Effect of an Extremely Low-Frequency Electromagnetic Field on the Concentration of Salivary Immunoglobulin A
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pasek, J.; Pasek, T.; Sieroń- Stołtny, K.; Cieślar, G.; Sieroń, A. Electromagnetic fields in medicine—The state of art. Electromagn. Biol. Med. 2016, 35, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.T.; Vanscoy-Cornett, A.; Vesper, D.N.; Swez, J.A.; Chamberlain, J.K.; Seaward, M.B.; Nindl, G. Electromagnetic fields used clinically to improve bone healing also impact lymphocyte proliferation in vitro. Biomed. Sci. Instrum. 2001, 37, 215–220. [Google Scholar] [PubMed]
- Markov, M. Magnetic field therapy. Electromagn. Biol. Med. 2007, 26, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Kopacz, Ł.; Ciosek, Ż.; Gronwald, H.; Skomro, P.; Ardan, R.; Lietz-Kijak, D. Comparative Analysis of the Influence of Selected Physical Factors on the Level of Pain in the Course of Temporomandibular Joint Disorders. Pain Res. Manag. 2020, 2020, 1036306. [Google Scholar] [CrossRef] [PubMed]
- Skomro, P.; Lietz-Kijak, D.; Kijak, E.; Bohdziewicz-Wałęsa, O.; Opalko, K. The change of electric potentials in the oral cavity after application of extremely low frequency pulsed magnetic field. Adv. Hyg. Exp. Med. 2012, 66, 991–995. [Google Scholar] [CrossRef] [PubMed]
- Opalko, K.; Dojs, A. Bone structure regeneration after low induction magnetic field treatment in teeth chosen for extraction. Adv. Med. Sci. 2006, 51 (Suppl. S1), 151–153. [Google Scholar] [PubMed]
- Lietz-Kijak, D.; Kijak, E.; Śliwiński, Z.; Opalko, K. The use of physiotherapy in the regeneration of periapical bone structures of the teeth, prepared to load the prosthetic. Adv. Hyg. Exp. Med. 2013, 67, 643–647. [Google Scholar] [CrossRef]
- Takano-Yamamoto, T.; Kawakami, M.; Sakuda, M. Effect of a pulsing electromagnetic field on demineralized bone-matrix induced bone formation in a bony defect in the premaxilla of rats. J. Dent. Res. 1992, 71, 1920–1925. [Google Scholar] [CrossRef]
- Skomro, P.; Opalko, K.; Bohdziewicz, O.; Noceń, I.; Janiszewska-Olszowska, J. Limited effect of low frequency magnetic fields on the concentrations of calcium, magnesium and fluoride in saliva. Magnes. Res. 2009, 22, 89–92. [Google Scholar] [CrossRef]
- Okokon, E.; Roivainen, P.; Kheifets, L.; Mezei, G.; Juutilainen, J. Indoor transformer stations and ELF magnetic field exposure: Use of transformer structural characteristics to improve exposure assessment. J. Exp. Sci. Environ. Epidemiol. 2014, 24, 100–104. [Google Scholar] [CrossRef]
- Wilson, B.W.; Wright, C.W.; Morris, J.E.; Buschbom, R.L.; Brown, D.P.; Miller, D.L.; Sommers-Flannigan, R.; Anderson, L.E. Evidence for an effect of ELF electromagnetic fields on human pineal gland function. J. Pineal Res. 1990, 9, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Pall, M.L. Electromagnetic fields act via activation of voltage-gated calcium channels to produce beneficial or adverse effects. J. Cell Mol. Med. 2013, 17, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Leslie, F. Distortion of twisted orientation patterns in liquid crystals by magnetic field. Mol. Cryst. Liq. Cryst. 1970, 1, 57–72. [Google Scholar] [CrossRef]
- Santini, M.T.; Rainaldi, G.; Indovina, P.L. Cellular effects of extremely low frequency (ELF) electromagnetic fields. Int. J. Radiat. Biol. 2009, 4, 294–313. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuw Amerongen, A.; Bolscher, J.G.M.; Veerman, E.C.I. Salivary proteins: Protective and diagnostic value in cariology? Caries Res. 2004, 38, 247–253. [Google Scholar] [CrossRef]
- Van Anders, S.M. Chewing gum has large effects on salivary testosterone, estradiol, and secretory immunoglobulin A assays in women and men. Psychoneuroendocrinology 2009, 15, 305–309. [Google Scholar] [CrossRef] [Green Version]
- Allgrove, J.E.; Geneen, L.; Latif, S.; Gleeson, M. Influence of a fed or fasted state on the s-IgA response to prolonged cycling in active men and women. Int. J. Sport Nutr. Exerc. Metab. 2009, 19, 209–221. [Google Scholar] [CrossRef] [Green Version]
- Davidson, G.; Allgrove, J.; Gleeson, M. Salivary antimicrobial peptides (LL-37 and alpha-defensins HNP1-3), antimicrobial and IgA responses to prolonged exercise. Eur. J. Appl. Physiol. 2009, 106, 277–284. [Google Scholar] [CrossRef]
- Kono, Y.; Kubota, A.; Taira, M.; Katsuyama, N.; Sugimoto, K. Effects of oral stimulation with capsaicin on salivary secretion and neural activities in the autonomic system and the brain. J. Dent. Sci. 2018, 13, 116–123. [Google Scholar] [CrossRef]
- Chang, C.K.; Cohen, M.E.; Bienek, D.R. Efficiency of oral fluid collection devices in extracting antibodies. Oral Microbiol. Immunol. 2009, 24, 231–235. [Google Scholar] [CrossRef]
- Wróbel, M.P.; Szymborska-Kajanek, A.; Wystrychowski, G.; Biniszkiewicz, T.; Sieroń-Słotny, K.; Sieroń, A.; Pierzchała, K.; Grzeszczak, W.; Strojek, K. Impact of low frequency pulsed magnetic fields on pain intensity, quality of life and sleep disturbances in patients with painful diabetic polyneuropathy. Diabetes Metab. 2008, 4, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.A.; Juen, N.; Théberge JWeller, J.; Drost, D.J.; Prato, F.S.; Thomas, A.W. Evidence for a dose-dependent effect of pulsed magnetic fields on pain processing. Neurosci. Lett. 2010, 2, 160–162. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.A.; Thomas, A.W.; Bureau, Y.; Prato, F.S. The influence of extremely low frequency magnetic fields of cytoprotection and repair. Bioelectromagnetics 2007, 1, 16–30. [Google Scholar] [CrossRef] [PubMed]
- Miyakoshi, J. Effects of static magnetic fields at the cellular level. Prog. Biophys. Mol. Biol. 2005, 87, 213–223. [Google Scholar] [CrossRef]
- Volpe, P. Interactions of zero-frequency and oscillating magnetic fields with biostruc-tures and biosystems. Photohem. Photobiol. Sci. 2003, 2, 637–648. [Google Scholar] [CrossRef]
- Mestecky, J.; Leu, C.; Russell, M.W. Selective transport of IgA: Cellular and molecular aspects. Gastroenterol. Clin. N. Am. 1991, 20, 441–471. [Google Scholar]
- Bachrach, G.; Muster, Z.; Raz, I.; Chaushu, G.; Stabholz, A.; Nussbaum, G.; Gutner, M.; Chaushu, S. Assessing the levels of immunoglobulins in the saliva of diabetic individuals with periodontitis using checkerboard immunodetection. Oral Dis. 2008, 14, 51–59. [Google Scholar] [CrossRef]
- Auşar, A.; Darka, Ö.; Bodrumlu, E.H.; Bek, Y. Evaluation of the relationship between passive smoking and salivary electrolytes, protein, secretory IgA, sialic acid and amylase in young children. Arch. Oral Biol. 2009, 54, 457–463. [Google Scholar] [CrossRef]
- Helenius, L.M.; Meurman, J.H.; Helenius, I.; Kari, K.; Hietanen, J.; Suuronen, R.; Hallikainen, D.; Kautiainen, H.; Leirisalo-Repo, M.; Lindqvist, C. Oral and salivary parameters in patients with rheumatic diseases. Acta Odont. Scand. 2005, 63, 284–293. [Google Scholar] [CrossRef]
- Lutovac, M.; Popova, O.V.; Macanovic, G.; Kristina, R.; Lutovac, B.; Ketin, S.; Biocanin, R. Testing the Effect of Aggressive Beverage on the Damage of Enamel Structure. Open Access Maced. J. Med. Sci. 2017, 5, 987–993. [Google Scholar] [CrossRef] [Green Version]
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers Micro-Hardness of New Restorative CAD/CAM Dental Materials: Evaluation and Comparison after Exposure to Acidic Drink. Materials 2019, 12, 1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, Z.L.; Szafrański, S.P.; Jarek, M.; Bhuju, S.; Wagner-Döbler, I. Dysbiosis in chronic periodontitis: Key microbial players and interactions with the human host. Sci. Rep. 2017, 7, 3703–3715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scribante, A.; Poggio, C.; Gallo, S.; Riva, P.; Cuocci, A.; Carbone, M.; Arciola, C.R.; Colombo, M. In Vitro Re-Hardening of Bleached Enamel Using Mineralizing Pastes: Toward Preventing Bacterial Colonization. Materials 2020, 13, 818. [Google Scholar] [CrossRef] [Green Version]
- Ikram, S.; Hassan, N.; Raffat, M.A.; Mirza, S.; Akram, Z. Systematic review and meta-analysis of double-blind, placebo- controlled, randomized clinical trials using probiotics in chronic periodontitis. J. Investig. Clin. Dent. 2018, 9, e12338. [Google Scholar] [CrossRef] [PubMed]
- Teame, T.; Wang, A.; Xie, M.; Zhang, Z.; Yang, Y.; Ding, Q.; Gao Ch Olsen, R.E.; Ran Ch Zhou, Z. Paraprobiotics and Postbiotics of Probiotic Lactobacilli, Their Positive Effects on the Host and Action Mechanisms: A Review. Front. Nutr. 2020, 7, 570344. [Google Scholar] [CrossRef] [PubMed]
- Butera, A.; Gallo, S.; Molino, C.D.; Chiesa, A.; Preda, C.; Esposito, F.; Scribante, A. Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters. Microorganisms 2021, 9, 69. [Google Scholar] [CrossRef]
- Cuevas-González, P.F.; Liceaga, A.M.; Aguilar-Toalá, J.E. Postbiotics and paraprobiotics: From concepts to applications. Food Res. Int. 2020, 136, 109502. [Google Scholar] [CrossRef]
- Nataraj, B.H.; Ali, S.A.; Behare, P.V.; Yadav, H. Postbiotics-parabiotics: The new horizons in microbial biotherapy and functional foods. Microb. Cell Fact. 2020, 19, 168. [Google Scholar] [CrossRef]



| Distribution Characteristics | Before the Treatment | After 5 Treatments | After 10 Treatments | After 15 Treatments |
|---|---|---|---|---|
| n | 24 | 24 | 24 | 24 |
| min–max | 62.5–159.0 | 85.0–159.8 | 99.0–170.2 | 122.7–190.0 |
| Q1–Q3 | 85.6–142.1 | 108.3–150.6 | 121.9–156.2 | 135.5–160.6 |
| me | 100.2 | 127.2 | 137.4 | 156.1 |
| M ± SD | 111.2 ± 31.6 | 127.9 ± 23.8 | 137.6 ± 19.5 | 151.3 ± 17.4 |
| W | 0.911 | 0.921 | 0.951 | 0.939 |
| p | <0.04 | >0.06 | >0.28 | >0.16 |
| Wilcoxon Test | 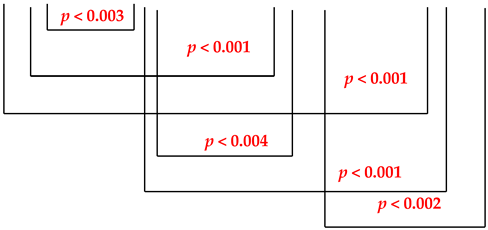 | |||
| Distribution Characteristics | 1st Examination | 2nd Examination | 3rd Examination |
|---|---|---|---|
| n | 25 | 25 | 25 |
| min–max | 72.5–170.2 | 67.8–165.3 | 70.3–160.8 |
| Q1–Q3 | 97.7–129.3 | 97.8–130.8 | 97.4–130.5 |
| me | 120.3 | 115.3 | 120.3 |
| M ± SD | 116.2 ± 27.2 | 116.5 ± 29.0 | 117.3 ± 27.0 |
| W | 0.959 | 0.954 | 0.955 |
| p | >0.41 | >0.31 | >0.33 |
| Student’s t-test |  | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skomro, P.; Lietz-Kijak, D.; Bogdziewicz-Wałęsa, O.; Janiszewska-Olszowska, J. Effect of an Extremely Low-Frequency Electromagnetic Field on the Concentration of Salivary Immunoglobulin A. Int. J. Environ. Res. Public Health 2022, 19, 5786. https://doi.org/10.3390/ijerph19105786
Skomro P, Lietz-Kijak D, Bogdziewicz-Wałęsa O, Janiszewska-Olszowska J. Effect of an Extremely Low-Frequency Electromagnetic Field on the Concentration of Salivary Immunoglobulin A. International Journal of Environmental Research and Public Health. 2022; 19(10):5786. https://doi.org/10.3390/ijerph19105786
Chicago/Turabian StyleSkomro, Piotr, Danuta Lietz-Kijak, Olga Bogdziewicz-Wałęsa, and Joanna Janiszewska-Olszowska. 2022. "Effect of an Extremely Low-Frequency Electromagnetic Field on the Concentration of Salivary Immunoglobulin A" International Journal of Environmental Research and Public Health 19, no. 10: 5786. https://doi.org/10.3390/ijerph19105786
APA StyleSkomro, P., Lietz-Kijak, D., Bogdziewicz-Wałęsa, O., & Janiszewska-Olszowska, J. (2022). Effect of an Extremely Low-Frequency Electromagnetic Field on the Concentration of Salivary Immunoglobulin A. International Journal of Environmental Research and Public Health, 19(10), 5786. https://doi.org/10.3390/ijerph19105786







