Cancer Screening Program Delivered by Community Health Workers for Chinese Married Immigrant Women in Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design and Ethical Considerations
2.2. Sample Size and Power Calculation
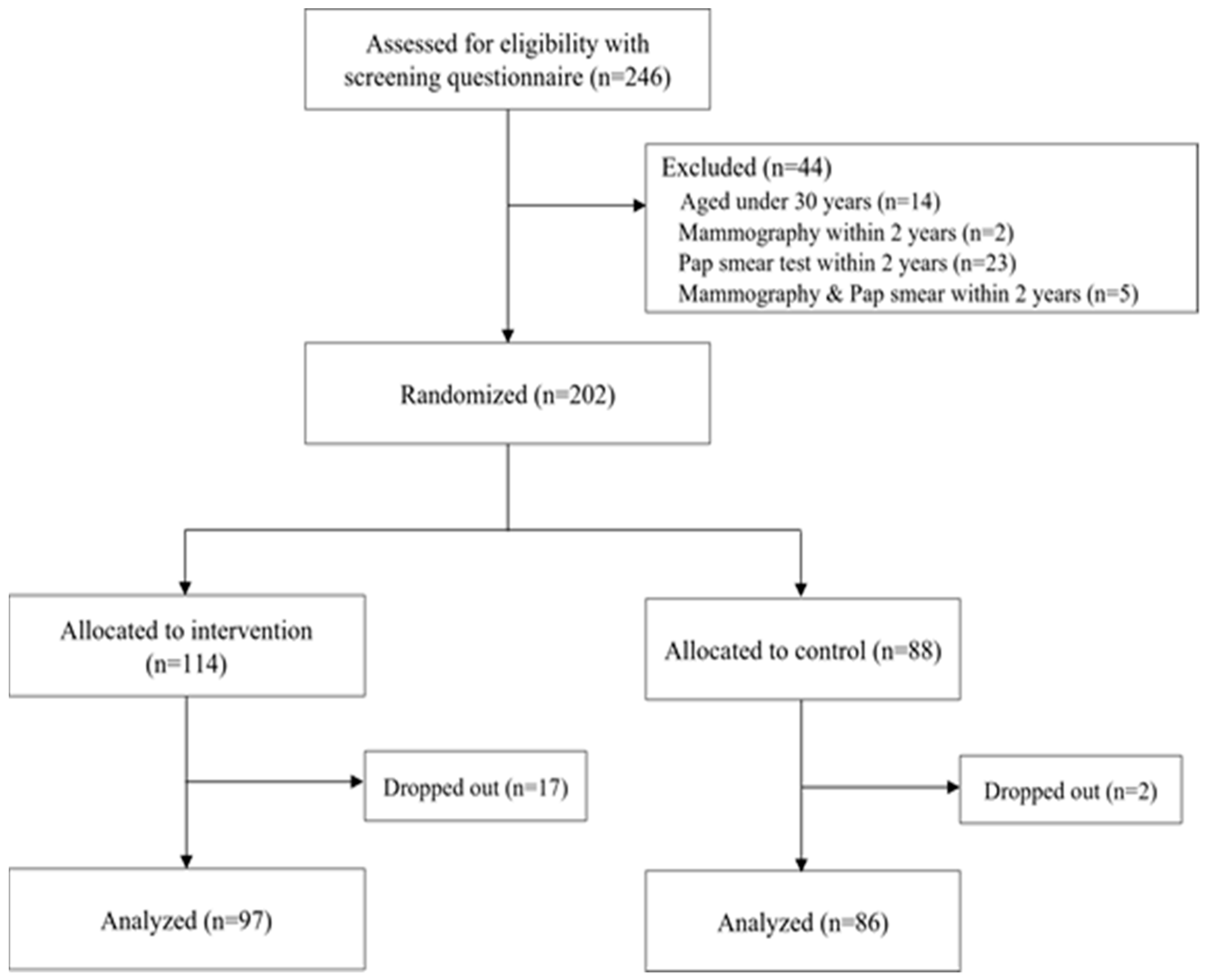
2.3. Participants and Study Setting
2.3.1. Study Procedure
2.3.2. CHWs Recruitment and Study Training
2.3.3. Recruiting Participants and Delivering Intervention by CHWs
2.4. Outcome Measures
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, J.; Yang, S.B.; Torneo, A.R. Marriage Immigration and Gender in South Korea: Accounting for Gender Disparities in International Marriages. Asia-Pacific Social Science Review. Asia-Pac. Soc. Sci. Rev. 2012, 12, 14–32. [Google Scholar]
- Song, J. Five phases of brokered international marriages in South Korea: A complexity perspective. Asian Studies. Asian Stud. 2015, 1, 147–176. [Google Scholar]
- Kim-Bossard, M. Challenging Homogeneity in Contemporary Korea-Immigrant Women, Immigrant Laborers, and Multicultural Families. Educ. Asia 2018, 23, 38–41. [Google Scholar]
- Kim, H.S. The Social Integration Policy for Foreigners in Korea and its Effects on Migrant Women’s Networks: An Observational Study. OMNES J. Multicult. Soc. 2018, 8, 126–160. [Google Scholar] [CrossRef]
- Kim, S.; Song, H.; Kim, K.; Choi, J. 2020 Multicultural Population Statistics; Statistics Korea: Daejeon, Korea, 2021. [Google Scholar]
- Park, M.N.; Choi, S.Y. Development of Reproductive Health Program and Identification of Effect for Married Women Immigrants. J. Korean Acad. Nurs. 2014, 44, 248–258. [Google Scholar] [CrossRef]
- Seol, D.H.; Kim, Y.; Kim, H.M.; Yoon, H. Foreign Wives’ Life in Korea: Focusing on the Policy of Welfare and Health; Ministry of Health and Welfare: Gwacheon, Korea, 2005; Available online: https://www.researchgate.net/publication/317953554_Foreign_wives’_life_in_Korea_Focusing_on_the_policy_of_welfare_and_health (accessed on 6 May 2022).
- Yang, S.J. Health Status, Health Care Utilization and Related Factors among Asian Immigrant Women in Korea. J. Korean Acad. Public Health Nurs. 2010, 24, 323–335. [Google Scholar]
- Choi, N.-Y.; Lee, B.-S. Factors of Breast and Cervical Cancer Screening Behaviors in Married Female Immigrants. J. Korea Contents Assoc. 2015, 15, 326–336. [Google Scholar] [CrossRef][Green Version]
- Seo, M.S.; Park, K.S.; Park, H.M.; Park, H.O. A Study on Health Behavior and Quality of Life of Married Immigrant Women. J. Korean Soc. Menopause 2013, 19, 121. [Google Scholar] [CrossRef]
- Kim, C.; Park, M.S.; Kim, E.M. Married Immigrant Women’s Utilization of Health Care and Needs of Health Services. J. Korean Acad. Community Health Nurs. 2011, 22, 333–341. [Google Scholar] [CrossRef][Green Version]
- National Cancer Center. National Cancer Screening Program. Available online: https://www.ncc.re.kr/main.ncc?uri=english/sub04_ControlPrograms03 (accessed on 6 May 2022).
- Lehmann, U.; Sanders, D. Community Health Workers: What Do We Know About Them? The State of the Evidence on Programmes, Activities, Costs an Impact on Health Outcomes of Using Community Health Workers. Geneva. 2007. Available online: https://www.hrhresourcecenter.org/node/1587.html (accessed on 9 May 2022).
- Herman, A.A. Community Health Workers and Integrated Primary Health Care Teams in the 21st Century. J. Ambul. Care Manag. 2011, 34, 354–361. [Google Scholar] [CrossRef]
- O’Brien, M.J.; Squires, A.; Bixby, R.A.; Larson, S.C. Role Development of Community Health Workers: An Examination of Selection and Training Processes in the Intervention Literature. Am. J. Prev. Med. 2009, 37, S262–S269. [Google Scholar] [CrossRef] [PubMed]
- Mock, J.; McPhee, S.J.; Nguyen, T.; Wong, C.; Doan, H.; Lai, K.Q.; Nguyen, K.H.; Nguyen, T.T.; Bui-Tong, N. Effective Lay Health Worker Outreach and Media-Based Education for Promoting Cervical Cancer Screening Among Vietnamese American Women. Am. J. Public Health 2007, 97, 1693–1700. [Google Scholar] [CrossRef] [PubMed]
- Han, H.-R.; Kim, K.B.; Kim, M.T. Evaluation of the training of Korean community health workers for chronic disease management. Health Educ. Res. 2006, 22, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Rohan, E.A.; McDougall, R.; Townsend, J.S. An Exploration of Patient Navigation and Community Health Worker Activities Across National Comprehensive Cancer Control Programs. Health Equity 2018, 2, 366–374. [Google Scholar] [CrossRef]
- Mojica, C.M.; Morales-Campos, D.Y.; Carmona, C.M.; Ouyang, Y.; Liang, Y. Breast, Cervical, and Colorectal Cancer Education and Navigation. Health Promot. Pr. 2015, 17, 353–363. [Google Scholar] [CrossRef]
- Nimmons, K.; Beaudoin, C.E.; John, J.A.S. The Outcome Evaluation of a CHW Cancer Prevention Intervention: Testing Individual and Multilevel Predictors Among Hispanics Living Along the Texas-Mexico Border. J. Cancer Educ. 2015, 32, 183–189. [Google Scholar] [CrossRef]
- Schuster, A.L.; Frick, K.D.; Huh, B.-Y.; Kim, K.B.; Kim, M.; Han, H.-R. Economic Evaluation of a Community Health Worker-Led Health Literacy Intervention to Promote Cancer Screening Among Korean American Women. J. Health Care Poor Underserved 2015, 26, 431–440. [Google Scholar] [CrossRef]
- Han, H.-R.; Song, Y.; Kim, M.; Hedlin, H.K.; Kim, K.; Ben Lee, H.; Roter, D. Breast and Cervical Cancer Screening Literacy Among Korean American Women: A Community Health Worker–Led Intervention. Am. J. Public Health 2017, 107, 159–165. [Google Scholar] [CrossRef]
- Kim, S.; Kim, Y.; Cho, A.; Kim, H.; Lee, H.; Seol, D.; Jung, K.; Shim, I. A Study on the National Multicultural Families Survey. Ministry of Gender Equality and Family. Seoul. 2009. Available online: http://www.mogef.go.kr/mp/pcd/mp_pcd_s001d.do;jsessionid=lb44XxRyznLcHoKpp6gpBzDX.mogef11?mid=plc503&bbtSn=429202 (accessed on 4 May 2022).
- Lam, T.K.; McPhee, S.J.; Mock, J.; Wong, C.; Doan, H.T.; Nguyen, T.; Lai, K.Q.; Ha-Iaconis, T.; Luong, T.-N. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. J. Gen. Intern. Med. 2003, 18, 516–524. [Google Scholar] [CrossRef]
- Health Promotion < National Health Insurance. Available online: https://www.nhis.or.kr/english/wbheaa02700m01.do (accessed on 12 May 2022).
- Dicolen, E.D.; Sanchez, N. Multicultural Family Support Centers (MFSCs) in South Korea: Promoting Harmony and Cultural. Integr. Int. J. Educ. Learn. 2016, 5, 57–70. [Google Scholar] [CrossRef]
- Grove, S.K.; Burns, N. The Practice of Nursing Research: Appraisal, Synthesis and Generation of Evidence, 6th ed.; Burns, N., Grove, S.K., Eds.; Saunders Elsevier: St. Louis, MO, USA, 2009. [Google Scholar]
- McCance, K.L.; Mooney, K.H.; Smith, K.R.; Field, R. Validity and Reliability of a Breast Cancer Knowledge Test. Am. J. Prev. Med. 1990, 6, 93–98. [Google Scholar] [CrossRef]
- Han, H.-R.; Huh, B.; Kim, M.T.; Kim, J.; Nguyen, T. Development and Validation of the Assessment of Health Literacy in Breast and Cervical Cancer Screening. J. Health Commun. 2014, 19, 267–284. [Google Scholar] [CrossRef] [PubMed]
- Wells, K.J.; Luque, J.; Miladinovic, B.; Vargas, N.; Asvat, Y.; Roetzheim, R.G.; Kumar, A. Do Community Health Worker Interventions Improve Rates of Screening Mammography in the United States? A Systematic Review. Cancer Epidemiol. Biomark. Prev. 2011, 20, 1580–1598. [Google Scholar] [CrossRef] [PubMed]
- Islam, N.; Shapiro, E.; Wyatt, L.; Riley, L.; Zanowiak, J.; Ursua, R.; Trinh-Shevrin, C. Evaluating community health workers’ attributes, roles, and pathways of action in immigrant communities. Prev. Med. 2017, 103, 1–7. [Google Scholar] [CrossRef]
- Witmer, A.; Seifer, S.D.; Finocchio, L.; Leslie, J.; O’Neil, E.H. Community health workers: Integral members of the health care work force. Am. J. Public Health 1995, 85, 1055–1058. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.; Han, H.-R. Chinese Immigrant Women’s Experiences as Community Health Workers in Korea: A Focus Group Study. J. Nurs. Res. 2021, 29, e172. [Google Scholar] [CrossRef]
- Seo, J.Y.; Li, J.; Li, K. Cervical Cancer Screening Experiences Among Chinese American Immigrant Women in the United States. J. Obstet. Gynecol. Neonatal Nurs. 2017, 47, 52–63. [Google Scholar] [CrossRef]
- Chen, W.-T.; Wang, J. Chinese Female Immigrants English-Speaking Ability and Breast and Cervical Cancer Early Detection Practices in the New York Metropolitan Area. Asian Pac. J. Cancer Prev. 2013, 14, 733–738. [Google Scholar] [CrossRef]
- Nguyen, G.T.; Chen, B.; Chan, M. Pap Testing, Awareness, and Acceptability of a Human Papillomavirus (HPV) Vaccine Among Chinese American Women. J. Immigr. Minor. Health 2012, 14, 803–808. [Google Scholar] [CrossRef]
- Wong, C.L.; Choi, K.C.; Law, B.M.H.; Chan, D.N.S.; So, W.K.W. Effects of a Community Health Worker-Led Multimedia Intervention on the Uptake of Cervical Cancer Screening among South Asian Women: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 3072. [Google Scholar] [CrossRef]
- Islam, N.S.; Wyatt, L.C.; Taher, M.; Riley, L.; Tandon, S.D.; Tanner, M.; Mukherji, B.R.; Trinh-Shevrin, C. A Culturally Tailored Community Health Worker Intervention Leads to Improvement in Patient-Centered Outcomes for Immigrant Patients With Type 2 Diabetes. Clin. Diabetes 2018, 36, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, A.R.; Morrison, C.; Anderson, N.N. The design and impact of culturally-safe community-based physical activity promotion for immigrant women: Descriptive review. BMC Public Health 2022, 22, 430. [Google Scholar] [CrossRef] [PubMed]
| Intervention | Control | Total | t/χ2 | p | |
|---|---|---|---|---|---|
| Age (years, range 30–64) | 38.28 ± 6.39 | 38.40 ± 7.73 | 38.33 ± 7.03 | −0.112 | 0.911 |
| Education | |||||
| Middle school graduate or less | 24 (13.1) | 19 (10.4) | 43 (23.5) | 1.401 | 0.496 |
| High school graduate | 47 (25.7) | 37 (20.2) | 84 (45.9) | ||
| College or more | 26 (14.2) | 30 (16.4) | 56 (30.6) | ||
| Length of stay in Korea (year, range 1–22) | 7.77 (4.30) | 8.31 ± 3.49 | 8.03 ± 3.94 | −0.926 | 0.356 |
| Employment | |||||
| Employed | 75 (41.0) | 58 (31.7) | 133 (72.7) | 2.240 | 0.134 |
| Unemployed | 22 (12.0) | 28 (15.3) | 50 (27.3) | ||
| Income level (Korean Won) | |||||
| 200 million or less | 37 (20.2) | 48 (26.2) | 85 (46.4) | 5.858 | 0.053 |
| 300 million or less | 34 (18.6) | 23 (12.6) | 57 (31.1) | ||
| Over 300 million | 26 (14.2) | 15 (8.2) | 41 (22.4) | ||
| Number of children | |||||
| 0 | 10 (5.5) | 7 (3.8) | 17 (9.3) | 0.361 | 0.835 |
| 1 | 55 (30.1) | 48 (26.2) | 103 (56.3) | ||
| 2 or more | 32 (17.5) | 31 (16.9) | 63 (34.4) | ||
| Mammography knowledge | 8.29 ± 4.09 | 6.44 ± 4.22 | 7.42 ± 4.24 | −3.002 | 0.003 |
| Pap test knowledge | 4.77 ± 2.60 | 4.20 ± 2.60 | 4.50 ± 2.61 | −1.493 | 0.137 |
| History of screening | |||||
| Underwent mammography | 14 (23.0) | 10 (16.4) | 24 (39.3) | 0.108 | 0.742 |
| Underwent a Pap test | 20 (10.9) | 20 (10.9) | 40 (21.9) | 0.186 | 0.667 |
| Variable | Groups | Pre | Post | Sources | F (p) | Post-Pre t (p) | |
|---|---|---|---|---|---|---|---|
| Mammography knowledge | Intervention (97) | 8.29 ± 4.09 | 9.41 ± 3.28 | Group | 9.297 | 0.003 | 4.643 (<0.001) |
| Control (86) | 6.44 ± 4.22 | 8.24 ± 4.16 | Time | 9.297 | 0.003 | 3.780 (<0.001) | |
| Group × Time | 9.297 | 0.003 | |||||
| Pap test knowledge | Intervention (97) | 4.77 ± 2.60 | 5.58 ± 2.17 | Group | 4.073 | 0.045 | 3.996 (<0.001) |
| Control (86) | 4.20 ± 2.60 | 4.90 ± 2.46 | Time | 15.698 | <0.001 | 2.361 (0.020) | |
| Group × Time | 0.079 | 0.779 |
| Pre | Post | p | ||
|---|---|---|---|---|
| Underwent mammography (%) | Intervention | 14 (23.0) | 19 (31.1) | 0.267 |
| Control | 10 (16.4) | 0 (0) | 0.002 | |
| Underwent Pap test (%) | Intervention | 20 (10.9) | 23 (23.7) | 0.690 |
| Control | 20 (10.9) | 9 (10.5) | 0.019 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Paik, Y.; Park, S. Cancer Screening Program Delivered by Community Health Workers for Chinese Married Immigrant Women in Korea. Int. J. Environ. Res. Public Health 2022, 19, 6655. https://doi.org/10.3390/ijerph19116655
Kim J, Paik Y, Park S. Cancer Screening Program Delivered by Community Health Workers for Chinese Married Immigrant Women in Korea. International Journal of Environmental Research and Public Health. 2022; 19(11):6655. https://doi.org/10.3390/ijerph19116655
Chicago/Turabian StyleKim, Jiyun, Yuna Paik, and Seungmi Park. 2022. "Cancer Screening Program Delivered by Community Health Workers for Chinese Married Immigrant Women in Korea" International Journal of Environmental Research and Public Health 19, no. 11: 6655. https://doi.org/10.3390/ijerph19116655
APA StyleKim, J., Paik, Y., & Park, S. (2022). Cancer Screening Program Delivered by Community Health Workers for Chinese Married Immigrant Women in Korea. International Journal of Environmental Research and Public Health, 19(11), 6655. https://doi.org/10.3390/ijerph19116655






