Key Care Provision Aspects That Affect Care Transition in the Long-Term Care Systems: Preliminary Review Findings
Abstract
1. Introduction
1.1. Consequences and Reasons for Suboptimal Care Transitions
1.2. What Is Known about Optimizing Care Transitions
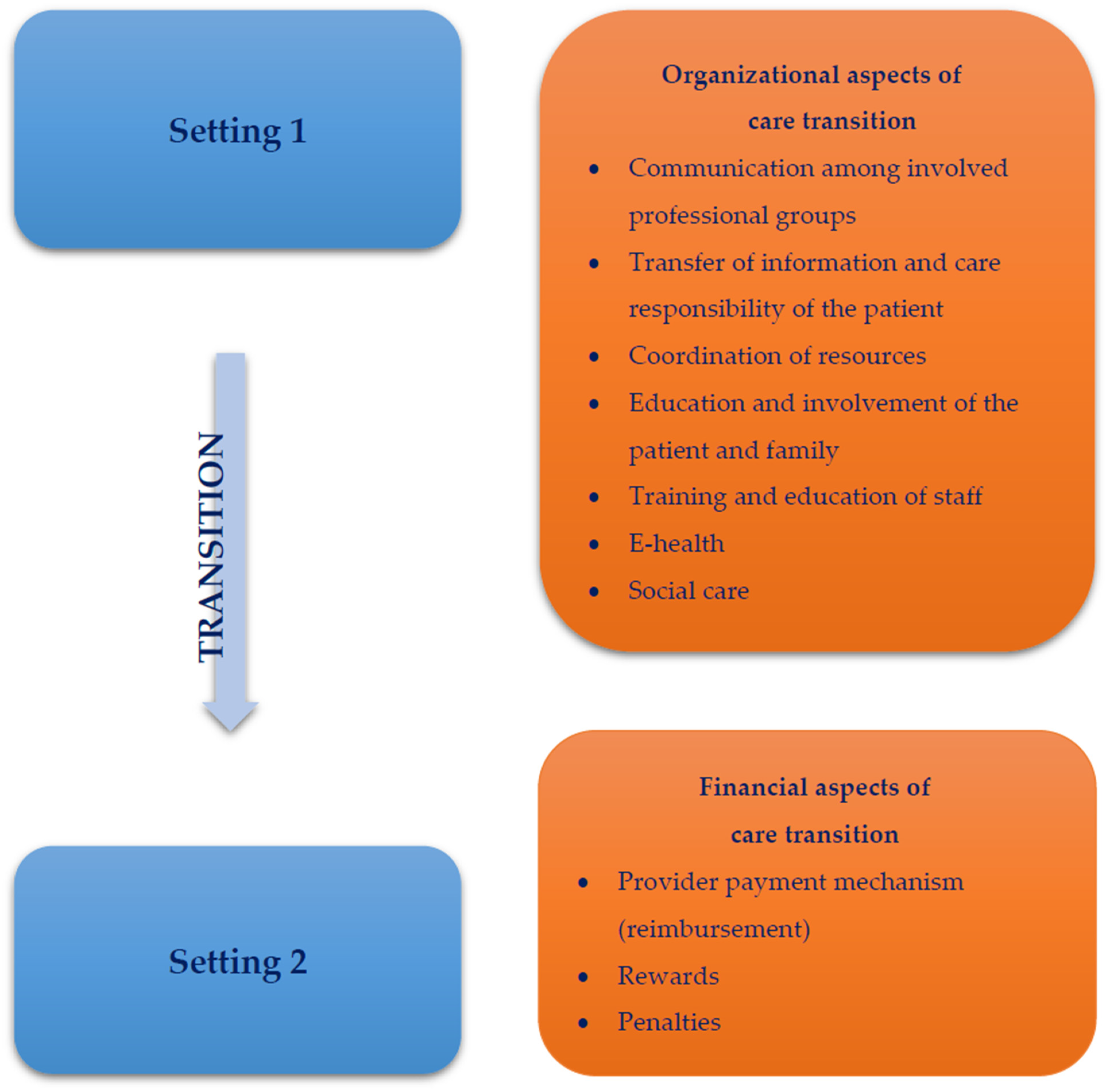
1.3. Why Focusing on Care Provision Aspects as Factors of Care Transition
2. Methods
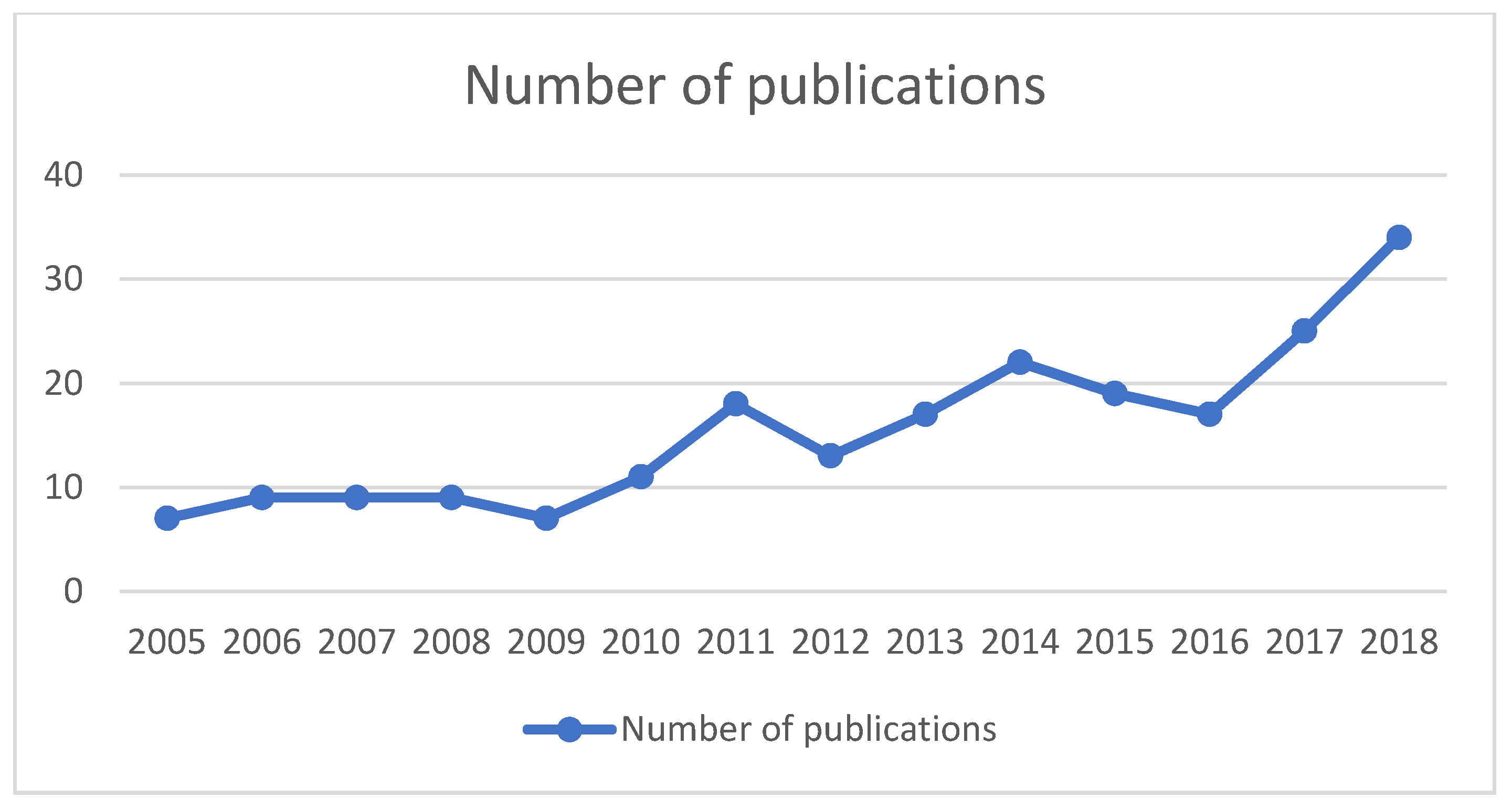
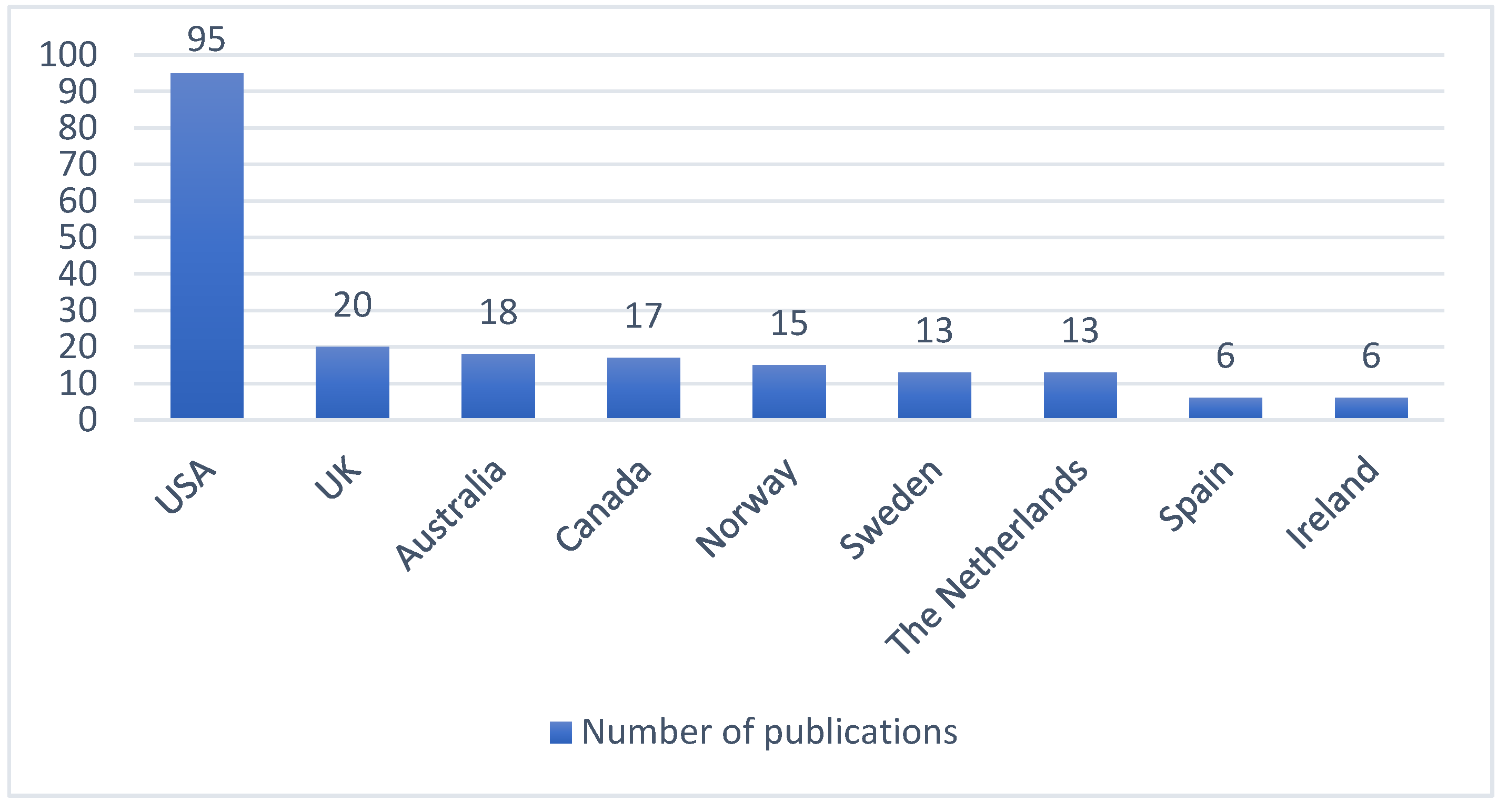
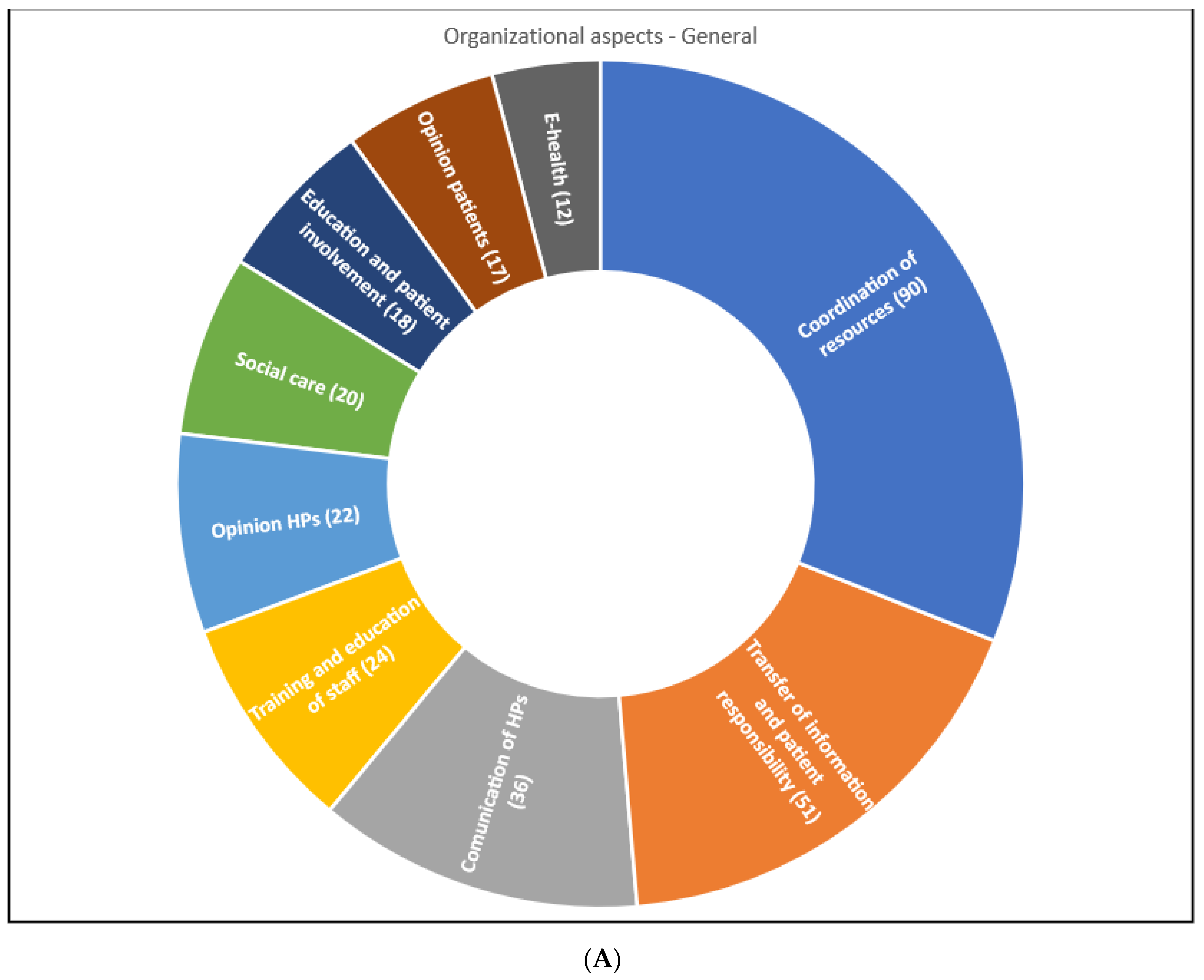
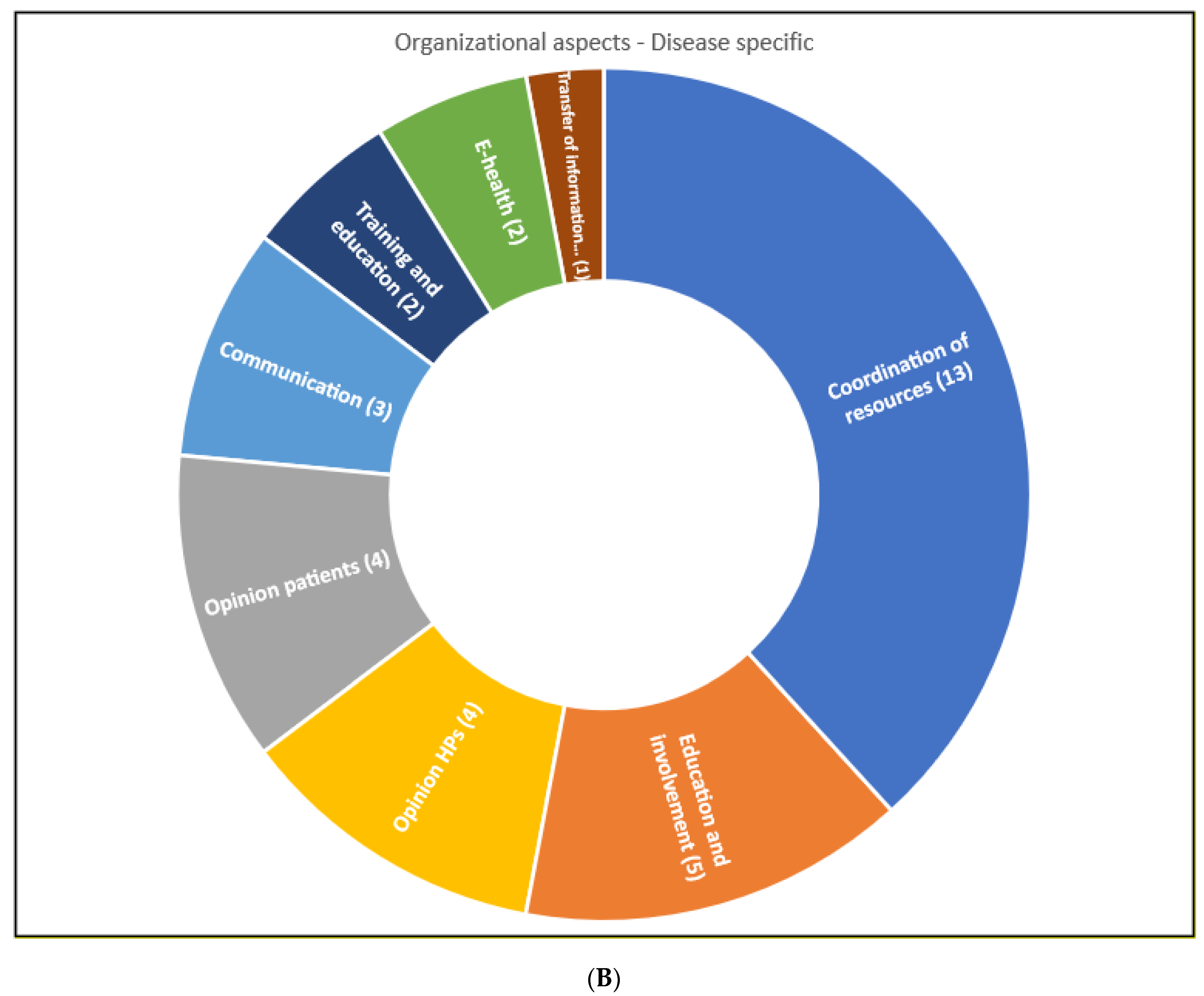
3. Results
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naylor, M.; Keating, S. Transitional Care: Moving patients from one care setting to another. Am. J. Nurs. 2008, 108, 58–63. [Google Scholar] [CrossRef]
- Coleman, E. Falling Through the Cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs. J. Am. Geriatr. Soc. 2003, 51, 549–555. [Google Scholar] [CrossRef]
- Naylor, M.D.; Shaid, E.C.; Carpenter, D.; Gass, B.; Levine, C.; Li, J.; Ma, C.L.; McCauley, K.; Nguyen, H.Q.; Watson, H.; et al. Components of Comprehensive and Effective Transitional Care. J. Am. Geriatr. Soc. 2017, 65, 1119–1125. [Google Scholar] [CrossRef]
- Coleman, E.; Boult, C. Improving the Quality of Transitional Care for Persons with Complex Care Needs. J. Am. Geriatr. Soc. 2003, 51, 556–557. [Google Scholar] [CrossRef]
- Aase, K.; Laugaland, K.; Dyrstad, D.; Storm, M. Quality and safety in transitional care of the elderly: The study protocol of a case study research design (phase 1). BMJ Open 2013, 3, e003506. [Google Scholar] [CrossRef][Green Version]
- Oakes, S.L.; Gillespie, S.M.; Ye, Y.; Finley, M.; Russell, M.; Patel, N.K.; Espino, D. Transitional Care of the Long-Term Care Patient. Clin. Geriatr. Med. 2011, 27, 259–271. [Google Scholar] [CrossRef]
- World Health Organization. Transitions of Care: Technical Series on Safer Primary Care; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Thorpe, K.E.; Howard, D.H. The Rise in Spending among Medicare Beneficiaries: The Role of Chronic Disease Prevalence and Changes in Treatment Intensity. Health Aff. 2006, 25, 378–388. [Google Scholar] [CrossRef]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Coleman, E.; Berenson, R. Lost in Transition: Challenges and Opportunities for Improving the Quality of Transitional Care. Ann. Intern. Med. 2004, 141, 533–536. [Google Scholar] [CrossRef]
- Elder, N.; Hickner, J. Missing Clinical Information. JAMA 2005, 293, 617. [Google Scholar] [CrossRef]
- Kripalani, S.; LeFevre, F.; Phillips, C.; Williams, M.; Basaviah, P.; Baker, D. Deficits in Communication and Information Transfer between Hospital-Based and Primary Care Physicians. JAMA 2007, 297, 831. [Google Scholar] [CrossRef]
- Schoen, C.; Osborn, R.; Huynh, P.; Doty, M.; Peugh, J.; Zapert, K. On The Front Lines of Care: Primary Care Doctors’ Office Systems, Experiences, and Views in Seven Countries. Health Aff. 2006, 25, 555–571. [Google Scholar] [CrossRef]
- Parry, C.; Mahoney, E.; Chalmers, S.; Coleman, E. Assessing the quality of transitional care: Further applications of the care transitions measure. Med. Care 2008, 46, 317–322. [Google Scholar] [CrossRef]
- Snow, V.; Beck, D.; Budnitz, T.; Miller, D.C.; Potter, J.; Wears, R.; Weiss, K.B.; Williams, M.V. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. J. Gen. Intern. Med. 2009, 24, 971–976. [Google Scholar] [CrossRef]
- Storm, M.; Siemsen, I.; Laugaland, K.; Dyrstad, D.; Aase, K. Quality in transitional care of the elderly: Key challenges and relevant improvement measures. Int. J. Integr. Care 2014, 14, e013. [Google Scholar] [CrossRef]
- Hastings, S.; Heflin, M. A Systematic Review of Interventions to Improve Outcomes for Elders Discharged from the Emergency Department. Acad. Emerg. Med. 2005, 12, 978–986. [Google Scholar] [CrossRef]
- Glasziou, P.P.; Buchan, H.; Del Mar, C.; Doust, J.; Harris, M.; Knight, R.; Scott, A.; Scott, I.; Stockwell, A. When financial incentives do more good than harm: A checklist. BMJ 2012, 345, e5047. [Google Scholar] [CrossRef][Green Version]
- Stokes, J.; Struckmann, V.; Kristensen, S.R.; Fuchs, S.; Van Ginneken, E.; Tsiachristas, A.; Van Mölken, M.R.; Sutton, M. Towards incentivising integration: A typology of payments for integrated care. Health Policy 2018, 122, 963–969. [Google Scholar] [CrossRef]
- Tsiachristas, A. Financial Incentives to Stimulate Integration of Care. Int. J. Integr. Care 2016, 16, 8. [Google Scholar] [CrossRef]
- Czypionka, T. Experimenting with a bundled payment system for diabetes care in The Netherlands: The first tangible effects. Int. J. Integr. Care 2011, 11, 4. [Google Scholar] [CrossRef]
- Wieczorek, E.; Kocot, E.; Evers, S.; Sowada, C.; Pavlova, M. Do financial aspects affect care transitions in long-term care systems? A systematic review. Arch. Public Health 2022, 80, 90. [Google Scholar] [CrossRef]
- Weaver, F.; Perloff, L.; Waters, T. Patients’ and Caregivers’ Transition from Hospital to Home: Needs and Recommendations. Home Health Care Serv. Q. 1998, 17, 27–48. [Google Scholar] [CrossRef]
- Coleman, E.; Smith, J.; Raha, D.; Min, S. Posthospital medication discrepancies: Prevalence and contributing factors. Arch. Intern. Med. 2005, 165, 1842–1847. [Google Scholar] [CrossRef]
- Kripalani, S.; Jackson, A.; Schnipper, J.; Coleman, E. Promoting effective transitions of care at hospital discharge: A review of key issues for hospitalists. J. Hosp. Med. 2007, 2, 314–323. [Google Scholar] [CrossRef]
- Baxter, R.; Shannon, R.; Murray, J.; O’Hara, J.K.; Sheard, L.; Cracknell, A.; Lawton, R. Delivering exceptionally safe transitions of care to older people: A qualitative study of multidisciplinary staff perspectives. BMC Health Serv. Res. 2020, 20, 780. [Google Scholar] [CrossRef]
- Kripalani, S.; Theobald, C.; Anctil, B.; Vasilevskis, E. Reducing Hospital Readmission Rates: Current Strategies and Future Directions. Annu. Rev. Med. 2014, 65, 471–485. [Google Scholar] [CrossRef]
- Coleman, E.; Parry, C.; Chalmers, S.; Min, S. The care transitions intervention: Results of a randomized controlled trial. Arch. Intern. Med. 2006, 166, 1822–1828. [Google Scholar] [CrossRef]
- Tomlinson, J.; Cheong, V.-L.; Fylan, B.; Silcock, J.; Smith, H.; Karban, K.; Blenkinsopp, A. Successful care transitions for older people: A systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing 2020, 49, 558–569. [Google Scholar] [CrossRef]
- Bland, M.; Stevens, A.; Nellis, P.; Mueggenburg, K.; Yau, T.; ChenJustin, C. Interprofessional education and transitions of care: A case-based educational pilot experience. J. Interprof. Care 2020, 35, 482–486. [Google Scholar] [CrossRef]
- Spasova, S.; Baeten, R.; Coster, S.; Ghailani, D.; Peña-Casas, R.; Vanhercke, B. Challenges in Long-Term Care in Europe. A Study of National Policies; European Social Policy Network (ESPN) Project KE-01-18-637-EN-N; European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Meador, R.; Chen, E.; Schultz, L.; Norton, A.; Henderson, C.; Pillemer, K. Going Home: Identifying and Overcoming Barriers to Nursing Home Discharge. Care Manag. J. 2011, 12, 2–11. [Google Scholar] [CrossRef]
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.; Ginsburg, A. Impact of mHealth Chronic Disease Management on Treatment Adherence and Patient Outcomes: A Systematic Review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef]
- Hanlon, P.; Daines, L.; Campbell, C.; McKinstry, B.; Weller, D.; Pinnock, H. Telehealth Interventions to Support Self-Management of Long-Term Conditions: A Systematic Metareview of Diabetes, Heart Failure, Asthma, Chronic Obstructive Pulmonary Disease, and Cancer. J. Med. Internet Res. 2017, 19, e172. [Google Scholar] [CrossRef]
- Pires, G.; Lopes, A.; Correia, P.; Almeida, L.; Oliveira, L.; Panda, R.; Jorge, D.; Mendes, D.; Dias, P.; Gomes, N.; et al. Usability of a telehealth solution based on TV interaction for the elderly: The VITASENIOR-MT case study. Univers. Access Inf. Soc. 2022. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wieczorek, E.; Kocot, E.; Evers, S.; Sowada, C.; Pavlova, M. Key Care Provision Aspects That Affect Care Transition in the Long-Term Care Systems: Preliminary Review Findings. Int. J. Environ. Res. Public Health 2022, 19, 6402. https://doi.org/10.3390/ijerph19116402
Wieczorek E, Kocot E, Evers S, Sowada C, Pavlova M. Key Care Provision Aspects That Affect Care Transition in the Long-Term Care Systems: Preliminary Review Findings. International Journal of Environmental Research and Public Health. 2022; 19(11):6402. https://doi.org/10.3390/ijerph19116402
Chicago/Turabian StyleWieczorek, Estera, Ewa Kocot, Silvia Evers, Christoph Sowada, and Milena Pavlova. 2022. "Key Care Provision Aspects That Affect Care Transition in the Long-Term Care Systems: Preliminary Review Findings" International Journal of Environmental Research and Public Health 19, no. 11: 6402. https://doi.org/10.3390/ijerph19116402
APA StyleWieczorek, E., Kocot, E., Evers, S., Sowada, C., & Pavlova, M. (2022). Key Care Provision Aspects That Affect Care Transition in the Long-Term Care Systems: Preliminary Review Findings. International Journal of Environmental Research and Public Health, 19(11), 6402. https://doi.org/10.3390/ijerph19116402






