Improvement in Quality of Life through Self-Management of Mild Symptoms during the COVID-19 Pandemic: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
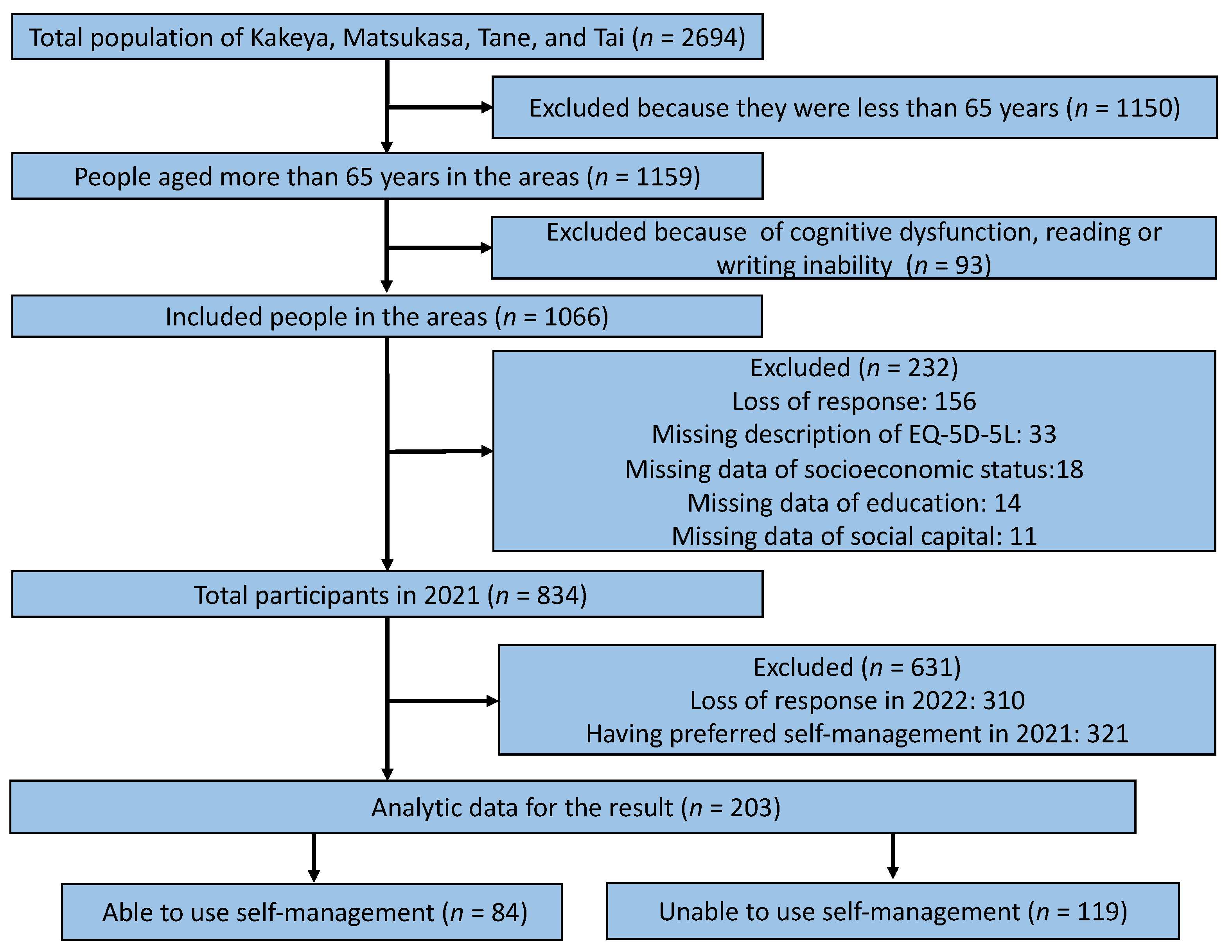
2.2. Participants
2.3. Measurements
2.3.1. Outcome Variable
2.3.2. Independent Variable
2.3.3. Covariates
2.4. Statistical Analyses
2.5. Ethical Considerations
3. Results
3.1. Demographic Data of the Participants
3.2. Change in the Single Health Status Index Scores on the EQ-5D-5L
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Begashaw, B.; Tessema, F.; Gesesew, H.A. Health care seeking behavior in Southwest Ethiopia. PLoS ONE 2016, 11, e0161014. [Google Scholar] [CrossRef]
- Andarini, S.; Arif, A.Z.; Al Rasyid, H.; Wahono, C.S.; Kalim, H.; Handono, K. Factors Associated with health care seeking behavior for musculoskeletal pain in Indonesia: A cross-sectional study. Int. J. Rheum. Dis. 2019, 22, 1297–1304. [Google Scholar] [CrossRef]
- Morikawa, M. Towards community-based integrated care: Trends and issues in Japan’s long-term care policy. Int. J. Integr. Care 2014, 14, e005. [Google Scholar] [CrossRef]
- Campbell, J.C.; Ikegami, N. Long-term care insurance comes to Japan. Health Aff. 2000, 19, 26–39. [Google Scholar] [CrossRef]
- Wereta, T.; Betemariam, W.; Karim, A.M.; Fesseha Zemichael, N.; Dagnew, S.; Wanboru, A.; Bhattacharya, A. Effects of a participatory community quality improvement strategy on improving household and provider health care behaviors and practices: A propensity score analysis. BMC Preg. Childbirth 2018, 18 (Suppl. 1), 364. [Google Scholar] [CrossRef]
- Cornally, N.; McCarthy, G. Help-seeking behaviour: A concept analysis. Int. J. Nurs. Pract. 2011, 17, 280–288. [Google Scholar] [CrossRef]
- Chi, W.C.; Wolff, J.; Greer, R.; Dy, S. Multimorbidity and decision-making preferences among older adults. Ann. Fam. Med. 2017, 15, 546–551. [Google Scholar] [CrossRef]
- Larsen, A.; Broberger, E.; Petersson, P. Complex caring needs without simple solutions: The experience of interprofessional collaboration among staff caring for older persons with multimorbidity at home care settings. Scand. J. Caring Sci. 2017, 31, 342–350. [Google Scholar] [CrossRef]
- Farquhar, J.W. Primordial prevention: The path from Victoria to Catalonia. Prev. Med. 1999, 29, S3–S8. [Google Scholar] [CrossRef]
- Sirri, L.; Fava, G.A.; Sonino, N. The unifying concept of illness behavior. Psychother. Psychosom. 2013, 82, 74–81. [Google Scholar] [CrossRef]
- Alberts, J.F.; Sanderman, R.; Gerstenbluth, I.; van den Heuvel, W.J. Sociocultural variations in help-seeking behavior for everyday symptoms and chronic disorders. Health Policy 1998, 44, 57–72. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Gomi, T.; Katsube, T. Challenges and solutions in the continuity of home care for rural older people: A thematic analysis. Home Health Care Serv. Q. 2020, 39, 126–139. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Sano, C.; Könings, K.D. Educational intervention to improve citizen’s healthcare participation perception in rural Japanese communities: A pilot study. Int. J. Environ. Res. Public Health 2021, 18, 1782. [Google Scholar] [CrossRef]
- Jørgensen, J.T.; Andersen, J.S.; Tjønneland, A.; Andersen, Z.J. Determinants of frequent attendance in Danish general practice: A cohort-based cross-sectional study. BMC Fam. Pract. 2016, 17, 9. [Google Scholar] [CrossRef]
- Kaneko, M.; Motomura, K.; Mori, H.; Ohta, R.; Matsuzawa, H.; Shimabukuro, A.; Matsushima, M. Gatekeeping function of primary care physicians under Japan’s free-access system: A prospective open cohort study involving 14 isolated islands. Fam. Pract. 2019, 36, 452–459. [Google Scholar] [CrossRef]
- Olivares-Tirado, P.; Tamiya, N.; Kashiwagi, M.; Kashiwagi, K. Predictors of the highest long-term care expenditures in Japan. BMC Health Serv. Res. 2011, 11, 103. [Google Scholar] [CrossRef]
- Ohta, R.; Ueno, A.; Sano, C. Changes in the comprehensiveness of rural medical care for older Japanese patients during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10772. [Google Scholar] [CrossRef]
- Coventry, L.L.; van Schalkwyk, J.W.; Thompson, P.L.; Hawkins, S.A.; Hegney, D.G. Myocardial infarction, patient decision delay and help-seeking behaviour: A thematic analysis. J. Clin. Nurs. 2017, 26, 1993–2005. [Google Scholar] [CrossRef]
- Zock, E.; Kerkhoff, H.; Kleyweg, R.P.; van Bavel-Ta, T.B.; Scott, S.; Kruyt, N.D.; Nederkoorn, P.J.; van de Beek, D. Help seeking behavior and onset-to-alarm time in patients with acute stroke: Sub-study of the preventive antibiotics in stroke study. BMC Neurol. 2016, 16, 241. [Google Scholar] [CrossRef]
- Ohta, R.; Sato, M.; Kitayuguchi, J.; Maeno, T.; Sano, C. Potential help-seeking behaviors associated with better self-rated health among rural older patients: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 9116. [Google Scholar] [CrossRef]
- Ohta, R.; Sato, M.; Kitayuguchi, J.; Maeno, T.; Sano, C. The association between the self-management of mild symptoms and quality of life of elderly populations in rural communities: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 8857. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kataoka, D.; Sano, C. Effectiveness and challenges in local self-governance: Multifunctional autonomy in Japan. Int. J. Environ. Res. Public Health 2021, 18, 574. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Otani, J. Rural physicians’ perceptions about the challenges of participating in interprofessional collaboration: Insights from a focus group study. J. Interprof. Educ. Pract. 2020, 20, 100345. [Google Scholar] [CrossRef]
- Matsumoto, M.; Kimura, K.; Inoue, K.; Kashima, S.; Koike, S.; Tazuma, S. Aging of hospital physicians in rural Japan: A longitudinal study based on national census data. PLoS ONE 2018, 13, e0198317. [Google Scholar] [CrossRef]
- Takamura, A.; Matsumoto, M.; Ishikawa, S. Rural health in Japan: Past and future. Rural Remote Health 2017, 17, 4521. [Google Scholar] [CrossRef][Green Version]
- Fukui, T.; Rahman, M.; Ohde, S.; Hoshino, E.; Kimura, T.; Urayama, K.Y.; Omata, F.; Deshpande, G.A.; Takahashi, O. Reassessing the ecology of medical care in Japan. J. Commun. Health 2017, 42, 935–941. [Google Scholar] [CrossRef]
- Kaneko, M.; Matsushima, M.; Irving, G. The ecology of medical care on an isolated island in Okinawa, Japan: A retrospective Open Cohort Study. BMC Health Serv. Res. 2017, 17, 37. [Google Scholar] [CrossRef]
- Shiroiwa, T.; Fukuda, T.; Ikeda, S.; Igarashi, A.; Noto, S.; Saito, S.; Shimozuma, K. Japanese Population Norms for Preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual. Life Res. 2016, 25, 707–719. [Google Scholar] [CrossRef]
- Ohta, R.; Sato, M.; Ryu, Y.; Kitayuguchi, J.; Maeno, T.; Sano, C. What resources do elderly people choose for managing their symptoms? Clarification of rural older people’s choices of help-seeking behaviors in Japan. BMC Health Serv. Res. 2021, 21, 640. [Google Scholar] [CrossRef]
- Elliott, A.M.; McAteer, A.; Hannaford, P.C. Revisiting the symptom iceberg in today’s primary care: Results from a UK population survey. BMC Fam. Pract. 2011, 12, 16. [Google Scholar] [CrossRef]
- McClure, N.S.; Sayah, F.A.; Ohinmaa, A.; Johnson, J.A. Minimally important difference of the EQ-5D-5L index score in adults with type 2 diabetes. Value Health 2018, 21, 1090–1097. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow. Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Alleaume, C.; Verger, P.; Peretti-Watel, P.; COCONEL Group. Psychological support in general population during the COVID-19 lockdown in France: Needs and access. PLoS ONE 2021, 16, e0251707. [Google Scholar] [CrossRef]
- Ranscombe, P. Rural areas at risk during COVID-19 pandemic. Lancet Infect. Dis. 2020, 20, 545. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Sano, C. Fears related to COVID-19 among rural older people in Japan. Healthcare 2021, 9, 524. [Google Scholar] [CrossRef]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef]
- Zhang, Y.; Ma, D.; Cui, R.; Haregot Hilawe, E.; Chiang, C.; Hirakawa, Y.; Hu, Y.; Wang, P.; Iso, H.; Aoyama, A. Facilitators and barriers of adopting healthy lifestyle in rural China: A qualitative analysis through social capital perspectives. Nagoya J. Med. Sci. 2016, 78, 163–173. [Google Scholar]
- Barcham, R.; Silas, E.; Irie, J. Health promotion and empowerment in Henganofi District, Papua New Guinea. Rural Remote Health 2016, 16, 3553. [Google Scholar] [CrossRef]
- Judd, F.; Jackson, H.; Komiti, A.; Murray, G.; Fraser, C.; Grieve, A.; Gomez, R. Help-seeking by rural residents for mental health problems: The importance of agrarian values. Aust. N. Z. J. Psychiatry 2006, 40, 769–776. [Google Scholar] [CrossRef]
- Zhao, Q.; Wang, J.; Nicholas, S.; Maitland, E.; Sun, J.; Jiao, C.; Xu, L.; Leng, A. Health-related 1uality of life and health service use among multimorbid middle-aged and older-aged adults in China: A cross-sectional study in Shandong Province. Int. J. Environ. Res. Public Health 2020, 17, 9261. [Google Scholar] [CrossRef]
- Lawrence-Bourne, J.; Dalton, H.; Perkins, D.; Farmer, J.; Luscombe, G.; Oelke, N.; Bagheri, N. What is rural adversity, how does it affect wellbeing and what are the implications for action? Int. J. Environ. Res. Public Health 2020, 17, 7205. [Google Scholar] [CrossRef] [PubMed]
- Vahia, V.N.; Shah, A.B. COVID-19 pandemic and mental health care of older adults in India. Int. Psychogeriatr. 2020, 32, 1125–1127. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Maiguma, K.; Yata, A.; Sano, C. A Solution for Loneliness in Rural Populations: The Effects of Osekkai Conferences during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 5054. [Google Scholar] [CrossRef] [PubMed]
- Kamada, M.; Kitayuguchi, J.; Abe, T.; Taguri, M.; Inoue, S.; Ishikawa, Y.; Bauman, A.; Lee, I.M.; Miyachi, M.; Kawachi, I. Community-Wide Intervention and Population-Level Physical Activity: A 5-Year Cluster Randomized Trial. Int. J. Epidemiol. 2018, 47, 642–653. [Google Scholar] [CrossRef]
- Gomi, T.; Kitayuguchi, J.; Okuyama, K.; Kamada, M.; Inoue, S.; Kamioka, H.; Mutoh, Y. Relationship between Neighborhood Food Environment and Diet Variety in Japanese Rural Community-Dwelling Elderly: A Cross-Sectional Study. J. Epidemiol. 2021. [Google Scholar] [CrossRef]
- Gray, I.; Williams, R.; Phillips, E. Rural community and leadership in the management of natural resources: Tensions between theory and policy. J. Environ. Policy Plan 2005, 7, 125–139. [Google Scholar] [CrossRef]
- Sirven, N. Endogenous social capital and self-rated health: Cross-sectional data from rural areas of Madagascar. Soc. Sci. Med. 2006, 63, 1489–1502. [Google Scholar] [CrossRef]
- Naito, Y.; Ohta, R.; Sano, C. Solving social problems in aging rural Japanese communities: The development and sustainability of the Osekkai Conference as a social prescribing during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 11849. [Google Scholar] [CrossRef]
- Ohta, R.; Yata, A. The revitalization of ‘Osekkai’: How the COVID-19 pandemic has emphasized the importance of Japanese voluntary social work. Qual. Soc. Work 2021, 20, 423–432. [Google Scholar] [CrossRef]
- Aslani, P. Patient empowerment and informed decision-making. Int. J. Pharm. Pract. 2013, 21, 347–348. [Google Scholar] [CrossRef]
- Ocloo, J.; Matthews, R. From tokenism to empowerment: Progressing patient and public involvement in healthcare improvement. BMJ Qual. Saf. 2016, 25, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Ryu, Y.; Sano, C. Older people’s help-seeking behaviors in rural contexts: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 3233. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K.; Mudgal, S.K.; Thakur, K.; Parihar, A.; Chundawat, D.S.; Joshi, J. Anxiety, depression and quality of life (QOL) related to COVID-19 among frontline health care professionals: A multicentric cross-sectional survey. J. Fam. Med. Prim. Care 2021, 10, 1383–1389. [Google Scholar] [CrossRef] [PubMed]
- Algahtani, F.D.; Hassan, S.U.; Alsaif, B.; Zrieq, R. Assessment of the quality of life during COVID-19 pandemic: A cross-sectional survey from the Kingdom of Saudi Arabia. Int. J. Environ. Res. Public Health 2021, 18, 847. [Google Scholar] [CrossRef]
- Iqbal, A.; Iqbal, K.; Arshad Ali, S.; Azim, D.; Farid, E.; Baig, M.D.; Bin Arif, T.; Raza, M. The COVID-19 sequelae: A cross-sectional evaluation of post-recovery symptoms and the need for rehabilitation of COVID-19 survivors. Cureus 2021, 13, e13080. [Google Scholar] [CrossRef]
| Variables | Using Self-Management (n = 84) | Not Using Self-Management (n = 119) | p-Value |
|---|---|---|---|
| Age, mean (SD) | 77.26 (8.30) | 78.50 (7.17) | 0.26 |
| Sex, male (%) | 38 (45.8) | 60 (51.3) | 0.47 |
| Weight (kg), mean (SD) | 55.39 (11.75) | 56.19 (11.11) | 0.629 |
| Height (cm), mean (SD) | 156.39 (9.75) | 156.66 (9.26) | 0.844 |
| Chronic Diseases (%) | 74 (92.5) | 107 (91.5) | 1 |
| Alcohol Use (%) | 27 (32.1) | 43 (36.4) | 0.552 |
| Smoking (%) | 8 (9.5) | 10 (8.4) | 0.806 |
| Higher Education (%) | 35 (42.2) | 51 (43.2) | 1 |
| Living with Family (%) | 74 (90.2) | 106 (90.6) | 1 |
| Annual Health Check (%) | 63 (76.8) | 88 (73.9) | 0.74 |
| High Socioeconomic Status (%) | 45 (54.9) | 57 (48.3) | 0.39 |
| High Social Support (%) | 71 (86.6) | 94 (80.3) | 0.339 |
| Variables | Using Self-Management (n = 84) | Not Using Self-Management (n = 119) | p-Value |
|---|---|---|---|
| Single Health Status Index Score | |||
| Change, mean (SD) | 0.08 (0.21) | -0.01 (0.20) | 0.002 |
| 2021 | 0.70 (0.21) | 0.64 (0.24) | 0.089 |
| 2022 | 0.78 (0.16) | 0.63 (0.24) | <0.001 |
| Dimension 1: Mobility | |||
| 2021 | 1.90 (1.36) | 2.10 (1.37) | 0.314 |
| 2022 | 1.51 (0.95) | 2.12 (1.35) | 0.001 |
| Dimension 2: Self-Care | |||
| 2021 | 1.42 (0.89) | 1.63 (1.13) | 0.15 |
| 2022 | 1.20 (0.71) | 1.66 (1.18) | 0.002 |
| Dimension 3: Usual Activities | |||
| 2021 | 1.69 (1.02) | 2.08 (1.15) | 0.015 |
| 2022 | 1.48 (0.84) | 2.12 (1.22) | <0.001 |
| Dimension 4: Pain/Discomfort | |||
| 2021 | 2.15 (0.91) | 2.41 (1.07) | 0.075 |
| 2022 | 1.93 (0.90) | 2.54 (1.10) | <0.001 |
| Dimension 5: Anxiety/Depression | |||
| 2021 | 1.81 (0.83) | 1.94 (1.01) | 0.327 |
| 2022 | 1.51 (0.70) | 2.04 (1.02) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohta, R.; Ryu, Y.; Sano, C. Improvement in Quality of Life through Self-Management of Mild Symptoms during the COVID-19 Pandemic: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 6652. https://doi.org/10.3390/ijerph19116652
Ohta R, Ryu Y, Sano C. Improvement in Quality of Life through Self-Management of Mild Symptoms during the COVID-19 Pandemic: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(11):6652. https://doi.org/10.3390/ijerph19116652
Chicago/Turabian StyleOhta, Ryuichi, Yoshinori Ryu, and Chiaki Sano. 2022. "Improvement in Quality of Life through Self-Management of Mild Symptoms during the COVID-19 Pandemic: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 19, no. 11: 6652. https://doi.org/10.3390/ijerph19116652
APA StyleOhta, R., Ryu, Y., & Sano, C. (2022). Improvement in Quality of Life through Self-Management of Mild Symptoms during the COVID-19 Pandemic: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 19(11), 6652. https://doi.org/10.3390/ijerph19116652







