1. Introduction
Finding, understanding, appraising and applying health information—behaviors associated with having adequate health literacy—are a necessity for improving and maintaining one’s health. This becomes particularly important during pregnancy, as pregnant women have great impact on their own health and that of their unborn child. During this period, women need to possess adequate health literacy to support a healthy lifestyle during this new and challenging time period.
Pregnant women can influence the health of their unborn child through a process referred to as perinatal programming, particularly by adapting their lifestyle. More precisely, unhealthy behavior, which leads for example to excessive weight gain during pregnancy, also influences the health and growth of the unborn child. Evidence suggests that a woman’s excessive weight gain during pregnancy results in higher odds of the unborn infant developing overweightness, obesity or a chronic condition later in life [
1,
2,
3,
4]. In light of this association, it is desirable that pregnant women adhere to healthy lifestyles. Since health literacy levels are closely related to health behaviors [
5,
6], it is important that pregnant women are supported regarding their health literacy. Studies indicate for example, that pregnant women with inadequate health literacy are more likely to make unhealthy lifestyle choices, have more hospital stays and engage less in prenatal care [
5,
7,
8].
There is little evidence regarding the health literacy levels of pregnant women in Germany. Studies from a recent international systematic review reported mixed findings, with some studies indicating that health literacy among pregnant women was adequate, while others indicated it was inadequate [
9]. Nonetheless, researchers are in agreement that adequate health literacy during pregnancy facilitates a healthy lifestyle [
6], informed decision making, and knowledge concerning prenatal tests [
10,
11].
In order to achieve adequate health literacy, interventions with a particular focus on strengthening health literacy are needed. Previous research indicates that health literacy sensitive interventions, by enhancing knowledge on the matter at hand, can be effective in improving health literacy, and are also beneficial in the promotion of a healthy lifestyle [
12], regardless of the educational level. To date, there exist only a small number of interventions that focus specifically on the improvement of health literacy in pregnant women [
13]. The GeMuKi (acronym for “Gemeinsam Gesund: Vorsorge plus für Mutter und Kind”—Strengthening health promotion: enhanced check-up visits for mother and child) intervention consists of brief lifestyle counseling sessions with a focus on pregnancy related topics. The counseling sessions are implemented into routine prenatal check-ups [
14]. The intervention is aimed at strengthening health literacy among pregnant women. The purpose of this study is to assess the status quo with regard to health literacy levels of pregnant women enrolled in the GeMuKi trial, and to evaluate whether the GeMuKi intervention improved health literacy levels [
15].
2. Materials and Methods
2.1. Study Design
Health literacy was assessed within the GeMuKi trial, a lifestyle intervention implemented between October 2017 and March 2022. The cluster-randomized controlled trial took place in ten regions in the state of Baden-Wuerttemberg, Germany. Five of the regions provided the intervention while the other five provided regular care. The intervention, which took the form of brief counseling sessions, took place over the course of up to six check-ups during pregnancy. It was provided by gynecologists and midwives, in case the women opted for midwifery care. The primary outcome was the prevention of excessive gestational weight gain during pregnancy. The secondary outcomes were the improvement of maternal and infant health outcomes, and improved health literacy. This paper focuses particularly on health literacy; the publication of results of the primary outcome and other secondary outcomes are in progress. A detailed description of the general design of the GeMuKi Project can be found elsewhere [
14,
15].
2.2. The GeMuKi Intervention
The GeMuKi intervention consists of brief lifestyle counseling sessions implemented as part of routine check-ups during pregnancy. Participants in the intervention group received additional counseling as part of their antenatal care, while the control group received care as usual. Participants of both groups filled in one paper-based questionnaire at baseline, and further questionnaires using an app developed for the purpose of the study.
2.3. Health Literacy Strengthening Components
The GeMuKi intervention aims to strengthen the health literacy of pregnant women by actively involving them in brief lifestyle counseling. The women decided for themselves which lifestyle topic they would like to receive counseling on, thus promoting participation that is key to improving health literacy [
16]. The topics were recommended by the ‘Healthy Start—Young Family Network’ (Netzwerk Gesund ins Leben), which is a national network that aims to promote a healthy lifestyle during pregnancy. Its recommendations are based on systematic reviews [
17]. Prior to the start of the intervention, the healthcare providers received training on communicating the key messages from the recommendations using motivation interviewing (MI) techniques [
18]. Since the primary outcome of the study was gestational weight gain, this was the main focus of the training content. MI is based on the notion that individuals will change their behavior autonomously, which is considered a health literacy skill [
19]. During the counseling sessions, healthcare providers listened to the information needs of the women and communicated using open-ended questions in order to trigger behavior change. This is in line with the ‘German Action Plan Health Literacy’, which states that healthcare providers should communicate sensitively according to the health literacy status of the patient in order to respond appropriately and strengthen the patient’s health literacy [
16]. At the end of the counseling session, the healthcare provider and the patient jointly came up with SMART (Specific, Measurable, Achievable, Reasonable, Time-Bound) lifestyle goals to be accomplished by the next counseling session. This ensured that the SMART goals were individual and tailored to the particular health literacy levels of the women in question.
In addition to the counseling, the intervention also made use of digital components to promote health literacy as recommended by the action plan [
16]. The GeMuKi-App provided the women participating in the intervention with a collection of hyperlinks related to health information on pregnancy. The app is easy to use, making it accessible for women with different health literacy and education levels. The participants also filled in questionnaires on health literacy using the app. The healthcare providers were provided with a digital interface, the GeMuKi-Assist counseling tool. The tool included supporting questions on each lifestyle topic for the healthcare providers to refer back to during counseling. In order to ensure that they were aligned with the health literacy levels of the respective women, these supporting questions were based on the principles of MI, i.e., they were open-ended questions that would trigger communication on the part of the woman in question. The healthcare providers entered the jointly agreed SMART goals into GeMuKi-Assist, after which they were displayed in the woman’s app in the form of push notifications.
2.4. Sample and Recruitment
Gynecologists participating in the GeMuKi trial recruited eligible pregnant women based on predefined inclusion and exclusion criteria. The women were deemed eligible if they were ≥18 years old, <12 weeks of gestation, carried statutory health insurance and possessed proficient language skills in German. The sample size was calculated based on the primary outcome of the GeMuKi study, for which a sample size of 1860 participants was required [
14].
2.5. Ethical Approval
GeMuKi was approved by the ethics committee of the University Hospital of Cologne (ID: 18-163) and the State Chamber of Physicians in Baden-Wuerttemberg (ID: B-F-2018-100). Inference to study participants is not possible since the collected data is pseudonymized in accordance with the EU General Data Protection Regulation (GDPR). Written informed consent was obtained prior to participation in the study. The participants were reassured that they were free to withdraw from the study at any time without consequences.
2.6. Data Collection
The data for the analysis in this paper were derived from two sources. The women filled in a paper-based questionnaire at baseline (before the 12th week of gestation) in order to provide demographic variables. Data regarding health literacy and knowledge of pregnancy related lifestyle topics were collected using questionnaires via the app.
2.7. Health Literacy Assessment
Health literacy was assessed using two questionnaires. The German version of the HLS-EU-16 was utilized at baseline (t0) to provide a detailed picture of the health literacy level distribution of the pregnant women in our sample compared to the general population.
The HLS-EU-16 is based on the health literacy definition of Sørensen et al. (2012), which is based on a broad conceptualization of health literacy, including functional and critical health literacy.
The participants were asked to answer questions on a 5-point Likert scale (‘Very difficult’–‘Very easy’; ‘I don’t know’). Since paper-based questionnaires also allow individuals to skip questions, we added the option ‘I do not want to answer this question’ to the app-based survey.
In order to observe changes in health literacy levels after the intervention, we utilized a modified version of the Brief Health Literacy Screener (BHLS). This likewise allowed participants to answer questions on a 5-point Likert scale ranging from ‘Never’ to ‘Always’. We also added ‘I do not want answer this question’ as an option. This questionnaire was used both at baseline (t0) and at the end of the pregnancy (t1).
Since the HLS-EU-16 and BHLS are both subjective health literacy measures which gauge general health literacy skills, we developed a knowledge-based questionnaire to provide objective estimates of pregnancy related health literacy [
20,
21]. The questionnaire was developed based on the topics from the national recommendations discussed during counseling. They cover: weight development during pregnancy, portion size, nutrition, alcohol consumption, smoking, physical activity, water intake and breast feeding. The questionnaire was applied at two time points, namely t0 and t1. The answering scale was ‘Yes/No/I don’t know’. A detailed description of this questionnaire can be found in the
Supplementary Table S1 while the baseline results can be found elsewhere [
20].
2.8. Data Analysis
Plausibility checks for the data were performed throughout data collection and prior to analysis. Descriptive statistics were used to analyze participant characteristics. Age, parity (nullipara), net income, migration background and educational level were used as independent variables in multiple regression analysis. Age was defined as a continuous variable. Nullipara and migration background were defined as dichotomous variables (Yes/No). Net income was calculated as a continuous variable. Education level was used as an ordinal variable. Percentages are provided for categorical variables and means for continuous variables.
The HLS-EU-16 was analyzed based on official recommendations [
22]: First, the individual items of the HLS-EU-16 were binarized by collapsing the two outer answer categories (“Very easy”/“Fairly easy” = 1; “Fairly difficult”/“Very difficult” = 0). Once this had been done, a sum score was calculated using the 16 binarized items. Respondents with more than two missing answers were excluded from the sum score calculation. The sum score was categorized into three health literacy levels: Adequate (score 13–16), Problematic (score 9–12) and Inadequate (score 1–8). This allowed for a display of the status quo with regard to health literacy level among pregnant women in accordance with prior population-based surveys in Germany and international studies [
23,
24,
25].
The BHLS is a three-item questionnaire designed to assess health literacy status by asking about confidence using health-related forms [
26]. Answers can be given on a 5-point Likert scale ranging from ‘Never’ to ‘Always’. Scores can range from 5 to 15 points. Means are provided as a classification of health literacy.
To answer the question of whether the GeMuKi intervention improved the general health literacy of pregnant women, multiple regression models using general estimation equations (GEE) were used to account for the cluster structure of the study. This GEE included the deviation (Δ) of the BHLS sum score between the two time points (BHLS sum score at t1—BHLS sum score at t0) as a continuous dependent variable and group (intervention group = 1, control group = 0) as an independent variable adjusted for age, nullipara, income, migration background and education level (covariates). To answer the question of whether the GeMuKi intervention improved specific pregnancy related and knowledge-based health literacy, a second GEE model was tested using the same independent variables and covariates and the deviation of the knowledge questionnaire sum score between the two time points (knowledge sum score at t1—knowledge sum score at t0) as the dependent variable. The sum score was calculated by adding the number of correct answers for every single question [
20]. Since health literacy was a secondary outcome of the cluster randomized controlled trial, no imputations were conducted. A
p-value of <0.05 indicated statistical significance.
All the analyses were conducted using IBM® SPSS® Statistics for Windows, Version 28.0 (Chicago, IL, USA).
3. Results
The mean age of the study participants was 31; half of the study population did not have any children at the time of participation (50%). The mean household net income was EUR 4293 per month. More than half of the pregnant women had a university degree (55.1%) and 22.7% came from a migration background (
Table 1).
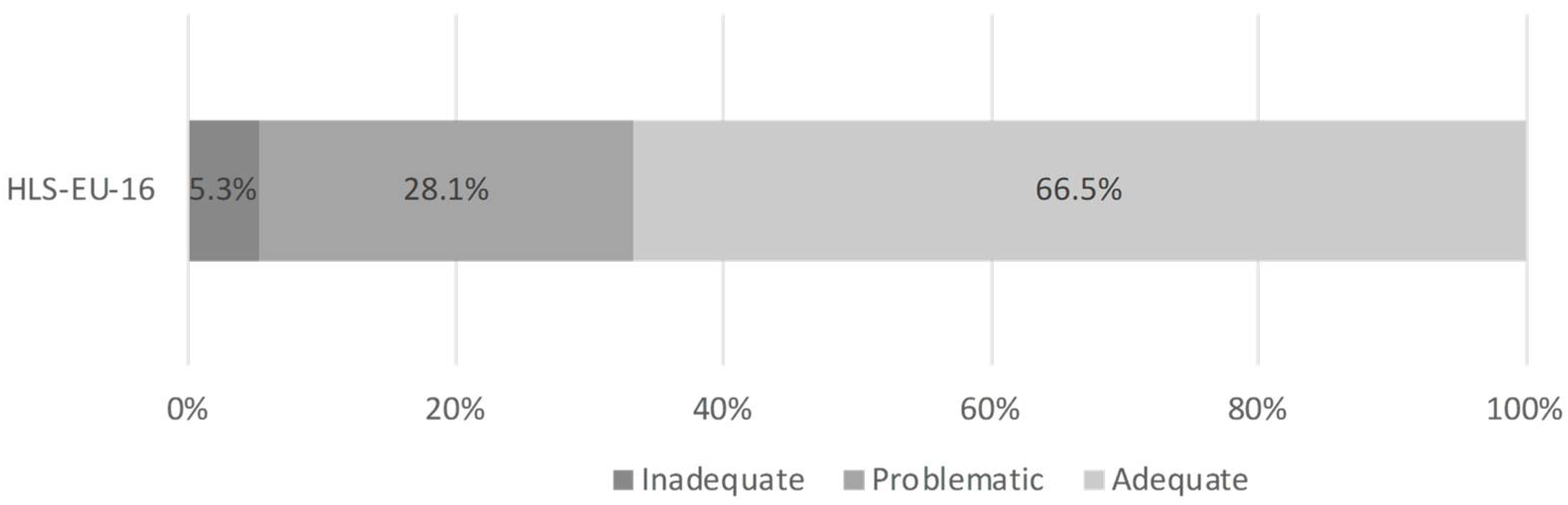
Health literacy levels in the GeMuKi study population were adequate, with 66.5% (n = 908) of the sample possessing adequate health literacy. Around one third of the women who participated in the study possessed inadequate (5.3%; n = 73) or problematic (28.1%; n = 384) health literacy (
Figure 1). Descriptive analysis of the BHLS revealed that participants had a mean score of 13.56 (n = 1373) at t0, and 13.54 at t1 (n = 1175).
Multivariable regression analysis using the BHLS as the dependent variable did not show any intervention effects on the improvement of health literacy (ß = 0.086, 95% CI [−0.016–0.187]) (
Table 2). No significant association was observed for the covariates age (ß = 0.000, 95% CI [−0.035–0.036]), migration (ß = −0.127, 95% CI [−0.366–0.112]), income (ß = 5.676, 95% CI [−2.583–3.718]), education (ß = −0.034, 95% CI [−0.089–0.021]) or parity (ß = 0.061, 95% CI [−0.072–0.194]).
Table 3 displays the GEE using Δ knowledge as the dependent variable. It was possible to observe a significant positive effect of the intervention on knowledge in the intervention group (ß = 0.089, 95% CI [0.024–0.154]). The only other significant association was seen with parity indicating that knowledge gain was predicted by giving birth for the first time (ß = 0.160, 95% CI [0.059–0.261]).
4. Discussion
This study is the first to our knowledge that provides data on the status quo for health literacy among pregnant women in Germany and assesses whether a lifestyle intervention during pregnancy improved general or pregnancy related health literacy levels.
The first point to note is that the analysis of the HLS-EU-16 indicates that about 33% of the pregnant women had inadequate or problematic health literacy, and more than two thirds of the pregnant women had sufficient health literacy right at the initiation of the GeMuKi trial. This is above average when compared to national and international studies on health literacy. A repeated representative study using the HLS-EU-16 in Germany from 2021 demonstrated that 59% of the population have problematic or inadequate health literacy [
24], which is a decline of about five percentage points to 54% compared to 2016 [
23]. The same holds true for data on the female population from the 2021 study, in which around 57% of the study participants possessed inadequate health literacy.
The comparatively high baseline health literacy levels among the trial participants were not surprising considering that the study population was highly educated, which is strongly associated with health literacy [
19], in comparison to the general population. Several explanations as to why our population was highly educated may apply in this case. The region in which the study took place ranks highly in national comparisons of educational achievements, making it likely that more educated women would participate in the study. It is possible that some women with migration backgrounds were not recruited by healthcare providers for the study due to insufficient language skills, which rules out one important vulnerable group. The inclusion criteria for participation in the study were set broadly; however, the choice of which women to include in the study was left to the gynecologists, which might have led to selection bias. This might also provide an explanation as to why we had so few women with a migration background in the study sample compared to the general population. Such women might have been excluded due to language barriers or because healthcare providers did not perceive them as eligible.
Multiple regression analysis using GEE did not show significant results regarding the question of whether this lifestyle intervention improved general health literacy. There are several explanations for why the intervention was not effective. Firstly, this again may be a result of the highly educated nature of the study population and the high initial levels of health literacy in both the intervention and control groups. Secondly, since it only contains three items, the BHLS does not offer a broad picture of health literacy. This could have been avoided by applying the HLS-EU-16 with 16 items at t1 as well as t0. For future studies we therefore highly recommend using a more detailed health literacy instrument. Thirdly, the intervention was not geared to general health literacy, which is measured using HLS-EU-16 and the BHLS. Therefore, the utilized instruments may have not been suitable. To depict pregnancy specific health literacy, we have developed a knowledge-based questionnaire. Fourthly, regarding the training the healthcare providers received, it can be argued that they might not have been educated well enough in the use of MI techniques which were supposed to be health literacy sensitive. It should be added that the content of the training mainly focused on the primary outcome of the intervention, which was gestational weight gain, rather than health literacy. The implementation of the counseling was not monitored, so we cannot assume that all the steps were conducted as taught in the training sessions. Lastly, we might have not met the needs of women with inadequate health literacy in our population. This can indicate that the intervention was not appropriate for that proportion of women.
According to the results of the GEE, the intervention was effective in improving the knowledge of pregnancy related lifestyles of women in the intervention group. The assessment of knowledge change in our study may have been successful as we developed a pregnancy specific health literacy instrument. The contents of the questionnaire were based on topics that the women received counseling on. This again speaks for the utilization of appropriate instruments for future studies, or that interventions are built based on the theoretical construct of the questionnaire, such as the HLS-EU-16.
The fact that the counseling helped pregnant women gain knowledge on pregnancy specific lifestyle topics can be seen as an argument in its favor. Scholars in the German healthcare setting support the provision of health information in the antenatal setting through gynecologists to improve pregnancy related lifestyle knowledge, since it has the potential to reach women of different socio-demographic status [
27]. Counseling becomes particularly important regarding significant results for women that are going to be first-time mothers, as they are new to the experience of being pregnant and potentially need counseling on lifestyle during pregnancy.
Studies indicate that educational interventions to improve knowledge on pregnancy specific topics are effective; however, the transition from knowledge to behavior still requires research [
28,
29]. Small scaled interventions, on the other hand, already show promising results in improving knowledge of physical activity and nutrition, and hence improving behavior [
30]. Similarly, interventions (also in the form of counseling) to reduce the risk of gestational weight gain were proven effective [
31,
32].
5. Conclusions
This study indicates that most women participating in a lifestyle intervention trial in Germany possessed adequate health literacy in our study population. Nevertheless, pregnant women with inadequate health literacy, who still make up about one third of the study population, should not be neglected, due to the effects that limited health literacy can have on the woman’s health and that of their unborn child. The intervention was not able to improve general health literacy; this may be due to several determinants. The women included in our study possess both high levels of education and adequate health literacy. The needs of women with inadequate health literacy might not have been met, which might stem from the training that the healthcare providers received which did not consider different health literacy-based subgroups of women. The main focus of the training was on the primary outcome of the study, the prevention of excessive gestational weight gain. Nevertheless, the study had a significant positive effect on knowledge levels, which provides strong support for providing additional lifestyle counseling during pregnancy, especially for first-time mothers.
Future interventions might benefit from a comprehensive approach to measuring health literacy throughout the study period, rather than using short screeners. Additionally, approved communication methods for increasing health literacy need to be an inherent part of counseling.
Author Contributions
Conceptualization, F.N.; formal analysis, F.N. and A.S.; writing—original draft preparation, F.N.; writing—review and editing, A.A., F.K., L.L. and S.S.; supervision, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study is funded by the Innovation Fund of the Federal Joint Committee (G-BA), Module 3: Improving communication with patients and promoting health literacy (Project No. 01NVF17014).
Institutional Review Board Statement
Ethical approval was obtained from the University Hospital of Cologne Research Ethics Committee (ID: 18-163) and the State Chamber of Physicians in Baden-Wuerttemberg (ID: B-F-2018-100). The study data will only be processed in a pseudonymized form in accordance with the EU General Data Protection Regulation (GDPR).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Acknowledgments
This work was carried out by a consortium of five partners: Plattform Ernährung und Bewegung, Institut für Gesundheitsökonomie und Klinische Epidemiologie Universitätsklinikum Köln, Fraunhofer Institut für Offene Kommunikationssysteme FOKUS, BARMER and Kassenärztliche Vereinigung Baden-Wuerttemberg. The authors would like to thank all participating practices, gynecologists, pediatricians, medical assistants, midwives, pregnant women and their families for their involvement. We would like to extend our deep thanks to Isabel Lück, Judith Kuchenbecker, Andrea Moreira, Andrea Seifarth, Elena Tschiltschke, Denise Torricella, and Hilke Friesenborg, who coordinated the study in the study regions in Baden-Wuerttemberg and provided essential support for data management in the field and Anne-Madeleine Bau, GeMuKi project leader, who coordinated the consortium. We would also like to thank Brigitte Neumann and Sonja Eichin for developing and conducting the training in all intervention regions. Furthermore, we acknowledge Stefan Klose, Christian Giertz, Benny Häusler and Michael John for developing and operating all digital intervention components. In addition, we would like to extend our thanks to Karsten Menn, Tobias Weigel, Rüdiger Kucher and Simone Deininger for their help with legal and contractual aspects of the project. We also acknowledge the members of the scientific advisory committee: Hans Hauner, Joachim Dudenhausen, Liane Schenk, Julika Loss and Andrea Lambeck. We also thank Arim Shukri for his assistance with the statistical analyses. Additionally, we would like to thank the following partners who have had an essential role in the success of the GeMuKi project: Gesund ins Leben—Netzwerk Junge Familie, Berufsverband der Kinder- und Jugendärzte, Berufsverband der Frauenärzte, Hebammenverband Baden-Wuerttemberg, Landesärztekammer Baden-Wuerttemberg, Universität Freiburg, AOK Baden-Wuerttemberg, Techniker Krankenkasse and all other health insurers participating in the project through GWQ Service Plus. Furthermore, we would like to thank Cornelia Wäscher for her contribution to the grant proposal. Finally, we gratefully acknowledge Thomas Kauth and Ulrike Korsten-Reck for contributing to the initial project idea and for their support during the implementation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Woo Baidal, J.A.; Locks, L.M.; Cheng, E.R.; Blake-Lamb, T.L.; Perkins, M.E.; Taveras, E.M. Risk Factors for Childhood Obesity in the First 1000 Days: A Systematic Review. Am. J. Prev. Med. 2016, 50, 761–779. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wu, Y.; Li, S.; Zhang, D. Maternal prepregnancy obesity and the risk of shoulder dystocia: A meta-analysis. BJOG Int. J. Obstet. Gynaecol. 2018, 125, 407–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torloni, M.R.; Betran, A.P.; Horta, B.L.; Nakamura, M.U.; Atallah, A.N.; Moron, A.F.; Valente, O. Prepregnancy BMI and the risk of gestational diabetes: A systematic review of the literature with meta-analysis. Obes. Rev. 2009, 10, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Meehan, S.; Beck, C.R.; Mair-Jenkins, J.; Leonardi-Bee, J.; Puleston, R. Maternal obesity and infant mortality: A meta-analysis. Pediatrics 2014, 133, 863–871. [Google Scholar] [CrossRef]
- Lupattelli, A.; Picinardi, M.; Einarson, A.; Nordeng, H. Health literacy and its association with perception of teratogenic risks and health behavior during pregnancy. Patient Educ. Couns. 2014, 96, 171–178. [Google Scholar] [CrossRef]
- Sahin, E.; Yesilcinar, I.; Geris, R.; Pasalak, S.I.; Seven, M. The impact of pregnant women’s health literacy on their health-promoting lifestyle and teratogenic risk perception. Health Care Women Int. 2021, 42, 598–610. [Google Scholar] [CrossRef]
- Smedberg, J.; Lupattelli, A.; Mardby, A.C.; Nordeng, H. Characteristics of women who continue smoking during pregnancy: A cross-sectional study of pregnant women and new mothers in 15 European countries. BMC Pregnancy Childbirth 2014, 14, 213. [Google Scholar] [CrossRef] [Green Version]
- Endres, L.K.; Sharp, L.K.; Haney, E.; Dooley, S.L. Health literacy and pregnancy preparedness in pregestational diabetes. Diabetes Care 2004, 27, 331–334. [Google Scholar] [CrossRef] [Green Version]
- Nawabi, F.; Krebs, F.; Vennedey, V.; Shukri, A.; Lorenz, L.; Stock, S. Health Literacy in Pregnant Women: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3847. [Google Scholar] [CrossRef]
- van Schendel, R.V.; Page-Christiaens, G.C.; Beulen, L.; Bilardo, C.M.; de Boer, M.A.; Coumans, A.B.; Faas, B.H.; van Langen, I.M.; Lichtenbelt, K.D.; van Maarle, M.C.; et al. Trial by Dutch laboratories for evaluation of non-invasive prenatal testing. Part II-women’s perspectives. Prenat. Diagn. 2016, 36, 1091–1098. [Google Scholar] [CrossRef]
- Yee, L.M.; Wolf, M.; Mullen, R.; Bergeron, A.R.; Cooper Bailey, S.; Levine, R.; Grobman, W.A. A randomized trial of a prenatal genetic testing interactive computerized information aid. Prenat. Diagn. 2014, 34, 552–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osborn, C.Y.; Paasche-Orlow, M.K.; Bailey, S.C.; Wolf, M.S. The mechanisms linking health literacy to behavior and health status. Am. J. Health Behav. 2011, 35, 118–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zibellini, J.; Muscat, D.M.; Kizirian, N.; Gordon, A. Effect of health literacy interventions on pregnancy outcomes: A systematic review. Women Birth J. Aust. Coll. Midwives 2021, 34, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Alayli, A.; Krebs, F.; Lorenz, L.; Nawabi, F.; Bau, A.M.; Luck, I.; Moreira, A.; Kuchenbecker, J.; Tschiltschke, E.; John, M.; et al. Evaluation of a computer-assisted multi-professional intervention to address lifestyle-related risk factors for overweight and obesity in expecting mothers and their infants: Protocol for an effectiveness-implementation hybrid study. BMC Public Health 2020, 20, 482. [Google Scholar] [CrossRef] [Green Version]
- Nawabi, F.; Alayli, A.; Krebs, F.; Lorenz, L.; Shukri, A.; Bau, A.M.; Stock, S. Health literacy among pregnant women in a lifestyle intervention trial: Protocol for an explorative study on the role of health literacy in the perinatal health service setting. BMJ Open 2021, 11, e047377. [Google Scholar] [CrossRef]
- Schaeffer, D.; Hurrelmann, K.; Bauer, U.; Kolpatzik, K. National Action Plan Health Literacy. Promoting Health Literacy in Germany; KomPart: Berlin, Germany, 2018. [Google Scholar]
- Koletzko, B.; Cremer, M.; Flothkotter, M.; Graf, C.; Hauner, H.; Hellmers, C.; Kersting, M.; Krawinkel, M.; Przyrembel, H.; Robl-Mathieu, M.; et al. Diet and Lifestyle Before and During Pregnancy—Practical Recommendations of the Germany-wide Healthy Start—Young Family Network. Geburtshilfe Frauenheilkd 2018, 78, 1262–1282. [Google Scholar] [CrossRef] [Green Version]
- Miller, W.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Sorensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [Green Version]
- Nawabi, F.; Krebs, F.; Lorenz, L.; Shukri, A.; Alayli, A.; Stock, S. Understanding Determinants of Pregnant Women’s Knowledge of Lifestyle-Related Risk Factors: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 658. [Google Scholar] [CrossRef]
- Liu, C.; Wang, D.; Liu, C.; Jiang, J.; Wang, X.; Chen, H.; Ju, X.; Zhang, X. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam. Med. Community Health 2020, 8, e000351. [Google Scholar] [CrossRef]
- Jordan, S.; Hoebel, J. Health literacy of adults in Germany: Findings from the German Health Update (GEDA) study. Bundesgesundheitsblatt Gesundh. Gesundh. 2015, 58, 942–950. [Google Scholar] [CrossRef]
- Schaeffer, D.; Berens, E.M.; Vogt, D. Health Literacy in the German Population. Dtsch. Arztebl. Int. 2017, 114, 53–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaeffer, D.; Berens, E.M.; Gille, S.; Griese, L.; Klinger, J.; de Sombre, S.; Vogt, D.; Hurrelmann, K. Gesundheitskompetenz der Bevölkerung in Deutschland vor und Während der Corona Pandemie: Ergebnisse des HLS-GER 2; Bielefeld University: Bielefeld, Germany, 2021. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chew, L.D.; Bradley, K.A.; Boyko, E.J. Brief questions to identify patients with inadequate health literacy. Fam. Med. 2004, 36, 588–594. [Google Scholar] [PubMed]
- Oechsle, A.; Wensing, M.; Ullrich, C.; Bombana, M. Health Knowledge of Lifestyle-Related Risks during Pregnancy: A Cross-Sectional Study of Pregnant Women in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8626. [Google Scholar] [CrossRef]
- Chivu, C.M.; Tulchinsky, T.H.; Soares-Weiser, K.; Braunstein, R.; Brezis, M. A systematic review of interventions to increase awareness, knowledge, and folic acid consumption before and during pregnancy. Am. J. Health Promot. 2008, 22, 237–245. [Google Scholar] [CrossRef]
- McDonald, S.D.; Park, C.K.; Pullenayegum, E.; Bracken, K.; Sword, W.; McDonald, H.; Neupane, B.; Taylor, V.H.; Beyene, J.; Mueller, V.; et al. Knowledge translation tool to improve pregnant women’s awareness of gestational weight gain goals and risks of gaining outside recommendations: A non-randomized intervention study. BMC Pregnancy Childbirth 2015, 15, 105. [Google Scholar] [CrossRef] [Green Version]
- Cavenagh, Y.; Simerson, D. A Lifestyle Intervention Program to Improve Knowledge and Health Behaviors in Women. Nurs. Women’s Health 2022, 26, 51–62. [Google Scholar] [CrossRef]
- Rauh, K.; Gabriel, E.; Kerschbaum, E.; Schuster, T.; von Kries, R.; Amann-Gassner, U.; Hauner, H. Safety and efficacy of a lifestyle intervention for pregnant women to prevent excessive maternal weight gain: A cluster-randomized controlled trial. BMC Pregnancy Childbirth 2013, 13, 151. [Google Scholar] [CrossRef] [Green Version]
- Chan, C.W.H.; Au Yeung, E.; Law, B.M.H. Effectiveness of Physical Activity Interventions on Pregnancy-Related Outcomes among Pregnant Women: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 1840. [Google Scholar] [CrossRef] [Green Version]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).