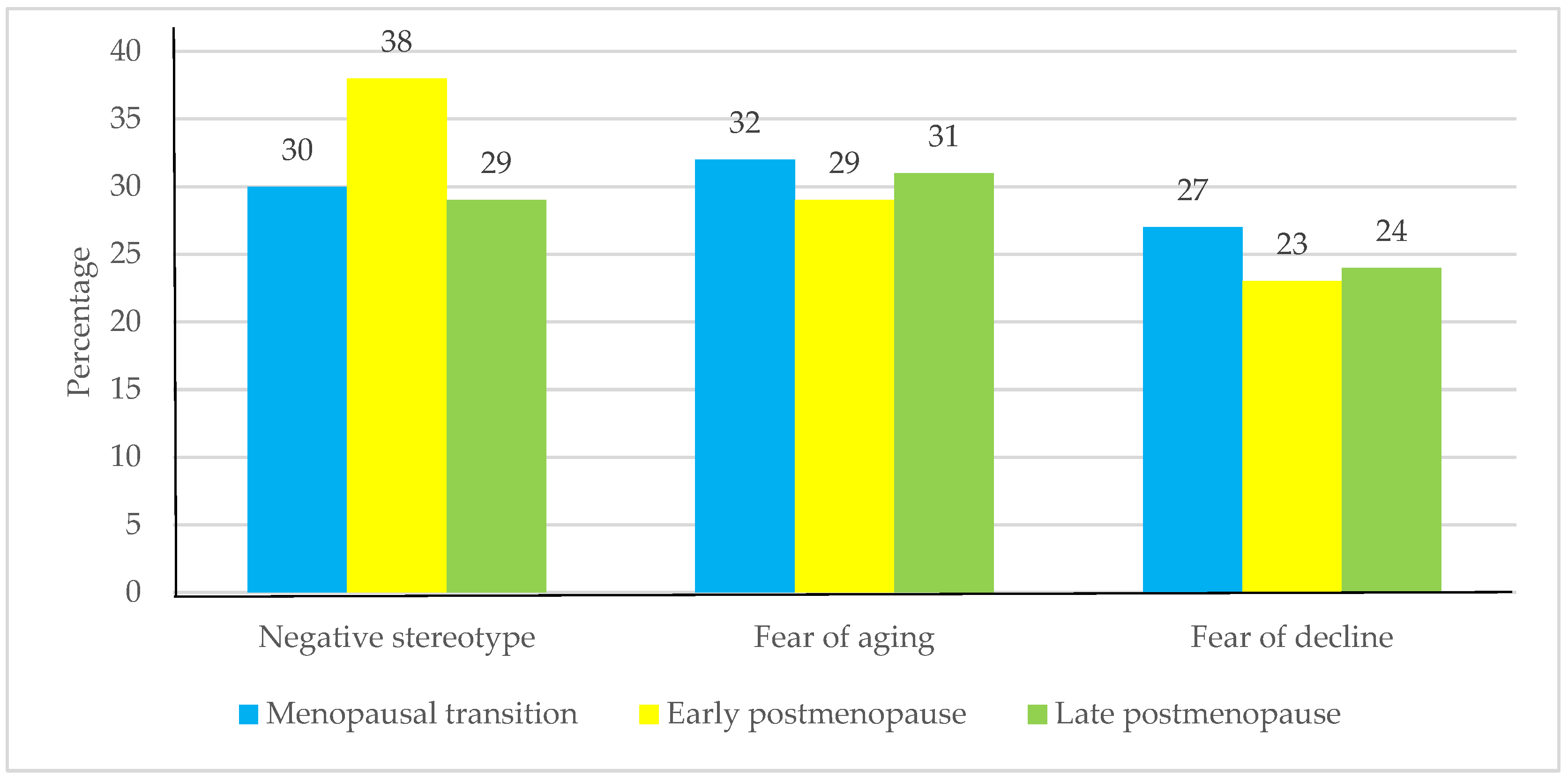
3.1. Self-Perception of Aging and Quality of Life
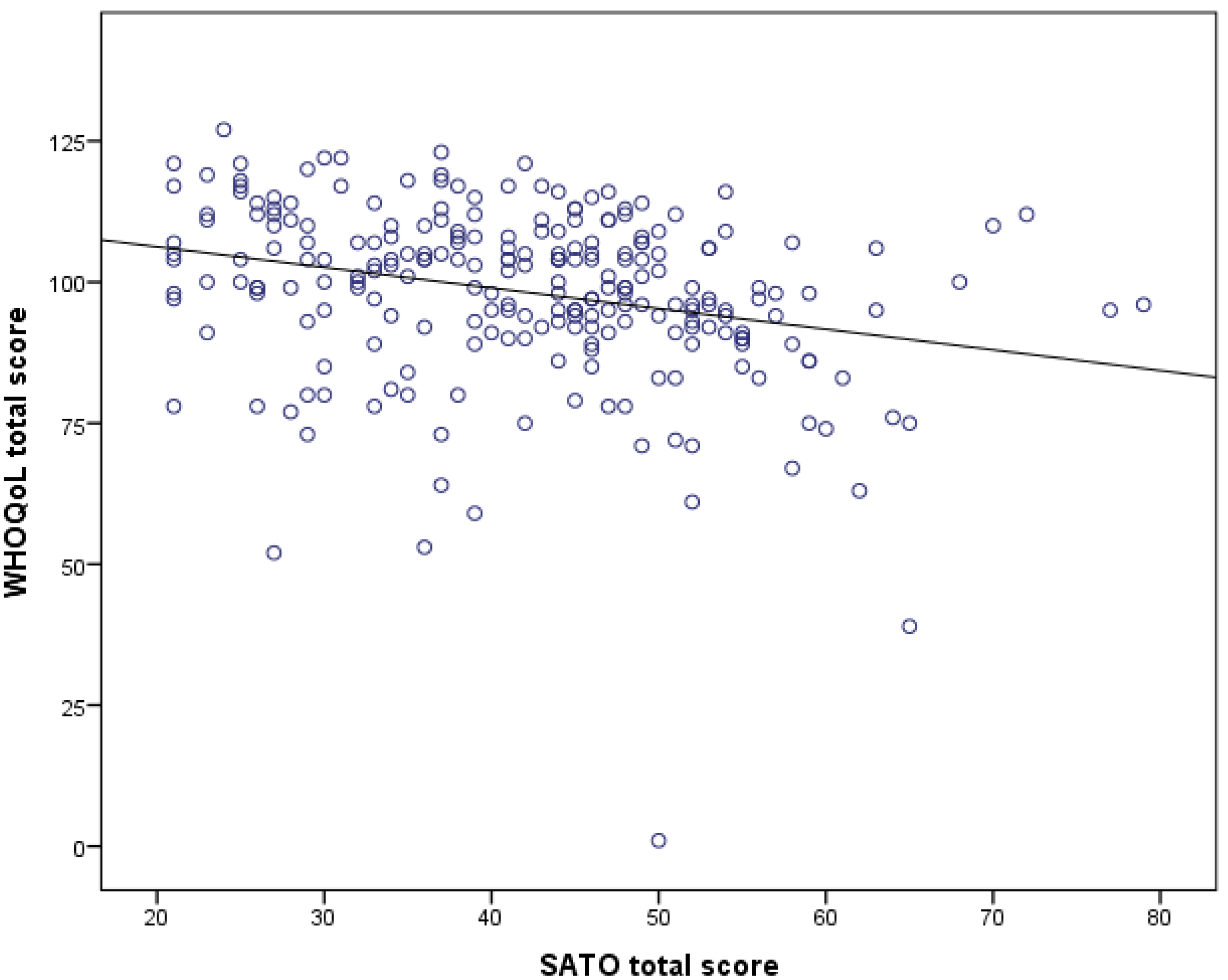
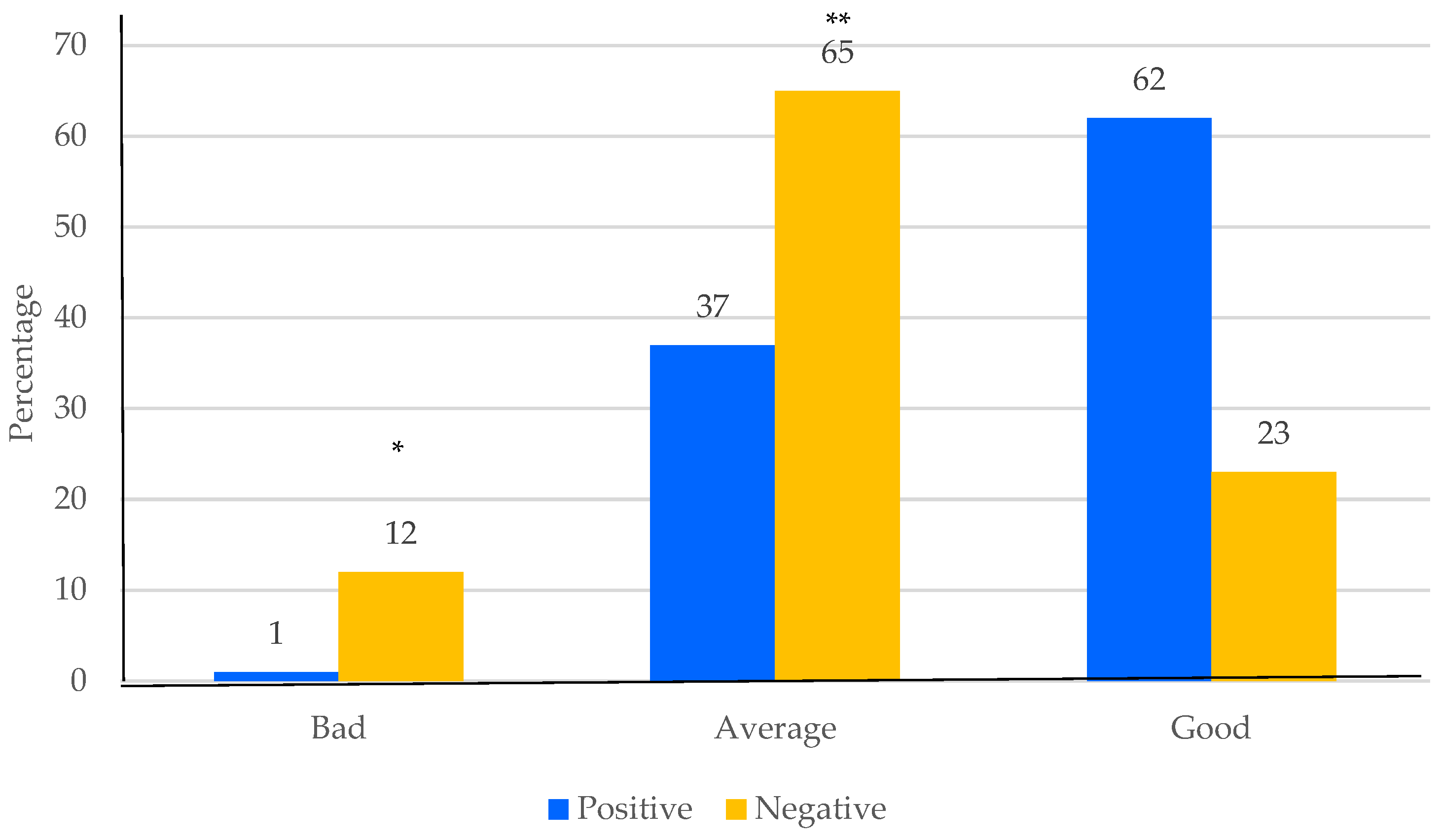
3.2. Association between Self-Perception of Aging and Quality of Life
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Broekmans, F.J.; Soules, M.R.; Fauser, B.C. Ovarian aging: Mechanisms and clinical consequences. Endocr. Rev. 2009, 30, 465–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Khoudary, S.R.; Greendale, G.; Crawford, S.L.; Avis, N.E.; Brooks, M.M.; Thurston, R.C.; Karvonen-Gutierrez, C.; Waetjen, L.E.; Matthews, K. The menopause transition and women’s health at midlife: A progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause 2019, 26, 1213–1227. [Google Scholar] [CrossRef] [PubMed]
- Masjoudi, M.; Amjadi, M.A.; Leyli, E.K.N. Severity and frequency of menopausal symptoms in middle aged women, Rasht, Iran. J. Clin. Diagn. Res. 2017, 11, QC17–QC21. [Google Scholar] [CrossRef]
- Zhao, D.; Liu, C.; Feng, X.; Hou, F.; Xu, X.; Li, P. Menopausal symptoms in different substages of perimenopause and their relationships with social support and resilience. Menopause 2019, 26, 233–239. [Google Scholar] [CrossRef]
- Hernández-Valencia, M.; Córdova-Pérez, N.; Basurto, L.; Saucedo, R.; Vargas, C.; Vargas, A.; Ruiz, M.; Manuel, L.; Zárate, A. Frecuencia de los síntomas del síndrome climatérico. Ginecol. Obstetr. Mex. 2010, 78, 232–237. [Google Scholar]
- Harlow, S.D.; Gass, M.; Hall, J.E.; Lobo, R.; Maki, P.; Rebar, R.W.; Sherman, S.; Sluss, P.M.; de Villiers, T.J.; STRAW + 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop + 10: Addressing the unfinished agenda of staging reproductive aging. Menopause 2012, 19, 387–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bitner, D.; Wild, R. Clinical intervention to reduce central obesity and menopausal symptoms in women aged 35 to 55 years. Menopause 2014, 21, 975–981. [Google Scholar] [CrossRef]
- Rodríguez-San Nicolás, A.; Sánchez-Rodríguez, M.A.; Zacarías-Flores, M.; Correa-Muñoz, E.; Mendoza-Núñez, V.M. Relación entre la obesidad central y el estrés oxidativo en mujeres premenopáusicas versus posmenopáusicas. Nutr. Hosp. 2020, 37, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Cameron, E.; Ward, P.; Mandville-Anstey, S.A.; Coombs, A. The female aging body: A systematic review of female perspectives on aging, health, and body image. J. Women Aging 2019, 31, 3–17. [Google Scholar] [CrossRef]
- Cortés, Y.I.; Marginean, V.; Berry, D. Physiologic and psychosocial changes of the menopause transition in US Latinas: A narrative review. Climacteric 2021, 24, 214–228. [Google Scholar] [CrossRef]
- de Salis, I.; Owen-Smith, A.; Donovan, J.L.; Lawlor, D.A. Experiencing menopause in the UK: The interrelated narratives of normality, distress, and transformation. J. Women Aging. 2018, 30, 520–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Officer, A.; de la Fuente-Núñez, V. A global campaign to combat ageism. Bull. World Health Organ 2018, 96, 299–300. [Google Scholar] [CrossRef] [PubMed]
- Dolberg, P.; Ayalon, L. Subjective meanings and identification with middle age. Int. J. Aging Human Dev. 2018, 87, 52–76. [Google Scholar] [CrossRef] [PubMed]
- Palmore, E.B. The Future of Ageism; International Longevity Center: New York, NY, USA, 2004; pp. 2–5. [Google Scholar]
- Freeman, A.T.; Santini, Z.I.; Tyrovolas, S.; Rummel-Kluge, C.; Haro, J.M.; Koyanagi, A. Negative perceptions of ageing predict the onset and persistence of depression and anxiety: Findings from a prospective analysis of the Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2016, 199, 132–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gum, A.M.; Ayalon, L. Self-perceptions of aging mediate the longitudinal relationship of hopelessness and depressive symptoms. Int. J. Geriatr. Psychiatry 2018, 33, 591–597. [Google Scholar] [CrossRef]
- Xiao, L.; Yang, H.; Du, W.; Lei, H.; Wang, Z.; Shao, J. Subjective age and depressive symptoms among Chinese older adults: A moderated mediation model of perceived control and self-perceptions of aging. Psychiatry Res. 2019, 271, 114–120. [Google Scholar] [CrossRef]
- Levy, B.R.; Slade, M.D.; Murphy, T.E.; Gill, T.M. Association between positive age stereotypes and recovery from disability in older persons. JAMA 2012, 308, 1972–1973. [Google Scholar] [CrossRef] [Green Version]
- Marquet, M.; Boutaayamou, M.; Schwartz, C.; Locquet, M.; Bruyère, O.; Croisier, J.L.; Adam, S. Does negative information about aging influence older adults’ physical performance and subjective age? Arch. Gerontol. Geriatr. 2018, 78, 181–189. [Google Scholar] [CrossRef]
- Ingrand, I.; Paccalin, M.; Liuu, E.; Gil, R.; Ingrand, P. Positive perception of aging is a key predictor of quality-of-life in aging people. PLoS ONE 2018, 13, e0204044. [Google Scholar] [CrossRef]
- Hernández-Pozo, M.R.; Torres, N.M.; Coronado, A.O.; Herrera, G.A.; Castillo, N.P.; Sánchez, V.A. Actitudes negativas hacia la vejez en población mexicana: Aspectos psicométricos de una escala. In Evaluación en Psicogerontología; González-Celis, R.A.L., Ed.; Manual Moderno: Ciudad de Mexico, Mexico, 2009; pp. 1–16. [Google Scholar]
- Mendoza-Núñez, V.M.; Sarmiento-Salmorán, E.; Marín-Cortés, R.; Martínez-Maldonado, M.L.; Ruiz-Ramos, M. Influence of the self-perception of old age on the effect of a Healthy Aging Program. J. Clin. Med. 2018, 7, 106. [Google Scholar] [CrossRef] [Green Version]
- WHOQOL Group. Development of the World Health Organization WHOQOLBREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phungrassami, T.; Katikarn, R.; Watanaarepornchai, S.; Sangtawan, D. Quality of life assessment in radiotherapy patients by WHOQOL-BREF-THAI: A feasibility study. J. Med. Assoc. Thai. 2004, 87, 1459–1465. [Google Scholar] [PubMed]
- Gewirtz-Meydan, A.; Ayalon, L. Forever young: Visual representations of gender and age in online dating sites for older adults. J. Women Aging 2018, 30, 484–502. [Google Scholar] [CrossRef] [PubMed]
- Reyhani, M.; Kazemi, A.; Keshvari, M. Rise and fall: Two sides of a coin of middle aged women’s perceptions of reproductive: A qualitative study. Arch. Womens Ment. Health 2018, 21, 421–428. [Google Scholar] [CrossRef]
- Giasson, H.L.; Queen, T.L.; Larkina, M.; Smith, J. Age group differences in perceived age discrimination: Associations with self-perceptions of aging. Gerontologist 2017, 57, S160–S168. [Google Scholar] [CrossRef] [Green Version]
- Levy, B.R. Mind matters: Cognitive and physical effects of aging self-stereotypes. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, P203–P211. [Google Scholar] [CrossRef] [Green Version]
- Levy, B. Stereotype embodiment: A psychosocial approach to aging. Curr. Dir. Psychol. Sci. 2009, 18, 332–336. [Google Scholar] [CrossRef] [Green Version]
- Binfa, L.; Castelo-Branco, C.; Blümel, J.E.; Cancelo, M.J.; Bonilla, H.; Muñoz, I.; Vergara, V.; Izaguirre, H.; Sarrá, S.; Ríos, R.V. Influence of psycho-social factors on climacteric symptoms. Maturitas 2004, 48, 425–431. [Google Scholar] [CrossRef]
- Sánchez-Rodríguez, M.A.; Castrejón-Delgado, L.; Zacarías-Flores, M.; Arronte-Rosales, A.; Mendoza-Núñez, V.M. Quality of life among post-menopausal women due to oxidative stress boosted by dysthymia and anxiety. BMC Women’s Health 2017, 17, 1. [Google Scholar] [CrossRef] [Green Version]
- Barnaś, E.; Penar-Zadarko, B.; Pikuła, A. The assessment of women’s life quality during climacterium. Polish J. Environ. Stud. 2006, 15, 31–33. [Google Scholar]
- Robak-Chołubek, D.; Wdowiak, A.; Makara-Studzińska, M.; Korczyńska, E. Perception and degree of acceptance of menopause-related changes in various spheres of life by postmenopausal women. Ann. Agric. Environ. Med. 2014, 21, 666–669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karacam, Z.; Seker, S.E. Factors associated with menopausal symptoms and their relationship with the quality of life among Turkish women. Maturitas 2007, 58, 75–82. [Google Scholar] [CrossRef]
- Krawczyk-Suszek, M.; Kleinrok, A. Health-Related Quality of Life (HRQoL) of people over 65 years of age. Int. J. Environ. Res. Public Health 2022, 19, 625. [Google Scholar] [CrossRef] [PubMed]
- Abolhassani, N.; Santos-Eggimann, B.; Büla, C.; Goy, R.; Guessous, I.; Henchoz, Y. Quality of life profile in three cohorts of community-dwelling Swiss older people. BMC Geriatrics 2019, 19, 96. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, Z.M.; Ghoneim, H.M.; Madny, E.; Kishk, E.A.; Lotfy, M.; Bahaa, A.; Taha, T.; Aboelroose, A.A.; Atwa, K.A.; Abbas, A.M.; et al. The effect of menopausal symptoms on the quality of life among postmenopausal Egyptian women. Climacteric 2020, 23, 9–16. [Google Scholar] [CrossRef]
- Fallahzadeh, H. Quality of life after the menopause in Iran: A population study. Qual. Life Res. 2010, 19, 813–819. [Google Scholar] [CrossRef]
- Levy, B.R.; Slade, M.D. Positive views of aging reduce risk of developing later-life obesity. Prev. Med. Rep. 2019, 13, 196–198. [Google Scholar] [CrossRef]
- Warmoth, K.; Tarrant, M.; Abraham, C.; Lang, I.A. Older adults’ perceptions of ageing and their health and functioning: A systematic review of observational studies. Psychol. Health Med. 2016, 21, 531–550. [Google Scholar] [CrossRef]
- Moshki, M.; Mohammadzadeh, F.; Dehnoalian, A. The effectiveness of a group-based educational program on the self-efficacy and self-acceptance of menopausal women: A randomized controlled trial. J. Women Aging. 2018, 30, 310–325. [Google Scholar] [CrossRef]
- Kalfoss, M.H. Attitudes to ageing among older Norwegian adults living in the community. Br. J. Community Nurs. 2017, 22, 238–245. [Google Scholar] [CrossRef]
- Sun, T.; Zhang, S.E.; Yan, M.Y.; Lian, T.H.; Yu, Y.Q.; Yin, H.Y.; Zhao, C.X.; Wang, Y.P.; Chang, X.; Ji, K.Y.; et al. Association between self-perceived stigma and quality of life among urban Chinese older adults: The moderating role of attitude toward own aging and traditionality. Front. Public Health 2022, 10, 767255. [Google Scholar] [CrossRef] [PubMed]
- Molina-Luque, F. The art of living as a community: Profiguration, sustainability, and social development in Rapa Nui. Sustainability 2020, 12, 6798. [Google Scholar] [CrossRef]
- Molina-Luque, F.; Stončikaitė, I.; Torres-González, T.; Sanvicen-Torné, P. Profiguration, active ageing, and creativity: Keys for quality of life and overcoming ageism. Int. J. Environ. Res. Public Health 2022, 19, 1564. [Google Scholar] [CrossRef] [PubMed]
- Casamali, F.F.C.; Schuch, F.B.; Scortegagna, S.A.; Legnania, E.; De Marchi, A.C.B. Accordance and reproducibility of the electronic version of the WHOQOLBREF and WHOQOL-OLD questionnaires. Exp. Gerontol. 2019, 125, 110683. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health; WHO: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 11 June 2021).
- World Health Organization. Promising strategies. In Global Report on Ageism; WHO: Geneva, Switzerland, 2021; pp. 139–146. [Google Scholar]
| Variable | Menopausal Transition | Early Postmenopause | Late Postmenopause |
|---|---|---|---|
| (n = 93) | (n = 80) | (n = 67) | |
| Age (years) | 46 ± 4 | 53 ± 4 * | 59 ± 5 * |
| Marital status | |||
| Single | 13 (14%) | 12 (15%) | 14 (21%) |
| Married | 58 (62%) | 39 (49%) | 38 (57%) |
| Separated/divorced | 17 (18%) | 17 (21%) | 8 (12%) |
| Widow | 5 (5%) | 12 (15%) | 7 (10%) |
| Educational level | |||
| Primary school | 0 | 2 (3%) | 2 (3%) |
| Secondary school | 11 (12%) | 5 (6%) | 6 (9%) |
| High school | 31 (33%) | 32 (40%) | 19 (28%) |
| University | 51 (55%) | 41 (51%) | 40 (60%) |
| Hysterectomy | 5 (5%) † | 18 (23%) | 17 (25%) |
| Oophorectomy | 0 | 7 (9%) | 5 (8%) |
| Parameter | Menopausal Transition | Early Postmenopause | Late Postmenopause |
|---|---|---|---|
| (n = 93) | (n = 80) | (n = 67) | |
| Self-perception of aging | |||
| Total score | 42.1 ± 10.6 | 42.1 ± 11.9 | 41.6 ± 12.6 |
| Positive perception (≤44) | 51 (55%) | 44 (55%) | 39 (58%) |
| Negative perception (≥59) | 4 (4%) | 8 (10%) | 5 (8%) |
| Quality of life score | |||
| Total | 97.5 ± 14.3 | 97.7 ± 14.8 | 99.9 ± 17.9 |
| Physical subscale | 26.5 ± 4.6 | 26.7 ± 4.7 | 26.5 ± 3.8 |
| Psychological subscale | 23.1 ± 3.7 | 22.8 ± 3.8 | 24.0 ± 6.8 |
| Environment subscale | 28.5 ± 5.2 | 29.5 ± 5.3 | 30.9 ± 6.4 * |
| Social subscale | 11.7 ± 2.4 | 11.3 ± 2.4 | 12.0 ± 2.5 |
| Quality of life classification | |||
| Good (>95) | 58 (62%) | 47 (59%) | 47 (70%) |
| Average (61–95) | 33 (36%) | 31 (39%) | 19 (28%) |
| Bad (<65) | 2 (2%) | 2 (2%) | 1 (2%) |
| WHO Quality of Life | Menopausal Transition | Early Postmenopause | Late Postmenopause |
|---|---|---|---|
| Total score | −0.273 * | −0.237 † | −0.307 * |
| Physical subscale | −0.212 † | −0.121 | −0.246 † |
| Psychological subscale | −0.282 * | −0.232 † | −0.059 |
| Environment subscale | −0.226 † | −0.241 † | −0.293 * |
| Social subscale | −0.211 † | −0.263 * | −0.385 * |
| Variable | Beta | Standard Error | p-Value |
|---|---|---|---|
| SATO score | −0.31 | 0.05 | <0.0001 |
| Years of school | 0.76 | 0.21 | <0.0001 |
| Age (years) | 0.21 | 0.22 | 0.338 |
| Years after last menstrual period | −0.16 | 0.31 | 0.590 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rivera-Ochoa, F.S.; González-Herrera, I.V.; Zacarías-Flores, M.; Correa-Muñoz, E.; Mendoza-Núñez, V.M.; Sánchez-Rodríguez, M.A. Relationship between Self-Perception of Aging and Quality of Life in the Different Stages of Reproductive Aging in Mexican Women. Int. J. Environ. Res. Public Health 2022, 19, 6839. https://doi.org/10.3390/ijerph19116839
Rivera-Ochoa FS, González-Herrera IV, Zacarías-Flores M, Correa-Muñoz E, Mendoza-Núñez VM, Sánchez-Rodríguez MA. Relationship between Self-Perception of Aging and Quality of Life in the Different Stages of Reproductive Aging in Mexican Women. International Journal of Environmental Research and Public Health. 2022; 19(11):6839. https://doi.org/10.3390/ijerph19116839
Chicago/Turabian StyleRivera-Ochoa, Frida Sara, Ixel Venecia González-Herrera, Mariano Zacarías-Flores, Elsa Correa-Muñoz, Víctor Manuel Mendoza-Núñez, and Martha A. Sánchez-Rodríguez. 2022. "Relationship between Self-Perception of Aging and Quality of Life in the Different Stages of Reproductive Aging in Mexican Women" International Journal of Environmental Research and Public Health 19, no. 11: 6839. https://doi.org/10.3390/ijerph19116839
APA StyleRivera-Ochoa, F. S., González-Herrera, I. V., Zacarías-Flores, M., Correa-Muñoz, E., Mendoza-Núñez, V. M., & Sánchez-Rodríguez, M. A. (2022). Relationship between Self-Perception of Aging and Quality of Life in the Different Stages of Reproductive Aging in Mexican Women. International Journal of Environmental Research and Public Health, 19(11), 6839. https://doi.org/10.3390/ijerph19116839






