Changes in Postural Control Ability after Wearing Corrective Glasses for Distance in Older Adults and Their Causes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
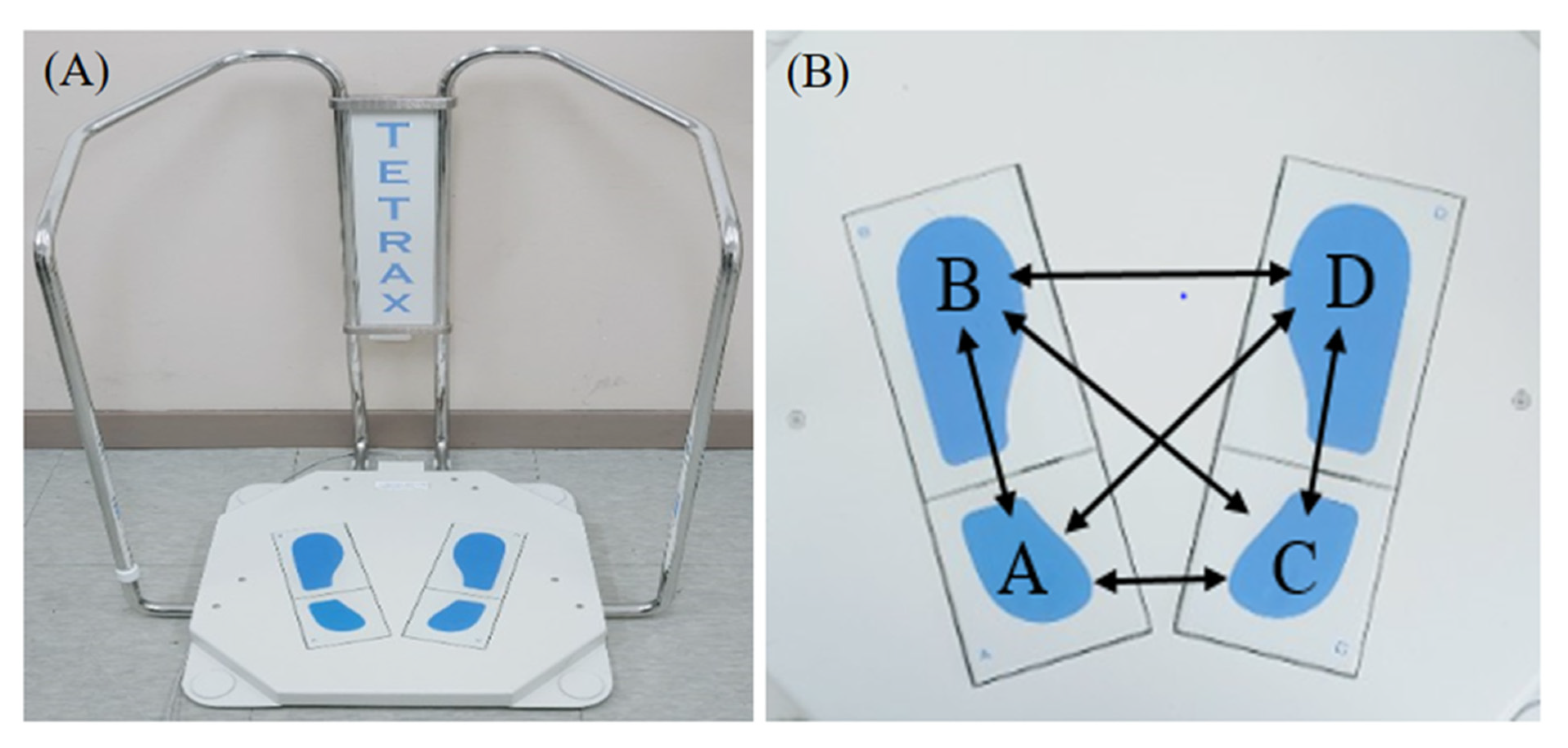
2.2. Measurement Equipment
2.3. Measurement Factors
2.3.1. Stability Index
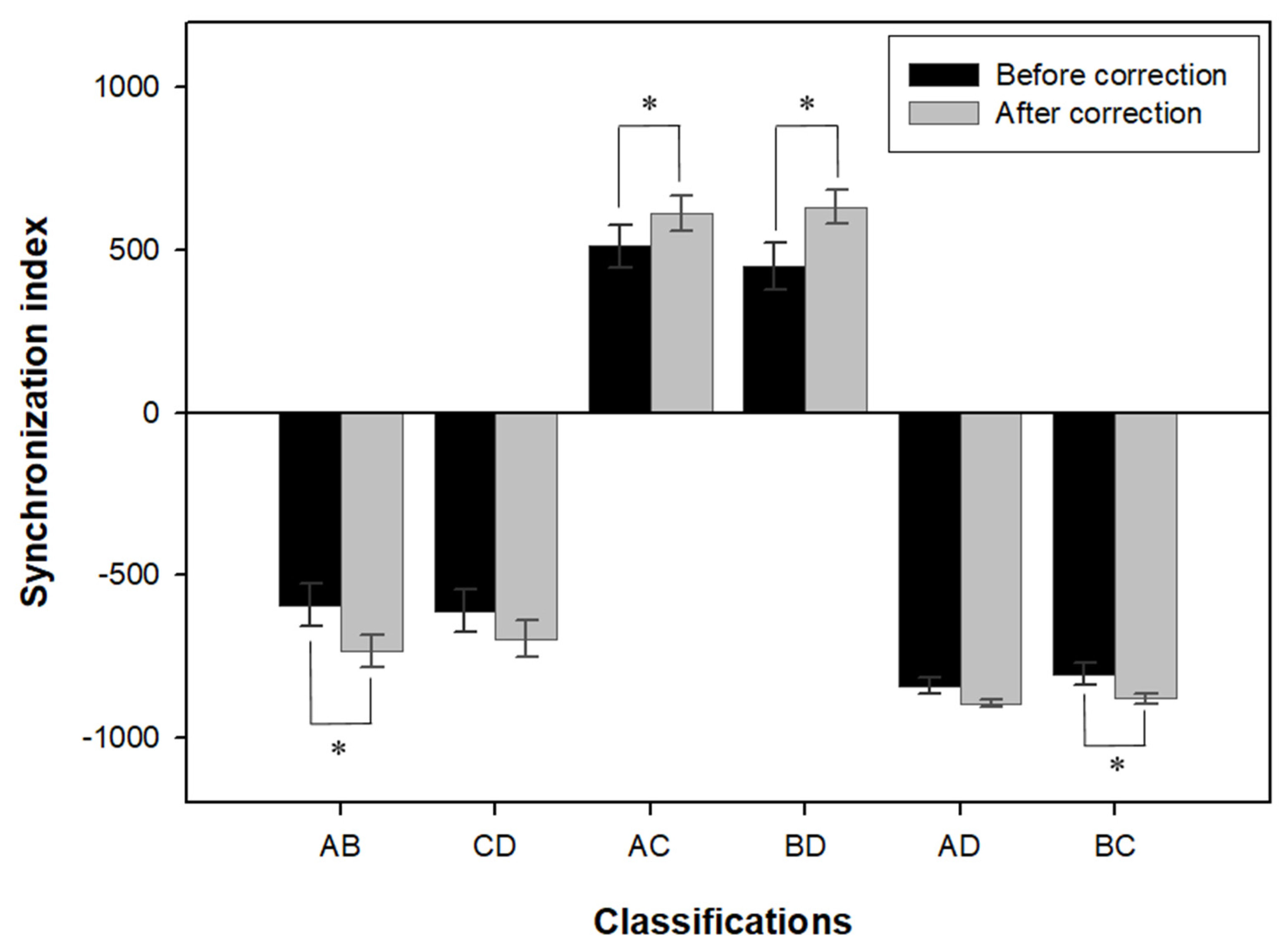
2.3.2. Synchronization Index
2.3.3. Sway Power Index
- Low frequency region: This refers to the 0.01–0.1 Hz region, and an abnormally increased value is associated with a visual dysfunction.
- Mid/low frequency region: This refers to the 0.1–0.5 Hz region, and an abnormally increased value is associated with a disorder of the peripheral vestibular system.
- Mid/high frequency region: This refers to the 0.5–0.75 Hz region, and an abnormally increased value is associated with a somatosensory dysfunction.
- High frequency region: This refers to the 1.0–3.0 Hz region, and an abnormally increased value is associated with a disorder of the central nervous system.
2.4. Measurement Method
2.5. Measurement Result Analysis
3. Results
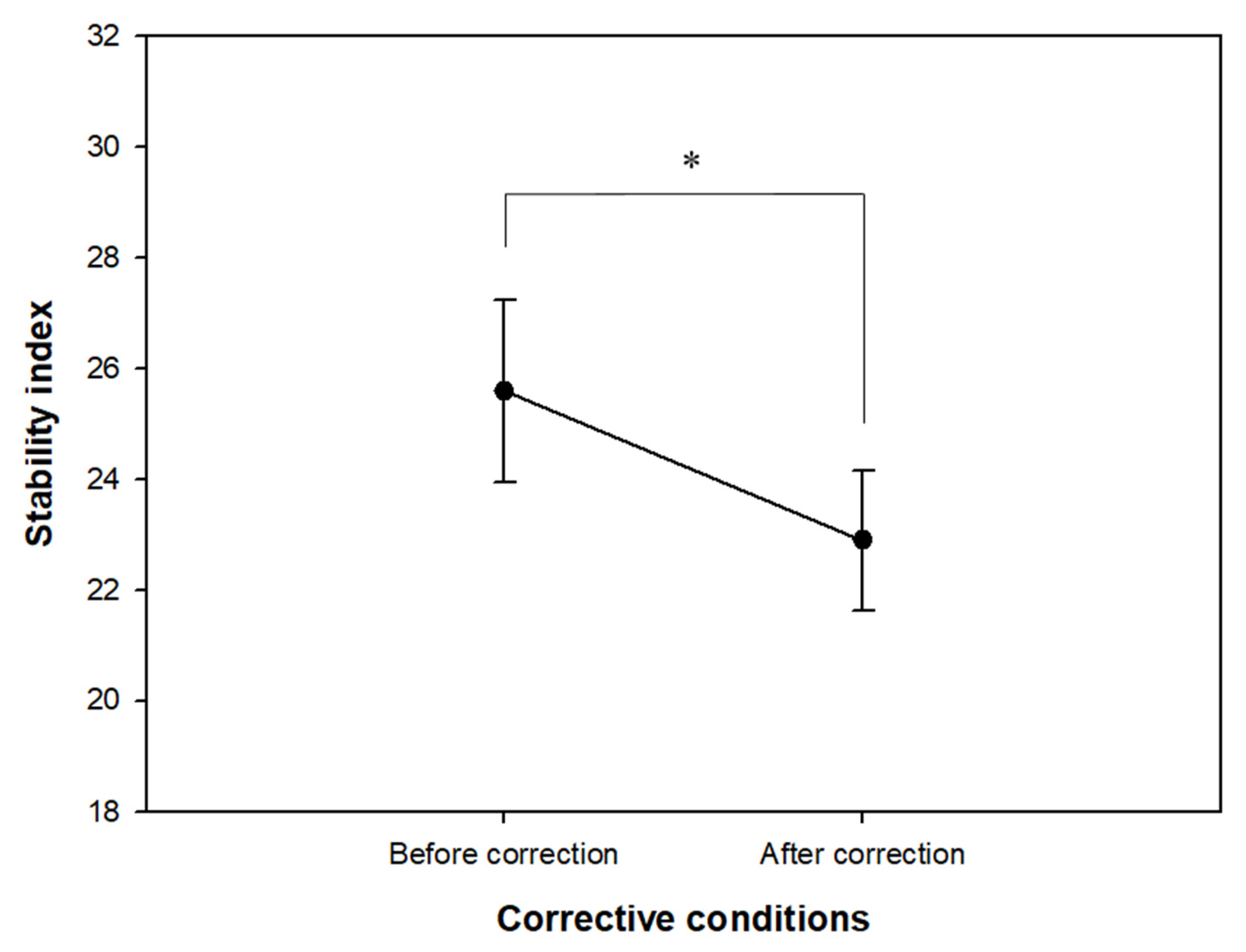
3.1. Changes in Stability Index
3.2. Changes in Synchronization Index
3.3. Analysis of Sway Power Index
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gaerlan, M.G.; Alpert, P.T.; Cross, C.; Louis, M.; Kowalski, S. Postural balance in young adults: The role of visual, vestibular and somatosensory systems. J. Am. Acad. Nurse Pract. 2012, 24, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.L.; Scarpace, D.; Alexander, N.B. Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adults. J. Am. Geriatr. Soc. 2004, 52, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Horlings, C.G.; van Engelen, B.G.; Allum, J.H.; Bloem, B.R. A weak balance: The contribution of muscle weakness to postural instability and falls. Nat. Clin. Pract. Neurol. 2008, 4, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Pijnappels, M.; van der Burg, P.J.; Reeves, N.D.; van Dieen, J.H. Identification of elderly fallers by muscle strength measures. Eur. J. Appl. Physiol. 2008, 102, 585–592. [Google Scholar] [CrossRef] [Green Version]
- Heitterachi, E.; Lord, S.R.; Meyerkort, P.; McCloskey, I.; Fitzpatrick, R. Blood pressure changes on upright tilting predict falls in older people. Age Ageing 2002, 31, 181–186. [Google Scholar] [CrossRef] [Green Version]
- Ooi, W.L.; Hossain, M.; Lipsitz, L.A. The association between orthostatic hypotension and recurrent falls in nursing home residents. Am. J. Med. 2000, 108, 106–111. [Google Scholar] [CrossRef]
- Klein, D.; Gabriele, N.; Andrea, K.; Hanno, U.; Barbara, R.; Hans, C.; Kilian, R. Blood pressure and falls in community-dwelling people aged 60 years and older in the VHM&PP cohort. BMC Geriatr. 2013, 13, 50. [Google Scholar]
- Magnusson, M.; Ekvall Hansson, E. Vestibular asymmetry predicts falls among elderly patients with multi- sensory dizziness. BMC Geriatr. 2013, 13, 77. [Google Scholar]
- Menant, J.C.; St George, R.J.; Fitzpatrick, R.C.; Lord, S.R. Perception of the postural vertical and falls in older people. Gerontology 2012, 58, 497–503. [Google Scholar] [CrossRef]
- Craig, C.E.; Goble, D.J.; Doumas, M. Proprioceptive acuity predicts muscle co-contraction of the tibialis anterior and gastrocnemius medialis in older adults’ dynamic postural control. Neuroscience 2016, 322, 251–261. [Google Scholar] [CrossRef] [Green Version]
- Lord, S.R.; Murray, S.M.; Chapman, K.; Munro, B.; Tiedemann, A. Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M539–M543. [Google Scholar] [CrossRef]
- Clark, R.D.; Lord, S.R.; Webster, I.W. Clinical parameters associated with falls in an elderly population. Gerontology 1993, 39, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R. Visual risk factors for falls in older people. Age Ageing 2006, 35 (Suppl. 2), ii42–ii45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, A.; Wood, J. Vision and falls. Clin. Exp. Optom. 2005, 88, 212–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coleman, A.L.; Cummings, S.R.; Yu, F.; Kodjebacheva, G.; Ensrud, K.E.; Gutierrez, P.; Stone, K.L.; Cauley, J.A.; Pedula, K.L.; Hochberg, M.C.; et al. Binocular visual-field loss increases the risk of future falls in older white women. J. Am. Geriatr. Soc. 2007, 55, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.Y.; Jeong, J.Y.; Lee, H.J. Predictive analysis of the Number of Cataract Surgeries. Korea J. Hosp. Manag. 2020, 25, 69–75. [Google Scholar]
- Anand, V.; Buckley, J.G.; Scally, A.; Elliott, D.B. Postural stability changes in the elderly with cataract simulation and refractive blur. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4670–4675. [Google Scholar] [CrossRef] [Green Version]
- Jack, C.I.; Smith, T.; Neoh, C.; Lye, M.; McGalliard, J.N. Prevalence of low vision in elderly patients admitted to an acute geriatric unit in Liverpool: Elderly people who fall are more likely to have low vision. Gerontology 1995, 41, 280–285. [Google Scholar] [CrossRef]
- Edwards, A.S. Body sway and vision. J. Exp. Psychol. 1946, 36, 526–535. [Google Scholar] [CrossRef]
- Paulus, W.M.; Straube, A.; Brandt, T. Visual stabilization of posture: Physiological stimulus characteristics and clinical aspects. Brain 1984, 107 Pt 4, 1143–1163. [Google Scholar] [CrossRef]
- Paulus, W.; Straube, A.; Quintern, J.; Brandt, T. Visual postural performance in ametropia and with optical distortion produced by bifocals and multifocals. Acta Otolaryngol. Suppl. 1989, 468, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Moon, B.Y.; Cho, H.G. Changes in falling risk depending on induced axis directions of astigmatism on static posture. J. Phys. Sci. 2015, 27, 1971–1973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, B.Y.; Choi, J.H.; Yu, D.S.; Kim, S.Y. Effect of induced hyperopia on fall risk and Fourier transformation of postural sway. PeerJ 2019, 7, e8329. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.I.; Yu, D.S.; and Kim, S.Y. Effect of optical correction by fully corrected glasses on postural stability. PLoS ONE 2020, 15, e0235919. [Google Scholar] [CrossRef]
- Bae, J.I.; Cho, H.G.; Moon, B.Y.; Yu, D.S.; Kim, S.Y. Changes in postural stability after wearing full-corrected new glasses. J. Korean Ophthalmic. Opt. Soc. 2016, 21, 259–264. [Google Scholar]
- Kim, T.H.; Yi, J.H.; Oh, S.G. Staticposture stability evaluation of female elderly using stability evaluation device. J. Korea Acad.-Ind. Coop. Soc. 2011, 12, 5518–5524. [Google Scholar]
- Kang, K.Y. Effects of functional electrical stimulation training on weight distribution and synchronization of the lower extremity of patients with post-stroke. J. Korean Phys. Ther. Sci. 2012, 19, 9–15. [Google Scholar]
- Park, C.S.; Kang, K.Y. Effect of visual biofeedback simulation training for balance in patients with incomplete spinal cord injury. J. Korea Contents Assoc. 2011, 11, 194–203. [Google Scholar] [CrossRef] [Green Version]
- Kohen-Raz, R. Tetrax Physician Guide; Beammed-Sunlight: Petah Tikva, Israel, 2004; pp. 1–2. [Google Scholar]
- Sunlight. TETRAX: Fourier Transformation of Postural Sway. 2006. Available online: https://pdfhall.com/1-tetrax-fourier-transformation-of-postural-sunlight_5b6e595c097c477e738b4614.html (accessed on 21 March 2022).
- Aniansson, A.; Hedberg, M.; Henning, G.B.; Grimby, G. Muscle morphology, enzymatic activity, and muscle strength in elderly men: A follow-up study. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 1986, 9, 585–591. [Google Scholar] [CrossRef]
- Anand, V.; Buckley, J.G.; Scally, A.; Elliott, D.B. Postural stability in the elderly during sensory perturbations and dual tasking: The influence of refractive blur. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2885–2891. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.N.; Eric, A. Visual proprioceptive control of standing in human infants. Percept. Psychophys. 1974, 15, 529–532. [Google Scholar] [CrossRef]
- Lee, D.N.; Lishman, J.R. Visual proprioceptive control of stance. J. Hum. Mov. Stud. 1975, 1, 87–95. [Google Scholar]
- DeWit, G. Optic versus vestibular and proprioceptive impulses, measured by posturography. Agressologie 1972, 13 (Suppl. B), 75–79. [Google Scholar]
- Loughlin, P.J.; Redfern, M.S. Spectral characteristics of visually induced postural sway in healthy elderly and healthy young subjects. IEEE Trans. Neural. Syst. Rehabil. Eng. 2001, 9, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Kollmitzer, J.; Ebenbichler, G.R.; Ebenbichler, G.R.; Sabo, A.; Kerschan, K.; Bochdansky, T. Effects of back extensor training versus balance training on postural control. Med. Sci. Sports Exerc. 2000, 32, 1770–1776. [Google Scholar] [CrossRef] [PubMed]
- Woollacott, M.H.; Shumway-Cook, A.; Nashner, L.M. Aging and posture control:changes in sensory organization and muscular coordination. Int. J. Aging Hum. Dev. 1986, 23, 97–114. [Google Scholar] [CrossRef] [PubMed]
| No | Age | Full-Corrective Prescription (Unit: Diopters) | Decimal Visual Acuity | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Right Eye | Left Eye | Before Correction | After Correction | ||||||
| RE 1 | LE 2 | BE 3 | RE | LE | BE | ||||
| 1 | 87 | S+1.50 C−0.75 Ax140 | S+2.25 C−1.75 Ax55 | 0.3 | 0.5 | 0.6 | 0.6 | 0.7 | 0.8 |
| 2 | 84 | S+1.00 C−0.50 Ax90 | S+1.00 C−0.50 Ax90 | 0.5 | 0.5 | 0.6 | 0.7 | 0.8 | 0.8 |
| 3 | 78 | S+1.50 C−0.50 Ax100 | S+0.75 C−0.50 Ax90 | 0.3 | 0.5 | 0.6 | 0.6 | 0.7 | 0.8 |
| 4 | 80 | S+1.75 C−0.75 Ax70 | S+2.00 C−0.75 Ax85 | 0.5 | 0.5 | 0.7 | 0.8 | 0.8 | 0.9 |
| 5 | 86 | S+0.50 C−1.00 Ax110 | S+1.00 C−1.00 Ax80 | 0.3 | 0.2 | 0.4 | 0.4 | 0.5 | 0.6 |
| 6 | 89 | S−0.25 C−1.00 Ax135 | C−0.50 Ax135 | 0.2 | 0.4 | 0.6 | 0.8 | 0.7 | 0.8 |
| 7 | 85 | S+2.50 C−0.50 Ax155 | S+2.75 C−0.75 Ax105 | 0.2 | 0.2 | 0.4 | 0.5 | 0.5 | 0.7 |
| 8 | 90 | S+1.75 C−1.50 Ax90 | S+2.50 C−1.75 Ax65 | 0.1 | 0.2 | 0.2 | 0.3 | 0.3 | 0.5 |
| 9 | 86 | C−2.00 Ax105 | S+0.50 C−2.00 Ax60 | 0.2 | 0.2 | 0.4 | 0.4 | 0.5 | 0.6 |
| 10 | 81 | S−0.50 | S+1.00 C−0.75 Ax90 | 0.4 | 0.5 | 0.6 | 0.7 | 0.7 | 0.8 |
| 11 | 81 | S+1.00 C−1.50 Ax100 | S+1.50 C−1.75 Ax110 | 0.6 | 0.5 | 0.7 | 0.7 | 0.8 | 0.9 |
| 12 | 90 | S+2.00 C−0.75 Ax95 | S+2.00 C−0.75 Ax70 | 0.1 | 0.1 | 0.3 | 0.4 | 0.4 | 0.5 |
| 13 | 68 | S+0.50 C−1.00 Ax90 | S+1.00 C−1.00 Ax80 | 0.4 | 0.3 | 0.6 | 0.8 | 0.7 | 0.9 |
| 14 | 77 | C−1.25 Ax180 | C−1.00 Ax165 | 0.4 | 0.6 | 0.7 | 0.7 | 0.8 | 0.9 |
| 15 | 75 | S+0.50 C−0.50 Ax170 | S+1.75 C−0.25 Ax180 | 0.5 | 0.4 | 0.6 | 0.9 | 0.8 | 0.9 |
| 16 | 75 | S+2.00 C−2.00Ax75 | S+1.25 C−1.50 Ax110 | 0.2 | 0.4 | 0.5 | 0.5 | 0.7 | 0.8 |
| 17 | 79 | S+1.75 C−1.00 Ax60 | S+1.25 C−0.75 Ax130 | 0.1 | 0.1 | 0.2 | 0.6 | 0.6 | 0.7 |
| 18 | 74 | S+2.00 C−1.00 Ax90 | S+3.25 C−0.75 Ax115 | 0.5 | 0.3 | 0.7 | 0.6 | 0.6 | 0.8 |
| 19 | 69 | S−0.50 C−2.50 Ax95 | S+0.75 C−2.00 Ax80 | 0.3 | 0.6 | 0.6 | 0.8 | 0.7 | 0.8 |
| 20 | 78 | S+2.00 C−0.75 Ax100 | S+2.25 C−1.00 Ax90 | 0.3 | 0.3 | 0.5 | 0.6 | 0.6 | 0.8 |
| 21 | 71 | S−0.50 | S+0.25 C−1.00 Ax130 | 0.7 | 0.8 | 0.9 | 1.0 | 1.0 | 1.0 |
| 22 | 77 | S+1.00 | C−0.50 Ax105 | 1.0 | 0.8 | 1.0 | 1.0 | 1.0 | 1.0 |
| 23 | 79 | S+0.50 C−0.75 Ax90 | S+1.25 C−2.00Ax70 | 0.7 | 0.6 | 0.7 | 0.7 | 0.7 | 0.8 |
| 24 | 66 | S+0.50 | S+0.50 C−0.50 Ax75 | 1.2 | 1.0 | 1.2 | 1.2 | 1.2 | 1.2 |
| 25 | 78 | S−0.75 C−0.50 Ax170 | C−0.50 Ax60 | 0.5 | 0.7 | 0.7 | 0.8 | 0.8 | 0.8 |
| 26 | 77 | S+0.75 C−1.75 Ax105 | S+0.50 C−1.50 Ax 90 | 0.4 | 0.4 | 0.6 | 0.7 | 0.6 | 0.8 |
| 27 | 69 | S−0.25 | S−0.50 | 0.6 | 0.5 | 0.8 | 1.0 | 0.9 | 1.0 |
| Age Groups (n) | Correction Condition | Stability Index | p-Value |
|---|---|---|---|
| Total (27) | Before | 25.59 ± 8.54 | t = 2.254, p = 0.017 * |
| After | 22.89 ± 6.64 | ||
| ≥80 (12) | Before | 25.40 ± 9.39 | z = −2.275, p = 0.023 ** |
| After | 21.04 ± 5.50 | ||
| 80 > (15) | Before | 25.74 ± 8.13 | z = −0.568, p = 0.570 |
| After | 24.37 ± 7.27 |
| Age Groups (n) | Correction Condition | Sway Power Index in Each Frequency Range | |||
|---|---|---|---|---|---|
| Low | Low to Medium | Medium to High | High | ||
| Total (27) | Before | 21.99 ± 9.05 | 10.58 ± 3.04 | 4.90 ± 1.83 | 0.83 ± 0.29 |
| After | 20.47 ± 7.11 | 10.73 ± 3.31 | 4.23 ± 1.54 | 0.73 ± 0.26 | |
| t/p-values | 0.919/0.367 | 0.296/0.769 | 2.557/0.017 * | 2.560/0.017 * | |
| ≥80 (12) | Before | 20.71 ± 7.19 | 10.51 ± 3.81 | 4.79 ± 1.64 | 0.83 ± 0.24 |
| After | 19.43 ± 6.89 | 10.53 ± 3.67 | 3.76 ± 1.20 | 0.67 ± 0.21 | |
| z/p-values | −0.392/0.695 | −0.157/0.875 | −2.353/0.019 ** | −2.432/0.015 ** | |
| 80 > (15) | Before | 23.00 ± 10.44 | 10.64 ± 2.39 | 4.99 ± 2.02 | 0.84 ± 0.33 |
| After | 21.31 ± 7.41 | 10.89 ± 3.11 | 4.60 ± 1.71 | 0.78 ± 0.29 | |
| z/p-values | 0.000/1.000 | −0.682/0.496 | −0.682/0.427 | −0.511/−0.609 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, D.-S.; Kim, S.-Y. Changes in Postural Control Ability after Wearing Corrective Glasses for Distance in Older Adults and Their Causes. Int. J. Environ. Res. Public Health 2022, 19, 6643. https://doi.org/10.3390/ijerph19116643
Yu D-S, Kim S-Y. Changes in Postural Control Ability after Wearing Corrective Glasses for Distance in Older Adults and Their Causes. International Journal of Environmental Research and Public Health. 2022; 19(11):6643. https://doi.org/10.3390/ijerph19116643
Chicago/Turabian StyleYu, Dong-Sik, and Sang-Yeob Kim. 2022. "Changes in Postural Control Ability after Wearing Corrective Glasses for Distance in Older Adults and Their Causes" International Journal of Environmental Research and Public Health 19, no. 11: 6643. https://doi.org/10.3390/ijerph19116643
APA StyleYu, D.-S., & Kim, S.-Y. (2022). Changes in Postural Control Ability after Wearing Corrective Glasses for Distance in Older Adults and Their Causes. International Journal of Environmental Research and Public Health, 19(11), 6643. https://doi.org/10.3390/ijerph19116643






