Comparing the Clinical Characteristics and Mortality of Residential and Non-Residential Older People with COVID-19: Retrospective Observational Study
Abstract
:1. Introduction
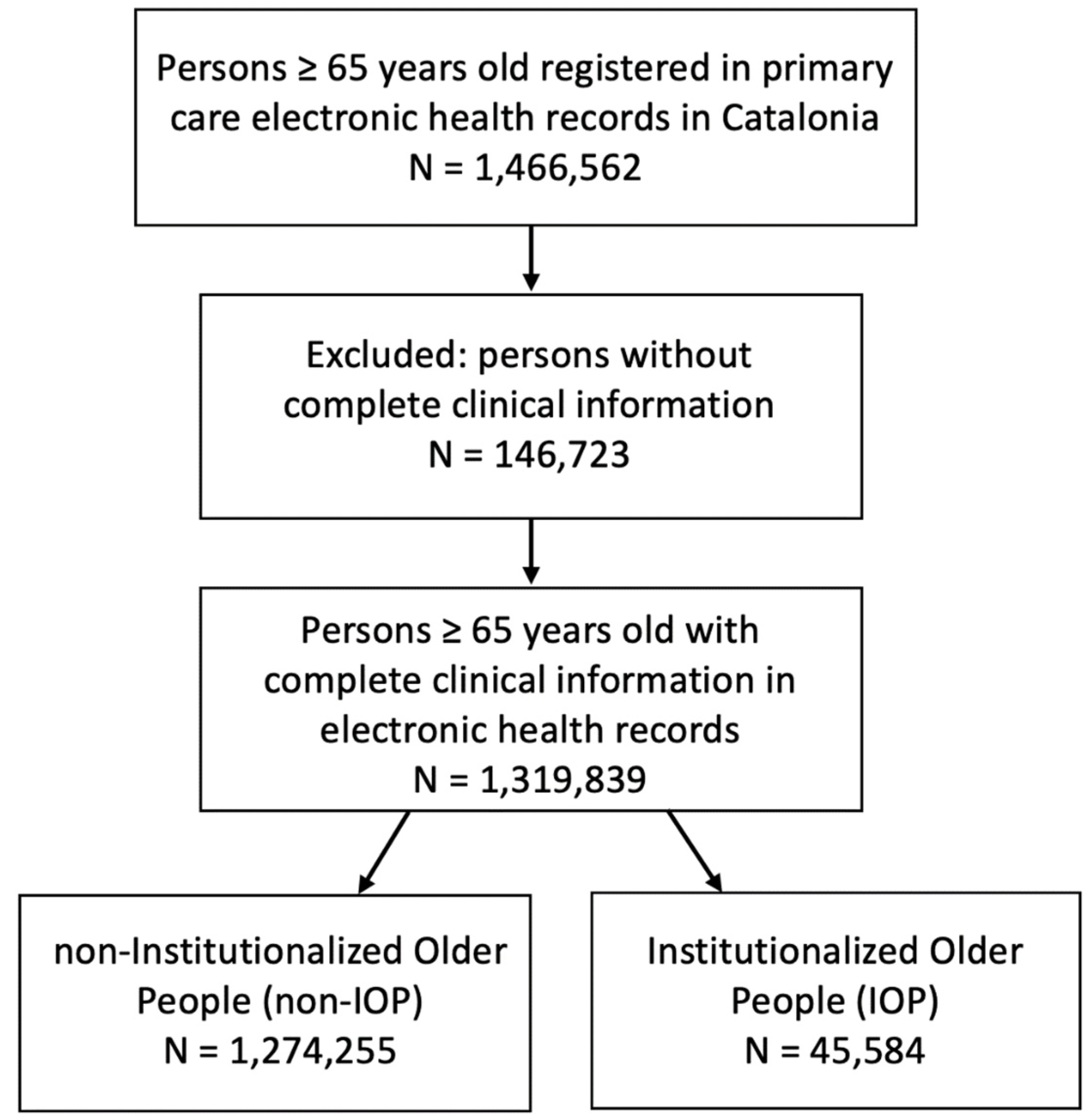
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Baseline Characteristics and Comorbidities
2.3. Outcomes
2.4. Statistical Methods
3. Results
3.1. Characteristics of the Sample
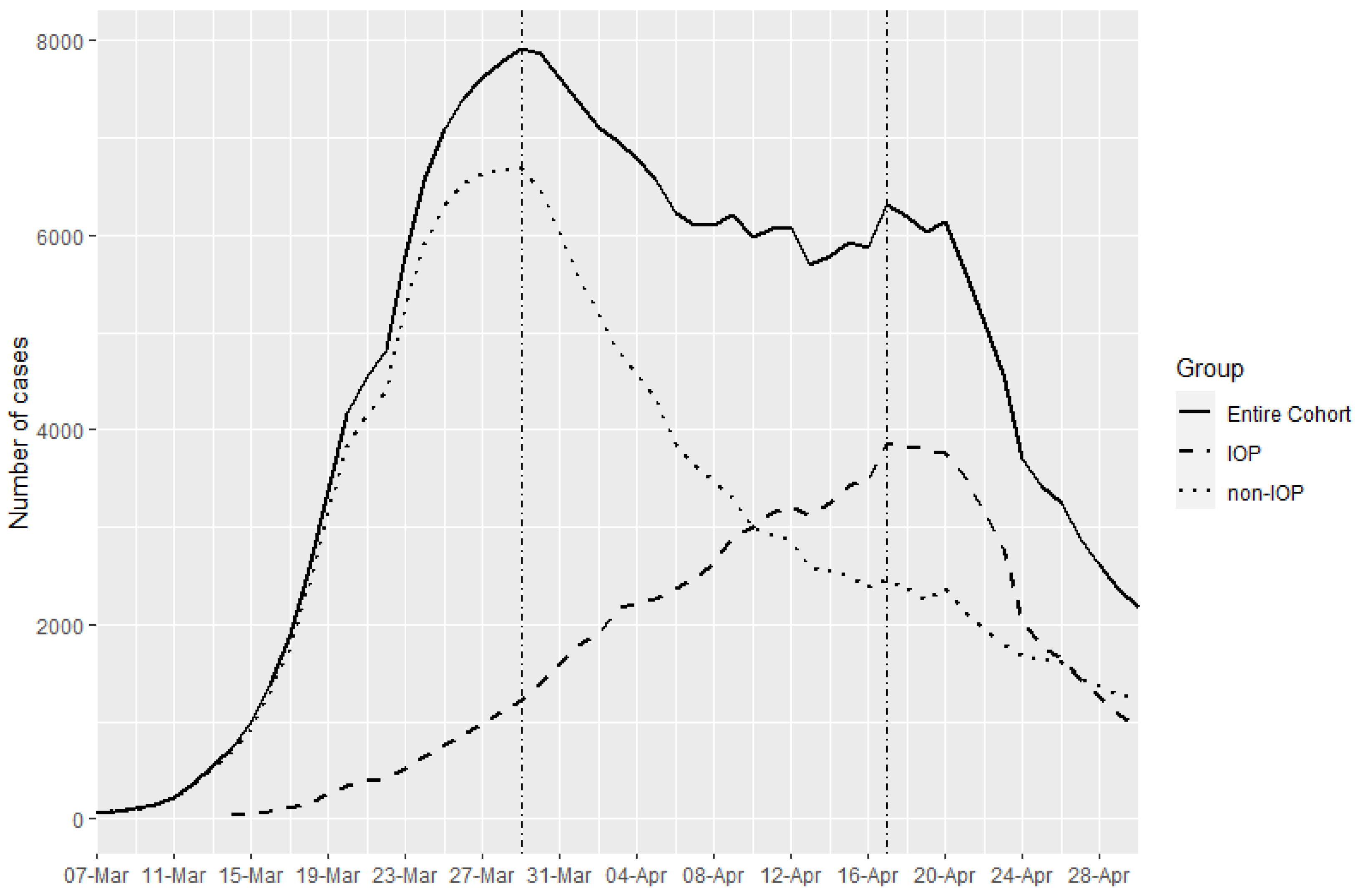
3.2. COVID-19 Cases
Cumulative Incidence Curve of COVID-19 Cases
3.3. Mortality Due to COVID-19
3.3.1. Weekly Mortality Rate by Place of Residence
3.3.2. Model of Overall Mortality Risk among COVID-19 Cases, According to the Place of Residence (sHR: Stratified Hazard Ratio)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sánchez-García, M.R.; Gutiérrez-Romero, J.A.; Fernández-Alcántara, M.; Hueso-Montoro, C.; Goodman, C.; Montoya-Juárez, R. End of life care in nursing homes in Spain: Exploratory analysis and evidences of validity of a new scale. Appl. Nurs. Res. 2017, 37, 6–12. [Google Scholar] [CrossRef] [Green Version]
- Broad, J.B.; Gott, M.; Kim, H.; Boyd, M.; Chen, H.; Connolly, M.J. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics. Int. J. Public Health 2013, 58, 257–267. [Google Scholar] [CrossRef]
- Cai, J.; Zhao, H.; Coyte, P. Socioeconomic Differences and Trends in the Place of Death among Elderly People in China. Int. J. Environ. Res. Public Health 2017, 14, 1210. [Google Scholar] [CrossRef] [Green Version]
- Roheger, M.; Zupanic, E.; Kåreholt, I.; Religa, D.; Kalbe, E.; Eriksdotter, M.; Garcia-Ptacek, S. Mortality and nursing home placement of dementia patients in rural and urban areas: A cohort study from the Swedish Dementia Registry. Scand. J. Caring Sci. 2018, 32, 1308–1313. [Google Scholar] [CrossRef]
- Hedinger, D.; Braun, J.; Zellweger, U.; Kaplan, V.; Bopp, M. Moving to and Dying in a Nursing Home Depends Not Only on Health—An Analysis of Socio-Demographic Determinants of Place of Death in Switzerland. PLoS ONE 2014, 9, e113236. [Google Scholar] [CrossRef] [Green Version]
- Wales, J.; Kalia, S.; Moineddin, R.; Husain, A. The Impact of Socioeconomic Status on Place of Death Among Patients Receiving Home Palliative Care in Toronto, Canada: A Retrospective Cohort Study. J. Palliat. Care 2020, 35, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.T.; McCorkle, R. Determinants of Place of Death for Terminal Cancer Patients. Cancer Investig. 2001, 19, 165–180. [Google Scholar] [CrossRef]
- Reilev, M.; Lundby, C.; Jensen, J.; Larsen, S.P.; Hoffmann, H.; Pottegård, A. Morbidity and mortality among older people admitted to nursing home. Age Ageing 2020, 49, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.-C.; Hung, I.F.-N.; Cheng, V.C.-C.; Luk, J.K.-H.; Woo, P.C.-Y.; Chu, L.-W.; Chan, F.H.-W. Is Nursing Home Residence an Independent Risk Factor of Mortality in Chinese Older Adults? J. Am. Geriatr. Soc. 2013, 61, 1430–1432. [Google Scholar] [CrossRef] [PubMed]
- Wauters, M.; Elseviers, M.; Vaes, B.; Degryse, J.; Vander Stichele, R.; Christiaens, T.; Azermai, M. Mortality, hospitalisation, institutionalisation in community-dwelling oldest old: The impact of medication. Arch. Gerontol. Geriatr. 2016, 65, 9–16. [Google Scholar] [CrossRef]
- McCann, M.; O’Reilly, D.; Cardwell, C. A Census-based longitudinal study of variations in survival amongst residents of nursing and residential homes in Northern Ireland. Age Ageing 2009, 38, 711–717. [Google Scholar] [CrossRef] [Green Version]
- Falcone, M.; Russo, A.; Gentiloni Silverj, F.; Marzorati, D.; Bagarolo, R.; Monti, M.; Velleca, R.; D’Angelo, R.; Frustaglia, A.; Zuccarelli, G.C.; et al. Predictors of mortality in nursing-home residents with pneumonia: A multicentre study. Clin. Microbiol. Infect. 2018, 24, 72–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, C.J.; Ho, Y.; Daveson, B.A.; Hall, S.; Higginson, I.J.; Gao, W. Place and Cause of Death in Centenarians: A Population-Based Observational Study in England, 2001 to 2010. PLoS Med. 2014, 11, e1001653. [Google Scholar] [CrossRef]
- Etard, J.-F.; Vanhems, P.; Atlani-Duault, L.; Ecochard, R. Potential lethal outbreak of coronavirus disease (COVID-19) among the elderly in retirement homes and long-term facilities, France, March 2020. Eurosurveillance 2020, 25, 2000448. [Google Scholar] [CrossRef]
- McMichael, T.M.; Clark, S.; Pogosjans, S.; Kay, M.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; Ferro, J.; Brostrom-Smith, C.; et al. COVID-19 in a Long-Term Care Facility—King County, Washington, February 27–March 9, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 339–342. [Google Scholar] [CrossRef] [Green Version]
- Meis-Pinheiro, U.; Lopez-Segui, F.; Walsh, S.; Ussi, A.; Santaeugenia, S.; Garcia-Navarro, J.A.; San-Jose, A.; Andreu, A.L.; Campins, M.; Almirante, B. Clinical characteristics of COVID-19 in older adults. A retrospective study in long-term nursing homes in Catalonia. PLoS ONE 2021, 16, e0255141. [Google Scholar] [CrossRef] [PubMed]
- España, P.P.; Bilbao, A.; García-Gutiérrez, S.; Lafuente, I.; Anton-Ladislao, A.; Villanueva, A.; Uranga, A.; Legarreta, M.J.; Aguirre, U.; Quintana, J.M.; et al. Predictors of mortality of COVID-19 in the general population and nursing homes. Intern. Emerg. Med. 2021, 16, 1487–1496. [Google Scholar] [CrossRef]
- Redondo-Bravo, L.; Moros, M.J.S.; Sanchez, E.V.M.; Lorusso, N.; Ubago, A.C.; Garcia, V.G.; Villanueva, P.S.; Azon, A.P.; Bescos, J.G.; Boone, A.L.D.; et al. The first wave of the COVID-19 pandemic in Spain: Characterisation of cases and risk factors for severe outcomes, as at 27 April 2020. Eurosurveillance 2020, 25, 2001431. [Google Scholar] [CrossRef]
- Coma, E.; Méndez, L. Experiencias para compartir SISAP: 4 años buceando en mares de datos. AMF Actual. Med. Fam. 2010, 6, 473–476. [Google Scholar]
- Avilés, F.; Méndez, L.; Medina, M. Sistema de Información de los Servicios de Atención Primaria. La Experiencia 2006–2008 de l’Institut Català de la Salut. Rev. Innovacion Sanit. y Atención Integr. 2008. Available online: https://www.researchgate.net/publication/33544050_Sistema_de_Informacion_de_los_Servicios_de_Atencion_Primaria_La_experiencia_2006-2008_del_Institut_Catala_de_la_Salut (accessed on 10 October 2021).
- Baena-Díez, J.M.; Garcia-Gil, M.; Comas-Cufí, M.; Ramos, R.; Prieto-Alhambra, D.; Salvador-González, B.; Elosua, R.; Dégano, I.R.; Peñafiel, J.; Grau, M. Association between chronic immune-mediated inflammatory diseases and cardiovascular risk. Heart 2018, 104, 119–126. [Google Scholar] [CrossRef]
- Garcia-Gil, M.; Elorza, J.-M.; Banque, M.; Comas-Cufí, M.; Blanch, J.; Ramos, R.; Méndez-Boo, L.; Hermosilla, E.; Bolibar, B.; Prieto-Alhambra, D. Linking of Primary Care Records to Census Data to Study the Association between Socioeconomic Status and Cancer Incidence in Southern Europe: A Nation-Wide Ecological Study. PLoS ONE 2014, 9, e109706. [Google Scholar] [CrossRef] [Green Version]
- Prieto-Alhambra, D.; Balló, E.; Coma, E.; Mora, N.; Aragón, M.; Prats-Uribe, A.; Fina, F.; Benítez, M.; Guiriguet, C.; Fàbregas, M.; et al. Filling the gaps in the characterization of the clinical management of COVID-19: 30-day hospital admission and fatality rates in a cohort of 118,150 cases diagnosed in outpatient settings in Spain. Int. J. Epidemiol. 2021, 49, 1930–1939. [Google Scholar] [CrossRef]
- Morales, D.R.; Conover, M.M.; You, S.C.; Pratt, N.; Kostka, K.; Duarte-Salles, T.; Fernández-Bertolín, S.; Aragón, M.; DuVall, S.L.; Lynch, K.; et al. Renin–angiotensin system blockers and susceptibility to COVID-19: An international, open science, cohort analysis. Lancet Digit. Health 2021, 3, e98–e114. [Google Scholar] [CrossRef]
- Burn, E.; Tebé, C.; Fernandez-Bertolin, S.; Aragon, M.; Recalde, M.; Roel, E.; Prats-Uribe, A.; Prieto-Alhambra, D.; Duarte-Salles, T. The natural history of symptomatic COVID-19 during the first wave in Catalonia. Nat. Commun. 2021, 12, 777. [Google Scholar] [CrossRef] [PubMed]
- Cabezas, C.; Coma, E.; Mora-Fernandez, N.; Li, X.; Martinez-Marcos, M.; Fina, F.; Fabregas, M.; Hermosilla, E.; Jover, A.; Contel, J.C.; et al. Associations of BNT162b2 vaccination with SARS-CoV-2 infection and hospital admission and death with covid-19 in nursing homes and healthcare workers in Catalonia: Prospective cohort study. BMJ 2021, 374, n1868. [Google Scholar] [CrossRef]
- Colls, C.; Mias, M.; García-Altés, A. Un índice de privación para reformar el modelo de financiación de la atención primaria en Cataluña. Gac. Sanit. 2020, 34, 44–50. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Monterde, D.; Vela, E.; Clèries, M. Los grupos de morbilidad ajustados: Nuevo agrupador de morbilidad poblacional de utilidad en el ámbito de la atención primaria. Aten. Primaria 2016, 48, 674–682. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Batiste, X.; Martínez-Muñoz, M.; Blay, C.; Amblàs, J.; Vila, L.; Costa, X.; Villanueva, A.; Espaulella, J.; Espinosa, J.; Figuerola, M.; et al. Identifying patients with chronic conditions in need of palliative care in the general population: Development of the NECPAL tool and preliminary prevalence rates in Catalonia. BMJ Support. Palliat. Care 2013, 3, 300–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gómez-Batiste, X.; Martínez-Muñoz, M.; Blay, C.; Amblàs, J.; Vila, L.; Costa, X. Identificación de personas con enfermedades crónicas avanzadas y necesidad de atención paliativa en servicios sanitarios y sociales: Elaboración del instrumento NECPAL CCOMS-ICO©. Med. Clin. 2013, 140, 241–245. [Google Scholar] [CrossRef]
- Gómez-Batiste, X.; Martínez-Muñoz, M.; Blay, C.; Amblàs, J.; Vila, L.; Costa, X.; Espaulella, J.; Espinosa, J.; Constante, C.; Mitchell, G.K. Prevalence and characteristics of patients with advanced chronic conditions in need of palliative care in the general population: A cross-sectional study. Palliat. Med. 2014, 28, 302–311. [Google Scholar] [CrossRef]
- Ahmad, O.B.; Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D. Age Standardization of Rates: A New WHO Standard; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Davidson, P.M.; Szanton, S.L. Nursing homes and COVID-19: We can and should do better. J. Clin. Nurs. 2020, 29, 2758–2759. [Google Scholar] [CrossRef] [Green Version]
- Adalja, A.A.; Toner, E.; Inglesby, T.V. Priorities for the US Health Community Responding to COVID-19. JAMA 2020, 323, 1343. [Google Scholar] [CrossRef] [Green Version]
- Briggs, R.; Holmerová, I.; Martin, F.C.; O’Neill, D. Towards standards of medical care for physicians in nursing homes. Eur. Geriatr. Med. 2015, 6, 401–403. [Google Scholar] [CrossRef]
- Morales Viera, A.; Rivas Rodríguez, R.; Otero Aguilar, P.; Briones Pérez de Blanca, E. Epidemiología de la COVID-19 entre el personal de centros sociosanitarios de Sevilla. Rev. Clin. Esp. 2021, in press. [CrossRef] [PubMed]
- McMichael, T.M.; Currie, D.W.; Clark, S.; Pogosjans, S.; Kay, M.; Schwartz, N.G.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; et al. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N. Engl. J. Med. 2020, 382, 2005–2011. [Google Scholar] [CrossRef] [PubMed]
- Graham, N.S.N.; Junghans, C.; McLaren, R.; Randell, P.; Lang, N.; Ladhani, S.N.; Sharp, D.J.; Sanderson, F. High rates of SARS-CoV-2 seropositivity in nursing home residents. J. Infect. 2021, 82, 282–327. [Google Scholar] [CrossRef]
- Suñer, C.; Ouchi, D.; Mas, M.À.; Lopez Alarcon, R.; Massot Mesquida, M.; Prat, N.; Bonet-Simó, J.M.; Expósito Izquierdo, M.; Garcia Sánchez, I.; Rodoreda Noguerola, S.; et al. A retrospective cohort study of risk factors for mortality among nursing homes exposed to COVID-19 in Spain. Nat. Aging 2021, 1, 579–584. [Google Scholar] [CrossRef]
- Panagiotou, O.A.; Kosar, C.M.; White, E.M.; Bantis, L.E.; Yang, X.; Santostefano, C.M.; Feifer, R.A.; Blackman, C.; Rudolph, J.L.; Gravenstein, S.; et al. Risk Factors Associated with All-Cause 30-Day Mortality in Nursing Home Residents With COVID-19. JAMA Intern. Med. 2021, 181, 439. [Google Scholar] [CrossRef]
- Abrams, H.R.; Loomer, L.; Gandhi, A.; Grabowski, D.C. Characteristics of U.S. Nursing Homes with COVID-19 Cases. J. Am. Geriatr. Soc. 2020, 68, 1653–1656. [Google Scholar] [CrossRef]
- Manabe, T.; Fujikura, Y.; Mizukami, K.; Akatsu, H.; Kudo, K. Pneumonia-associated death in patients with dementia: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0213825. [Google Scholar] [CrossRef] [Green Version]
- Hariyanto, T.I.; Putri, C.; Situmeang, R.F.V.; Kurniawan, A. Dementia is a predictor for mortality outcome from coronavirus disease 2019 (COVID-19) infection. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 393–395. [Google Scholar] [CrossRef]
- Boivin, G.; Hardy, I.; Tellier, G.; Maziade, J. Predicting Influenza Infections during Epidemics with Use of a Clinical Case Definition. Clin. Infect. Dis. 2000, 31, 1166–1169. [Google Scholar] [CrossRef] [PubMed]
- Monto, A.S.; Gravenstein, S.; Elliott, M.; Colopy, M.; Schweinle, J. Clinical Signs and Symptoms Predicting Influenza Infection. Arch. Intern. Med. 2000, 160, 3243. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Comorbidity | ICD10-CM Codes |
|---|---|
| Hypertension | I10, I11.0, I11.9, I12.0, I12.9, I13.0, I13.10, I13.2, I15.0, I15.1, I15.2, I15.8, I15.9 |
| Type 1 Diabetes Mellitus | E10.10, E10.29, E10.311, E10.359, E10.39, E10.49, E10.59, E10.621, E10.65, E10.69, E10.8, E10.9 |
| Type 2 Diabetes Mellitus | E11.01, E11.21, E11.22, E11.29, E11.311, E11.39, E11.40, E11.43, E11.49, E11.51, E11.59, E11.610. E11.621, E11.638, E11.641, E11.649, E11.65, E11.69, E11.8, E11.9, E13.10, E13.29, E13.39, E13.49, E13.59, E13.641, E13.69, E13.8, E13.9 |
| Chronic obstructive pulmonary disease (COPD) | J43.0, J43.1, J43.2, J43.8, J43.9, J44, J44.0, J44.1, J44.9 |
| Ischaemic heart disease | I20, I20.0, I20.8, I20.9, I24.0, I24.1, I24.8, I24.9, I25, I25.10, I25.2, I25.41, 125.5, I25.6, I25.89, I25.9, I70.90, I21, I21.0, I21.01, I21.02, I21.09, I21.1, I21.11, I21.19, I21.2, I21.29, I21.3, I21.4, I22.0, I22.1, I22.2, I22.8, I22.9, I23.0, I23.1, I23.2, I23.3, I23.4, I23.5, I23.6, I23.8 |
| Cerebrovascular disease | G45.0, G45.1, G45.2, G45.8, G45.9, G46.0, G46.1, G46.2, G46.3, G46.4, G46.5, G46.6, G46.7, G46.9, I63.00, I63.10, I63.20, I63.30, I63.40, I63.50, I63.6, I63.8, I63.9, I67.82, I67.9, I69.30, I69.320 I69.398, I69.80, I69.998 I61.0, I61.1, I61.2, I61.3, I61.4, I61.5, I61.6, I61.8, I61.9, I61.10 |
| Heart failure | I50.1, I50.20, I50.30, I50.32, I50.9 |
| Atrial fibrillation | I48.0. I48.1, I48.2, I48.91 |
| Liver failure | K70.0, K70.10, K70.2, K70.30, K70.9, K73.0, K73.1, K73.2, K73.8, K73.9, K75.0, K75.2, K75.3, K75.4, K75.89, k75.9, K76.5, K76.7, K76.9 |
| Type B Hepatitis | B16.0, B16.1, B16.2, B16.9, |
| Type C Hepatitis | B17.10, B18.2 |
| Cancer (all except non-melanoma skin cancer) | C00-C97 (except C44), D00-D09 |
| Chronic Kidney Disease | I12.0, I13.0, N03.9, N18.1, N18.2, N18.4, N18.5, N18.6, N18.9, N19, N28.9, N99.0, P96.0, Z94.0 |
| Obesity | E66.01, E66.09, E66.1, E66.2, E66.8, E66.9 |
| Entire Cohort N = 1,319,839 N (%) | Non-IOP N = 1,274,255 N (%) | IOP N = 45,584 N (%) | p-Value | |
|---|---|---|---|---|
| Age (in years), mean (SD) | 75.9 (7.95) | 75.5 (7.71) | 86.4 (7.35) | <0.001 |
| Age group (at baseline) | <0.001 | |||
| 65–74 years | 663,341 (50.3) | 659,690 (51.8) | 3651 (8.01) | |
| 75–84 years | 430,020 (32.6) | 418,063 (32.8) | 11,957 (26.2) | |
| ≥85 years | 226,478 (17.2) | 196,502 (15.4) | 29,976 (65.8) | |
| Gender | <0.001 | |||
| Female | 754,921 (57.2) | 721,205 (56.6) | 33,716 (74.0) | |
| Male | 564,918 (42.8) | 553,050 (43.4) | 11,868 (26.0) | |
| Rurality | <0.001 | |||
| Rural | 271,847 (25.0) | 259,269 (24.7) | 12,578 (33.1) | |
| Urban | 814,547 (75.0) | 789,072 (75.3) | 25,475 (66.9) | |
| CSI, mean (SD) | 45.2 (15.5) | 45.3 (15.6) | 42.1 (13.8) | <0.001 |
| CSI Levels | <0.001 | |||
| <25 | 110,381 (10.2) | 105,390 (10.1) | 4991 (13.1) | |
| 25–49 | 605,789 (55.8) | 582,095 (55.5) | 23,694 (62.3) | |
| 50–74 | 329,262 (30.3) | 320,542 (30.6) | 8720 (22.9) | |
| >75 | 40,962 (3.77) | 40,314 (3.85) | 648 (1.70) | |
| AMG_complexity Levels | <0.001 | |||
| Level 0 | 1,262,621 (95.7) | 1,229,661 (96.5) | 32,960 (72.3) | |
| Level 1 | 39,025 (2.96) | 29,964 (2.35) | 9061 (19.9) | |
| Level 2 | 15,716 (1.19) | 12,532 (0.98) | 3184 (6.98) | |
| Level 3 | 2308 (0.17) | 1949 (0.15) | 359 (0.79) | |
| Level 4 | 163 (0.01) | 144 (0.01) | 19 (0.04) | |
| Level 5 | 6 (0.00) | 5 (0.00) | 1 (0.00) | |
| CCP | 130,261 (9.87) | 108,605 (8.52) | 21,656 (47.5) | <0.001 |
| ACD | 20,230 (1.53) | 14,883 (1.17) | 5347 (11.7) | <0.001 |
| Medical conditions (at baseline) | ||||
| Hypertension | 824,012 (62.4) | 791,399 (62.1) | 32,613 (71.5) | <0.001 |
| Diabetes mellitus | 323,150 (24.5) | 310,573 (24.4) | 12,577 (27.6) | <0.001 |
| COPD | 112,149 (8.5) | 108,206 (8.49) | 3943 (8.65) | 0.237 |
| Ischaemic heart disease | 110,223 (8.35) | 106,139 (8.33) | 4084 (8.96) | <0.001 |
| Cerebrovascular disease | 74,986 (5.68) | 70,037 (5.50) | 4949 (10.9) | <0.001 |
| Congestive heart failure | 80,693 (6.11) | 74,648 (5.86) | 6045 (13.3) | <0.001 |
| Atrial fibrillation | 147,705 (11.2) | 139,402 (10.9) | 8303 (18.2) | <0.001 |
| Valvular disease | 86,984 (6.59) | 84,088 (6.60) | 2896 (6.35) | 0.039 |
| Liver failure | 98,338 (7.45) | 96,766 (7.59) | 1572 (3.45) | <0.001 |
| Type B Hepatitis | 4628 (0.35) | 4483 (0.35) | 145 (0.32) | 0.248 |
| Type C Hepatitis | 11,318 (0.86) | 10,743 (0.84) | 575 (1.26) | <0.001 |
| Cancer | 270,160 (20.5) | 261,455 (20.5) | 8705 (19.1) | <0.001 |
| Chronic kidney disease | 226,811 (17.2) | 214,490 (16.8) | 12,321 (27.0) | <0.001 |
| Obesity | 392,731 (29.8) | 383,707 (30.1) | 9024 (19.8) | <0.001 |
| Dementia | 76,550 (5.80) | 56,104 (4.40) | 20,446 (44.9) | <0.001 |
| Osteoarthritis | 505,726 (38.3) | 485,175 (38.1) | 20,551 (45.1) | <0.001 |
| Num. of Comorbidities | <0.001 | |||
| 0 | 164,305 (12.4) | 162,761 (12.8) | 1544 (3.39) | |
| 1 | 251,173 (19.0) | 245,949 (19.3) | 5224 (11.5) | |
| 2 | 287,447 (21.8) | 278,163 (21.8) | 9284 (20.4) | |
| 3 | 256,654 (19.4) | 245,988 (19.3) | 10,666 (23.4) | |
| ≥4 | 360,260 (27.3) | 341,394 (26.8) | 18,866 (41.4) | |
| COVID Cases | ||||
| Confirmed by RT-PCR | 23,488 (1.78) | 13,405 (1.05) | 10,083 (22.1) | <0.001 |
| Clinical diagnosis | 13,622 (1.03) | 10,565 (0.83) | 3057 (6.71) | <0.001 |
| Deaths | 9726 (0.74) | 5514 (0.43) | 4212 (9.24) | <0.001 |
| Total Cases N = 37,110 N (%) | Deaths N = 9726 N (%) | p-Value | Non-IOP N = 5514 N (%) | IOP N = 4212 N (%) | OR (CI95) | p-Value | |
|---|---|---|---|---|---|---|---|
| Age (in years), mean (SD) | 80.7 (9.15) | 84.6 (8.07) | <0.001 | 82.1 (8.04) | 87.8 (6.86) | 1.11 [1.10;1.11] | <0.001 |
| Age group (at baseline) | <0.001 | <0.001 | |||||
| 65–74 years | 11,088 (29.9) | 1288 (13.2) | 1091 (19.8) | 197 (4.68) | Ref. | ||
| 75–84 years | 11,510 (31.0) | 3009 (30.9) | 2090 (37.9) | 919 (21.8) | 2.43 [2.06;2.89] | ||
| ≥85 years | 14,512 (39.1) | 5429 (55.8) | 2333 (42.3) | 3096 (73.5) | 7.34 [6.27;8.65] | ||
| Gender | <0.001 | <0.001 | |||||
| Female | 21,972 (59.2) | 5092 (52.4) | 2345 (42.5) | 2747 (65.2) | 2.53 [2.33;2.75] | ||
| Male | 15,138 (40.8) | 4634 (47.6) | 3169 (57.5) | 1465 (34.8) | Ref. | ||
| Rurality | 0.080 | <0.001 | |||||
| Rural | 6536 (21.2) | 1677 (20.5) | 828 (18.0) | 849 (23.8) | 1.43 [1.28;1.59] | ||
| Urban | 24,253 (78.8) | 6486 (79.5) | 3775 (82.0) | 2711 (76.2) | Ref. | ||
| CSI, mean (SD) | 44.3 (15.7) | 43.5 (15.6) | <0.001 | 45.3 (16.1) | 41.2 (14.4) | 0.98 [0.98;0.99] | <0.001 |
| CSI Levels | <0.001 | <0.001 | |||||
| <25 | 3434 (11.2) | 941 (11.5) | 463 (10.1) | 478 (13.4) | Ref. | ||
| 25–49 | 17,683 (57.4) | 4861 (59.5) | 2606 (56.6) | 2255 (63.3) | 0.84 [0.73;0.96] | ||
| 50–74 | 8465 (27.5) | 2079 (25.5) | 1316 (28.6) | 763 (21.4) | 0.56 [0.48;0.66] | ||
| >75 | 1207 (3.92) | 282 (3.45) | 218 (4.74) | 64 (1.80) | 0.29 [0.21;0.39] | ||
| AMG complexity Levels | <0.001 | 0.020 | |||||
| Level 0 | 26,782 (72.2) | 2425 (24.9) | 1422 (25.8) | 1003 (23.8) | |||
| Level 1 | 7127 (19.2) | 5092 (52.4) | 2748 (49.8) | 2344 (55.7) | |||
| Level 2 | 2765 (7.45) | 1922 (19.8) | 1142 (20.7) | 780 (18.5) | |||
| Level 3 | 405 (1.09) | 271 (2.79) | 191 (3.46) | 80 (1.90) | |||
| Level 4 | 30 (0.08) | 15 (0.15) | 11 (0.20) | 4 (0.09) | |||
| Level 5 | 1 (0.00) | 1 (0.01) | 0 (0.00) | 1 (0.02) | |||
| CCP | 10,666 (28.7) | 3500 (36.0) | <0.001 | 1494 (27.1) | 2006 (47.6) | 2.45 [2.25;2.66] | <0.001 |
| ACD | 2354 (6.34) | 911 (9.37) | <0.001 | 279 (5.06) | 632 (15.0) | 3.31 [2.86;3.84] | <0.001 |
| Medical conditions (at baseline) | |||||||
| Hypertension | 25,303 (68.2) | 7040 (72.4) | <0.001 | 4014 (72.8) | 3026 (71.8) | 0.95 [0.87;1.04] | 0.308 |
| Diabetes mellitus | 10,635 (28.7) | 3154 (32.4) | <0.001 | 1959 (35.5) | 1195 (28.4) | 0.72 [0.66;0.78] | <0.001 |
| COPD | 4216 (11.4) | 1304 (13.4) | <0.001 | 898 (16.3) | 406 (9.64) | 0.55 [0.48;0.62] | <0.001 |
| Ischaemic heart disease | 4063 (10.9) | 1288 (13.2) | <0.001 | 872 (15.8) | 416 (9.88) | 0.58 [0.51;0.66] | <0.001 |
| Cerebrovascular disease | 3366 (9.07) | 976 (10.0) | <0.001 | 515 (9.34) | 461 (10.9) | 1.19 [1.04;1.36] | 0.010 |
| Congestive heart failure | 4428 (11.9) | 1488 (15.3) | <0.001 | 872 (15.8) | 616 (14.6) | 0.91 [0.82;1.02] | 0.113 |
| Atrial fibrillation | 6380 (17.2) | 1917 (19.7) | <0.001 | 1165 (21.1) | 752 (17.9) | 0.81 [0.73;0.90] | <0.001 |
| Valvular disease | 2881 (7.76) | 823 (8.46) | 0.003 | 556 (10.1) | 267 (6.34) | 0.60 [0.52;0.70] | <0.001 |
| Liver failure | 2527 (6.81) | 545 (5.60) | <0.001 | 417 (7.56) | 128 (3.04) | 0.38 [0.31;0.47] | <0.001 |
| Type B Hepatitis | 141 (0.38) | 32 (0.33) | 0.393 | 21 (0.38) | 11 (0.26) | 0.69 [0.32;1.41] | 0.399 |
| Type C Hepatitis | 441 (1.19) | 129 (1.33) | 0.159 | 72 (1.31) | 57 (1.35) | 1.04 [0.73;1.47] | 0.910 |
| Cancer | 8584 (23.1) | 2468 (25.4) | <0.001 | 1653 (30.0) | 815 (19.3) | 0.56 [0.51;0.62] | <0.001 |
| Chronic kidney disease | 8981 (24.2) | 2942 (30.2) | <0.001 | 1751 (31.8) | 1191 (28.3) | 0.85 [0.78;0.92] | <0.001 |
| Obesity | 10,476 (28.2) | 2564 (26.4) | <0.001 | 1808 (32.8) | 756 (17.9) | 0.45 [0.41;0.49] | <0.001 |
| Dementia | 8045 (21.7) | 2933 (30.2) | <0.001 | 766 (13.9) | 2167 (51.4) | 6.57 [5.96;7.24] | <0.001 |
| Osteoarthritis | 16,156 (43.5) | 4230 (43.5) | 0.929 | 2357 (42.7) | 1873 (44.5) | 1.07 [0.99;1.16] | 0.094 |
| Number of Medical conditions | <0.001 | <0.001 | |||||
| 0 | 2362 (6.36) | 367 (3.77) | 236 (4.28) | 131 (3.11) | Ref. | ||
| 1 | 4968 (13.4) | 998 (10.3) | 556 (10.1) | 442 (10.5) | 1.43 [1.12;1.84] | ||
| 2 | 7323 (19.7) | 1740 (17.9) | 926 (16.8) | 814 (19.3) | 1.58 [1.25;2.00] | ||
| 3 | 7794 (21.0) | 2072 (21.3) | 1084 (19.7) | 988 (23.5) | 1.64 [1.31;2.07] | ||
| ≥4 | 4549 (46.8) | 2712 (49.2) | 1837 (43.6) | 1.22 [0.98;1.53] | |||
| COVID Cases | <0.001 | <0.001 | |||||
| Confirmed by RT-PCR | 23,488 (63.3) | 5505 (56.6) | 3489 (63.3) | 2016 (47.9) | |||
| Clinical diagnosis | 13,622 (36.7) | 4221 (43.4) | 2025 (36.7) | 2196 (52.1) |
| Non-IOP | IOP | |||||
|---|---|---|---|---|---|---|
| Deaths N = 5514 | Population N = 1,274,255 | MR 1 (95% CI) | Deaths N = 4212 | Population N = 45,584 | MR 1 (95% CI) | |
| Age group | ||||||
| 65–74 years | 1091 | 659,690 | 1.04 (1.03–1.04) | 197 | 3651 | 33.95 (32.85–35.06) |
| 75–84 years | 2090 | 418,063 | 1.047 (1.47–1.48) | 919 | 11,957 | 21.31 (20.93–21.69) |
| ≥85 years | 2333 | 196,502 | 0.84 (0.84–0.85) | 3091 | 29,976 | 7.36 (7.28–7.44) |
| Gender | ||||||
| Female | ||||||
| 65–74 years | 349 | 354,609 | 0.62 (0.62–0.62) | 78 | 1832 | 26.73 (25.51–27.95) |
| 75–84 years | 787 | 238,703 | 0.97 (0.97–0.98) | 495 | 7971 | 18.33 (17.92–18.73) |
| ≥85 years | 1209 | 127,839 | 0.67 (0.67–0.68) | 2174 | 23,797 | 6.49 (6.4–6.57) |
| Male | ||||||
| 65–74 years | 742 | 305,053 | 1.53 (1.52–1.53) | 119 | 1810 | 41.28 (39.37–43.18) |
| 75–84 years | 1303 | 179,320 | 2.14 (2.13–2.15) | 424 | 3944 | 31.72 (30.73–32.71) |
| ≥85 years | 1124 | 68,613 | 1.16 (1.15–1.17) | 922 | 6059 | 10.8 (10.53–11.08) |
| COVID Cases | ||||||
| RT-PCR | ||||||
| 65–74 years | 794 | 5088 | 97.97 (95.28–100.6) | 113 | 776 | 91.42 (84.99–97.85) |
| 75–84 years | 1433 | 4956 | 85.33 (82.95–87.7) | 472 | 2576 | 54.07 (51.98–56.16) |
| ≥85 years | 1262 | 3253 | 29.91 (28.88–30.94) | 1431 | 6567 | 16.8 (16.39–17.21) |
| ICD-10-CM | ||||||
| 65–74 years | 297 | 5038 | 37.01 (35.99–38.03) | 84 | 149 | 353.9 (297.1–410.7) |
| 75–84 years | 657 | 3209 | 60.42 (58.33–62.51) | 447 | 687 | 192.0 (177.6–206.3) |
| ≥85 years | 1071 | 2308 | 35.78 (34.32–37.24) | 1665 | 2214 | 57.98 (55.57–60.4) |
| Entire Cohort * | Non-IOP | IOP | |||||||
|---|---|---|---|---|---|---|---|---|---|
| sHR | 95% CI | p-Value | HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age (in years) | 1.01 | 1.00–1.02 | <0.001 | 1.02 | 1.01–1.03 | <0.001 | 1.00 | 0.99–1.01 | 0.295 |
| Age: 75 to 84 years | 1.39 | 1.26–1.53 | <0.001 | 1.23 | 1.09–1.39 | <0.001 | 1.12 | 0.92–1.35 | 0.229 |
| Age: >84 years | 1.37 | 1.18–1.58 | 0.000 | 1.09 | 0.90–1.32 | 0.361 | 1.25 | 0.98–1.59 | 0.066 |
| Gender: Male | 1.24 | 1.18–1.31 | <0.001 | 1.27 | 1.19–1.35 | <0.001 | 1.19 | 1.11–1.29 | <0.001 |
| SCI | 1.00 | 0.99–1.00 | 0.187 | 1.00 | 0.99–1.00 | 0.067 | 0.99 | 0.99–1.00 | 0.548 |
| SCI: 25 to 49 | 0.92 | 0.83–1.02 | 0.138 | 0.90 | 0.78–1.04 | 0.169 | 0.98 | 0.85–1.14 | 0.893 |
| SCI: 50 to 74 | 0.85 | 0.73–0.99 | 0.049 | 0.80 | 0.64–0.98 | 0.039 | 0.97 | 0.77–1.24 | 0.860 |
| SCI: >75 | 0.83 | 0.65–1.07 | 0.161 | 0.74 | 0.54–1.03 | 0.076 | 1.10 | 0.71–1.70 | 0.641 |
| Rurality: Urban | 1.09 | 1.03–1.15 | 0.001 | 1.06 | 0.98–1.15 | 0.093 | 1.12 | 1.03–1.21 | 0.004 |
| AMG level 1 | 11.53 | 10.8–12.2 | <0.001 | 16.93 | 15.6–18.3 | <0.001 | 6.86 | 6.31–7.46 | <0.001 |
| AMG level 2 | 12.91 | 11.9–13.9 | <0.001 | 19.44 | 17.4–21.6 | <0.001 | 7.68 | 6.85–8.62 | <0.001 |
| AMG level 3 | 14.33 | 12.3–16.6 | <0.001 | 22.16 | 18.3–26.7 | <0.001 | 8.36 | 6.41–10.9 | <0.001 |
| AMG level 4 | 8.86 | 5.17–15.1 | <0.001 | 14.05 | 7.38–26.7 | <0.001 | 4.89 | 1.79–13.3 | 0.001 |
| AMG level 5 | 43.52 | 6.05–312.7 | <0.001 | - | - | - | 29.55 | 4.01–217.4 | <0.001 |
| CCP | 0.90 | 0.85–0.94 | <0.001 | 0.80 | 0.75–0.87 | <0.001 | 0.95 | 0.88–1.03 | 0.236 |
| ACD | 0.68 | 0.62–0.73 | <0.001 | 0.57 | 0.49–0.65 | <0.001 | 0.75 | 0.67–0.83 | <0.001 |
| Hypertension | 0.97 | 0.91–1.03 | 0.400 | 1.07 | 0.93–1.10 | 0.693 | 0.93 | 0.84–1.03 | 0.178 |
| Diabetes mellitus | 1.05 | 0.99–1.11 | 0.060 | 1.08 | 1.00–1.16 | 0.034 | 0.99 | 0.90–1.08 | 0.846 |
| COPD | 0.90 | 0.84–0.97 | 0.007 | 0.91 | 0.84–1.00 | 0.059 | 0.85 | 0.74–0.96 | 0.011 |
| Ischaemic heart disease | 1.00 | 0.93–1.08 | 0.831 | 1.04 | 0.95–1.14 | 0.301 | 0.94 | 0.83–1.06 | 0.339 |
| Cerebrovascular disease | 0.96 | 0.88–1.04 | 0.330 | 0.93 | 0.83–1.03 | 0.200 | 1.01 | 0.89–1.13 | 0.862 |
| Congestive heart failure | 0.90 | 0.84–0.97 | 0.008 | 0.89 | 0.81–0.98 | 0.020 | 0.93 | 0.83–1.04 | 0.222 |
| Atrial fibrillation | 0.92 | 0.86–0.98 | 0.015 | 0.91 | 0.84–0.99 | 0.031 | 0.93 | 0.84–1.02 | 0.159 |
| Valvular disease | 0.96 | 0.88–1.04 | 0.401 | 0.95 | 0.86–1.05 | 0.376 | 0.97 | 0.84–1.12 | 0.711 |
| Liver failure | 0.97 | 0.88–1.07 | 0.599 | 1.03 | 0.92–1.16 | 0.503 | 0.78 | 0.64–0.96 | 0.021 |
| Type B Hepatitis | 0.97 | 0.67–1.39 | 0.870 | 1.15 | 0.73–1.82 | 0.534 | 0.78 | 0.43–1.44 | 0.439 |
| Type C Hepatitis | 1.01 | 0.83–1.22 | 0.906 | 1.09 | 0.84–1.41 | 0.494 | 0.97 | 0.72–1.30 | 0.871 |
| Cancer | 0.95 | 0.95–1.05 | 0.089 | 0.94 | 0.88–1.01 | 0.144 | 0.94 | 0.85–1.03 | 0.233 |
| Chronic kidney disease | 1.00 | 0.94–1.06 | 0.953 | 0.99 | 0.92–1.07 | 0.889 | 0.99 | 0.90–1.08 | 0.898 |
| Obesity | 1.09 | 1.03–1.15 | 0.002 | 1.10 | 1.03–1.19 | 0.005 | 1.06 | 0.96–1.17 | 0.197 |
| Dementia | 1.21 | 1.14–1.28 | <0.001 | 1.04 | 0.95–1.15 | 0.318 | 1.32 | 1.22–1.44 | <0.001 |
| Osteoarthritis | 0.96 | 0.91–1.01 | 0.151 | 0.96 | 0.89–1.03 | 0.278 | 0.99 | 0.91–1.07 | 0.830 |
| Comorbidities num.: 1 | 0.85 | 0.74–0.98 | 0.026 | 0.87 | 0.72–1.04 | 0.143 | 0.67 | 0.54–0.84 | <0.001 |
| Comorbidities num.: 2 | 0.72 | 0.62–0.83 | <0.001 | 0.73 | 0.60–0.88 | 0.001 | 0.54 | 0.42–0.68 | <0.001 |
| Comorbidities num.: 3 | 0.59 | 0.50–0.70 | <0.001 | 0.60 | 0.48–0.74 | <0.001 | 0.44 | 0.34–0.58 | <0.001 |
| Comorbidities num.: ≥4 | 0.54 | 0.44–0.66 | <0.001 | 0.52 | 0.40–0.67 | <0.001 | 0.42 | 0.31–0.58 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marin-Gomez, F.X.; Mendioroz-Peña, J.; Mayer, M.-A.; Méndez-Boo, L.; Mora, N.; Hermosilla, E.; Coma, E.; Vilaseca, J.-M.; Leis, A.; Medina, M.; et al. Comparing the Clinical Characteristics and Mortality of Residential and Non-Residential Older People with COVID-19: Retrospective Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 483. https://doi.org/10.3390/ijerph19010483
Marin-Gomez FX, Mendioroz-Peña J, Mayer M-A, Méndez-Boo L, Mora N, Hermosilla E, Coma E, Vilaseca J-M, Leis A, Medina M, et al. Comparing the Clinical Characteristics and Mortality of Residential and Non-Residential Older People with COVID-19: Retrospective Observational Study. International Journal of Environmental Research and Public Health. 2022; 19(1):483. https://doi.org/10.3390/ijerph19010483
Chicago/Turabian StyleMarin-Gomez, Francesc X., Jacobo Mendioroz-Peña, Miguel-Angel Mayer, Leonardo Méndez-Boo, Núria Mora, Eduardo Hermosilla, Ermengol Coma, Josep-Maria Vilaseca, Angela Leis, Manolo Medina, and et al. 2022. "Comparing the Clinical Characteristics and Mortality of Residential and Non-Residential Older People with COVID-19: Retrospective Observational Study" International Journal of Environmental Research and Public Health 19, no. 1: 483. https://doi.org/10.3390/ijerph19010483
APA StyleMarin-Gomez, F. X., Mendioroz-Peña, J., Mayer, M.-A., Méndez-Boo, L., Mora, N., Hermosilla, E., Coma, E., Vilaseca, J.-M., Leis, A., Medina, M., Miró Catalina, Q., & Vidal-Alaball, J. (2022). Comparing the Clinical Characteristics and Mortality of Residential and Non-Residential Older People with COVID-19: Retrospective Observational Study. International Journal of Environmental Research and Public Health, 19(1), 483. https://doi.org/10.3390/ijerph19010483








