Progressive Changes in Lumbopelvic Alignment during the Three Month-Postpartum Recovery Period
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
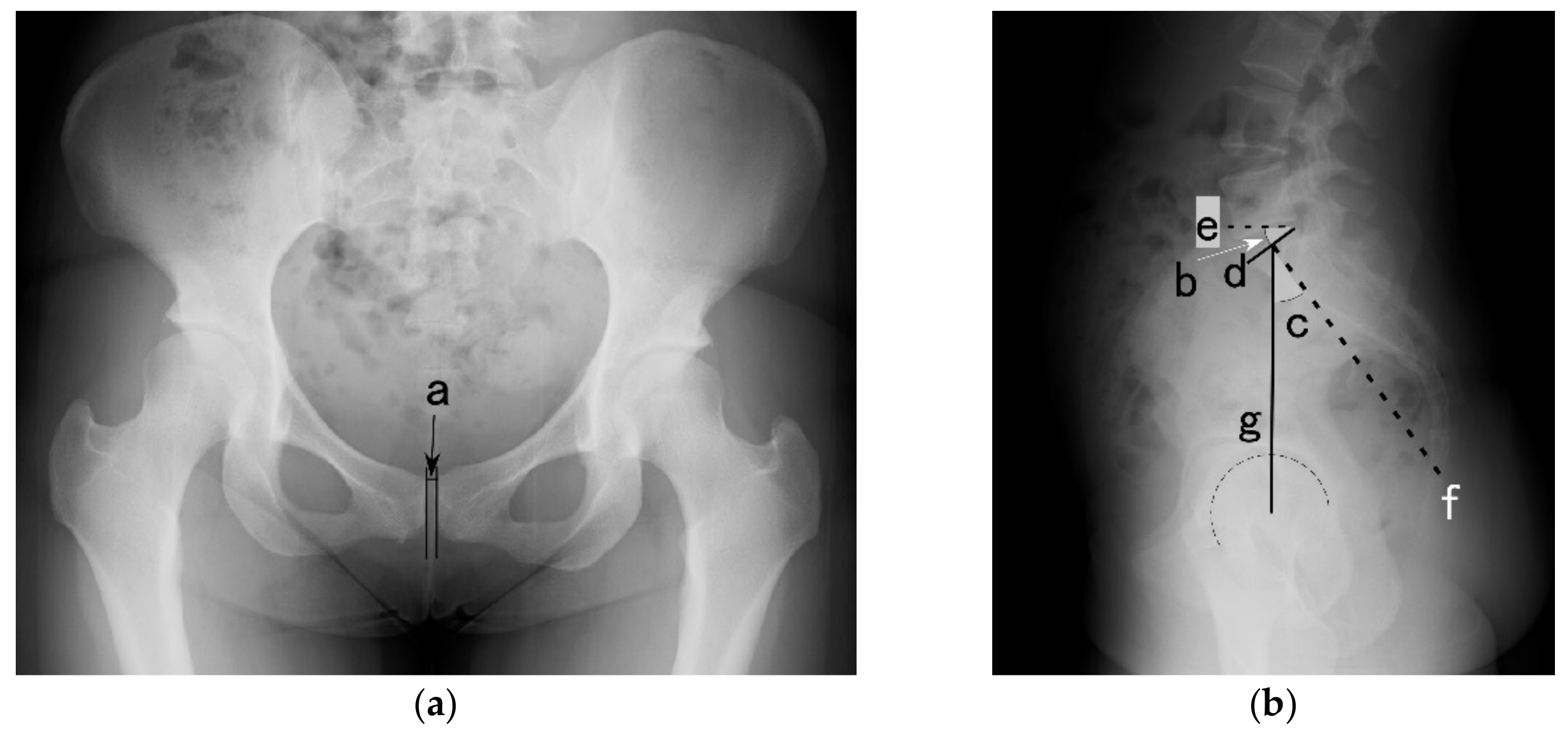
2.2. X-ray Assessment
2.3. Curl-Up Performance
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, W.H.; Meijer, O.G.; Uegaki, K.; Mens, J.M.; van Dieen, J.H.; Wuisman, P.I.; Ostgaard, H.C. Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur. Spine J. 2004, 13, 575–589. [Google Scholar] [CrossRef] [PubMed]
- Vleeming, A.; Albert, H.B.; Ostgaard, H.C.; Sturesson, B.; Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J. 2008, 17, 794–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aldabe, D.; Milosavljevic, S.; Bussey, M.D. Is pregnancy related pelvic girdle pain associated with altered kinematic, kinetic and motor control of the pelvis? A systematic review. Eur. Spine J. 2012, 21, 1777–1787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damen, L.; Buyruk, H.M.; Guler-Uysal, F.; Lotgering, F.K.; Snijders, C.J.; Stam, H.J. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet. Gynecol. Scand. 2001, 80, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Verstraete, E.H.; Vanderstraeten, G.; Parewijck, W. Pelvic Girdle Pain during or after Pregnancy: A review of recent evidence and a clinical care path proposal. Facts Views Vis. ObGyn 2013, 5, 33–43. [Google Scholar] [PubMed]
- Aldabe, D.; Ribeiro, D.C.; Milosavljevic, S.; Dawn Bussey, M. Pregnancy-related pelvic girdle pain and its relationship with relaxin levels during pregnancy: A systematic review. Eur. Spine J. 2012, 21, 1769–1776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Catena, R.D.; Campbell, N.; Wolcott, W.C.; Rothwell, S.A. Anthropometry, standing posture, and body center of mass changes up to 28 weeks postpartum in Caucasians in the United States. Gait Posture 2019, 70, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Morino, S.; Ishihara, M.; Umezaki, F.; Hatanaka, H.; Yamashita, M.; Aoyama, T. Pelvic alignment changes during the perinatal period. PLoS ONE 2019, 14, e0223776. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S.; Bakar, R.Z.; Aydin, C.A.; Ozcan, P. Assessment of postpartum symphysis pubis distention with 3D ultrasonography: A novel method. Clin. Imaging 2016, 40, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Gilleard, W.L.; Crosbie, J.; Smith, R. Static trunk posture in sitting and standing during pregnancy and early postpartum. Arch. Phys. Med. Rehabil. 2002, 83, 1739–1744. [Google Scholar] [CrossRef] [PubMed]
- Committee Opinion No. 650 Summary: Physical Activity and Exercise during Pregnancy and the Postpartum Period. Obstet. Gynecol. 2015, 126, 1326–1327. [CrossRef]
- Legaye, J.; Duval-Beaupere, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agten, C.A.; Metzler, C.; Rosskopf, A.B.; Zanetti, M.; Binkert, C.A.; Prentl, E.; Pfirrmann, C.W.A. MR imaging of pubic symphysis after uncomplicated vaginal delivery and planned caesarean delivery in the first postpartum week. Clin. Imaging 2019, 56, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Brandon, C.; Jacobson, J.A.; Low, L.K.; Zielinski, R.; Ashton-Miller, J.; Delancey, J.O. MRI findings in patients considered high risk for pelvic floor injury studied serially after vaginal childbirth. AJR Am. J. Roentgenol. 2010, 195, 786–791. [Google Scholar] [CrossRef] [Green Version]
- Fukano, M.; Tsukahara, Y.; Takei, S.; Nose-Ogura, S.; Fujii, T.; Torii, S. Recovery of Abdominal Muscle Thickness and Contractile Function in Women after Childbirth. Int. J. Environ. Res. Public Health 2021, 18, 2130. [Google Scholar] [CrossRef]
- Gausel, A.M.; Malmqvist, S.; Andersen, K.; Kjaermann, I.; Larsen, J.P.; Dalen, I.; Okland, I. Subjective recovery from pregnancy-related pelvic girdle pain the first 6 weeks after delivery: A prospective longitudinal cohort study. Eur. Spine J. 2020, 29, 556–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Group | Postpartum | Control | |||
|---|---|---|---|---|---|
| (n = 30) | (n = 20) | ||||
| Variables | Mean | SD | Mean | SD | p-Value |
| Height (cm) | 157.6 | 4.9 | 157.6 | 4.4 | 0.98 |
| Weight (kg) *1 | 53.8 | 9.9 | 51.3 | 6.8 | 0.76 |
| Age (years) | 33.0 | 4.4 | 32.0 | 10.6 | 0.77 |
| Pelvic incidence (deg) | 51.1 | 8.8 | 46.9 | 8.7 | 0.11 |
| Group | Postpartum | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| Immediately | 1 Month | 3 Months | (n = 20) | |||||
| Variables | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Pubic symphysis width (mm) | 6.0 | 1.1 * | 5.0 | 1.2 * | 3.9 | 1.1 | 3.4 | 0.4 |
| Sacral slope (deg) | 37.8 | 5.9 | 39.9 | 6.6 * | 37.8 | 6.7 | 34.8 | 5.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukano, M.; Aisaka, K.; Nose-Ogura, S.; Fujii, T.; Torii, S. Progressive Changes in Lumbopelvic Alignment during the Three Month-Postpartum Recovery Period. Int. J. Environ. Res. Public Health 2022, 19, 5807. https://doi.org/10.3390/ijerph19105807
Fukano M, Aisaka K, Nose-Ogura S, Fujii T, Torii S. Progressive Changes in Lumbopelvic Alignment during the Three Month-Postpartum Recovery Period. International Journal of Environmental Research and Public Health. 2022; 19(10):5807. https://doi.org/10.3390/ijerph19105807
Chicago/Turabian StyleFukano, Mako, Kozo Aisaka, Sayaka Nose-Ogura, Tomoyuki Fujii, and Suguru Torii. 2022. "Progressive Changes in Lumbopelvic Alignment during the Three Month-Postpartum Recovery Period" International Journal of Environmental Research and Public Health 19, no. 10: 5807. https://doi.org/10.3390/ijerph19105807
APA StyleFukano, M., Aisaka, K., Nose-Ogura, S., Fujii, T., & Torii, S. (2022). Progressive Changes in Lumbopelvic Alignment during the Three Month-Postpartum Recovery Period. International Journal of Environmental Research and Public Health, 19(10), 5807. https://doi.org/10.3390/ijerph19105807






